Pragmatic techniques for monitoring and coaching breathing
Posted: December 14, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, emotions, meditation, mindfulness, neurofeedback, Pain/discomfort, posture, relaxation, self-healing, Uncategorized | Tags: art, books, Breathing rate, coaching, FlowMD app, nasal breathing, personal-development, self-monitoring, writing 4 CommentsDaniella Matto, MA, BCIA BCB-HRV , Erik Peper, PhD, BCB, and Richard Harvey, PhD
Adapted from: Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
This blog aims to describe several practical strategies to observe and monitor breathing patterns to promote effortless diaphragmatic breathing. The goal of these strategies is to foster effortless, whole-body diaphragmatic breathing that promote health.
Breathing is usually covert and people are not usually aware of their breathing rate (breaths per minute) or pattern (abdominal or thoracic, breath holding or shallow breathing) unless they have an illness such as asthma, emphysema or are performing physical activity (Boulding et al, 2015)). Observing breathing is challenging; awareness of respiration often leads to unaware changes in the breath pattern or to an attempt to breathe perfectly (van Dixhoorn, 2021). Ideally breathing patterns should be observed/monitored when the person is unaware of their breathing pattern and the whole body participates (van Dixhoorn, 2008). A useful strategy is to have the person perform a task and then ask, “What happened to your breathing?”. For example, ask a person to simulate putting a thread through the eye of a needle or quickly look to the extreme right and left while keeping their head still. In almost all cases, the person holds their breath (Peper et al., 2002).
Teaching effortless slow diaphragmatic breathing is a precursor of Heart rate variability (HRV) biofeedback and is based on slow paced breathing (Lehrer & Gevirtz, 2014; Steffen et al., 2017; Shaffer and Meehan, 2020). Mastering effortless diaphragmatic breathing is a powerful tool in the treatment of a variety of physical, behavioural, and cognitive conditions; however, to integrate this method into clinical or educational practice is easier said than done. Clients with dysfunctional breathing patterns often have difficulty following a breath pacer or mastering effortless breathing at a slower pace.
The purpose of this paper is to describe a few simple strategies that can be used to observe and monitor breathing patterns, provide economic strategies for observation and training, and suggestions to facilitate effortless diaphragmatic breathing.
Strategies to observe and monitor breathing pattern
Observation of the breathing patterns
- Is the breathing through the nose or mouth? Nose is usually better (Watso et al., 2023; Nestor, 2020).
- Does the abdomen expand during inhalation and constricts during exhalation or does the chest expand and rise during inhalation and fall during exhalation? Abdominal movement is usually better.
- Is exhalation flow softly or explosively like a sigh? Slow flow exhalation is preferred.
- Is the breath held or continues during activities? In most cases continued breathing is usually better.
- Does the person gasp before speaking or allows to speak while normally exhaling?
- What is the breathing rate (breaths per minute)? When sitting peacefully less than 14 breaths/minute is usually better and about 6 breaths per minute to optimize HRV
Physiological monitoring.
- Monitoring breathing with strain gauges around the abdomen and chest, and heart rate is the most common approach to identify the location of breath, the breathing pattern and heart rate variability. The strain gauges are placed around the chest and abdomen and heart rate is monitored with a blood volume pulse amplitude sensor from the finger. representative recording shows the effect of thoughts on breathing, heartrate and pulse amplitude of which the participant is totally unaware as shown in Figure 1.
Figure 1. Physiological recording of breathing patterns with strain gauges.
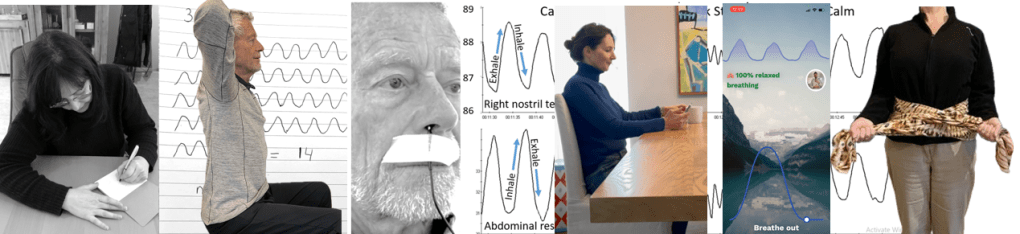
- Monitoring breathing with a thermistor placed at the entrance of the nostril that has the most airflow (nasal patency) (Jovanov et al., 2001; Lerman et al., 2016). When the person exhales through the nose, the thermistor temperature increases and decreases when they inhale. A representative recording of a person being calm, thinking a stressful thought. and being calm. Although there were significant changes as indicated by the change in breathing patterns, the person was unaware of the changes as shown in Figure 2.
Figure 2. Use of a thermistor to monitor breathing from the dominant nostril compared to the abdominal expansion as monitored by a strain gauge around the abdomen.
- Additional physiological monitoring approaches. There are many other physiological measures can be monitored to such as end-tidal carbon dioxide (EtCO2), a non-invasive measurement of the amount of carbon dioxide (CO2) in exhaled breath (Meuret et al., 2008; Meckley, 2013); scalene/trapezius EMG to identify thoracic breathing (Peper & Tibbett, 1992; Peper & Tibbets, 1994); low abdominal EMG to identify transfers and oblique tightening during exhalation and relaxation during inhalation (Peper et al., 2016; and heart rate to monitor cardiorespiratory synchrony (Shaffer & Meehan, 2020). Physiological monitoring is useful; since, the clinician and the participant can observe the actual breathing pattern in real time, how the pattern changes in response the cognitive and physical tasks, and used for feedback training. The recorded data can document breathing problems and evidence of mastery.
The challenges of using physiological monitoring arethat the equipment may be expensive, takes skill to operate and interpret the data, and is usually located in the office and not at home.
Economic strategies for observation and training breathing
To complement the physiological monitoring and allow observations outside the office and at home, some of the following strategies may be used to observe breathing pattern (rate and expansion of the breath in the body), and suggestion to facilitate effortless diaphragmatic breathing. These exercises make excellent homework for the client. Practicing awareness and internal self-regulation by the client outside the clinic contributes enormously to the effect of biofeedback training (Wilson et al., 2023),
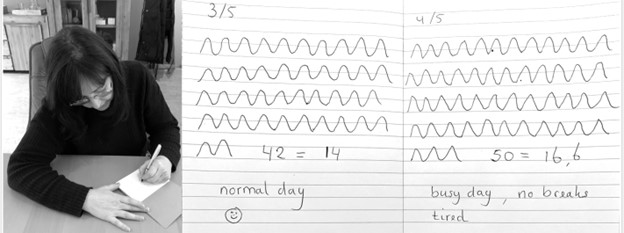
Observe breathing rate: Draw the breathing pattern
Take a piece of paper, a pen and a timer, set to 3 minutes. Start the timer. Upon inhalation draw the line up and upon exhalation draw the line down, creating a wave. When the timer stops, after 3 minutes, calculate the breathing rate per minute by dividing the number of waves by 3 as shown in Figure 3.
Figure 3. Drawing the breathing pattern for three minutes during two different days.
From these drawings, the breathing rate become evident. Many individuals are often surprised to discover that their breathing rate increased during periods of stress, such as a busy day with no breaks, compared to their normal days.
Monitoring and training diaphragmatic breathing
The scarf technique for abdominal feedback
Many participants are unaware that they are predominantly breathing in their chest and their abdomen expansion is very limited during inhalation. Before beginning, have participant loosen their belt and or stand upright since sitting collapsed/slouched or having the waist constriction such as a belt of tight constrictive clothing that inhibits abdominal expansion during inhalation.
Place the middle part of a long scarf or shawl on your lower back, take the ends in both hands and cross the ends: your left hand is holding the right part of the scarf, and the right hand is holding the left end of the scarf. Give a bit of a pull, so you can feel any movement of the scarf. When breathing more abdominally you will feel a pull at the ends of the scarf as you lower back, and flanks will expand as shown in Figure 4.

Figure 4. Using a scarf as feedback.
FlowMD app
A recent cellphone app, FlowMD, is unique because it uses the cellphone camera to detect the subtle movements of the chest and abdomen (FlowMD, 2024). It provides real time feedback of the persons breathing pattern. Using this app, the person sits in front of their cellphone camera and after calibration, the breathing pattern is displayed as shown in Figure 5.

Figure 5. Training breathing with FlowMD,.
Suggestions to optimize abdominal breathing that may lead to a slower breath rate when the client practices the technique
Beach pose
By locking the upper chest and sitting up straight it is often easier to breathe so that the abdomen can expand and constrict. Place your hands behind your head and Interlock your finger of both hands, pull your elbows back and up. The person can practice this either laying down on their back or sitting straight up at the edge of the chair as shown in Figure 6.

Figure 6. Sitting erect with the shoulders pulled back and up to allow abdominal expansion and constriction as the breathing pattern.
Observe the effect of posture on breathing
Have the person sit slouched/collapsed like a letter C and take a few slow breath, then have them sit up in a tall and erect position and take a few slow breaths. Usually they will observe that it is easier to breathe slower and lower and tall and erect.
Using your hands for feedback to guide natural breathing
Holding your hands with index fingers and thumbs touching the lower abdomen. When inhaling the fingers and thumbs separate and when exhaling they touch again (ensuring a full exhale and avoiding over breathing). The slight increase in lower abdominal muscle tension during the exhalation and relaxation during inhalation and the abdominal wall expands can also be felt with fingertips as shown in Figure 7.
Figure 7. Using your hands and finger for feedback to guide the natural breathing of expansion and constriction of the abdomen. Reproduced by permission from Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Coaching suggestions
There are many strategies to observe, teach and implement effortless breathing (Peper et al., 2024).. Even though breathing is natural and babies and young children breathe diaphragmatically as their large belly expands and constricts. Yet, in many cases the natural breathing shifts to dysfunctional breathing for multiple reasons such as chronic triggering defense reactions to avoiding pain following abdominal surgery (Peper et al, 2015). When participants initially attempt to relearn this natural pattern, it can be challenging especially, if the person habitually breathes shallowly, rapidly and predominantly in their chest.
When initially teaching effortless breathing, have the person exhale more air than normal without the upper chest compressing down and instead allow the abdomen comes in and up thereby exhaling all the air. If the person is upright then allow inhalation to occur without effort by letting the abdominal wall relaxes and expands. Initially inhale more than normal by expanding the abdomen without lifting the chest. Then exhale very slowly and continue to breathe so that the abdomen expands in 360 degrees during inhalation and constricts during exhalation. Let the breathing go slower with less and less effort. Usually, the person can feel the anus dropping and relaxing during inhalation.
Another technique is to ask the person to breathe in more air than normal and then breathe in a little extra air to completely fill the lungs, before exhaling fully. Clients often report that it teaches them to use the full capacity of the lungs.
The goal is to breath without effort. Indirectly this can be monitored by finger temperature. If the finger temperature decreases, the participant most likely is over-breathing or breathing with too much effort, creating sympathetic activity; if the finger temperature increases, breathing occurs slower and usually with less effort indicating that the person’s sympathetic activation is reduced.
Conclusion
There are many strategies to monitor and coach breathing. Relearning diaphragmatic breathing can be difficult due to habitual shallow chest breathing or post-surgical adaptations. Initial coaching may involve extended exhalations, conscious abdominal expansion, and gentle inhalation without chest movement. Progress can be monitored through indirect physiological markers like finger temperature, which reflects changes in sympathetic activity. The integration of these techniques into clinical or educational practice enhances self-regulation, contributing significantly to therapeutic outcomes. In this article we provided a few strategies which may be useful for some clients.
Additional blogs on breathing
https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
REFERENCES
Boulding, R., Stacey, R., & Niven, N. (2016). Dysfunctional breathing: a review of the literature and proposal for classification. European Respiratory Review, 25(141),: 287-294. https://doi.org/10.1183/16000617.0088-2015
FlowMD. (2024). FlowMD app. Accessed December 13, 2024. https://desktop.flowmd.co/
Jovanov, E., Raskovic, D., & Hormigo, R. (2001). Thermistor-based breathing sensor for circadian rhythm evaluation. Biomedical sciences instrumentation, 37, 493–497. https://pubmed.ncbi.nlm.nih.gov/11347441/
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Lerman, J., Feldman, D., Feldman, R. et al. Linshom respiratory monitoring device: a novel temperature-based respiratory monitor. (2016). Can J Anesth/J Can Anesth, 63, 1154–1160. https://doi.org/10.1007/s12630-016-0694-y
Meckley, A. (2013). Balancing Unbalanced Breathing: The Clinical Use of Capnographic Biofeedback. Biofeedback, 41(4), 183–187. https://doi.org/10.5298/1081-5937-41.4.02
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (2008). Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of psychiatric research, 42(7), 560–568. https://doi.org/10.1016/j.jpsychires.2007.06.005
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath-New-Science-Lost-Art/dp/0735213615/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make Health Happen. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Peper, E., & Tibbetts, V. (1992). Fifteen-month follow-up with asthmatics utilizing EMG/incentive inspirometer feedback. Biofeedback and self-regulation, 17(2), 143–151. https://doi.org/10.1007/BF01000104
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. https://biofeedbackhealth.org/wp-content/uploads/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Shaffer, F. and Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., and Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
van Dixhoorn, J.V. (2008). Whole-body breathing. Biofeedback, 36,54–58. https://www.euronet.nl/users/dixhoorn/L.513.pdf
van Dixhoorn, J.V. (2021). Functioneel ademen-Adem-en ontspannings oefeningen voor gevorderden. Amersfoort: Uiteveriy Van Dixhoorn. https://www.bol.com/nl/nl/p/functioneel-ademen/9300000132165255/
Watso, J. C., Cuba, J.N., Boutwell, S.L, Moss, J…(2023). Acute nasal breathing lowers diastolic blood pressure and increases parasympathetic contributions to heart rate variability in young adults. American Journal of Physiology Regulatory, Integrative and Comparative Physiology.
325I(6), R797-R80. https://doi.org/10.1152/ajpregu.00148.2023
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Health Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 415 338 7683 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com