Quick Rescue Techniques When Stressed
Posted: February 4, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, education, emotions, Evolutionary perspective, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, posture, relaxation, stress management, Uncategorized | Tags: alarm reaction, anxiety, box breathing, Breathing, conditioning, defense reaction, health, huming, Parasympathetic response, rumination, safety, sniff inhale, somatic practices, stress, sympathetic arousal, tactical breathing, Toning, yoga 2 CommentsErik Peper, PhD, Yuval Oded, PhD, and Richard Harvey, PhD
Adapted from Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1).

“If a problem is fixable, if a situation is such that you can do something about it, then there is no need to worry. If it’s not fixable, then there is no help in worrying. There is no benefit in worrying whatsoever.” ― Dalai Lama XIV
To implement the Dalai Lama’s quote is challenging. When caught up in an argument, being angry, extremely frustrated, or totally stressed, it is easy to ruminate, worry. It is much more challenging to remember to stay calm. When remembering the message of the Dalai Lama’s quote, it may be possible to shift perspective about the situation although a mindful attitude may not stop ruminating thoughts. The body typically continues to reacti to the torrents of thoughts that may occur when rehashing rage over injustices, fear over physical or psychological threats, or profound grief and sadness over the loss of a family member. Some people become even more agitated and less rational as illustrated in the following examples.
I had an argument with my ex and I am still pissed off. Each time I think of him or anticipate seeing them, my whole body tightened. I cannot stomach seeing him and I already see the anger in his face and voice. My thoughts kept rehashing the conflict and I am getting more and more upset.
A car cut right in front of me to squeeze into my lane. I had to slam on my brakes. What an idiot! My heart rate was racing and I wanted to punch the driver.
When threatened, we respond quickly in our thoughts and body with a defense reaction that may negatively affect those around us as well as ourselves. What can we do to interrupt negative stress reactions?
Background
Many approaches exist that allow us to become calmer and less reactive. General categories include techniques of cognitive reappraisal (seeing the situation from the other person’s point of view and labeling your own feelings and emotions) and stress management techniques. Practices that are beneficial include mindfulness meditation, benign humor (versus gallows humor), listening to music, taking a time out while implementing a variety of self-soothing practices, or incorporating slow breathing (e.g., heart rate variability and/or box breathing) throughout the day.
No technique fits all as we respond differently to our stressful life circumstances. For example, some people during stress react with a “tend and befriend stress response” (Cohen & Lansing, 2021; Taylor et al., 2000). This response appears to be mostly mediated by the hormone oxytocin acting in ways that sooth or calm the nervous system as an analgesic. These neurophysiological mechanisms of the soothing with the calming analgesic effects of oxytocin have been characterized in detail by Xin, et al. (2017).
The most common response is a fight/flight/freeze stress response that is mediated by excitatory hormones such as adrenalin and inhibitory neurotransmitters such as gamma amino butyric acid (GABA). There is a long history of fight/flight/freeze stress response research, which is beyond the scope of this blog with major theories and terms such as interior milleau (Bernard, 1872); homeostasis and fight/flight (Cannon, 1929); general adaptation syndrome (Selye, 1951); polyvagal theory (Porges, 1995); and, allostatic load (McEwen, 1998). A simplified way to start a discussion about stress reactions begins with the fight/flight stress response. When stressed our defense reactions are triggered. Our sympathetic nervous system becomes activated our mind and body stereotypically responds as illustrated in Figure 1.
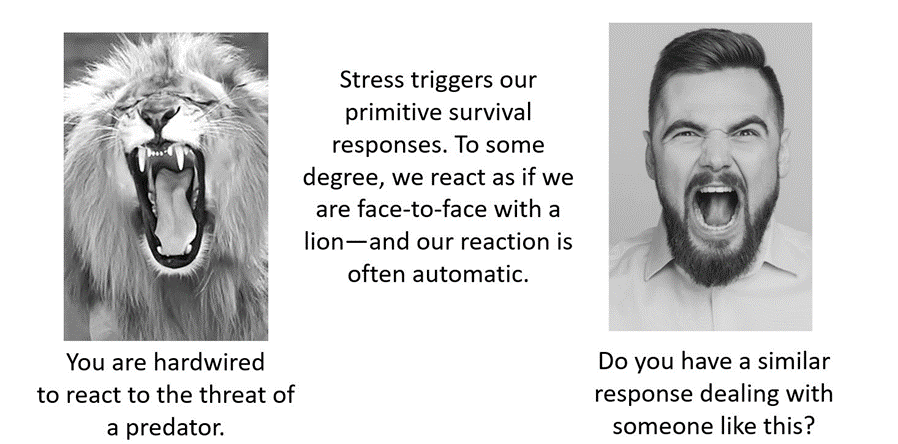
Figure 1. An intense confrontation tends to evoke a stress response (reproduced from Peper et al., 2020).
The flight/fight response triggers a cascade of stress hormones or neurotransmitters (e.g., hypothalamus-pituitary-adrenal cascade) and produces body changes such as the heart pounding, quicker breathing, an increase in muscle tension and sweating. Our body mobilizes itself to protect itself from danger. Our focus is on immediate survival and not what will occur in the future (Porges, 2021; Sapolsky, 2004). It is as if we are facing an angry lion—a life-threatening situation—and we feel threatened and unsafe.
Rather than sitting still, a quick effective strategy is to interrupt this fight/flight response process by completing the alarm reaction such as by moving our muscles (e.g., simulating a fight or flight behavior) before continuing with slower breathing or other self-soothing strategies. Many people have experienced their body tension is reduced and they feel calmer when they do vigorous exercise after being upset, frustrated or angry. Similarly, athletes often have reported that they experience reduced frequency and/or intensity of negative thoughts after an exhausting workout (Thayer, 2003; Liao et al., 2015; Basso & Suzuki, 2017).
Becoming aware of the escalating cascades of physical, behavioral and psychological responses to a stressor is the first step in interrupting the escalating process. After becoming aware, reduce the body’s arousal and change the though patterns using any of the techniques described in this blog. The self-regulation skills presented in this blog are ideally over-learned and automated so that these skills can be rapidly implemented to shift from being stressed to being calm. Examples of skills that can shift from sympathetic neervous system overarousal to parasympathetic nervous system calm include techniques of autogenic traing (Schulz & Luthe, 1959), the quieting reflex developed by Charles Stroebel in 1985 or more recently rescue breathing developed by Richard Gevirtz (Stroebel, 1985; Gevirtz, 2014; Peper, Gibney & Holt, 2002; Peper & Gibney, 2003).
Concepts underlying the rescue techniques
- Psychophysiological principle: “Every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, conscious or unconscious, and conversely, every change in the mental-emotional state, conscious or unconscious, is accompanied by an appropriate change in the physiological state” (Green et al. 1970, p. 3).
- Posture evokes memories and feelings associated with the position. When the body posture is erect and tall while looking slightly up. It is easier to evoke empowering, positive thoughts and feelings. When looking down it is easier to evoke hopeless, helpless and powerless thoughts and feelings (Peper et al., 2017).
- Healing occurs more easily when relaxed and feeling safe. Feeling safe and nurtured enhances the parasympathetic state and reduces the sympathetic state. Use memory recall to evoke those experiences when you felt safe (Peper, 2021).
- Interrupting thoughts is easier with somatic movement than by redirecting attention and thinking of something else without somatic movement.
- Focus on what you want to do not want to do. Attempting to stop thinking or ruminating about something tends to keeps it present (e.g., do not think of pink elephants. What color is the elephant? When you answer, “not pink,” you are still thinking pink). A general concept is to direct your attention (or have others guide you) to something else (Hilt & Pollak, 2012; Oded, 2018; Seo, 2023).
- Skill mastery takes practice and role rehearsal (Lally et al., 2010; Peper & Wilson, 2021).
- Use classical conditioning concepts to facilitate shifting states. Practice the skills and associate them with an aroma, memory, sounds or touch cues. Then when you the situation occurs, use these classical conditioned cues to facilitate the regeneration response (Peper & Wilson, 2021).
Rescue techniques
Coping When Highly Stressed and Agitated
- Complete the alarm/defense reaction with physical activity (Be careful when you do these physical exercises if you have back, hip, knee, or ankle problems).
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Check whether the situation is actually a threat. If yes, then do anything to get out of immediate danger (yell, scream, fight, run away, or dial 911).
- If there is no actual physical threat, then leave the situation and perform vigorous physical activity to complete your alarm reaction, such as going for a run or walking quickly up and down stairs. As you do the exercise, push yourself so that the muscles in your thighs are aching, which focusses your attention on the sensations in your thighs. In our experience, an intensive run for 20 minutes quiets the brain while it often takes 40 minutes when walking somewhat quickly.
- After recovering from the exhaustive exercise, explore new options to resolve the conflict.
- Complete the alarm/defense reaction and evoke calmness with the S.O.S™ technique (Oded, 2023)
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Squat against a wall (similar to the wall-sit many skiers practice). While tensing your arms and fists as shown in Figure 2, gaze upward because it is more difficult to engage in negative thinking while looking upwards. If you continue to ruminate, then scan the room for object of a certain color or feature to shift visual attention and be totally present on the visual object.
- Do this set of movements for 7 to 10 seconds or until you start shaking. Than stand up and relax hands and legs. While standing, bounce up and down loosely for 10 to 15 seconds as you become aware of the vibratory sensations in your arms and shoulders, as shown in Figure 3.

Figure 2.Defense position wall-sit to tighten muscles in the protective defense posture (Oded, 2023). Figure 3. Bouncing up and down to loosen muscles ((Oded, 2023).
- Acknowledge you have reacted and have chosen to interrupt your automatic response. Swing your arms back and forth for 20 seconds. Allow the arms to swing freely as illustrated in Figure 4.

Figure 4. Swinging the arms to loosen the body and spine (Oded, 2023).
- Rest and ground. Lie on the floor and put your calves and feet on a chair seat so that the psoas muscle can relax, as illustrated in Figure 5. Allow yourself to be totally supported by the floor and chair. Be sure there is a small pillow under your head and put your hand on your abdomen so that you can focus on abdominal breathing.

Figure 5. Lying down to allow the psoas muscle to relax and feel grounded (Oded, 2023).
- While lying down, imagine a safe place or memory and make it as real as possible. It is often helpful to listen to a guided imagery or music. The experience can be enhanced if cues are present that are associated with the safe place, such as pictures, sounds, or smells. Continue to breathe effortlessly at about six breaths per minute. If your attention wanders, bring it back to the memory or to the breathing. Allow yourself to rest for 10 minutes.
In most cases, thoughts stop and the body’s parasympathetic activity becomes dominant as the person feels safe and calm. Usually, the hands warm and the blood volume pulse amplitude increases as an indicator of feeling safe, as shown in Figure 6.

Figure 6. Blood volume pulse increases as the person is relaxing, feels safe and calm.
Coping When You Can’t Get Away (adapted from Peper, Harvey & Faass, 2020)
In many cases, it is difficult or embarrassing to remove yourself from the situation when you are stressed out such as at work, in a business meeting or social gathering.
- Become aware that you have reacted.
- Excuse yourself for a moment and go to a private space, such as a restroom. Going to the bathroom is one of the only acceptable social behaviors to leave a meeting for a short time.
- In the bathroom stall, do the 5-minute Nyingma exercise, which was taught by Tarthang Tulku Rinpoche in the tradition of Tibetan Buddhism, as a strategy for thought stopping (see Figure 7). Stand on your toes with your heels touching each other. Lift your heels off the floor while bending your knees. Place your hands at your sides and look upward. Breathe slowly and deeply (e.g., belly breathing at six breaths a minute) and imagine the air circulating through your legs and arms. Do this slow breathing and visualization next to a wall so you can steady yourself if necessary to keep balance. Stay in this position for 5 minutes or longer. Do not straighten your legs—keep squatting despite the discomfort. In a very short time, your attention is captured by the burning sensation in your thighs. Continue. After 5 minutes, stop and shake your arms and legs.
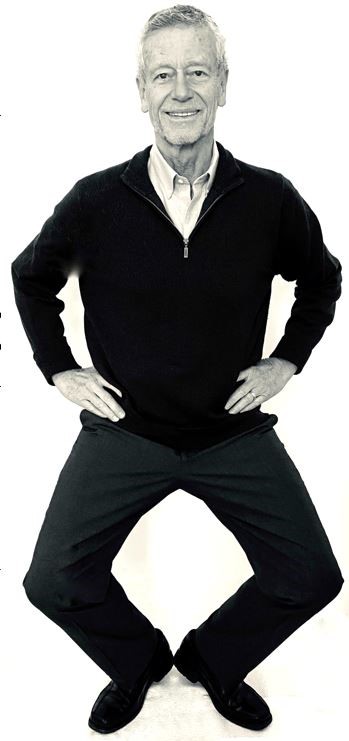
Figure 7. Stressor squat Nyingma exercise (reproduced from Peper et al., 2020).
- Follow this practice with slow abdominal breathing to enhance the parasympathetic response. Be sure that the abdomen expands as the inhalation occurs. Breathe in and out through the nose at about six breaths per minute.
- Once you feel centered and peaceful, return to the room.
- After this exercise, your racing thoughts most likely will have stopped and you will be able to continue your day with greater calm.
What to do When Ruminating, Agitated, Anxious or Depressed
(adapted from Peper, Harvey, & Hamiel, 2019).
- Shift your position by sitting or standing erect in a power position with the back of the head reaching upward to the ceiling while slightly gazing upward. Then sniff quickly through nose, hold and again sniff quickly then very slowly exhale. Be sure as you exhale your abdomen constricts. Then sniff again as your abdomen gets bigger, hold, and sniff one more time letting the abdomen get even bigger. Then, very slow, exhale through the nose to the internal count of six (adapted from Balban et al., 2023). When you sniff or gasp, your racing thoughts will stop (Peper et al., 2016).
- Continue with box breathing (sometimes described as tactical breathing or battle breathing) by exhaling slowly through your nose for 4 seconds, holding your breath for 4 seconds, inhaling slowly for 4 seconds through your nose, holding your breath for 4 seconds and then repeating this cycle of breathing for a few minutes (Röttger et al., 2021; Balban et al., 2023). Focusing your attention on performing the box breathing makes it almost impossible to think of anything else. After a few minutes, follow this with slow effortless diaphragmatic breathing at about six breaths per minute. While exhaling slowly through your nose, look up and when you inhale imagine the air coming from above you. Then as you exhale, imagine and feel the air flowing down and through your arms and legs and out the hands and feet.
- While gazing upward, elicit a positive memory or a time when you felt safe, powerful, strong and/or grounded. Make the positive memory as real as possible.
- Implement cognitive strategies such as reframing the issue, sending goodwill to the person, seeing the problem from the other person’s point of view, and ask is this problem worth dying over (Peper, Harvey, & Hamiel, 2019).
What to Do When Thoughts Keep Interrupting
Practice humming or toning. When you are humming or toning, your focus is on making the sound and the thoughts tend to stop. Generally, breathing will slow down to about six breaths per minute (Peper, Pollack et al., 2019). Explore the following:
- Box breathing (Röttger et al., 2021; Balban et al., 2023)
- Humming also known as bee breath (Bhramari Pranayama) (Abishek et al., 2019; Yoga, 2023) – Allow the tongue to rest against the upper palate, sit tall and erect so that the back of the head is reaching upward to the ceiling, and inhale through your nose as the abdomen expands. Then begin humming while the air flows out through your nose, feel the vibration in the nose, face and throat. Let humming last for about 7 seconds and then allow the air to blow in through the nose and then hum again. Continue for about 5 minutes.
- Toning – Inhale through your nose and then vocalize a single sound such as Om. As you vocalize the lower sound, feel the vibration in your throat, chest and even going down to the abdomen. Let each toning exhalation last for about 6 to 7 seconds and then inhale through your nose. Continue for about 5 minutes (Peper, al., 2019).
Many people report that after practice these skills, they become aware that they are reacting and are able to reduce their automatic reaction. As a result, they experience a significant decrease in their stress levels, fewer symptoms such as neck and holder tension and high blood pressure, and they feel an increase in tranquility and the ability to communicate effectively.
Practicing these skills does not resolve the conflicts; they allow you to stop reacting automatically. This process allows you a time out and may give you the ability to be calmer, which allows you to think more clearly. When calmer, problem solving is usually more successful. As phrased in a popular meme, “You cannot see your reflection in boiling water. Similarly, you cannot see the truth in a state of anger. When the waters calm, clarity comes” (author unknown).

Boiling water (photo modified from: https://www.facebook.com/photo/?fbid=388991500314839&set=a.377199901493999)
Below are additional resources that describe the practices. Please share these resources with friends, family and co-workers.
Stressor squat instructions
Toning instructions
Diaphragmatic breathing instructions
Reduce stress with posture and breathing
Conditioning
References
Abishek, K., Bakshi, S. S., & Bhavanani, A. B. (2019). The efficacy of yogic breathing exercise bhramari pranayama in relieving symptoms of chronic rhinosinusitis. International Journal of Yoga, 12(2), 120–123. https://doi.org/10.4103/ijoy.IJOY_32_18
Balban, M. Y., Neri, E., Kogon, M. M., Weed, L., Nouriani, B., Jo, B., Holl, G., Zeitzer, J. M., Spiegel, D., Huberman, A. D. (2023). Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Reports Medicine, 4(1), 10089. https://doi.org/10.1016/j.xcrm.2022.100895
Basso, J. C. & Suzuki, W. A. (2017). The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plast, 2(2), 127–152. https://doi.org/10.3233/BPL-160040
Bernard, C. (1872). De la physiologie générale. Paris: Hachette livre. https://www.amazon.ca/PHYSIOLOGIE-GENERALE-BERNARD-C/dp/2012178596
Cannon, W. B. (1929). Organization for Physiological Homeostasis. Physiological Reviews, 9, 399–431. https://doi.org/10.1152/physrev.1929.9.3.399
Cohen, L. & Lansing, A. H. (2021). The tend and befriend theory of stress: Understanding the biological, evolutionary, and psychosocial aspects of the female stress response. In: Hazlett-Stevens, H. (eds), Biopsychosocial Factors of Stress, and Mindfulness for Stress Reduction. pp. 67–81, Springer, Cham. https://doi.org/10.1007/978-3-030-81245-4_3
Gevirtz, R. (2014). HRV Training and its Importance – Richard Gevirtz, Ph.D., Pioneer in HRV Research & Training. Thought Technology. Accessed December 29, 2023. https://www.youtube.com/watch?v=9nwFUKuJSE0
Green, E. E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological. Journal of Transpersonal Psychology, 2, 1–26. https://atpweb.org/jtparchive/trps-02-70-01-001.pdf
Hilt, L. M., & Pollak, S. D. (2012). Getting out of rumination: comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165.
https://doi.org/10.1007/s10802-012-9638-3
Lally, P., VanJaarsveld, C. H., Potts, H. W., & Wardle, J. (2010). How habits are formed: Modelling habit formation the real world. European Journal of Social Psychology, 40, 998–1009. https://doi.org/10.1002/ejsp.674
Liao, Y., Shonkoff, E. T., & Dunton, G. F. (2015). The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology. 6, 1975. https://doi.org/10.3389/fpsyg.2015.01975
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44.
https://doi.org/10.1111/j.1749-6632.1998.tb09546.x
Oded, Y. (2018). Integrating mindfulness and biofeedback in the treatment of posttraumatic stress disorder. Biofeedback, 46(2), 37-47. https://doi.org/10.5298/1081-5937-46.02.03
Oded, Y. (2023). Personal communication. S.O.S 1™ technique is part of the Sense Of Safety™ method. www.senseofsafety.co
Peper, E. (2021). Relive memory to create healing imagery. Somatics, XVIII(4), 32–35.https://www.researchgate.net/publication/369114535_Relive_memory_to_create_healing_imagery
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., & Gibney, K.H. (2003). A teaching strategy for successful hand warming. Somatics. XIV(1), 26–30. https://www.researchgate.net/publication/376954376_A_teaching_strategy_for_successful_hand_warming
Peper, E., Harvey, R., & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153–160. https://doi.org/10.15540/nr.6.3.153
Peper, E., Lee, S., Harvey, R., & Lin, I-M. (2016). Breathing and math performance: Implication for performance and neurotherapy. NeuroRegulation, 3(4), 142–149. http://dx.doi.org/10.15540/nr.3.4.142
Peper, E., Lin, I-M, Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128–133. https://www.neuroregulation.org/article/view/19345/13263
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 9(2), 46–49. https://doi.org/10.5298/1081-5937-49-2-04
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology, 32(4), 301–318. https://doi.org/10.1111/j.1469-8986.1995.tb01213.x
Porges, S.W. (2021) Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry, 20(2),296-298. Porges SW. Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry. 2021 Jun;20(2):296-298. https://doi.org10.1002/wps.20871
Röttger, S., Theobald, D. A., Abendroth, J., & Jacobsen, T. (2021). The effectiveness of combat tactical breathing as compared with prolonged exhalation. Applied Psychophysiology and Biofeedback, 46, 19–28. https://doi.org/10.1007/s10484-020-09485-w
Sapolsky, R. (2004). Why zebras don’t get ulcers (3rd ed.). New York:Holt. https://www.amazon.com/Why-Zebras-Dont-Ulcers-Third/dp/0805073698/
Schultz, J. H., & Luthe, W. (1959). Autogenic training: A psychophysiologic approach to psychotherapy. Grune & Stratton. https://www.google.com/books/edition/Autogenic_Training/y8SwQgAACAAJ?hl=en
Selye, H. (1951). The general-adaptation-syndrome. Annual Review of Medicine, 2(1), 327–342. https://doi.org/10.1146/annurev.me.02.020151.001551
Seo, H. (2023). How to stop ruminating. The New York Times. Accessed January 3, 2024. https://www.nytimes.com/2023/02/01/well/mind/stop-rumination-worry.html
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-quieting-reflex-Charles-Stroebel/dp/0425085066
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A. R., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. https://doi.org/10.1037/0033-295X.107.3.411
Thayer, R. E. (2003). Calm energy: How people regulate mood with food and exercise. Oxford University Press. https://www.amazon.com/Calm-Energy-People-Regulate-Exercise/dp/0195163397
Xin, Q., Bai, B., & Liu, W. (2017). The analgesic effects of oxytocin in the peripheral and central nervous system. Neurochemistry International, 103, 57–64. https://doi.org/10.1016/j.neuint.2016.12.021
Yoga, N. (2023). This simple breath practice is scientifically proven to calm your mind. The nomadic yogi. Accessed December 31, 2023. https://www.leahsugerman.com/blog/bhramari-pranayama-humming-bee-breath#
Is mindfulness training old wine in new bottles?
Posted: January 11, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, healing, health, meditation, self-healing, stress management | Tags: anxiety, autogenic training, biofeedback, health, meditation, mental-health, mindfulness, pain, passive attention, progressive muscle relaxation, wellness, yoga Leave a commentAdapted from: Peper, E., Harvey, R., & Lin, I-M. (2019). Mindfulness training has themes common to other technique. Biofeedback. 47(3), 50-57. https://doi.org/10.5298/1081-5937-47.3.02
This extensive blog discusses the benefits of mindfulness-based meditation (MM) techniques and explores how similar beneficial outcomes occur with other mind-centered practices such as transcendental meditation, and body-centered practices such as progressive muscle relaxation (PMR), autogenic training (AT), and yoga. For example, many standardized mind-body techniques such as mindfulness-based stress reduction and mindfulness-based cognitive therapy (a) are associated with a reduction in symptoms of symptoms such as anxiety, pain and depression. This article explores the efficacy of mindfulness based techniques to that of other self-regulation techniques and identifies components shared between mindfulness based techniques and several previous self-regulation techniques, including PMR, AT, and transcendental meditation. The authors conclude that most of the commonly used self-regulation strategies have comparable efficacy and share many elements.
Mindfulness-based strategies are based in ancient Buddhist practices and have found acceptance as one of the major contemporary behavioral medicine techniques (Hilton et al, 2016; Khazan, 2013). Throughout this blog the term mindfulness will refer broadly to a mental state of paying total attention to the present moment, with a non-judgmental awareness of the inner and/ or outer experiences (Baer et al., 2004; Kabat-Zinn, 1994).
In 1979, Jon Kabat-Zinn introduced a manual for a standardized Mindfulness-Based Stress Reduction (MBSR) program at the University of Massachusetts Medical Center (Kabat-Zinn, 1994, 2003). The eight-week program combined mindfulness as a form of insight meditation with specific types of yoga breathing and movements exercises designed to focus on awareness of the mind and body, as well as thoughts, feelings, and behaviors.
There is a substantial body of evidence that mindfulness-based cognitive therapy (MBCT); Teasdale et al., 1995) and mindfulness-based stress reduction (MBSR) (Kabat-Zinn, 1994, 2003) have combined with skills of cognitive therapy for ameliorating stress symptoms such as negative thinking, anxiety and depression. For example, MBSR and MBCT has been confirmed to be clinical beneficial in alleviating a variety of mental and physical conditions, for people dealing with anxiety, depression, cancer-related pain and anxiety, pain disorder, or high blood pressure (The following are only a few of the hundred studies published: Andersen et al., 2013; Carlson et al., 2003; Fjorback et al., 2011; Greeson, & Eisenlohr-Moul, 2014; Hoffman et al., 2012; Marchand, 2012; Baer, 2015; Demarzo et al., 2015; Khoury et al, 2013; Khoury et al, 2015; Chapin et al., 2014; Witek Janusek et al., 2019). Currently, MBSR and MBCT techniques that are more standardized are widely applied in schools, hospitals, companies, prisons, and other environments.
The Relationship Between Mindfulness and Other Self-Regulation Techniques
This section addresses two questions: First, how do mindfulness-based interventions compare in efficacy to older self-regulation techniques? Second, and perhaps more basically, how new and different are mindfulness-based therapies from other self-regulation-oriented practices and therapies?
Is mindfulness more effective than other mind/body body/mind approaches?
Although mindfulness-based meditation (MM) techniques are effective, it does not mean that is is more effective than other traditional meditation or self-regulation approaches. To be able to conclude that MM is superior, it needs to be compared to equivalent well-coached control groups where the participants were taught other approaches such as progressive relaxation, autogenic training, transcendental meditation, or biofeedback training. In these control groups, the participants would be taught by practitioners who were self-experienced and had mastered the skills and not merely received training from a short audio or video clip (Cherkin et al, 2016). The most recent assessment by the National Centere for Complementary and Integrative Health, National Institutes of Health (NCCIH-NIH, 2024) concluded that generally “the effects of mindfulness meditation approaches were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise especially when they include how to generalize the skills during the day” (NCCIH, 2024). Generalizing the learned skills into daily life contributes to the successful outcome of Autogenic Training, Progressive Relaxation, integrated biofeedback stress management training, or the Quieting Response (Luthe, 1979; Davis et al., 2019; Wilson et al., 2023; Stroebel, 1982).
Unfortunately, there are few studies that compare the effective of mindfulness meditation to other sitting mental techniques such as Autogenic Training, Transcendental Meditation or similar meditative practices that are used therapeutically. When the few randomized control studies of MBSR versus autogenic training (AT) was done, no conclusions could be drawn as to the superior stress reduction technique among German medical students (Kuhlmann et al., 2016).
Interestingly, Tanner, et al (2009) in a waitlist study of students in Washington, D.C. area universities practicing TM used the concept of mindfulness, as measured by the Kentucky Inventory of Mindfulness Skills (KIM) (Baer et al, 2004) as a dependent variable, where TM practice resulted in greater degrees of ‘mindfulness.’ More direct comparisons of MM with body-focused techniques, such as progressive relaxation, or Autogenic training mindfulness-based approaches, have not found superior benefit. For example, Agee et al (2009) compared the stress management effects of a five-week Mindfulness Meditation (MM) to a five-week Progressive Muscle Relaxation (PMR) course and found no meaningful reports of superiority of one over the other program; both MM and PMR were effective in reducing symptoms of stress.
In a persuasive meta-analysis comparing MBSR with other similar stress management techniques used among military service members, Crawford, et al (2013) described various multimodal programs for addressing post-traumatic stress disorder (PTSD) and other military or combat-related stress reactions. Of note, Crawford, et al (2013) suggest that all of the multi-modal approaches that include Autogenic Training, Progressive Muscle Relaxation, movement practices including Yoga and Tai Chi, as well as Mindfulness Meditation, and various types of imagery, visualization and prayer-based contemplative practices ALL provide some benefit to service members experiencing PTSD.
An important observation by Crawford et al (2013) pointed out that when military service members had more physical symptoms of stress, the meditative techniques appeared to work best, and when the chief complaints were about cognitive ruminations, the body techniques such as Yoga or Tai Chi worked best to reduce symptoms. Whereas it may not be possible to say that mindfulness meditation practices are clearly superior to other mind-body techniques, it may be possible to raise questions about mechanisms that unite the mind-body approaches used in therapeutic settings.
Could there be negative side effects?
Another point to consider is the limited discussion of the possible absence of benefit or even harms that may be associated with mind-body therapies. For example, for some people, meditation does not promote prosocial behavior (Kreplin et al, 2018). For other people, meditation can evoke negative physical and/or psychological outcomes (Lindahl et al, 2017; Britton et al., 2021). There are other struggles with mind-body techniques when people only find benefit in the presence of a skilled clinician, practitioner, or guru, suggesting a type of psychological dependency or transference, rather than the ability to generalize the benefits outside of a set of conditions (e.g. four to eight weeks of one to four hour trainings) or a particular setting (e.g. in a natural and/or quiet space).
Whereas the detailed instructions for many mindfulness meditation trainings, along with many other types of mind-body practices (e.g. Transcendental Meditation, Autogenic Training, Progressive Muscle Relaxation, Yoga, Tai Chi…) create conditions that are laudable because they are standardized, a question is raised as to ‘critical ingredients’, using the metaphor of baking. The difference between a chocolate and a vanilla cake is not ingredients such as flour, or sugar, etc., which are common to all cakes, but rather the essential or critical ingredient of the chocolate or vanilla flavoring. So what are the essential or critical ingredients in mind-body techniques? Extending the metaphor, Crawford, et al (2013, p. 20) might say the critical ingredient common to the mind-body techniques they studied was that people “can change the way their body and mind react to stress by changing their thoughts, emotions, and behaviors…” with techniques that, relatively speaking, “involve minimal cost and training time.”
The skeptical view suggested here is that MM techniques share similar strategies with other mind-body approaches that encouraging learners to ‘pay attention and shift intention.’ This strategy is part of the instructions when learning Progressive Relaxation, Autogenic Training, Transcendental Meditation, movement meditation of Yoga and Tai Chi and, with instrumented self-regulation techniques such as bio/neurofeedback. In this sense, MM training repackages techniques that have been available for millennia and thus becomes ‘old wine sold in new bottles.’
We wonder if a control group for compassionate mindfulness training would report more benefits if they were asked not only to meditate on compassionate acts, but actually performed compassionate tasks such as taking care of person in pain, helping a homeless person, or actually writing and delivering a letter of gratitude to a person who has helped them in the past? The suggestion is to titrate the effects of MM techniques, moving from a more basic level of benefit to a more fully actualized level of benefit, generalizing their skill beyond a training setting, as measured by the Baer et al (2004) Kentucky Inventory of Mindfulness Skills.
Each generation of clinicians and educators rediscover principles without always recognizing that the similar principles were part of the previous clinical interventions. The analogies and language has changed; however, the underlying concepts may be the same. Mindfulness interventions are now the new, current and popular approach. Some of the underlying ‘mindfulness’ concepts that are shared in common with successfully other mind-body and self-regulation approaches include:
The practitioner must be self-experienced in mindfulness practice. This means that the practitioners do not merely believe the practice is effective; they know it is effective from self-experience. Inner confidence conveyed to clients and patients enhances the healing/placebo effect. It is similar to having sympathy or empathy for clients and patients that occurs from have similar life experiences, such as when a clinician speaks to a patient. For example, a male physician speaking to a female patient who has had a mastectomy may be compassionate; however, empathy occurs more easily when another mastectomy patient (who may also be a physician) shares how she struggled overcame her doubts and can still be loved by her partner.
There may also be a continuum of strengthening beliefs about the benefits of mindfulness techniques that leads to increase benefits for the approach. Knowing there are some kinds of benefits from initiating a practice of mindfulness increases empathy/compassion for others as they learn. Proving that mindfulness techniques are causing benefits after systematically comparing their effectiveness with other approaches strengthens the belief in the mindfulness approaches. Note that a similar process of strengthening one’s belief in an approach occurs gradually, over time as clients and patients progress through beginner, intermediate and advanced levels of mind-body practices.
Observing thoughts without being captured. Being a witness to the thoughts, emotions, and external events results in a type of covert global desensitization and skill mastery of NOT being captured by those thoughts and emotions. This same process of non-attachment and being a witness is one of the underpinnings of techniques that tacitly and sometime covertly support learning ways of controlling attention, such as with Autogenic Training; namely how to passively attend to a specific body part without judgment and, report on the subjective experience without comparison or judgment.
Ongoing daily practice. Participants take an active role in their own healing process as they learn to control and focus their attention. Participants are often asked to practice up to one hour a day and apply the practices during the day as mini-practices or awareness cues to interrupt the dysfunctional behavior. For example in Autogenic training, trainees are taught to practice partial formula (such my “neck and shoulders are heavy”) during the day to bring the body/mind back to balance. While with Progressive Relaxation, the trainee learns to identify when they tighten inappropriate muscles (dysponesis) and then inhibit this observed tension.
Peer support by being in a group. Peer support is a major factor for success as people can share their challenges and successes. Peer support tends to promote acceptance of self-and others and provides role modeling how to cope with stressors. It is possible that some peer support groups may counter the benefits of a mind-body technique, especially when the peers do not provide support or may in fact impede progress when they complain of the obstacles or difficulties in their process.
These concepts are not unique to Mindfulness Meditation (MM) training. Similar instructions have been part of the successful/educational intervention of Progressive Relaxation, Autogenic Training, Yogic practices, and Transcendental Meditation. These approaches have been most successful when the originators, and their initial students, taught their new and evolving techniques to clients and patients; however, they became less successful as later followers and practitioners used these approaches without learning an in-depth skill mastery. For example, Progressive relaxation as taught by Edmund Jacobson consisted of advanced skill mastery by developing subtle awareness of different muscle tension that was taught over 100 sessions (Mackereth & Tomlinson, 2010). It was not simply listening once to a 20-minute audio recording about tightening and relaxing muscles. Similarly, Autogenic training is very specific and teaches passive attention over a three to six-month time-period while the participant practices multiple times daily. Stating the obvious, learning Autogenic Training, Mindfulness, Progressive Relaxation, Bio/Neurofeedback or any other mind-body technique is much more than listening to a 20-minute audio recording.
The same instructions are also part of many movement practices. For many participants focusing on the movement automatically evoked a shift in attention. Their attention is with the task and they are instructed to be present in the movement.
Areas to explore.
Although Mindfulness training with clients and patients has resulted in remarkable beneficial outcomes for the participants, it is not clear whether mindfulness training is better than well taught PR, AT, TM or other mind/body or body/mind approaches. There are also numerous question to explore such as: 1) Who drops out, 2) Is physical exercise to counter sitting disease and complete the alarm reaction more beneficial, and 3) Strategies to cope with wandering attention.
- Who drops out?
We wonder if mindfulness is appropriate for all participants as sometimes participants drop out or experience negative abreactions. It not clear who those participants are. Interestingly, hints for whom the techniques may be challenging can be found in the observations of Autogenic Training that lists specific guidelines for contra-, relative- and non-indications (Luthe, 1970).
- Physical movement to counter sitting disease and complete the alarm reaction.
Although many mindfulness meditation practices may include yoga practices, most participants practice it in a sitting position. It may be possible that for some people somatic movement practices such as a slow Zen walk may quiet the inner dialogue more quickly. In our experience, when participants are upset and highly stressed, it is much easier to let go of agitation by first completing the triggered fight/flight response with vigorous physical activity such as rapidly walking up and downs stairs while focusing on the burning sensations of the thigh muscles. Once the physical stress reaction has been completed and the person feels physically calmer then the mind is quieter. Then have the person begin their meditative practice.
- Strategies to cope with wandering attention.
Some participants have difficulty staying on task, become sleepy, worry, and/or are preoccupied. We observed that first beginning with physical movement practices or Progressive Relaxation appears to be a helpful strategy to reduce wandering thoughts. If one has many active thoughts, progressive relaxation continuously pulls your attention to your body as you are directed to tighten and let go of muscle groups. Being guided supports developing the passive focus of attention to bring awareness back to the task at hand. Once internally quieter, it is easier hold their attention while doing Autogenic Training, breathing or Mindfullness Meditation.
By integrating somatic components with the mindfulness such as done in Progressive Relaxation or yoga practices facilitates the person staying present. Similarly, when teaching slower breathing, if a person has a weight on their abdomen while practicing breathing, it is easier to keep attending to the task: allow the weight to upward when inhaling and feeling the exhalation flowing out through the arms and legs.
Therapeutic and education strategies that implicitly incorporate mindfulness
Progressive relaxation
In the United States during the 1920 progressive relaxation (PR) was developed and taught by Edmund Jacobson (1938). This approach was clinically very successful for numerous illnesses ranging from hypertension, back pain, gastrointestinal discomfort, and anxiety; it included 50 year follow-ups. Patients were active participants and practiced the skills at home and at work and interrupt their dysfunctional patterns during the day such as becoming aware of unnecessary muscle tension (dyponetic activity) and then release the unnecessary muscle tension (Whatmore & Kohli, 1968). This structured approach is totally different than providing an audio recording that guides clients and patients through a series of tightening and relaxing of their muscles. The clinical outcome of PR when taught using the original specific procedures described by Jacobson (1938) was remarkable. The incorporation of Progressive Relaxation as the homework practice was an important cofactor in the successful outcome in the treatment of muscle tension headache using electromyography (EMG) biofeedback by Budzynski, Stoyva and Adler (1970).
Autogenic Training
In 1932 Johannes Schultz in Germany published a book about Autogenic Training describing the basic training procedure. The basic autogenic procedure, the standard exercises, were taught over a minimum period of three month in which the person practiced daily. In this practice they directed theri passive attention to the following cascading sequence: heaviness of their arms, warmth of their arms, heart beat calm and regular, breathing calm and regular or it breathes me, solar plexus is warm, forehead is cool, and I am at peace (Luthe, 1979). Three main principles of autonomic training mentioned by Luthe (1979) are: (1) mental repetition of topographically oriented verbal formulae for brief periods; (2) passive concentration; and (3) reduction of exteroceptive and proprioceptive afferent stimulation. The underlying concepts of Autogenic Therapy include as described by Peper and Williams (1980):
The body has an innate capacity for self-healing and it is this capacity that is allowed to become operative in the autogenic state. Neither the trainer nor trainee has the wisdom necessary to direct the course of the self-balancing process; hence, the capacity is allowed to occur and not be directed.
- Homeostatic self-regulation is encouraged.
- Much of the learning is done by the trainee at home; hence, the responsibility for the training lies primarily with the trainee.
- The trainer/teacher must be self-experience in the practice.
- The attitude necessary for successful practice is one of passive attention; active striving and concern with results impedes the learning process. An attitude of acceptance is cultivated, letting be whatever comes up. This quality of attention is known as “mindfulness’ in meditative traditions.
The clinical outcome for autogenic therapy is very promising. The detailed guided self-awareness training and uncontrolled studies showed benefits across a wide variety of psychosomatic illness such as asthma, cancer, hypertension, anxiety, pain irritable bowel disease, depression (Luthe & Schultz, 1970a; Luthe & Schultz, 1970b). Autogenic training components have also been integrated in biofeedback training. Elmer and Alice Green included the incorporation of autogenic training phrases with temperature biofeedback for the very successful treatment of migraines (Green & Green, 1989). Autonomic training combine with biofeedback in clinical practices produced better results than control group for headache population (Luthe, 1979). Empirical research found that autonomic training was applied efficiently in emotional and behavioral problems, and physical disorder (Klott, 2013), such as skin disorder (Klein & Peper, 2013), insomnia (Bowden et al., 2012), Meniere’s disease (Goto, Nakai, & Ogawa, 2011) and the multitude of stress related symptoms (Wilson et al., 2023).
Bio/neurofeedback training
Starting in the late 1960s, biofeedback procedures have been developed as a successful treatment approach for numerous illnesses ranging from headaches, hypertension, to ADHD (Peper et al., 1979; Peper & Shaffer, 2010; Khazan, 2013). In most cases, the similar instructions that are part of mindfulness meditation are also embedded in the bio/neurofeedback instructions. The participants are instructed to learn control over some physiological parameter and then practice the same skill during daily life. This means that during the learning process, the person learn passive attention and is not be captured by marauding thoughts and feeling. and during the day develop awareness Whenever they become aware of dysfunctional patterns, thoughts, emotions, they initiated their newly learned skill. The ongoing biological feedback signals continuously reminds them to focus.
Transcendental meditation
The next fad to hit the American shore was Transcendental Meditation (TM)– a meditation practice from the ancient Vedic tradition in India. The participant were given a mantra that they mentally repeated and if their attention wanders, they go back to repeating the mantra internally. The first study that captured the media’s attention was by Wallace (1970) published in the Journal Science which reported that “During meditation, oxygen consumption and heart rate decreased, skin resistance increased, and the electroencephalogram showed specific changes in certain frequencies. These results seem to distinguish the state produced by Transcendental Meditation from commonly encountered states of consciousness and suggest that it may have practical applications.” (Wallace, 1970).
The participants were to practice the mantra meditation twice a day for about 20 minutes. Meta-analysis studies have reported that those who practiced TM as compared to the control group experienced significant improved of numerous disorders such as CVD risk factors, anxiety, metabolic syndrome, drug abuse and hypertension (Paul-Labrador et al, 2006; Rainforth et al., 2007; Hawkins, 2003).
To make it more acceptable for the western audience, Herbert Benson, MD, adapted and simplified techniques from TM training and then labelled a core element, the ‘relaxation response’ (Benson et al., 1974) Instead of giving people a secret mantra and part of a spiritual tradition, he recommend using the word “one” as the mantra. Numerous studies have demonstrated that when patients practice the relaxation response, many clinical symptoms were reduced. The empirical research found that practiced transcendental meditation caused increasing prefrontal low alpha power (8-10Hz) and theta power of EEG; as well as higher prefrontal alpha coherence than other locations at both hemispheres. Moreover, some individuals also showed lower sympathetic activation and higher parasympathetic activation, increased respiratory sinus arrhythmic and frontal blood flow, and decreased breathing rate (Travis, 2001, 2014). Although TM and Benson’s relaxation response continues to be practiced, mindfulness has taking it place.
Conclusion
Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) are very beneficial and yet may be considered ‘old wine in new bottles’ where the metaphor refers to millennia old meditation techniques as ‘old wine’ and the acronyms such as MBSR or MBCT as ‘new bottles’. Like many other ‘new’ therapeutic approaches or for that matter, many other ‘new’ medications, use it now before it becomes stale and loses part of its placebo power. As long as the application of a new technique is taught with the intensity and dedication of the promotors of the approach, and as long as the participants are required to practice while receiving support, the outcomes will be very beneficial, and most likely similar in effect to other mind-body approaches.
The challenge facing mindfulness practices just as those from Autogenic Training, Progressive Relaxation and Transcendental Meditation, is that familiarity breeds contempt and that clients and therapists are continuously looking for a new technique that promises better outcome. Thus as Mindfulness training is taught to more and more people, it may become less promising. In addition, as mindfulness training is taught in less time, (e.g. fewer minutes and/or fewer sessions), and with less well-trained instructors, who may offer less support and supervision for people experiencing possible negative effects, the overall benefits may decrease. Thus, mindfulness practice, Autogenic training, progressive relaxation, Transcendental Meditation, movement practices, meditation, breathing practices as well as the many spiritual practices all appear to share common fate of fading over time. Whereas the core principles of mind-body techniques are ageless, the execution is not always assured.
References
Agee, J. D., Danoff-Burg, S., & Grant, C. A. (2009). Comparing brief stress management courses in a community sample: Mindfulness skills and progressive muscle relaxation. Explore: The Journal of Science and Healing, 5(2), 104-109. https://doi.org/10.1016/j.explore.2008.12.004
Andersen, S. R., Würtzen, H., Steding-Jessen, M., Christensen, J., Andersen, K. K., Flyger, H., … & Dalton, S. O. (2013). Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients. Acta Oncologica, 52(2), 336-344. https://doi.org/10.3109/0284186X.2012.745948
Alvarez-Jimenez, M., Gleeson, J. F., Bendall, S., Penn, D. L., Yung, A. R., Ryan, R. M., … Nelson, B. (2018). Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy. Schizophrenia Research, 202, 369-377 https://doi.org/10.1016/j.schres.2018.07.022
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. https://doi.org/10.1093/clipsy/bpg015
Baer, R. A.. (2015). Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. New York: Elsevier. https://www.elsevier.com/books/mindfulness-based-treatment-approaches/baer/978-0-12-416031-6
Baer, R., Smith, G., & Allen, K. (2004). Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment, 11, 191–206. https://doi.org/10.1177/1073191104268029
Benson, H., Beary, J. F., & Carol, M. P. (1974).The Relaxation Response. Psychiatry, 37(1), 37-46. https://www.tandfonline.com/loi/upsy20
Bowden, A., Lorenc, A., & Robinson, N. (2012). Autogenic Training as a behavioural approach to insomnia: A prospective cohort study. Primary Health Care Research & Development, 13, 175-185. https://doi.org/10.1017/S1463423611000181
Britton, W.B., Lindahl, J.R., Coope, D.J., Canby, N.K., & Palitsky, R. (2021). Defining and Measuring Meditation-Related Adverse Effects in Mindfulness-Based Programs. Clinical Psychological Science, 9(6), 1185-1204. https://doi.org/10.1177/2167702621996340
Budzynski, T., Stoyva, J., & Adler, C. (1970). Feedback-induced muscle relaxation: Application to tension headache. Journal of Behavior Therapy and Experimental Psychiatry, 1(3), 205-211. https://doi.org/10.1016/0005-7916(70)90004-2
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2003). Mindfulness‐based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine, 65(4), 571-581. https://doi.org/10.1097/01.psy.0000074003.35911.41
Chapin, H. L., Darnall, B. D., Seppala, E. M., Doty, J. R., Hah, J. M., & Mackey, S. C. (2014). Pilot study of a compassion meditation intervention in chronic pain. J Compassionate Health Care, 1(4), 1-12. https://doi.org/10.1186/s40639-014-0004-x
Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., … & Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA, 315(12), 1240-1249. https://doi.org/10.1001/jama.2016.2323
Crawford, C., Wallerstedt, D. B., Khorsan, R., Clausen, S. S., Jonas, W. B., & Walter, J. A. (2013). A systematic review of biopsychosocial training programs for the self-management of emotional stress: Potential applications for the military. Evidence-Based Complementary and Alternative Medicine, 747694: 1-23. https://doi.org/10.1155/2013/747694
Davis, M., Eshelman, E.R., & McKay, M. (2019). The Relaxation and Stress Reduction Workbook. Oakland, CA: New Harbinger Publications. https://www.amazon.com/Relaxation-Reduction-Workbook-Harbinger-Self-Help/dp/1684033349
Demarzo, M. M., Montero-Marin, J., Cuijpers, P., Zabaleta-del-Olmo, E., Mahtani, K. R., Vellinga, A., Vincens, C., Lopez del Hoyo, Y., & García-Campayo, J. (2015). The efficacy of mindfulness-based interventions in primary care: A meta-analytic review. The Annals of Family Medicine, 13(6), 573-582. https://doi.org/10.1370/afm.1863
Fjorback, L. O., Arendt, M., Ørnbøl, E., Fink, P., & Walach, H. (2011). Mindfulness‐Based Stress Reduction and Mindfulness‐Based Cognitive Therapy–A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica, 124(2), 102-119. https://doi.org/10.1111/j.1600-0447.2011.01704.x
Goto, F., Nakai, K., & Ogawa, K. (2011). Application of autogenic training in patients with Meniere disease. European Archives of Oto-Rhino-Laryngology, 268(10), 1431-1435. https://doi.org/10.1007/s00405-011-1530-1
Greeson, J., & Eisenlohr-Moul, T. (2014). Mindfulness-based stress reduction for chronic pain. In R. A. Baer (Ed.), Mindfulness-Based Treatment Approaches: Clinician’s Guide to Evidence Base and Applications, 269-292. San Diego, CA: Academic Press. https://psycnet.apa.org/record/2014-40932-000
Green, E. and Green, A. (1989). Beyond Biofeedback. New York: Knoll. https://www.amazon.com/Beyond-Biofeedback-Elmer-Green/dp/0940267144
Hawkins, M. A. (2003). Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery. Journal of Offender Rehabilitation, 36(1-4), 47- 65. https://doi.org/10.1300/J076v36n01_03
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., …Maglione, M. A. (2016). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199-213. https://doi.org/10.1007/s12160-016-9844-2
Hoffman, C. J., Ersser, S. J., Hopkinson, J. B., Nicholls, P. G., Harrington, J. E., & Thomas, P. W. (2012). Effectiveness of mindfulness-based stress reduction in mood, breast-and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology, 30(12), 1335-1342. https://doi.org/10.1200/JCO.2010.34.0331
Jacobson, E. (1938). Progressive relaxation. Chicago, IL: University of Chicago Press. https://www.amazon.com/Progressive-Relaxation-Physiological-Investigation-Significance/dp/0226390594
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion. https://www.amazon.com/Wherever-You-There-Are-Mindfulness/dp/0306832011
Kabat-Zinn, J. (2003). Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences, 8, 73–107. https://psycnet.apa.org/record/2004-19791-008
Khazan, I. Z. (2013). The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. New York: John Wiley & Sons. https://www.amazon.com/Clinical-Handbook-Biofeedback-Step-Step/dp/1119993717
Klein, A., & Peper, E. (2013). There Is hope: Autogenic biofeedback training for the treatment of psoriasis. Biofeedback, 41 (4), 194-201. https://doi.org/10.5298/1081-5937-41.4.01
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763-771. https://doi.org/10.1016/j.cpr.2013.05.005
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519-528.
Klott, O. (2013). Autogenic Training–a self-help technique for children with emotional and behavioural problems. Therapeutic Communities: The International Journal of Therapeutic Communities, 34(4), 152-158. https://doi.org/10.1108/TC-09-2013-0027
Kreplin, U., Farias, M., & Brazil, I. A. (2018). The limited prosocial effects of meditation: A systematic review and meta-analysis. Sci Rep, 8, 2403. https://doi.org/10.1038/s41598-018-20299-z
Kuhlmann, S. M., Huss, M., Bürger, A., & Hammerle, F. (2016). Coping with stress in medical students: results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Medical Education, 16(1), 316. https://doi.org/10.1186/s12909-016-0833-8
Lindahl, J. R., Fisher, N. E., Cooper, D. J., Rosen, R. K, & Britton, W. B. (2017). The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoSONE, 12(5): e0176239. https://doi.org/10.1371/journal.pone.0176239
Luthe, W. (1970). Autogenic therapy: Research and theory. New York: Grune and Stratton. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/abs/autogenic-therapy-edited-by-wolfgang-luthe-volume-4-research-and-theory-by-wolfgang-luthe-grune-and-stratton-new-york-1970-pp-276-price-1475/6C8521C36C37254A08AAD1F2FE08211C
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970a). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
Luthe, W. & Schultz, J. H. (1970b). Autogenic therapy: Applications in psychotherapy. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-Applications-Psychotherapy-v/dp/0808902725
Mackereth, P.A. & Tomlinson, L. (2010). Progressive muscle relaxation. In Cawthorn, A. & Mackereth, P.A. eds. Integrative Hypnotherapy. London: Churchill Livingstone. https://www.amazon.com/Integrative-Hypnotherapy-Complementary-approaches-clinical/dp/0702030821
Marchand, W. R. (2012). Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice, 18(4), 233-252. https://doi.org/10.1097/01.pra.0000416014.53215.86
NCCIH (2024). Meditation and Mindfulness: What You Need To Know. National Center for Complementary and Integrative Health, National Institutes of Health. Accessed January 31, 2024. https://www.nccih.nih.gov/health/meditation-and-mindfulness-what-you-need-to-know?
Paul-Labrador, M., Polk, D., Dwyer, J.H. et al. (2006). Effects of a randomized controlled trial of Transcendental Meditation on components of the metabolic syndrome in subjects with coronary heart disease. Archive of Internal Medicine, 166(11), 1218-1224. https://doi.org/10.1001/archinte.166.11.1218
Peper, E., Ancoli, S. & Quinn, M. (Eds). (1979). Mind/Body Integration: Essential Readings in Biofeedback. New York: Plenum. https://www.amazon.com/Mind-Body-Integration-Essential-Biofeedback/dp/0306401029
Peper, E. & Shaffer, F. (2010). Biofeedback History: An Alternative View. Biofeedback, 38 (4): 142–147. https://doi.org/10.5298/1081-5937-38.4.03
Peper, E., & Williams, E.A. (1980). Autogenic therapy. In A. C. Hastings, J. Fadiman, & J. S. Gordon (Eds.), Health for the whole person (pp137-141).. Boulder: Westview Press. https://biofeedbackhealth.files.wordpress.com/2016/02/autogenic-therapy-peper-and-williams.pdf
Rainforth, M.V., Schneider, R.H., Nidich, S.I., Gaylord-King, C., Salerno, J.W., & Anderson, J.W. (2007). Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Current Hypertension Reports, 9(6), 520–528. https://doi.org/10.1007/s11906-007-0094-3
Stroebel, C. (1982). QR: The Quieting Reflex. New York: Putnam Pub Group. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570
Tanner, M. A., Travis, F., Gaylord‐King, C., Haaga, D. A. F., Grosswald, S., & Schneider, R. H. (2009). The effects of the transcendental meditation program on mindfulness. Journal of Clinical Psychology 65(6), 574-589. https://doi.org/10.1002/jclp.20544
Teasdale, J. D., Segal, Z., & Williams, J. M. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy, 33, 25–39. https://doi.org/10.1016/0005-7967(94)e0011-7
Travis, F. (2001). Autonomic and EEG patterns distinguish transcending from other experiences during transcendental meditation practice. International Journal of Psychophysiology, 42, 1–9. https://doi.org/10.1016/s0167-8760(01)00143-x
Travis, F. (2014). Transcendental experiences during meditation practice. Annals of the New York Academy of Sciences, 1307, 1–8. https://doi.og10.1111/nyas.12316
Wallace, K.W. (1970). Physiological Effects of Transcendental Meditation. Science, 167 (3926), 1751-1754. https://doi.org/10.1126/science.167.3926.1751
Whatmore, G. B., & Kohli, D. R. (1968). Dysponesis: A neurophysiologic factor in functional disorders. Behavioral Science, 13(2), 102–124. https://doi.org/10.1002/bs.3830130203
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
Witek Janusek, L., Tel,l D., & Mathews, H.L. (2019). Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: A randomized trial with active control. Brain Behav Immun, 80:358-373. https://doi.org/10.1016/j.bbi.2019.04.012
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythm
Posted: July 4, 2023 Filed under: ADHD, behavior, computer, digital devices, education, emotions, Evolutionary perspective, health, laptops, screen fatigue, Uncategorized | Tags: anxiety, autism, bonding, circadian rhythms, depression, nature, still face experiment 3 Comments
Adapted from: Peper, E. Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation,10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Over the past two decades, there has been a significant increase in the prevalence of autism, Attention-Deficit/hyperactivity disorder (ADHD), anxiety, depression, and pediatric suicidal behavior. Autism rates have risen from 1 in 150 children in 2000 to 1 in 36 children in 2020 (CDC, 2023), while ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18-25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020), and depression rates for U.S. teens ages 12-17 have increased from 8% in 2007 to 13% in 2017 (Geiger & Davis, 2019; Walrave et al., 2022). Pediatric suicide attempts have also increased by 163% from 2009 to 2019 (Arakelyan et al., 2023), and during the COVID-19 pandemic, these rates have increased by more than 25% (WHO, 2022; Santomauro et al., 2021). In addition, the prevalence of these disorders has tripled for US adults during the pandemic compared to before (Ettman et al., 2020).
The rapid increase of these disorders is not solely due to improved diagnostic methods, genetic factors or the COVID-19 pandemic. The pandemic amplified pre-existing increasing trends. More likely, individuals who were at risk had their disorders triggered or amplified by harmful environmental and behavioral factors. Conceptually, Genetics loads the gun; epigenetics, behavior, and environment pull the trigger.
While behavioral strategies such as neurofeedback, Cognitive Behavior Therapy, biofeedback, meditation techniques, and pharmaceuticals can treat or ameliorate these disorders, the focus needs to be on risk reduction. In some ways, treatment can be likened to closing the barn doors after the horses have bolted.
Evolutionary perspective to reduce risk factors
Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto), provides an evolutionary perspective and offers simple rules of health by reducing risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, sugar, digital media).
- We do not need evidence of harm to claim that a drug or an unnatural procedure is dangerous. If evidence of harm does not exist, it does not mean harm does not exist.
- Only resort to medical techniques when the health payoff is very large (to save a life), exceeds its potential harm, such as incontrovertibly needed surgery or life-saving medicine (penicillin).
- Avoid the iatrogenics and negative side effects of prescribed medication.
Writer and scholar Taleb’s suggestions are reminiscent of the perspective described by the educator Joseph C. Pearce (1993) in his book, Evolution’s End. Pearce argued that modern lifestyles have negatively affected the secure attachment and bonding between caregivers and infants. The lack of nurturing and responsive caregiving in early childhood may lead to long-term emotional and psychological problems. He points out that we have radically adapted behaviors that differ from those that evolved over thousands of generations and that allowed us to thrive and survive. In the last 100 years, babies have often been separated from their mothers at birth or early infancy by being put in a nursery or separate room, limited or no breastfeeding with the use of formula, exposure to television for entertainment, lack of exploratory play outdoors, and the absence of constant caretakers in high-stress and unsafe environments.
As Pearce pointed out, “If you want true learning, learning that involves the higher frontal lobes – the intellectual, creative brain – then again, the emotional environment must be positive and supportive. This is because at the first sign of anxiety the brain shifts its functions from the high, prefrontal lobes to the old defenses of the reptilian brain… These young people need audio-vocal communication, nurturing, play, body movement, eye contact, sweet sounds and close heart contact on a physical level” (Mercogliano & Debus, 1999).
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past. The proposed recommendations are based upon Talib’s perspective that anything that was not part of our evolutionary past is probably harmful; thus, it is wise to remove the unnatural/unfamiliar and adopt the precautionary principle, which states that if evidence of harm does not exist, it does not mean harm does not exist (Kriebel et al., 2010).
This article is the first of a three-part series. Part 1 focuses on increasing reciprocal communication between infant and caretaker, reducing screen time, and re-establishing circadian rhythms; Part 2 focuses on reducing exposure to neurotoxins, eliminating processed foods, and supporting the human biome; and Part 3 focuses on respiration and movement.
Part 1- Increase bonding, reduce screen time, and re-establish circadian rhythms
Increase bonding between infant and caretaker
Infants develop emotional communication through reciprocal interactions with their caregivers, during which the caregiver responds to the infant’s expressions. When this does not occur, it can be highly stressful and detrimental to the infant’s development. Unfortunately, more and more babies are emotionally and socially isolated while their caregivers are focussed on, and captured by, the content on their digital screens. Moreover, infants and toddlers are entertained (babysat) by cellphones and tablets instead of dynamically interacting with their caretakers. Screens do not respond to the child’s expressions; the screen content is programmed to capture the infant’s attention through rapid scene changes. Without reciprocal interaction, babies often become stressed, as shown by the research of developmental psychologist Professor Edward Tronick, who conducted the “Still Face” experiment (Tronick & Beeghly, 2011; Weinberg et al, 2008).
The “Still Face” experiment illustrated what happens when caregivers are not responding to infants’ communication. The caregivers were asked to remain still and unresponsive to their babies, resulting in the infants becoming increasingly distressed and disengaged from their surroundings. Not only does this apply to infants but also to children, teenagers and older individuals. Watch the short Still Face experiment, which illustrates what happens when the caretaker is not responding to the infant’s communication.
Recommendation. Do not use cellphone and digital media while being with an infant in the first two years of life. It is important for caregivers to limit their cellphone use and prioritize reciprocal interactions with their infants for healthy emotional and psychological development.
Reduce screen time (television, social media, streaming videos, gaming)[1]
From an evolutionary perspective, screen time is an entirely novel experience. Television, computers, and cellphones are modern technologies that have significantly impacted infants’ and young people’s development. To grow, infants, toddlers, and children require opportunities to explore the environment through movement, touch, and play with others, which is not possible with screens. Research has shown that excessive screen time can negatively affect children’s motor development, attention span, socialization skills, and contribute to obesity and other health problems (Hinkley et al., 2014; Carson et al., 2016; Mark, 2023).
When four-year-olds watch fast-paced videos, they exhibit reduced executive functions and impulse control, which may be a precursor for ADHD, compared to children who engage in activities such as drawing (Lillard & Peterson, 2011; Mark, 2023).
Furthermore, excessive screen time and time spent on social media are causal in increasing depression in young adults-–as was discovered when Facebook became available at selected universities. Researchers compared the mental health of students at similar universities where Facebook was or was not available and observed how the students’ mental health changed when Facebook became available (Braghieri et al., 2022). Their research showed that “College-wide access to Facebook led to an increase in severe depression by 7% and anxiety disorders by 20%. In total, the negative effect of Facebook on mental health appeared to be roughly 20% the magnitude of what is experienced by those who lose their job” (Walsh, 2022).
Exposure to digital media has also significantly reduced our attention span from 150 seconds in 2004 to an average of 44 seconds in 2021. The shortening of attention span may contribute to the rise of ADHD and anxiety (Mark, 2022, p. 96).
Recommendations: Reduce time spent on social media, gaming, mindlessly following one link after the other, or watching episode after episode of streaming videos. Instead, set time limits for screen use, turn off notifications, and prioritize in-person interactions with friends, family and colleagues while engaging in collaborative activities. Encourage children to participate in physical and social activities and to explore nature.
To achieve this, follow the guidelines from the American Academy of Pediatrics’ recommendation on screen time (Council on Communications and Media, 2016), which suggest these limits on screen time for children of different age groups:
- Children under 18 months of age should avoid all screen time, except for video chatting with family and friends.
- Children aged 18-24 months should have limited screen time, and only when watched together with a caretaker.
- Children aged 2 to 5 years should have no more than one hour of screen time per day with parental supervision.
- For adolescents, screen and social media time should be limited to no more than an hour a day.
In our experience, when college students reduce their time spent on social media, streaming videos, and texting, they report that it is challenging; however, they then report an increase in well-being and performance over time (Peper et al., 2021). It may require more effort to provide children with actual experiential learning and entertainment than allowing them to use screens, but it is worthwhile. Having children perform activities and play outdoors–in a green nature environment–appears to reduce ADHD symptoms (Louv, 2008; Kuo & Taylor, 2004).
Reestablish circadian (daily) rhythms
Our natural biological and activity rhythms were regulated by natural light until the 19th century. It is hard to imagine not having light at night to read, to work on the computer, or to answer email. However, light not only illuminates, but also affects our physiology by regulating our biological rhythms. Exposure to light at night can interfere with the production of melatonin, which is essential for sleep. Insufficient sleep affects 30% of toddlers, preschoolers, and school-age children, as well as the majority of adolescents. The more media is consumed at bedtime, the more bedtime is delayed and total sleep time is reduced (Hale et al., 2018). Reduced sleep is a contributing factor to increased ADHD symptoms of inattention, hyperactivity and impulsivity (Cassoff et al., 2012).
Recommendations: Support the circadian rhythms. Avoid screen time one hour before bedtime. This will reduce exposure to blue light and reduce sympathetic arousal triggered by the content on the screen or reactions to social media and emails. Sleep in total darkness, and establish a regular bedtime and waking time to avoid “social jetlag,” which can negatively affect health and performance (Caliandro et al., 2021). Implement sleep hygiene strategies such as developing a bedtime ritual to improve sleep quality (Stager et al., 2023; Suni, 2023). Thus, go to bed and wake up at the same time each day, including weekends. Avoid large meals, caffeine, and alcohol before bedtime. Consistency is key to success.
Conclusion
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past, and explore strategies that support behaviors that have allowed the human being to thrive and survive. Improve clinical outcomes and optimize health by enhancing reciprocal communication interactions, reducing screen time and re-establishing the circadian rhythm.
References
Arakelyan, M., Freyleue, S., Avula, D., McLaren, J.L., O’Malley, A.J., & Leyenaar, J.K. (2023). Pediatric Mental Health Hospitalizations at Acute Care Hospitals in the US, 2009-2019. JAMA, 329(12), 1000–1011. https://doi.org/10.1001/jama.2023.1992
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Caliandro, R., Streng, A.A., van Kerkhof, L.W.M., van der Horst, G.T.J., & Chaves, I. (2021). Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients, 13(12), 4543. https://doi.org/10.3390/nu13124543
Carson, V., Tremblay, M.S., Chaput, J.P., & Chastin, S.F. (2016). Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab, 41(6 Suppl 3), S294-302. https://doi.org/10.1139/apnm-2016-0026
Cassoff, J., Wiebe, S.T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nat Sci Sleep, 4, 73-80. https://doi.org/10.2147/NSS.S31269
CDC. (2022). Attention-Deficit/hyperactivity disorder (ADHD): ADHD through the years. Centers for Disease Control and Prevention. Assessed March 27, 2023. https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. (2023). Data & Statistics on Autism Spectrum Disorder. CDC Centers for Disease Control and Prevention. Assessed March 25, 2023. https://www.cdc.gov/ncbddd/autism/data.html
Council on Communications and Media. (2016). Media and young minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M.,& Galea, S. (2020), Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Geiger, A.W. & Davis, L. (2019). A growing number of American teenagers-particularly girls-are facing depression. Pew Research Center. Accessed March 28, 2023.
Goodwin, R.D., Weinberger, A.H., Kim, J.H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. J Psychiatr Res. 130, 441-446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hale, L., Kirschen, G/W., LeBourgeois, M.K., Gradisar, M., Garrison, M.M., Montgomery-Downs, H., Kirschen, H., McHale, S.M., Chang, A.M., & Buxton, O.M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc Psychiatr Clin N Am, 27(2),229-245. https://doi.org/10.1016/j.chc.2017.11.014
Hinkley, T., Verbestel, V., Ahrens, W., Lissner, L., Molnár, D., Moreno, L.A., Pigeot, I., Pohlabeln, H., Reisch, L.A., Russo, P., Veidebaum, T., Tornaritis, M., Williams, G., De Henauw, S., De Bourdeaudhuij, I; IDEFICS Consortium. (2014). Early childhood electronic media use as a predictor of poorer well-being: a prospective cohort study. JAMA Pediatr,. May;168(5):485-92. https://doi.org/10.1001/jamapediatrics.2014.94
Kriebel, D., Tickner, J., Epstein, P., Lemons, J., Levins, R., Loechler, E.L., Quinn, M., Rudel, R., Schettler, T., Stoto, M. (2001). The precautionary principle in environmental science. Environ Health Perspect, 109(9):871-6. https://doi.org/10.1289/ehp.01109871
Kuo. F.E. & Taylor, A.F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 94(9),1580-6. https://doi.org/10.2105/ajph.94.9.1580
Lillard, A.S. & Peterson, J. The immediate impact of different types of television on young children’s executive function. Pediatrics, 128(4), 644-9. https://doi.org/10.1542/peds.2010-1919
Louv, R. (2008). Last Child in the Woods: Saving Our Children from Nature-Deficit Disorder. Algonquin Books. Chapel Hill, NC: Algonquin Books
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press.
Mercogliano, C. & Debus, K. (1999). Nurturing Heart-Brain Development Starting With Infants 1999 Interview with Joseph Chilton Pearce. Journal of Family Life, 5(1). https://www.michaelmount.co.za/nurturing-heart-brain-development-starting-with-infants-1999-interview-with-joseph-chilton-pearce/
Pearce, J.C. (1993). Evolutions’s End. New York: HarperOne.
Peper, E., Wilson, V., Martin, M., Rosegard, E., & Harvey, R. (2021). Avoid Zoom fatigue, be present and learn. NeuroRegulation, 8(1), 47–56. https://doi.org/10.15540/nr.8.1.47
Santomauro, D.F., Mantilla Herrera, A.M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D.M., Abbafati, C., Adolph, C., …. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(103121700-1712., https://doi.org/10.1016/S0140-6736(21)02143-7
Stager, L.M., Caldwell, A., Bates, C., & Laroche, H. (2023). Helping kids get the sleep they need. Society of Behavioral Medicine. Accessed March 29, 2023 https://www.sbm.org/healthy-living/helping-kids-get-the-sleep-they-need?gclid=Cj0KCQjww4-hBhCtARIsAC9gR3ZM7v9VSvqaFkLnceBOH1jIP8idiBIyQcqquk5y_RZaNdUjAR9Wpx4aAhTBEALw_wcB
Suni, E. (2023). Sleep hygiene- What it is, why it matters, and how to revamp your habits to get better nightly sleep. Sleep Foundation. Accessed March 29, 2023. https://www.sleepfoundation.org/sleep-hygiene
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto) Random House Publishing Group. (Kindle Locations 5906-5908).
Tronick, E. & Beeghly, M. (2011).Infants’ meaning-making and the development of mental health problems. Am Psychol, 66(2),107-19. https://doi.org/10.1037/a0021631
Walrave, R., Beerten, S.G., Mamouris, P. et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 23, 163 (2022). https://doi.org/10.1186/s12875-022-01769-w
Walsh, D. (2022 September 14). Study: Social media use linked to decline in mental health. MIT Management Ideas Made to Matter. Accessed March 28, 2023. https://mitsloan.mit.edu/ideas-made-to-matter/study-social-media-use-linked-to-decline-mental-health#:~:text=College%2Dwide%20access%20to%20Facebook,with%20either%20psychotherapy%20or%20antidepressants
Weinberg, M.K., Beeghly, M., Olson, K.L., & Tronick, E. (2008). A Still-face Paradigm for Young Children: 2½ Year-olds’ Reactions to Maternal Unavailability during the Still-face. J Dev Process, 3(1):4-22. https://pubmed.ncbi.nlm.nih.gov/22384309/
WHO (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. Assessed march 26, 2023. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
[1] The critique of social media does not imply that there are no benefits. If used judiciously, it is a powerful tool to connect with family and friends or access information.
Breathing: Informative YouTube videos and blogs
Posted: March 20, 2023 Filed under: behavior, Breathing/respiration, health, mindfulness, Pain/discomfort, relaxation, self-healing | Tags: anxiety, box breathing, carbon dioxide, exhaling, hickups 3 Comments
Breathing is a voluntary and involuntary process and affects our body, emotions, mind and performance. The focus of breathing is to bring oxygen into the body and eliminate carbon dioxide. This is the basic physiological process that underlies the concepts described in the videos; however, it does not included the concept as breathing as a pump to optimize abdominal venous and lymph circulation. The pumping action may reduce abdominal discomfort such as irritable bowel disease, acid reflux and pelvic floor discomfort. Effortless whole body breathing also supports pelvic floor muscle tone balance and spinal column dynamics. Effortless diaphragmatic breathing can only occur if the abdomen is able to expand and constrict in 360 degrees and not constricted by tight clothing around the waist (designer’s jean syndrome), self-image (holding the abdomen in to look slimmer), or learned disuse of abdominal movement (breathing shallowly and in the chest to avoid movement at the incisionsafter abdominal surgery).
The outstanding videos discuss the psychophysiology, mechanics, chemistry of respiration as well as useful practices practices to enhance health..
- How to Breathe Correctly for Optimal Health, Mood, Learning & Performance | Huberman Lab Podcast (Skip the advertisements embedded in this video)
- Dr. Jack Feldman: Breathing for Mental & Physical Health & Performance | Huberman Lab Podcast #54 (Skip the advertisements embedded in this video)
The videos provide additional approaches to improve breathing and health
- 5 Ways to Improve your Breathing with James Nestor
- Patrick McKeown-Why we breathe: How to improve your sleep, concentration, focus & performance
The blogs that explores how diaphragmatic breathing may reduce symptoms of irritable bowel syndrome, acid reflux, and pelvic floor pain.
- Healing irritable bowel syndrome with diaphragmatic breathing
- Breathing to reduce acid reflux and dysmenorrhea
- Enjoy sex: Breath away the pain
- Resolving pelvic floor pain-a casae report
Below are the descriptions of the youtube videos.
How to Breathe Correctly for Optimal Health, Mood, Learning & Performance | Huberman Lab Podcast
In this episode, I explain the biology of breathing (respiration), how it delivers oxygen and carbon dioxide to the cells and tissues of the body and how is best to breathe—nose versus mouth, fast versus slow, deliberately versus reflexively, etc., depending on your health and performance needs. I discuss the positive benefits of breathing properly for mood, to reduce psychological and physiological stress, to halt sleep apnea, and improve facial aesthetics and immune system function. I also compare what is known about the effects and effectiveness of different breathing techniques, including physiological sighs, box breathing and cyclic hyperventilation, “Wim Hof Method,” Prānāyāma yogic breathing and more. I also describe how to breath to optimize learning, memory and reaction time and I explain breathing at high altitudes, why “overbreathing” is bad, and how to breathe specifically to relieve cramps and hiccups. Breathwork practices are zero-cost and require minimal time yet provide a unique and powerful avenue to improve overall quality of life that is grounded in clear physiology. Anyone interesting in improving their mental and physical health or performance in any endeavor ought to benefit from the information and tools in this episode.
Dr. Jack Feldman: Breathing for Mental & Physical Health & Performance | Huberman Lab Podcast #54
This episode my guest is Dr. Jack Feldman, Distinguished Professor of Neurobiology at University of California, Los Angeles and a pioneering world expert in the science of respiration (breathing). We discuss how and why humans breathe the way we do, the function of the diaphragm and how it serves to increase oxygenation of the brain and body. We discuss how breathing influences mental state, fear, memory, reaction time, and more. And we discuss specific breathing protocols such as box-breathing, cyclic hyperventilation (similar to Wim Hof breathing), nasal versus mouth breathing, unilateral breathing, and how these each effect the brain and body. We discuss physiological sighs, peptides expressed by specific neurons controlling breathing, and magnesium compounds that can improve cognitive ability and how they work. This conversation serves as a sort of “Master Class” on the science of breathing and breathing related tools for health and performance.
5 Ways To Improve Your Breathing with James Nestor
James Nestor believes we’re all breathing wrong. Here he breaks down 5 ways to transform your breathing, from increasing your lung capacity to stopping breathing through your mouth. There is nothing more essential to our health and wellbeing than breathing: take air in, let it out, repeat 25,000 times a day. Yet, as a species, humans have lost the ability to breathe correctly, with grave consequences. In Breath, journalist James Nestor travels the world to discover the hidden science behind ancient breathing practices to figure out what went wrong and how to fix it. Modern research is showing us that making even slight adjustments to the way we inhale and exhale can: – jump-start athletic performance – rejuvenate internal organs – halt snoring, allergies, asthma and autoimmune disease, and even straighten scoliotic spines None of this should be possible, and yet it is. Drawing on thousands of years of ancient wisdom and cutting-edge studies in pulmonology, psychology, biochemistry and human physiology, Breath turns the conventional wisdom of what we thought we knew about our most basic biological function on its head. You will never breathe the same again.
Patrick McKeown – Why We Breathe: How to Improve Your Sleep, Concentration, Focus & Performance
Watch Oxygen Advantage founder and world-renowned breathing expert Patrick McKeown speak to an influential group of health professionals at the recent Health Optimisation Summit in London. Patrick was presenting his very well-received topic: ‘Why We Breathe: How to Improve Your Sleep, Concentration, Focus & Performance’. The aim of the event was to “unite the health, wellness and science disciplines”, and in doing so, it brought together thousands of industry professionals and members of the public. Patrick would like to take this opportunity to thank the organisers of The Health Optimisation Summit for an excellent event and for giving him the opportunity to speak among such luminaries of the health and wellbeing world and on a subject about which he is very passionate.
Breathing is more than gas exchange
Effortless diaphragmatic breathing is optimized when the abdomen is able to expand and constrict in 360 degrees like and not constricted by tight clothing (designer’s jean syndrome induced by the constriction of the waist), self-image (holding the abdomen in to look slimmer), or learned disuse of abdominal movement (breathing shallowly and in the chest to avoid movement at the incisions site after abdominal surgery).
Hope for insomnia, depression, anxiety, ADHD, exhaustion, and nasal congestion -Breathe light, slow and deep
Posted: July 9, 2022 Filed under: ADHD, behavior, Breathing/respiration, emotions, Exercise/movement, health, Pain/discomfort, relaxation, Uncategorized | Tags: allergies, anxiety, asthma, depression, hyperventilation, insomnia, nasal congestion, nose breathing Leave a commentAnxiety, depression, insomnia, exhaustion, ADHD, allergies, poor performance have all increased (Barendse et al., 2021; London & Landes, 2021; Peper et al, 2022a; Peper et al, 2022b; Vasileiadou et al, 2021). One of the unrecognized contributing factor is dysfunctional mouth breathing (McKeown, 2022). Improve health by learning to breathe in and out through the nose during the day and night. Listen to the inspiring presentation by Patrick McKeown, author of the superb book, The breathing cure-Develop new habits for a healthier, happier & long life (McKeown, 2022). In this presentation, he describes the science behind these disorders, the rationale for breathing light, slow and deep and offers simple breathing exercises to reduce symptoms and improve performance.
References
Barendse, M., Flannery, J., Cavanagh, C., Aristizabal, M., Becker, S. P., Berger, E., … & Pfeifer, J. (2021). Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID-19 pandemic: A collaborative of 12 samples from 3 countries. https://doi.org/10.31234/osf.io/hn7us
London, A.S. & Landes, S.D. (2021). Cohort Change in the Prevalence of ADHD Among U.S. Adults: Evidence of a Gender-Specific Historical Period Effect. Journal of attention disorders, 25(6), 771-782. https://doi.org/10.1177/1087054719855689
McKeown, P. (2022). The breathing cure-Develop new habits for a healthier, happier & long life. West Palm Beach, FL: Humanix Books.
Peper, E. (2022). Reduce anxiety. the peperperspective. https://peperperspective.com/2022/03/23/reduce-anxiety/
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022b). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Vasileiadou, S., Ekerljung, L., Bjerg, A., & Goksor, E. (2021). Asthma increased in young adults from 2008–2016 despite stable allergic rhinitis and reduced smoking. PLoS ONE, 16(6): e0253322. https://doi.org/10.1371/journal.pone.0253322
Reduce anxiety
Posted: March 23, 2022 Filed under: behavior, Breathing/respiration, CBT, cognitive behavior therapy, digital devices, education, emotions, health, mindfulness, posture, relaxation, self-healing, stress management | Tags: anxiety, concentration, insomnia, menstrual cramps, pain Leave a comment
The purpose of this blog is to describe how a university class that incorporated structured self-experience practices reduced self-reported anxiety symptoms (Peper, Harvey, Cuellar, & Membrila, 2022). This approach is different from a clinical treatment approach as it focused on empowerment and mastery learning (Peper, Miceli, & Harvey, 2016).
As a result of my practice, I felt my anxiety and my menstrual cramps decrease. — College senior
When I changed back to slower diaphragmatic breathin, I was more aware of my negative emotions and I was able to reduce the stress and anxiety I was feeling with the deep diaphragmatic breathing.– College junior
Background
More than half of college students now report anxiety (Coakley et al., 2021). In our recent survey during the first day of the spring semester class, 59% of the students reported feeling tired, dreading their day, being distracted, lacking mental clarity and had difficulty concentrating.
Before the COVID pandemic nearly one-third of students had or developed moderate or severe anxiety or depression while being at college (Adams et al., 2021. The pandemic accelerated a trend of increasing anxiety that was already occurring. “The prevalence of major depressive disorder among graduate and professional students is two times higher in 2020 compared to 2019 and the prevalence of generalized anxiety disorder is 1.5 times higher than in 2019” As reported by Chirikov et al (2020) from the UC Berkeley SERU Consortium Reports.
This increase in anxiety has both short and long term performance and health consequences. Severe anxiety reduces cognitive functioning and is a risk factor for early dementia (Bierman et al., 2005; Richmond-Rakerd et al, 2022). It also increases the risk for asthma, arthritis, back/neck problems, chronic headache, diabetes, heart disease, hypertension, pain, obesity and ulcer (Bhattacharya et al., 2014; Kang et al, 2017).
The most commonly used treatment for anxiety are pharmaceutical and cognitive behavior therapy (CBT) (Kaczkurkin & Foa, 2015). The anti-anxiety drugs are usually benzodiazepines (e.g., alprazolam (Xanax), clonazepam (Klonopin), chlordiazepoxide (Librium), diazepam (Valium) and lorazepam (Ativan). Although these drugs they may reduce anxiety, they have numerous side effects such as drowsiness, irritability, dizziness, memory and attention problems, and physical dependence (Shri, 2012; Crane, 2013).
Cognitive behavior therapy techniques based upon the assumption that anxiety is primarily a disorder in thinking which then causes the symptoms and behaviors associated with anxiety. Thus, the primary treatment intervention focuses on changing thoughts.
Given the significant increase in anxiety and the potential long term negative health risks, there is need to provide educational strategies to empower students to prevent and reduce their anxiety. A holistic approach is one that assumes that body and mind are one and that soma/body, emotions and thoughts interchangeably affect the development of anxiety. Initially in our research, Peper, Lin, Harvey & Perez (2017) reported that it was easier to access hopeless, helpless, powerless and defeated memories in a slouched position than an upright position and it was easier to access empowering positive memories in an upright position than a slouched position. Our research on transforming hopeless, helpless, depressive thought to empowering thoughts, Peper, Harvey & Hamiel (2019) found that it was much more effective if the person first shifts to an upright posture, then begins slow diaphragmatic breathing and finally reframes their negative to empowering/positive thoughts. Participants were able to reframe stressful memories much more easily when in an upright posture compared to a slouched posture and reported a significant reduction in negative thoughts, anxiety (they also reported a significant decrease in negative thoughts, anxiety and tension as compared to those attempting to just change their thoughts).
The strategies to reduce anxiety focus on breathing and posture change. At the same time there are many other factors that may contribute the onset or maintenance of anxiety such as social isolation, economic insecurity, etc. In addition, low glucose levels can increase irritability and may lower the threshold of experiencing anxiety or impulsive behavior (Barr, Peper, & Swatzyna, 2019; Brad et al, 2014). This is often labeled as being “hangry” (MacCormack & Lindquist, 2019). Thus, by changing a high glycemic diet to a low glycemic diet may reduce the somatic discomfort (which can be interpreted as anxiety) triggered by low glucose levels. In addition, people are also sitting more and more in front of screens. In this position, they tend to breathe quicker and more shallowly in their chest.
Shallow rapid breathing tends to reduce pCO2 and contributes to subclinical hyperventilation which could be experienced as anxiety (Lum, 1981; Wilhelm et al., 2001; Du Pasquier et al, 2020). Experimentally, the feeling of anxiety can rapidly be evoked by instructing a person to sequentially exhale about 70 % of the inhaled air continuously for 30 seconds. After 30 seconds, most participants reported a significant increase in anxiety (Peper & MacHose, 1993). Thus, the combination of sitting, shallow breathing and increased stress from the pandemic are all cofactors that may contribute to the self-reported increase in anxiety.
To reduce anxiety and discomfort, McGrady and Moss (2013) suggested that self-regulation and stress management approaches be offered as the initial treatment/teaching strategy in health care instead of medication. One of the useful approaches to reduce sympathetic arousal and optimize health is breathing awareness and retraining (Gilbert, 2003).
Stress management as part of a university holistic health class
Every semester since 1976, up to 180 undergraduates have enrolled in a three-unit Holistic Health class on stress management and self-healing (Klein & Peper, 2013). Students in the class are assigned self-healing projects using techniques that focus on awareness of stress, dynamic regeneration, stress reduction imagery for healing, and other behavioral change techniques adapted from the book, Make Health Happen (Peper, Gibney & Holt, 2002).
82% of students self-reported that they were ‘mostly successful’ in achieving their self-healing goals. Students have consistently reported achieving positive benefits such as increasing physical fitness, changing diets, reducing depression, anxiety, and pain, eliminating eczema, and even reducing substance abuse (Peper et al., 2003; Bier et al., 2005; Peper et al., 2014).
This assessment reports how students’ anxiety decreased after five weeks of daily practice. The students filled out an anonymous survey in which they rated the change in their discomfort after practicing effortless diaphragmatic breathing. More than 70% of the students reported a decrease in anxiety. In addition, they reported decreases in symptoms of stress, neck and shoulder pain as shown in Figure 1.

Figure 1. Self-report of decrease in symptoms after practice diaphragmatic breathing for a week.
In comparing the self-reported responses of the students in the holistic health class to those of the control group (N=12), the students in the holistic health class reported a significant decrease in symptoms since the beginning of the semester as compared to the control group as shown in Figure 2.

Figure 2. Change in self-reported symptoms after 6 weeks of practice the integrated holistic health skills as compared to the control group who did not practice these skills.
Changes in symptoms Most students also reported an increase in mental clarity and concentration that improved their study habits. As one student noted: Now that I breathe properly, I have less mental fog and feel less overwhelmed and more relaxed. My shoulders don’t feel tense, and my muscles are not as achy at the end of the day.
The teaching components for the first five weeks included a focus on the psychobiology of stress, the role of posture, and psychophysiology of respiration. The class included didactic presentations and daily self-practice
Lecture content
- Diadactic presentation on the physiology of stress and how posture impacts health.
- Self-observation of stress reactions; energy drain/energy gain and learning dynamic relaxation.
- Short experiential practices so that the student can experience how slouched posture allows easier access to helpless, hopeless, powerless and defeated memories.
- Short experiential breathing practices to show how breathing holding occurs and how 70% exhalation within 30 seconds increases anxiety.
- Didactic presentation on the physiology of breathing and how a constricted waist tends to have the person breathe high in their chest (the cause of neurasthemia) and how the fight/flight response triggers chest breathing, breath holding and/or shallow breathing.
- Explanation and practice of diaphragmatic breathing.
Daily self-practice
Students were assigned weekly daily self-practices which included both skill mastery by practicing for 20 minutes as well and implementing the skill during their daily life. They then recorded their experiences after the practice. At the end of the week, they reviewed their own log of week and summarized their observations (benefits, difficulties) and then met in small groups to discuss their experiences and extract common themes. These daily practices consisted of:
- Awareness of stress. Monitoring how they reacted to daily stressor
- Practicing dynamic relaxation. Students practiced for 20 minutes a modified progressive relaxation exercise and observed and inhibit bracing pattern
- Changing energy drain and energy gains. Students observed what events reduced or increased their subjective energy and implemented changes in their behavior to decrease events that reduced their energy and increased behaviors that increase their enery
- Creating a memory of wholeness practice
- Practicing effortless breathing. Students practiced slowly diaphragmatic abdominal breathing for 20 minutes per day and each time they become aware of dysfunctional breathing (breath holding, shallow chest breathing, gasping) during the day, they would shift to slower diaphragmatic breathing.
Discussion
Almost all students were surprised how beneficial these practices were to reduce their anxiety and symptoms. Generally, the more the students would interrupt their personal stress responses during the day by shifting to diaphragmatic breathing the more did they experience success. We hypothesize that some of the following factors contributed to the students’ improvement.
- Learning through self-mastery as an education approach versus clinical treatment.
- Generalizing the skills into daily life and activities. Practicing the skills during the day in which the cue of a stress reaction triggered the person to breathe slowly. The breathing would reduce the sympathetic activation.
- Interrupting escalating sympathetic arousal. Responding with an intervention reduced the sense of being overwhelmed and unable to cope by the participant by taking charge and performing an active task.
- Redirecting attention and thoughts away from the anxiety triggers to a positive task.
- Increasing heart rate variability. Through slow breathing heart rate variability increased which enhanced sympathetic parasympathetic balance.
- Reducing subclinical hyperventilation by breathing slower and thereby increasing pC02.
- Increasing social support by meeting in small groups. The class discussion group normalized the anxiety experiences.
- Providing hope. The class lectures, assigned readings and videos provide hope; since, it included reports how other students had reversed their chronic disorders such as irritable bowel disease, acid reflux, psoriasis with behavioral interventions.
Although the study lacked a control group and is only based upon self-report, it offers an economical non-pharmaceutical approach to reduce anxiety. These stress management strategies may not resolve anxiety for everyone. Nevertheless, we recommend that schools implement this approach as the first education intervention to improve health in which students are taught about stress management, learn and practice relaxation and diaphragmatic breathing and then practice these skills during the day whenever they experience stress or dysfunctional breathing.
I noticed that breathing helped tremendously with my anxiety. I was able to feel okay without having that dreadful feeling stay in my chest and I felt it escape in my exhales. I also felt that I was able to breathe deeper and relax better altogether. It was therapeutic, I felt more present, aware, and energized.
See the following blogs for detailed breathing instructions
References
Adams. K.L., Saunders KE, Keown-Stoneman CDG, et al. (2021). Mental health trajectories in undergraduate students over the first year of university: a longitudinal cohort study. BMJ Open 2021; 11:e047393. https://doi.org/10.1136/bmjopen-2020-047393
Barr, E. A., Peper, E. & Swatzyna, R.J. (2019). Slouched Posture, Sleep Deprivation, and Mood Disorders: Interconnection and Modulation by Theta Brain Waves. Neuroregulation, 6(4), 181–189 https://doi.org/10.15540/nr.6.41.181
Bhattacharya, R., Shen, C. & Sambamoorthi, U. (2014). Excess risk of chronic physical conditions associated with depression and anxiety. BMC Psychiatry 14, 10 (2014). https://doi.org/10.1186/1471-244X-14-10
Bier, M., Peper, E., & Burke, A. (2005). Integrated stress management with ‘Make Health Happen: Measuring the impact through a 5-month follow-up. Poster presentation at the 36th Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract published in: Applied Psychophysiology and Biofeedback, 30(4), 400. https://biofeedbackhealth.files.wordpress.com/2013/12/2005-aapb-make-health-happen-bier-peper-burke-gibney3-12-05-rev.pdf
Bierman, E.J.M., Comijs, H.C. , Jonker, C. & Beekman, A.T.F. (2005). Effects of Anxiety Versus Depression on Cognition in Later Life. The American Journal of Geriatric Psychiatry,13(8), 686-693, https://doi.org/10.1097/00019442-200508000-00007.
Brad, J., Bushman, C., DeWall, N., Pond, R.S., &. Hanus, M.D. (2014).. Low glucose relates to greater aggression in married couples. PNAS, April 14, 2014. https://doi.org/10.1073/pnas.1400619111
Chirikov, I., Soria, K. M, Horgos, B., & Jones-White, D. (2020). Undergraduate and Graduate Students’ Mental Health During the COVID-19 Pandemic. UC Berkeley: Center for Studies in Higher Education. Retrieved from https://escholarship.org/uc/item/80k5d5hw
Coakley, K.E., Le, H., Silva, S.R. et al. Anxiety is associated with appetitive traits in university students during the COVID-19 pandemic. Nutr J 20, 45 (2021). https://doi.org/10.1186/s12937-021-00701-9
Crane,E.H. (2013).Highlights of the 2011 Drug Abuse Warning Network (DAWN) Findings on Drug-Related Emergency Department Visits. 2013 Feb 22. In: The CBHSQ Report. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2013-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384680/
Du Pasquier, D., Fellrath, J.M., & Sauty, A. (2020). Hyperventilation syndrome and dysfunctional breathing: update. Revue Medicale Suisse, 16(698), 1243-1249. https://europepmc.org/article/med/32558453
Gilbert C. Clinical Applications of Breathing Regulation: Beyond Anxiety Management. Behavior Modification. 2003;27(5):692-709. https://doi.org/10.1177/0145445503256322
Kaczkurkin, A.N. & Foa, E.B. (2015). Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues Clin Neurosci. 17(3):337-46. https://doi.org/10.31887/DCNS.2015.17.3/akaczkurkin
Kang, H. J., Bae, K. Y., Kim, S. W., Shin, H. Y., Shin, I. S., Yoon, J. S., & Kim, J. M. (2017). Impact of Anxiety and Depression on Physical Health Condition and Disability in an Elderly Korean Population. Psychiatry investigation, 14(3), 240–248. https://doi.org/10.4306/pi.2017.14.3.240
Klein, A. & Peper, W. (2013). There is Hope: Autogenic Biofeedback Training for the Treatment of Psoriasis. Biofeedback, 41(4), 194–201. https://doi.org/10.5298/1081-5937-41.4.01
Lum, L. C. (1981). Hyperventilation and anxiety state. Journal of the Royal Society of Medicine, 74(1), 1-4. https://journals.sagepub.com/doi/pdf/10.1177/014107688107400101
MacCormack, J. K., & Lindquist, K. A. (2019). Feeling hangry? When hunger is conceptualized as emotion. Emotion, 19(2), 301–319. https://doi.org/10.1037/emo0000422
McGrady, A. & Moss, D. (2013). Pathways to illness, pathways to health. New York: Springer. https://link.springer.com/book/10.1007/978-1-4419-1379-1
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make health happen: Training yourself to create wellness. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/make-health-happen
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91 https://www.neuroregulation.org/article/view/22815/14575
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. doi:10.15540/nr.6.3.1533-1 https://www.neuroregulation.org/article/view/19455/13261
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Lin, I-M, Harvey, R., Gilbert, M., Gubbala, P., Ratkovich, A., & Fletcher, F. (2014). Transforming chained behaviors: Case studies of overcoming smoking, eczema and hair pulling (trichotillomania). Biofeedback, 42(4), 154-160. https://doi.org/10.5298/1081-5937-42.4.06
Peper, E., MacHose, M. (1993). Symptom prescription: Inducing anxiety by 70% exhalation. Biofeedback and Self-Regulation 18, 133–139). https://doi.org/10.1007/BF00999790
Peper, E., Miceli, B., & Harvey, R. (2016). Educational Model for Self-healing: Eliminating a Chronic Migraine with Electromyography, Autogenic Training, Posture, and Mindfulness. Biofeedback, 44(3), 130–137. https://doi.org/10.5298/1081-5937-44.3.03
Peper, E., Sato-Perry, K & Gibney, K. H. (2003). Achieving Health: A 14-Session Structured Stress Management Program—Eczema as a Case Illustration. 34rd Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract in: Applied Psychophysiology and Biofeedback, 28(4), 308. Proceeding in: http://www.aapb.org/membersonly/articles/P39peper.pdf
Richmond-Rakerd, L.S., D’Souza, S, Milne, B.J, Caspi, A., & Moffitt, T.E. (2022). Longitudinal Associations of Mental Disorders with Dementia: 30-Year Analysis of 1.7 Million New Zealand Citizens. JAMA Psychiatry. Published online February 16, 2022. https://doi.org/10.1001/jamapsychiatry.2021.4377
Shri, R. (2012). Anxiety: Causes and Management. The Journal of Behavioral Science, 5(1), 100–118. Retrieved from https://so06.tci-thaijo.org/index.php/IJBS/article/view/2205
Wilhelm, F.H., Gevirtz, R., & Roth, W.T. (2001). Respiratory dysregulation in anxiety, functional cardiac, and pain disorders. Assessment, phenomenology, and treatment. Behav Modif, 25(4), 513-45. https://doi.org/10.1177/0145445501254003
Do nose breathing FIRST in the age of COVID-19
Posted: May 30, 2020 Filed under: Breathing/respiration, health, self-healing, Uncategorized | Tags: anxiety, COVID-19, HRV, nasal breathing, respiration 3 Comments
Breathing affects every cell of our body and should be the first intervention strategy to improve physical and mental well-being (Peper & Tibbetts, 1994). Breathing patterns are much more subtle than indicated by the respiratory function tests (spirometry, lung capacity, airway resistance, diffusing capacity and blood gas analysis) or commonly monitored in medicine and psychology (breathing rate, tidal volume, peak flow, oxygen saturation, end-tidal carbon dioxide) (Gibson, Loddenkemper, Sibille & Lundback, 2019).
When a person feels safe, healthy and peaceful, the breathing is effortless and the breath flows in and out of the nose without awareness. Functional and dysfunctional breathing patterns includes an assessment of the whole body pattern by which breathing occurs such as nose versus mouth breathing, alternation of nasal patency, the rate of air flow rate during inhalation and exhalation, the length of time during inhalation and exhalation, the post exhalation pause time. the pattern of transition between inhaling and exhaling, the location and timing of expansion in the truck, the range of diaphragmatic movement, and the subjective quality of breathing effort (Gilbert, 2019; Peper, Gilbert, Harvey & Lin, 2015; Nestor, 2020).
Breathing patterns affect sympathetic and parasympathetic nervous systems (Levin & Swoap, 2019). Inhaling tends to activate the sympathetic nervous system (fight/flight response) while exhaling activates the parasympathetic nervous system (rest and repair response) (Lehrer & Gevirtz, 2014). To observe how breathing affects your heart rate, monitor your pulse from either the radial artery in the wrist or the carotid artery in your neck as shown in Figure 1 and practice the following.
After sensing the baseline rate of your pulse, continue to feel your radial artery pulse in your wrist or at the carotid artery in your neck. Then inhale for the count of four hold for a moment and gently exhale for the count of 5 or 6. Repeat two or three times.
Most people observe that during inhalation, their heart rate increased (sympathetic activation for action) and during exhalation, the heart rate decreases (restoration during safety).
Nearly everyone who is anxious tends to breathe rapidly and shallowly or when stressed, unknowingly gasp or holds their breath–they may even freeze up and blank out (Peper et al, 2016). In addition, many people habitually breathe through their mouth instead of their nose and wake up tired with a dry mouth with bad breath. Mouth breathing combined with chest breathing in the absence of slower diaphragmatic breathing (the lower ribs and abdomen expand during inhalation and constrict during exhalation) is a risk factor for disorders such as irritable bowel syndrome, hypertension, tiredness, anxiety, panic attacks, asthma, dysmenorrhea, epilepsy, cold hands and feet, emphysema, and insomnia. Many of our clients who aware of their dysfunctional breathing patterns and are able to implement effortless breathing report significant reduction in symptoms (Chaitow, Bradley, & Gilbert, 2013; Peper, Mason, Huey, 2017; Peper & Cohen, 2017; Peper, Martinez Aranda, & Moss, 2015).
Breathing is usually overlooked as a first treatment strategy-it is not as glamorous as drugs, surgery or psychotherapy. Teaching breathing takes skill since practitioners needs to be experienced. Namely, they need to be able to demonstrate in action how to breathe effortlessly before teaching it to others. Although it seems unbelievable, a small change in our breathing pattern can have major physical, mental, and emotional effects as can be experienced in the following practice.
Begin by breathing normally and then exhale only 70% of the inhaled air, and inhale normally and again exhale only 70% of the inhaled air. With each exhalation exhale on 70% of the inhaled air. Continue this for 30 seconds. Stop and note how you feel.
Almost every reports that the 30 seconds feels like a minute and experience some of the following symptoms listed in table 1.

Table 1. Symptoms experienced after 30-45 seconds of sequentially exhaling 70% percent of the inhales air (Peper & MacHose, 1993).
Even though many therapists have long pointed out that breathing is essential, it is usually the forgotten ingredient. It is now being rediscovered in the age of the COVID-19 as respiratory health may reduce the risk of COVID-19.
Simply having very sick patients lie on their side or stomach can improve gas exchange. By lying on your side or prone, breathing is easier as the lung can expand more which appears to reduce the utilization of respirators and intubation (Long & Singh, 2020; Farkas, 2020). This side or prone breathing approach is thousands of years old.
One of the natural and health promoting breathing patterns to promote lung health is to breathe predominantly through the nose. The nose filters, warms, moisturizes and slows the airflow so that airway irritation is reduced. Nasal breathing also increases nitric oxide production that significantly increases oxygen absorption in the body. More importantly for dealing with COVID-19, nitric oxide, produced and released inside the nasal cavities and the lining of the blood vessels, acts as an anti-viral and is a secondary strategy to protect against viral infections (Mehta, Ashkar & Mossman, 2012). During inspiration through the nose, the nitric oxide helps dilate the airways in your lungs and blood vessels (McKeown, 2016).
To increase your health, breathe through your nose, yes, even at night (McKeown, 2020). As you practice this during the day be sure that the lower ribs and abdomen expand during inhalation and decrease in diameter during exhalation. It is breathing without effort although many people will report that it initially feels unnatural. Exhale to the count of about 5 or 6 and inhale (allow the air to flow in) to the count of 4 or 5. Mastering nasal breathing takes practice, practice and practice. See the following for more information.
Watch the Youtube presentation by Patrick McKeown author of the Oxygen Advantage, Practical 40 minute free breathing session with Patrick McKeown to improve respiratory health. https://www.youtube.com/watch?v=AiwrtgWQeDc&t=680s
Listen to Terry Gross interviewing James Nestor on “How The ‘Lost Art’ Of Breathing Can Impact Sleep And Resilience” on May 27, 2020 on the NPR radio show, Fresh Air.
Look at the Peperperspective blogs that focus on breathing in the age of Covid-19.
Read science writer James Nestor’s book, Breath The new science of a lost art, Breath The new science of a lost art.

References
Allen, R. (2017).The health benefits of nose breathing. Nursing in General Practice.
Christopher, G. (2019). A Guide to Monitoring Respiration. Biofeedback, 47(1), 6-11.
Farkas, J. (2020). PulmCrit – Awake Proning for COVID-19. May 5, 2020.
Long, L. & Singh, S. (2020). COVID-19: Awake Repositioning / Proning. EmDocs
McKeown, P. (2016). Oxygen advantage. New York: William Morrow.
Nestor, James. (2020). Breath The new science of a lost art. New York: Riverhead Books
Anxiety, lightheadedness, palpitations, prodromal migraine symptoms? Breathing to the rescue!
Posted: March 24, 2019 Filed under: behavior, Breathing/respiration, emotions, health, Pain/discomfort, relaxation, Uncategorized | Tags: anxiety, aura, diaphragmatic breathing, dizzyness, light headedness, migraine, prodrome, symptom prescription 5 Comments
I quickly gasped twice and a sharp pain radiated up my head and into my eye. I shifted to slow breathing and it faded away.
I felt anxious and became aware of my heart palpitations at the end of practicing 70% exhalation for 30 seconds. I was very surprised how quickly my anxiety was triggered when I changed my breathing pattern.
Breathing is the body/mind/emotion/spirit interface which is reflected in our language with phrases such as a sigh of relief, all choked up, breathless, full of hot air, waiting with bated breath, inspired or expired, all puffed up, breathing room, or it takes my breath away. The colloquial phrases reflect that breathing is more than gas exchange and may have the following effects.
- Changes the lymph and venous blood return from the abdomen (Piller, Leduc, & Ryan, 2006). The downward movement of the diaphragm with the corresponding expansion of the abdomen occurs during inhalation as well as slight relaxation of the pelvic floor. The constriction of the abdomen and slight tightening of the pelvic floor causing the diaphragm to go upward and allows exhalation. This dynamic movement increases and decreases internal abdominal and thoracic pressures and acts a pump to facilitate the venous and lymph return from the abdomen. In many people this dynamic pumping action is reduced because the abdomen does not expand during inhalation as it is constricted by tight clothing (designer jean syndrome), holding the abdomen in to maintain a slim self-image, tightening the abdomen in response to fear, or the result of learned disuse to reduce pain from abdominal surgery, gastrointestinal disorders, or abdominal insults (Peper et al, 2015).
- Increases spinal disk movement. Effortless diaphragmatic breathing is a whole body process and associated with improved functional movement (Bradley, & Esformes, 2014). The spine slightly flexes when we exhale and extends when we inhale which allows dynamic disk movement unless we sit in a chair.
- Communicates our emotional state as our breathing patterns reflect our emotional state. When we are anxious or fearful the breath usually quickens and becomes shallow while when we relax the breath slows and the movement is more in the abdomen (Homma, & Masoka, 2008).
- Evokes, maintains, inhibits symptoms or promotes healing. Breathing changes our physiology, thoughts and emotions. When breathing slowly to about 6 breaths a minute, it may enhance heart rate variability and thereby increase sympathetic and parasympathetic balance (Lehrer & Gevirtz, 2014; Moss & Shaffer, 2017).
Can breathing trigger symptoms?
A fifty-five year old woman asked for suggestions what she could do to prevent the occurrence of episodic prodrome and aura symptoms of visual disturbances and problems in concentration that would signal the onset of a migraine. In the past, she had learned to control her migraines with biofeedback; however, she now experienced these prodromal sensation more and more frequently without experiencing the migraine. As she was talking, I observed that she was slightly gasping before speaking with shallow rapid breathing in her chest.
To explore whether breathing pattern may contribute to evoke, maintain or amplify symptoms, the following two behavioral breathing challenges can suggest whether breathing is a factor: Rapid fearful gasping or 70% exhalation.
Behavioral breathing challenge: Rapid fearful gasping
Take a rapid fearful gasp when inhaling as if your feel scared or fearful. Let the air really quickly come in and repeat two or three times as described in the video. Then describe what you experienced.
If you became aware of the onset of a symptom or that the symptom intensified, then your dysfunctional breathing patterns (e.g., gasping, breath holding or shallow chest breathing) may contribute to development or maintenance of these symptoms. For many people when they gasp–a big rapid inhalation as if they are terrified–it may evoke their specific symptom such as a pain sensation in the back of the eye, slight pain in the neck, blanking out, not being able to think clearly, tightness and stiffness in their back, or even an increase in achiness in their joints (Peper et al, 2016).
To reduce or avoid triggering the symptom, breathe diaphragmatically without effort; namely each time you gasp, hold your breath or breathe shallowly, shift to effortless diaphragmatic breathing.
The above case of the woman with the prodromal migraine symptoms, she experienced visual disturbances and fuzziness in her head after the gasping. This experience allowed her to realize that her breathing style could be a contributing in triggering her symptoms. When she then practiced slow diaphragmatic breathing for a few breaths her symptoms disappeared. Hopefully, if she replaces gasping and shallow breathing with effortless diaphragmatic breathing then there is a possibility that her symptoms may no longer occur.
Behavioral breathing challenge: 70% exhalation
While sitting, breathe normally for a minute. Now change your breathing pattern so that you exhale only 70% or your previous inhaled air. Each time you exhale, exhale only 70% of the inhaled volume. If you need to stop, just stop, and then return to this breathing pattern again by exhaling only 70 percent of the inhaled volume of air. After 30 seconds, let go and breathe normally as guided by the video clip. Observe what happened?
In our research study with 35 volunteers, almost all participants experienced an increase in arousal and symptoms such as lightheadedness, dizziness, anxiety, breathless, neck and shoulder tension after 30 seconds of incomplete exhalation as shown in Figure 1 and Table 1 (Peper and MacHose, 1993).

Figure 1. Increase in anxiety evoked by 70% exhalation.

Table 1. Symptoms experienced after exhalation 70%.
Although these symptoms may be similar to those evoked by hyperventilation and overbreathing, they are probably not caused by the reduction of end-tidal carbon dioxide (CO2). The apparent decrease in end-tidal PCO2 is cause by the room air mixing with the exhaled air and not a measure of end-tidal CO2 (Peper and Tibbets, 1992). Most likely the symptoms are associated by the shallow breathing that occurs when we were scared or terrified.
People who have a history of anxiety, panic, nervousness and tension as compared to those who report low anxiety tend to report more symptoms when exhaling 70% of inhaled air for 30 seconds. If this practice evoked symptoms, then changing the breathing patterns to slower diaphragmatic breathing may be a useful self-regulation strategy to optimize health.
These two behavior breathing challenges are useful demonstrations for students and clients that breathing patterns can influence symptoms. By experiencing ON and OFF control over their symptoms with breathing, the person now knows that breathing can affect their health and well being.
BLOGS WITH INSTRUCTIONS FOR LEARNING EFFORTLESS DIAPHRAGMATIC BREATHING
https://peperperspective.com/2017/11/17/breathing-to-improve-well-being/
https://peperperspective.com/2018/10/04/breathing-reduces-acid-reflux-and-dysmenorrhea-discomfort/
https://peperperspective.com/2015/02/18/reduce-hot-flashes-and-premenstrual-symptoms-with-breathing/
https://peperperspective.com/2017/03/19/enjoy-sex-breathe-away-the-pain/
REFERENCES
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Frontiers in Psychology, 5
Breathing to improve well-being
Posted: November 17, 2017 Filed under: Breathing/respiration, Exercise/movement, Neck and shoulder discomfort, Pain/discomfort, self-healing, stress management, Uncategorized | Tags: anxiety, Breathing, health, mindfulness, pain, respiration, stress 8 CommentsBreathing affects all aspects of your life. This invited keynote, Breathing and posture: Mind-body interventions to improve health, reduce pain and discomfort, was presented at the Caribbean Active Aging Congress, October 14, Oranjestad, Aruba. www.caacaruba.com
The presentation includes numerous practices that can be rapidly adapted into daily life to improve health and well-being.

