360-Degree Belly Breathing with Jamie McHugh
Posted: April 26, 2024 Filed under: attention, Breathing/respiration, emotions, healing, health, meditation, mindfulness, Pain/discomfort, relaxation, self-healing | Tags: abdominal braething, belly breathing, daiphragm, effortless breathing, passive attention, self-acceptance, somatic awreness 1 Comment
Breathing is a whole mind-body experience and reflects our physical, cognitive and emotional well-being. By allowing the breath to occur effortlessly, we provide ourselves the opportunity to regenerate. Although there are many directed breathing practices that specifically directs us to inhale or exhale at specific rhythms or depth to achieve certain goals, healthy breathing is whole body experience. Many focus on being paced at a specific rhythm such as 5.5 breath per minute; however, effortless breathing is dynamic and constantly changing. It is contstantly adapting to the body’s needs: sometimes the breath is slightly slower, sometimes slightly faster, sometimes slightly deeper, sometimes slightly more shallower. The breathing process is effortless. This process can be described by the Autogenic training phrase, “It breathes me” (Luthe, 1969; Luthe, 1979; Luthe & de Rivera, 2015). Read the essay by Jamie McHugh, Registered Master Somatic Movement Therapist and then let yourself be guided in this non-striving somatic approach to allow effortless 360 degree belly breathing for regeneration.
The 360 degree belly breathing by Jamie McHugh, MSMT, is a somatic exploration to experience that breathing is not just abdominal breathing by letting the belly expand forward, but a rhythmic 360 degree increase and decrease in abdominal volume without effort. This effortless breathing pattern can often be observed in toddlers when they sit peacefully erect on the floor. This pattern of breathing not only enhances gas exchange, more importantly, it enhances abdominal blood and lymph circulation.
“The usual psychodynamic foundation for the self-experience is that of hunger, not breath. The body is experienced as an alien entity that has to be kept satisfied; the way an anxious mother might experience a new baby. When awareness is shifted from appetite to breath, the anxieties about not being enough are automatically attenuated. It requires a settling down or relaxing into one’s own body. When this fluidity moves to the forefront of awareness…there is a relaxation of the tensed self…and the emergence of a simpler, breath-based self that is capable of surrender to the moment.” – Mark Epstein (2013).
The intention behind 360 Degree Belly Breathing is to access and express the movement of the breath in all three dimensions. This is the basis for all subsequent somatic explorations within the Embodied Mindfulness protocol, a body-based approach to traditional meditation practices I have developed over the past 20 years (McHugh, 2016). Embodied Mindfulness explores the inner landscape of the body with the essential somatic technologies of breath, vocalization, self-contact, stillness and subtle movement. We focus and sustain mental attention while pleasurably cultivating bodily calm and clarity as a daily practice for survival in these turbulent times. Coupled with individual variations and experimentation, this practice becomes a reliable sanctuary from overwhelm, scattered attention, and emotional turmoil.
The Central Diaphragm
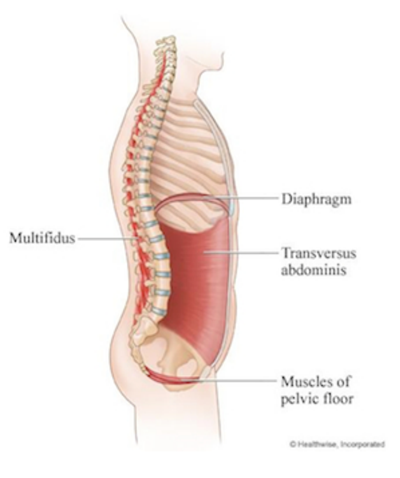
The central diaphragm, a dome-shaped muscular sheath that divides the thorax (chest) and the abdomen (belly), is the primary mechanism for breathing. It is the floor for your heart and lungs and the ceiling for your belly. The central diaphragm is a mostly impenetrable divide, with a few openings through it for the aorta, vena cava and the esophagus. Each time you inhale, the diaphragm contracts and flattens out a bit as it presses down towards your pelvis. Each time you exhale, the diaphragm relaxes and floats back up towards your heart. The motion of the diaphragm impacts the barometric pressure in your chest: the downward movement of the diaphragm on the inhale pulls oxygen into your lungs, and the subsequent exhale expels carbon dioxide into the world as the diaphragm releases upwards.
The movement of the diaphragm is twofold: involuntary and voluntary. Involuntary, ordinary breathing is a homebase and a point of return. Breathing just automatically happens – you don’t have to think about it. Breathing is also voluntary; you can choose to change the tempo (quick or slow), the duration (short or long) and quality (smooth or sharp) of this movement to “charge up and chill out” at will. Knowing how to collaborate with your diaphragm, discovering your own rhythm of diaphragmatic action, and undulating between the automatic and the chosen is a foundation for physiological equilibrium and emotional “self-soothing”.
Watch these two brief videos to get a visual image of your diaphragm in motion:
Beginning Sitting Practice
“When your back becomes straight, your mind will become quiet.” – Shunryu Suzuki
What does it mean to have a “straight back”? What are the inner coordinates and outer parameters of this position in space? And what kind of environment is needed to support this uprightness? This simple orientation to sitting can create more comfort, ease and support in your structure, which will stimulate more fluidity in your breathing and your thinking.
As you sit on a chair, consider two points of focus: body and environment. Can I sit upright with ease and comfort on this chair? If not, what changes can I make with my body and how can I adapt the environment of this chair to meet my needs? Since we are all various heights, it is not surprising a one-size-fits-all chair would need adaptation. Don’t be content with your first solution – experiment until you find just the right configuration. Valuing and seeking bodily comfort and ease are simple yet profound acts of self-kindness.
Do you need to move your pelvis forward on the chair or back? If you move your pelvis back, do you get the necessary support from the back of the chair for your pelvic bowl? If the back of the chair is too far away and/or makes you lean back into space, place a small cushion or two between the back of the chair and the base of your spine. With your back supported, are your feet on the floor? If not, place a folded blanket or a cushion under them.
With pelvis and feet in place, take a few full breaths to stabilize your pelvis and let your weight drop down through your sitz bones into the chair. The upper body receives more support from the core muscles of the lower body when your center of gravity drops – you don’t have to work so hard to maintain uprightness. Finally, rock on your sitz bones forward, backward, and side-to-side. Movement awakens bodily feedback so you can feel where center is in this moment. That sense of center will continue to change throughout the duration of the practice period so feel free to periodically adjust your position.
After this initial structural orientation, the next step is attending to the combination of breath and self-contact to fill out our self-perception. Self-contact is like using a magnifying glass – focusing the mind by feeling the substance of the belly’s movement in our hands. Since the diaphragm is a 360-degree phenomenon that generates movement in our sides and our back as well as our front, spreading awareness out not only creates different patterns of muscular activation – it also changes the brain’s map of the body and how we perceive ourselves. This change of orientation over time recalibrates our alignment and how we settle in ourselves, with awareness of our back in equal proportion to our front and sides.
360-Degree Belly Breath
“To stop your mind does not mean to stop the activities of the mind. It means your mind pervades your whole body.” – Shunryu Suzuki
Read text below or be guided by the audio file or YouTube video. http://somaticexpression.com/classes/360DegreeBreathingwithJamieMcHugh.mp3
Sit comfortably and place your hands on the front of your belly. With each inhale, become aware of the forward movement of your belly swelling. Then, with each exhale, notice the release of your belly and the settling back to center. Give this action and each subsequent action at least 5-7 breath cycles. Intersperse this way of breathing with ordinary, effortless breathing by letting the body breathe automatically. Return time and again to ordinary breathing, letting go of the focus and the effort to rest in the aftermath.
Now, slide your hands to the sides of your belly. Notice with each breath cycle how your belly moves laterally out to the sides on the inhale and then settles back to center again on the exhale.
Now, slide your hands to the back of your belly. You may wish to make contact with the back of your hands instead of your palms if it is more comfortable. With each inhale, focus on the movement into the backspace – this will be much smaller than the movement to the front; and with each exhale, the movement settling back to center.
Finally, connect all three directions: your belly radiates out 360 degrees on the horizon with each inhale, simultaneously moving forward, backward, and out to both sides, and then settles inward with each exhale.
Finish with open awareness – scanning your whole inner landscape from feet to head, back to front, and center to extremities, and letting your body breathe itself, as you notice what is alive in you now.
Inhale – Belly Radiates Outwards; Exhale – Belly Settles Inwards
“The belly is an extraordinary diagnostic instrument. It displays the armoring of the heart as a tension in the belly. Trying tightens the belly. Trying stimulates judgment. Hard belly is often judging belly. Observing the relative openness or closedness of the belly gives insight into when and how we are holding (on) to our pain. The deeper our relationship to the belly, the sooner we discover if we are holding in the mind or opening into the heart.” – Steven Levine (1991)
The contact of your hands on your belly helps the mind pay attention to the subtle movement created by the inhale-exhale cycle of the diaphragm. The combination of tactility and interoceptive awareness focusing on the belly shifts attention into our “second brain” (the enteric nervous system) and signals the mind it can rest and soften. More pleasurable sensation is often accompanied by an emergent feeling of safety as you settle into sensing the rhythm of a slower, more even breath, creating a feedback loop between bodily/somatic ease and mental calm. Giving yourself some daily “breathing room” in this way can help you build the calm muscle!
Naturally, there can be hiccups along the way so it is not all unicorns and rainbows! By giving the mind bodily tasks to accomplish, particularly in relationship to deepening and expanding the movement of the breath, we ease the self into a slower, more receptive state of being. Yet, in this receptive state of ease, whatever is in the background of awareness can arise and slip through the “border control”, sometimes taking us by surprise and causing distress. Depending upon the nature of the information, there are layers of action strategies that can be progressively taken to modulate and buffer what arises:
Tether your awareness to the breath rhythm with hands on your belly to stay present as a witness. Next step up: open your eyes softly and look around to orient in your present environment. Further step up: breath flow, hands-on belly, eyes open a wee bit looking around, and adding simple movement, like rocking a bit in all directions or expressing an exhale as a sigh, a yawn or a hum.
Note: If you find your personal resources are insufficient, find a guide to work with one-on-one to discover your own individual path for increasing the “window of capacity”. Above all, be gentle with yourself – take your time – cultivate your garden – and enjoy your breath!
References
Epstein, M. (2013) Thoughts without a Thinker: Psychotherapy from a Buddhist Perspective. New York: Basic Books. https://www.amazon.com/Thoughts-Without-Thinker-Psychotherapy-Perspective/dp/0465050948
Levine, S. (1991). Guided Meditations, Explorations and Healings. New York: Anchor. https://www.amazon.com/Guided-Meditations-Explorations-Healings-Stephen/dp/0385417373
Luthe, W. (1969). Autogenic Therapy Volume 1 Autogenic Methods. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-1-Methods/dp/B0013457B4/
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & de Rivera, L. (2015). Wolfgang Luthe Introductory workshop: Introduction to the Methods of Autogenic Training, Therapy and Psychotherapy (Autogenic Training & Psychotherapy). CreateSpace Independent Publishing Platform. https://www.amazon.com/WOLFGANG-LUTHE-INTRODUCTORY-WORKSHOP-Psychotherapy/dp/1506008038/
Is mindfulness training old wine in new bottles?
Posted: January 11, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, healing, health, meditation, self-healing, stress management | Tags: anxiety, autogenic training, biofeedback, health, meditation, mental-health, mindfulness, pain, passive attention, progressive muscle relaxation, wellness, yoga Leave a commentAdapted from: Peper, E., Harvey, R., & Lin, I-M. (2019). Mindfulness training has themes common to other technique. Biofeedback. 47(3), 50-57. https://doi.org/10.5298/1081-5937-47.3.02
This extensive blog discusses the benefits of mindfulness-based meditation (MM) techniques and explores how similar beneficial outcomes occur with other mind-centered practices such as transcendental meditation, and body-centered practices such as progressive muscle relaxation (PMR), autogenic training (AT), and yoga. For example, many standardized mind-body techniques such as mindfulness-based stress reduction and mindfulness-based cognitive therapy (a) are associated with a reduction in symptoms of symptoms such as anxiety, pain and depression. This article explores the efficacy of mindfulness based techniques to that of other self-regulation techniques and identifies components shared between mindfulness based techniques and several previous self-regulation techniques, including PMR, AT, and transcendental meditation. The authors conclude that most of the commonly used self-regulation strategies have comparable efficacy and share many elements.
Mindfulness-based strategies are based in ancient Buddhist practices and have found acceptance as one of the major contemporary behavioral medicine techniques (Hilton et al, 2016; Khazan, 2013). Throughout this blog the term mindfulness will refer broadly to a mental state of paying total attention to the present moment, with a non-judgmental awareness of the inner and/ or outer experiences (Baer et al., 2004; Kabat-Zinn, 1994).
In 1979, Jon Kabat-Zinn introduced a manual for a standardized Mindfulness-Based Stress Reduction (MBSR) program at the University of Massachusetts Medical Center (Kabat-Zinn, 1994, 2003). The eight-week program combined mindfulness as a form of insight meditation with specific types of yoga breathing and movements exercises designed to focus on awareness of the mind and body, as well as thoughts, feelings, and behaviors.
There is a substantial body of evidence that mindfulness-based cognitive therapy (MBCT); Teasdale et al., 1995) and mindfulness-based stress reduction (MBSR) (Kabat-Zinn, 1994, 2003) have combined with skills of cognitive therapy for ameliorating stress symptoms such as negative thinking, anxiety and depression. For example, MBSR and MBCT has been confirmed to be clinical beneficial in alleviating a variety of mental and physical conditions, for people dealing with anxiety, depression, cancer-related pain and anxiety, pain disorder, or high blood pressure (The following are only a few of the hundred studies published: Andersen et al., 2013; Carlson et al., 2003; Fjorback et al., 2011; Greeson, & Eisenlohr-Moul, 2014; Hoffman et al., 2012; Marchand, 2012; Baer, 2015; Demarzo et al., 2015; Khoury et al, 2013; Khoury et al, 2015; Chapin et al., 2014; Witek Janusek et al., 2019). Currently, MBSR and MBCT techniques that are more standardized are widely applied in schools, hospitals, companies, prisons, and other environments.
The Relationship Between Mindfulness and Other Self-Regulation Techniques
This section addresses two questions: First, how do mindfulness-based interventions compare in efficacy to older self-regulation techniques? Second, and perhaps more basically, how new and different are mindfulness-based therapies from other self-regulation-oriented practices and therapies?
Is mindfulness more effective than other mind/body body/mind approaches?
Although mindfulness-based meditation (MM) techniques are effective, it does not mean that is is more effective than other traditional meditation or self-regulation approaches. To be able to conclude that MM is superior, it needs to be compared to equivalent well-coached control groups where the participants were taught other approaches such as progressive relaxation, autogenic training, transcendental meditation, or biofeedback training. In these control groups, the participants would be taught by practitioners who were self-experienced and had mastered the skills and not merely received training from a short audio or video clip (Cherkin et al, 2016). The most recent assessment by the National Centere for Complementary and Integrative Health, National Institutes of Health (NCCIH-NIH, 2024) concluded that generally “the effects of mindfulness meditation approaches were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise especially when they include how to generalize the skills during the day” (NCCIH, 2024). Generalizing the learned skills into daily life contributes to the successful outcome of Autogenic Training, Progressive Relaxation, integrated biofeedback stress management training, or the Quieting Response (Luthe, 1979; Davis et al., 2019; Wilson et al., 2023; Stroebel, 1982).
Unfortunately, there are few studies that compare the effective of mindfulness meditation to other sitting mental techniques such as Autogenic Training, Transcendental Meditation or similar meditative practices that are used therapeutically. When the few randomized control studies of MBSR versus autogenic training (AT) was done, no conclusions could be drawn as to the superior stress reduction technique among German medical students (Kuhlmann et al., 2016).
Interestingly, Tanner, et al (2009) in a waitlist study of students in Washington, D.C. area universities practicing TM used the concept of mindfulness, as measured by the Kentucky Inventory of Mindfulness Skills (KIM) (Baer et al, 2004) as a dependent variable, where TM practice resulted in greater degrees of ‘mindfulness.’ More direct comparisons of MM with body-focused techniques, such as progressive relaxation, or Autogenic training mindfulness-based approaches, have not found superior benefit. For example, Agee et al (2009) compared the stress management effects of a five-week Mindfulness Meditation (MM) to a five-week Progressive Muscle Relaxation (PMR) course and found no meaningful reports of superiority of one over the other program; both MM and PMR were effective in reducing symptoms of stress.
In a persuasive meta-analysis comparing MBSR with other similar stress management techniques used among military service members, Crawford, et al (2013) described various multimodal programs for addressing post-traumatic stress disorder (PTSD) and other military or combat-related stress reactions. Of note, Crawford, et al (2013) suggest that all of the multi-modal approaches that include Autogenic Training, Progressive Muscle Relaxation, movement practices including Yoga and Tai Chi, as well as Mindfulness Meditation, and various types of imagery, visualization and prayer-based contemplative practices ALL provide some benefit to service members experiencing PTSD.
An important observation by Crawford et al (2013) pointed out that when military service members had more physical symptoms of stress, the meditative techniques appeared to work best, and when the chief complaints were about cognitive ruminations, the body techniques such as Yoga or Tai Chi worked best to reduce symptoms. Whereas it may not be possible to say that mindfulness meditation practices are clearly superior to other mind-body techniques, it may be possible to raise questions about mechanisms that unite the mind-body approaches used in therapeutic settings.
Could there be negative side effects?
Another point to consider is the limited discussion of the possible absence of benefit or even harms that may be associated with mind-body therapies. For example, for some people, meditation does not promote prosocial behavior (Kreplin et al, 2018). For other people, meditation can evoke negative physical and/or psychological outcomes (Lindahl et al, 2017; Britton et al., 2021). There are other struggles with mind-body techniques when people only find benefit in the presence of a skilled clinician, practitioner, or guru, suggesting a type of psychological dependency or transference, rather than the ability to generalize the benefits outside of a set of conditions (e.g. four to eight weeks of one to four hour trainings) or a particular setting (e.g. in a natural and/or quiet space).
Whereas the detailed instructions for many mindfulness meditation trainings, along with many other types of mind-body practices (e.g. Transcendental Meditation, Autogenic Training, Progressive Muscle Relaxation, Yoga, Tai Chi…) create conditions that are laudable because they are standardized, a question is raised as to ‘critical ingredients’, using the metaphor of baking. The difference between a chocolate and a vanilla cake is not ingredients such as flour, or sugar, etc., which are common to all cakes, but rather the essential or critical ingredient of the chocolate or vanilla flavoring. So what are the essential or critical ingredients in mind-body techniques? Extending the metaphor, Crawford, et al (2013, p. 20) might say the critical ingredient common to the mind-body techniques they studied was that people “can change the way their body and mind react to stress by changing their thoughts, emotions, and behaviors…” with techniques that, relatively speaking, “involve minimal cost and training time.”
The skeptical view suggested here is that MM techniques share similar strategies with other mind-body approaches that encouraging learners to ‘pay attention and shift intention.’ This strategy is part of the instructions when learning Progressive Relaxation, Autogenic Training, Transcendental Meditation, movement meditation of Yoga and Tai Chi and, with instrumented self-regulation techniques such as bio/neurofeedback. In this sense, MM training repackages techniques that have been available for millennia and thus becomes ‘old wine sold in new bottles.’
We wonder if a control group for compassionate mindfulness training would report more benefits if they were asked not only to meditate on compassionate acts, but actually performed compassionate tasks such as taking care of person in pain, helping a homeless person, or actually writing and delivering a letter of gratitude to a person who has helped them in the past? The suggestion is to titrate the effects of MM techniques, moving from a more basic level of benefit to a more fully actualized level of benefit, generalizing their skill beyond a training setting, as measured by the Baer et al (2004) Kentucky Inventory of Mindfulness Skills.
Each generation of clinicians and educators rediscover principles without always recognizing that the similar principles were part of the previous clinical interventions. The analogies and language has changed; however, the underlying concepts may be the same. Mindfulness interventions are now the new, current and popular approach. Some of the underlying ‘mindfulness’ concepts that are shared in common with successfully other mind-body and self-regulation approaches include:
The practitioner must be self-experienced in mindfulness practice. This means that the practitioners do not merely believe the practice is effective; they know it is effective from self-experience. Inner confidence conveyed to clients and patients enhances the healing/placebo effect. It is similar to having sympathy or empathy for clients and patients that occurs from have similar life experiences, such as when a clinician speaks to a patient. For example, a male physician speaking to a female patient who has had a mastectomy may be compassionate; however, empathy occurs more easily when another mastectomy patient (who may also be a physician) shares how she struggled overcame her doubts and can still be loved by her partner.
There may also be a continuum of strengthening beliefs about the benefits of mindfulness techniques that leads to increase benefits for the approach. Knowing there are some kinds of benefits from initiating a practice of mindfulness increases empathy/compassion for others as they learn. Proving that mindfulness techniques are causing benefits after systematically comparing their effectiveness with other approaches strengthens the belief in the mindfulness approaches. Note that a similar process of strengthening one’s belief in an approach occurs gradually, over time as clients and patients progress through beginner, intermediate and advanced levels of mind-body practices.
Observing thoughts without being captured. Being a witness to the thoughts, emotions, and external events results in a type of covert global desensitization and skill mastery of NOT being captured by those thoughts and emotions. This same process of non-attachment and being a witness is one of the underpinnings of techniques that tacitly and sometime covertly support learning ways of controlling attention, such as with Autogenic Training; namely how to passively attend to a specific body part without judgment and, report on the subjective experience without comparison or judgment.
Ongoing daily practice. Participants take an active role in their own healing process as they learn to control and focus their attention. Participants are often asked to practice up to one hour a day and apply the practices during the day as mini-practices or awareness cues to interrupt the dysfunctional behavior. For example in Autogenic training, trainees are taught to practice partial formula (such my “neck and shoulders are heavy”) during the day to bring the body/mind back to balance. While with Progressive Relaxation, the trainee learns to identify when they tighten inappropriate muscles (dysponesis) and then inhibit this observed tension.
Peer support by being in a group. Peer support is a major factor for success as people can share their challenges and successes. Peer support tends to promote acceptance of self-and others and provides role modeling how to cope with stressors. It is possible that some peer support groups may counter the benefits of a mind-body technique, especially when the peers do not provide support or may in fact impede progress when they complain of the obstacles or difficulties in their process.
These concepts are not unique to Mindfulness Meditation (MM) training. Similar instructions have been part of the successful/educational intervention of Progressive Relaxation, Autogenic Training, Yogic practices, and Transcendental Meditation. These approaches have been most successful when the originators, and their initial students, taught their new and evolving techniques to clients and patients; however, they became less successful as later followers and practitioners used these approaches without learning an in-depth skill mastery. For example, Progressive relaxation as taught by Edmund Jacobson consisted of advanced skill mastery by developing subtle awareness of different muscle tension that was taught over 100 sessions (Mackereth & Tomlinson, 2010). It was not simply listening once to a 20-minute audio recording about tightening and relaxing muscles. Similarly, Autogenic training is very specific and teaches passive attention over a three to six-month time-period while the participant practices multiple times daily. Stating the obvious, learning Autogenic Training, Mindfulness, Progressive Relaxation, Bio/Neurofeedback or any other mind-body technique is much more than listening to a 20-minute audio recording.
The same instructions are also part of many movement practices. For many participants focusing on the movement automatically evoked a shift in attention. Their attention is with the task and they are instructed to be present in the movement.
Areas to explore.
Although Mindfulness training with clients and patients has resulted in remarkable beneficial outcomes for the participants, it is not clear whether mindfulness training is better than well taught PR, AT, TM or other mind/body or body/mind approaches. There are also numerous question to explore such as: 1) Who drops out, 2) Is physical exercise to counter sitting disease and complete the alarm reaction more beneficial, and 3) Strategies to cope with wandering attention.
- Who drops out?
We wonder if mindfulness is appropriate for all participants as sometimes participants drop out or experience negative abreactions. It not clear who those participants are. Interestingly, hints for whom the techniques may be challenging can be found in the observations of Autogenic Training that lists specific guidelines for contra-, relative- and non-indications (Luthe, 1970).
- Physical movement to counter sitting disease and complete the alarm reaction.
Although many mindfulness meditation practices may include yoga practices, most participants practice it in a sitting position. It may be possible that for some people somatic movement practices such as a slow Zen walk may quiet the inner dialogue more quickly. In our experience, when participants are upset and highly stressed, it is much easier to let go of agitation by first completing the triggered fight/flight response with vigorous physical activity such as rapidly walking up and downs stairs while focusing on the burning sensations of the thigh muscles. Once the physical stress reaction has been completed and the person feels physically calmer then the mind is quieter. Then have the person begin their meditative practice.
- Strategies to cope with wandering attention.
Some participants have difficulty staying on task, become sleepy, worry, and/or are preoccupied. We observed that first beginning with physical movement practices or Progressive Relaxation appears to be a helpful strategy to reduce wandering thoughts. If one has many active thoughts, progressive relaxation continuously pulls your attention to your body as you are directed to tighten and let go of muscle groups. Being guided supports developing the passive focus of attention to bring awareness back to the task at hand. Once internally quieter, it is easier hold their attention while doing Autogenic Training, breathing or Mindfullness Meditation.
By integrating somatic components with the mindfulness such as done in Progressive Relaxation or yoga practices facilitates the person staying present. Similarly, when teaching slower breathing, if a person has a weight on their abdomen while practicing breathing, it is easier to keep attending to the task: allow the weight to upward when inhaling and feeling the exhalation flowing out through the arms and legs.
Therapeutic and education strategies that implicitly incorporate mindfulness
Progressive relaxation
In the United States during the 1920 progressive relaxation (PR) was developed and taught by Edmund Jacobson (1938). This approach was clinically very successful for numerous illnesses ranging from hypertension, back pain, gastrointestinal discomfort, and anxiety; it included 50 year follow-ups. Patients were active participants and practiced the skills at home and at work and interrupt their dysfunctional patterns during the day such as becoming aware of unnecessary muscle tension (dyponetic activity) and then release the unnecessary muscle tension (Whatmore & Kohli, 1968). This structured approach is totally different than providing an audio recording that guides clients and patients through a series of tightening and relaxing of their muscles. The clinical outcome of PR when taught using the original specific procedures described by Jacobson (1938) was remarkable. The incorporation of Progressive Relaxation as the homework practice was an important cofactor in the successful outcome in the treatment of muscle tension headache using electromyography (EMG) biofeedback by Budzynski, Stoyva and Adler (1970).
Autogenic Training
In 1932 Johannes Schultz in Germany published a book about Autogenic Training describing the basic training procedure. The basic autogenic procedure, the standard exercises, were taught over a minimum period of three month in which the person practiced daily. In this practice they directed theri passive attention to the following cascading sequence: heaviness of their arms, warmth of their arms, heart beat calm and regular, breathing calm and regular or it breathes me, solar plexus is warm, forehead is cool, and I am at peace (Luthe, 1979). Three main principles of autonomic training mentioned by Luthe (1979) are: (1) mental repetition of topographically oriented verbal formulae for brief periods; (2) passive concentration; and (3) reduction of exteroceptive and proprioceptive afferent stimulation. The underlying concepts of Autogenic Therapy include as described by Peper and Williams (1980):
The body has an innate capacity for self-healing and it is this capacity that is allowed to become operative in the autogenic state. Neither the trainer nor trainee has the wisdom necessary to direct the course of the self-balancing process; hence, the capacity is allowed to occur and not be directed.
- Homeostatic self-regulation is encouraged.
- Much of the learning is done by the trainee at home; hence, the responsibility for the training lies primarily with the trainee.
- The trainer/teacher must be self-experience in the practice.
- The attitude necessary for successful practice is one of passive attention; active striving and concern with results impedes the learning process. An attitude of acceptance is cultivated, letting be whatever comes up. This quality of attention is known as “mindfulness’ in meditative traditions.
The clinical outcome for autogenic therapy is very promising. The detailed guided self-awareness training and uncontrolled studies showed benefits across a wide variety of psychosomatic illness such as asthma, cancer, hypertension, anxiety, pain irritable bowel disease, depression (Luthe & Schultz, 1970a; Luthe & Schultz, 1970b). Autogenic training components have also been integrated in biofeedback training. Elmer and Alice Green included the incorporation of autogenic training phrases with temperature biofeedback for the very successful treatment of migraines (Green & Green, 1989). Autonomic training combine with biofeedback in clinical practices produced better results than control group for headache population (Luthe, 1979). Empirical research found that autonomic training was applied efficiently in emotional and behavioral problems, and physical disorder (Klott, 2013), such as skin disorder (Klein & Peper, 2013), insomnia (Bowden et al., 2012), Meniere’s disease (Goto, Nakai, & Ogawa, 2011) and the multitude of stress related symptoms (Wilson et al., 2023).
Bio/neurofeedback training
Starting in the late 1960s, biofeedback procedures have been developed as a successful treatment approach for numerous illnesses ranging from headaches, hypertension, to ADHD (Peper et al., 1979; Peper & Shaffer, 2010; Khazan, 2013). In most cases, the similar instructions that are part of mindfulness meditation are also embedded in the bio/neurofeedback instructions. The participants are instructed to learn control over some physiological parameter and then practice the same skill during daily life. This means that during the learning process, the person learn passive attention and is not be captured by marauding thoughts and feeling. and during the day develop awareness Whenever they become aware of dysfunctional patterns, thoughts, emotions, they initiated their newly learned skill. The ongoing biological feedback signals continuously reminds them to focus.
Transcendental meditation
The next fad to hit the American shore was Transcendental Meditation (TM)– a meditation practice from the ancient Vedic tradition in India. The participant were given a mantra that they mentally repeated and if their attention wanders, they go back to repeating the mantra internally. The first study that captured the media’s attention was by Wallace (1970) published in the Journal Science which reported that “During meditation, oxygen consumption and heart rate decreased, skin resistance increased, and the electroencephalogram showed specific changes in certain frequencies. These results seem to distinguish the state produced by Transcendental Meditation from commonly encountered states of consciousness and suggest that it may have practical applications.” (Wallace, 1970).
The participants were to practice the mantra meditation twice a day for about 20 minutes. Meta-analysis studies have reported that those who practiced TM as compared to the control group experienced significant improved of numerous disorders such as CVD risk factors, anxiety, metabolic syndrome, drug abuse and hypertension (Paul-Labrador et al, 2006; Rainforth et al., 2007; Hawkins, 2003).
To make it more acceptable for the western audience, Herbert Benson, MD, adapted and simplified techniques from TM training and then labelled a core element, the ‘relaxation response’ (Benson et al., 1974) Instead of giving people a secret mantra and part of a spiritual tradition, he recommend using the word “one” as the mantra. Numerous studies have demonstrated that when patients practice the relaxation response, many clinical symptoms were reduced. The empirical research found that practiced transcendental meditation caused increasing prefrontal low alpha power (8-10Hz) and theta power of EEG; as well as higher prefrontal alpha coherence than other locations at both hemispheres. Moreover, some individuals also showed lower sympathetic activation and higher parasympathetic activation, increased respiratory sinus arrhythmic and frontal blood flow, and decreased breathing rate (Travis, 2001, 2014). Although TM and Benson’s relaxation response continues to be practiced, mindfulness has taking it place.
Conclusion
Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) are very beneficial and yet may be considered ‘old wine in new bottles’ where the metaphor refers to millennia old meditation techniques as ‘old wine’ and the acronyms such as MBSR or MBCT as ‘new bottles’. Like many other ‘new’ therapeutic approaches or for that matter, many other ‘new’ medications, use it now before it becomes stale and loses part of its placebo power. As long as the application of a new technique is taught with the intensity and dedication of the promotors of the approach, and as long as the participants are required to practice while receiving support, the outcomes will be very beneficial, and most likely similar in effect to other mind-body approaches.
The challenge facing mindfulness practices just as those from Autogenic Training, Progressive Relaxation and Transcendental Meditation, is that familiarity breeds contempt and that clients and therapists are continuously looking for a new technique that promises better outcome. Thus as Mindfulness training is taught to more and more people, it may become less promising. In addition, as mindfulness training is taught in less time, (e.g. fewer minutes and/or fewer sessions), and with less well-trained instructors, who may offer less support and supervision for people experiencing possible negative effects, the overall benefits may decrease. Thus, mindfulness practice, Autogenic training, progressive relaxation, Transcendental Meditation, movement practices, meditation, breathing practices as well as the many spiritual practices all appear to share common fate of fading over time. Whereas the core principles of mind-body techniques are ageless, the execution is not always assured.
References
Agee, J. D., Danoff-Burg, S., & Grant, C. A. (2009). Comparing brief stress management courses in a community sample: Mindfulness skills and progressive muscle relaxation. Explore: The Journal of Science and Healing, 5(2), 104-109. https://doi.org/10.1016/j.explore.2008.12.004
Andersen, S. R., Würtzen, H., Steding-Jessen, M., Christensen, J., Andersen, K. K., Flyger, H., … & Dalton, S. O. (2013). Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients. Acta Oncologica, 52(2), 336-344. https://doi.org/10.3109/0284186X.2012.745948
Alvarez-Jimenez, M., Gleeson, J. F., Bendall, S., Penn, D. L., Yung, A. R., Ryan, R. M., … Nelson, B. (2018). Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy. Schizophrenia Research, 202, 369-377 https://doi.org/10.1016/j.schres.2018.07.022
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. https://doi.org/10.1093/clipsy/bpg015
Baer, R. A.. (2015). Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. New York: Elsevier. https://www.elsevier.com/books/mindfulness-based-treatment-approaches/baer/978-0-12-416031-6
Baer, R., Smith, G., & Allen, K. (2004). Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment, 11, 191–206. https://doi.org/10.1177/1073191104268029
Benson, H., Beary, J. F., & Carol, M. P. (1974).The Relaxation Response. Psychiatry, 37(1), 37-46. https://www.tandfonline.com/loi/upsy20
Bowden, A., Lorenc, A., & Robinson, N. (2012). Autogenic Training as a behavioural approach to insomnia: A prospective cohort study. Primary Health Care Research & Development, 13, 175-185. https://doi.org/10.1017/S1463423611000181
Britton, W.B., Lindahl, J.R., Coope, D.J., Canby, N.K., & Palitsky, R. (2021). Defining and Measuring Meditation-Related Adverse Effects in Mindfulness-Based Programs. Clinical Psychological Science, 9(6), 1185-1204. https://doi.org/10.1177/2167702621996340
Budzynski, T., Stoyva, J., & Adler, C. (1970). Feedback-induced muscle relaxation: Application to tension headache. Journal of Behavior Therapy and Experimental Psychiatry, 1(3), 205-211. https://doi.org/10.1016/0005-7916(70)90004-2
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2003). Mindfulness‐based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine, 65(4), 571-581. https://doi.org/10.1097/01.psy.0000074003.35911.41
Chapin, H. L., Darnall, B. D., Seppala, E. M., Doty, J. R., Hah, J. M., & Mackey, S. C. (2014). Pilot study of a compassion meditation intervention in chronic pain. J Compassionate Health Care, 1(4), 1-12. https://doi.org/10.1186/s40639-014-0004-x
Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., … & Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA, 315(12), 1240-1249. https://doi.org/10.1001/jama.2016.2323
Crawford, C., Wallerstedt, D. B., Khorsan, R., Clausen, S. S., Jonas, W. B., & Walter, J. A. (2013). A systematic review of biopsychosocial training programs for the self-management of emotional stress: Potential applications for the military. Evidence-Based Complementary and Alternative Medicine, 747694: 1-23. https://doi.org/10.1155/2013/747694
Davis, M., Eshelman, E.R., & McKay, M. (2019). The Relaxation and Stress Reduction Workbook. Oakland, CA: New Harbinger Publications. https://www.amazon.com/Relaxation-Reduction-Workbook-Harbinger-Self-Help/dp/1684033349
Demarzo, M. M., Montero-Marin, J., Cuijpers, P., Zabaleta-del-Olmo, E., Mahtani, K. R., Vellinga, A., Vincens, C., Lopez del Hoyo, Y., & García-Campayo, J. (2015). The efficacy of mindfulness-based interventions in primary care: A meta-analytic review. The Annals of Family Medicine, 13(6), 573-582. https://doi.org/10.1370/afm.1863
Fjorback, L. O., Arendt, M., Ørnbøl, E., Fink, P., & Walach, H. (2011). Mindfulness‐Based Stress Reduction and Mindfulness‐Based Cognitive Therapy–A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica, 124(2), 102-119. https://doi.org/10.1111/j.1600-0447.2011.01704.x
Goto, F., Nakai, K., & Ogawa, K. (2011). Application of autogenic training in patients with Meniere disease. European Archives of Oto-Rhino-Laryngology, 268(10), 1431-1435. https://doi.org/10.1007/s00405-011-1530-1
Greeson, J., & Eisenlohr-Moul, T. (2014). Mindfulness-based stress reduction for chronic pain. In R. A. Baer (Ed.), Mindfulness-Based Treatment Approaches: Clinician’s Guide to Evidence Base and Applications, 269-292. San Diego, CA: Academic Press. https://psycnet.apa.org/record/2014-40932-000
Green, E. and Green, A. (1989). Beyond Biofeedback. New York: Knoll. https://www.amazon.com/Beyond-Biofeedback-Elmer-Green/dp/0940267144
Hawkins, M. A. (2003). Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery. Journal of Offender Rehabilitation, 36(1-4), 47- 65. https://doi.org/10.1300/J076v36n01_03
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., …Maglione, M. A. (2016). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199-213. https://doi.org/10.1007/s12160-016-9844-2
Hoffman, C. J., Ersser, S. J., Hopkinson, J. B., Nicholls, P. G., Harrington, J. E., & Thomas, P. W. (2012). Effectiveness of mindfulness-based stress reduction in mood, breast-and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology, 30(12), 1335-1342. https://doi.org/10.1200/JCO.2010.34.0331
Jacobson, E. (1938). Progressive relaxation. Chicago, IL: University of Chicago Press. https://www.amazon.com/Progressive-Relaxation-Physiological-Investigation-Significance/dp/0226390594
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion. https://www.amazon.com/Wherever-You-There-Are-Mindfulness/dp/0306832011
Kabat-Zinn, J. (2003). Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences, 8, 73–107. https://psycnet.apa.org/record/2004-19791-008
Khazan, I. Z. (2013). The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. New York: John Wiley & Sons. https://www.amazon.com/Clinical-Handbook-Biofeedback-Step-Step/dp/1119993717
Klein, A., & Peper, E. (2013). There Is hope: Autogenic biofeedback training for the treatment of psoriasis. Biofeedback, 41 (4), 194-201. https://doi.org/10.5298/1081-5937-41.4.01
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763-771. https://doi.org/10.1016/j.cpr.2013.05.005
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519-528.
Klott, O. (2013). Autogenic Training–a self-help technique for children with emotional and behavioural problems. Therapeutic Communities: The International Journal of Therapeutic Communities, 34(4), 152-158. https://doi.org/10.1108/TC-09-2013-0027
Kreplin, U., Farias, M., & Brazil, I. A. (2018). The limited prosocial effects of meditation: A systematic review and meta-analysis. Sci Rep, 8, 2403. https://doi.org/10.1038/s41598-018-20299-z
Kuhlmann, S. M., Huss, M., Bürger, A., & Hammerle, F. (2016). Coping with stress in medical students: results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Medical Education, 16(1), 316. https://doi.org/10.1186/s12909-016-0833-8
Lindahl, J. R., Fisher, N. E., Cooper, D. J., Rosen, R. K, & Britton, W. B. (2017). The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoSONE, 12(5): e0176239. https://doi.org/10.1371/journal.pone.0176239
Luthe, W. (1970). Autogenic therapy: Research and theory. New York: Grune and Stratton. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/abs/autogenic-therapy-edited-by-wolfgang-luthe-volume-4-research-and-theory-by-wolfgang-luthe-grune-and-stratton-new-york-1970-pp-276-price-1475/6C8521C36C37254A08AAD1F2FE08211C
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970a). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
Luthe, W. & Schultz, J. H. (1970b). Autogenic therapy: Applications in psychotherapy. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-Applications-Psychotherapy-v/dp/0808902725
Mackereth, P.A. & Tomlinson, L. (2010). Progressive muscle relaxation. In Cawthorn, A. & Mackereth, P.A. eds. Integrative Hypnotherapy. London: Churchill Livingstone. https://www.amazon.com/Integrative-Hypnotherapy-Complementary-approaches-clinical/dp/0702030821
Marchand, W. R. (2012). Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice, 18(4), 233-252. https://doi.org/10.1097/01.pra.0000416014.53215.86
NCCIH (2024). Meditation and Mindfulness: What You Need To Know. National Center for Complementary and Integrative Health, National Institutes of Health. Accessed January 31, 2024. https://www.nccih.nih.gov/health/meditation-and-mindfulness-what-you-need-to-know?
Paul-Labrador, M., Polk, D., Dwyer, J.H. et al. (2006). Effects of a randomized controlled trial of Transcendental Meditation on components of the metabolic syndrome in subjects with coronary heart disease. Archive of Internal Medicine, 166(11), 1218-1224. https://doi.org/10.1001/archinte.166.11.1218
Peper, E., Ancoli, S. & Quinn, M. (Eds). (1979). Mind/Body Integration: Essential Readings in Biofeedback. New York: Plenum. https://www.amazon.com/Mind-Body-Integration-Essential-Biofeedback/dp/0306401029
Peper, E. & Shaffer, F. (2010). Biofeedback History: An Alternative View. Biofeedback, 38 (4): 142–147. https://doi.org/10.5298/1081-5937-38.4.03
Peper, E., & Williams, E.A. (1980). Autogenic therapy. In A. C. Hastings, J. Fadiman, & J. S. Gordon (Eds.), Health for the whole person (pp137-141).. Boulder: Westview Press. https://biofeedbackhealth.files.wordpress.com/2016/02/autogenic-therapy-peper-and-williams.pdf
Rainforth, M.V., Schneider, R.H., Nidich, S.I., Gaylord-King, C., Salerno, J.W., & Anderson, J.W. (2007). Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Current Hypertension Reports, 9(6), 520–528. https://doi.org/10.1007/s11906-007-0094-3
Stroebel, C. (1982). QR: The Quieting Reflex. New York: Putnam Pub Group. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570
Tanner, M. A., Travis, F., Gaylord‐King, C., Haaga, D. A. F., Grosswald, S., & Schneider, R. H. (2009). The effects of the transcendental meditation program on mindfulness. Journal of Clinical Psychology 65(6), 574-589. https://doi.org/10.1002/jclp.20544
Teasdale, J. D., Segal, Z., & Williams, J. M. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy, 33, 25–39. https://doi.org/10.1016/0005-7967(94)e0011-7
Travis, F. (2001). Autonomic and EEG patterns distinguish transcending from other experiences during transcendental meditation practice. International Journal of Psychophysiology, 42, 1–9. https://doi.org/10.1016/s0167-8760(01)00143-x
Travis, F. (2014). Transcendental experiences during meditation practice. Annals of the New York Academy of Sciences, 1307, 1–8. https://doi.og10.1111/nyas.12316
Wallace, K.W. (1970). Physiological Effects of Transcendental Meditation. Science, 167 (3926), 1751-1754. https://doi.org/10.1126/science.167.3926.1751
Whatmore, G. B., & Kohli, D. R. (1968). Dysponesis: A neurophysiologic factor in functional disorders. Behavioral Science, 13(2), 102–124. https://doi.org/10.1002/bs.3830130203
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
Witek Janusek, L., Tel,l D., & Mathews, H.L. (2019). Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: A randomized trial with active control. Brain Behav Immun, 80:358-373. https://doi.org/10.1016/j.bbi.2019.04.012
Mind-Guided Body Scans for Awareness and Healing Youtube Interview of Erik Peper, PhD by Larry Berkelhammer, PhD
Posted: February 19, 2016 Filed under: Uncategorized | Tags: autogenic training, body scan, mind-body, mindfulness, pain, passive attention, stress management Leave a commentIn this interview psychophysiology expert Dr. Erik Peper explains the ways how a body scan can facilitate awareness and healing. The discussion describes how the mind-guided body scan can be used to improve immune function and maintain passive attention (mindfulness), and become centered. It explores the process of passive attentive process that is part of Autogenic Training and self-healing mental imagery. Mind-guided body scanning involves effortlessly observing and attending to body sensations through which we can observe our own physiological processes. Body scanning can be combined with imagery to be in a nonjudgmental state that supports self-healing and improves physiological functioning.
Mind-Guided Body Scans for Awareness and Healing–Youtube Interview of Erik Peper, PhD by Larry Berkelhammer, PhD
Posted: December 23, 2013 Filed under: Uncategorized | Tags: biofeedback, body scan, body sensations, healing, Imagery, meditation, mind-body, passive attention, visualization 1 CommentIn this interview psychophysiology expert Dr. Erik Peper explains the ways how a body scan can facilitate awareness and healing. The discussion describes how the mind-guided body scan can be used to improve immune function and hold passive attention (mindfulness) to become centered. It explores the process of passive attentive process that is part of Autogenic Training and self-healing mental imagery. Mind-guided body scanning involves effortlessly observing and attending to body sensations through which we can observe our own physiological processes. Body scanning can be combined with imagery to be in a nonjudgmental state that supports self-healing and improves physiological functioning.