Quick Rescue Techniques When Stressed
Posted: February 4, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, education, emotions, Evolutionary perspective, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, posture, relaxation, stress management, Uncategorized | Tags: alarm reaction, anxiety, box breathing, Breathing, conditioning, defense reaction, health, huming, Parasympathetic response, rumination, safety, sniff inhale, somatic practices, stress, sympathetic arousal, tactical breathing, Toning, yoga 2 CommentsErik Peper, PhD, Yuval Oded, PhD, and Richard Harvey, PhD
Adapted from Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312

“If a problem is fixable, if a situation is such that you can do something about it, then there is no need to worry. If it’s not fixable, then there is no help in worrying. There is no benefit in worrying whatsoever.” ― Dalai Lama XIV
To implement the Dalai Lama’s quote is challenging. When caught up in an argument, being angry, extremely frustrated, or totally stressed, it is easy to ruminate, worry. It is much more challenging to remember to stay calm. When remembering the message of the Dalai Lama’s quote, it may be possible to shift perspective about the situation although a mindful attitude may not stop ruminating thoughts. The body typically continues to reacti to the torrents of thoughts that may occur when rehashing rage over injustices, fear over physical or psychological threats, or profound grief and sadness over the loss of a family member. Some people become even more agitated and less rational as illustrated in the following examples.
I had an argument with my ex and I am still pissed off. Each time I think of him or anticipate seeing them, my whole body tightened. I cannot stomach seeing him and I already see the anger in his face and voice. My thoughts kept rehashing the conflict and I am getting more and more upset.
A car cut right in front of me to squeeze into my lane. I had to slam on my brakes. What an idiot! My heart rate was racing and I wanted to punch the driver.
When threatened, we respond quickly in our thoughts and body with a defense reaction that may negatively affect those around us as well as ourselves. What can we do to interrupt negative stress reactions?
Background
Many approaches exist that allow us to become calmer and less reactive. General categories include techniques of cognitive reappraisal (seeing the situation from the other person’s point of view and labeling your own feelings and emotions) and stress management techniques. Practices that are beneficial include mindfulness meditation, benign humor (versus gallows humor), listening to music, taking a time out while implementing a variety of self-soothing practices, or incorporating slow breathing (e.g., heart rate variability and/or box breathing) throughout the day.
No technique fits all as we respond differently to our stressful life circumstances. For example, some people during stress react with a “tend and befriend stress response” (Cohen & Lansing, 2021; Taylor et al., 2000). This response appears to be mostly mediated by the hormone oxytocin acting in ways that sooth or calm the nervous system as an analgesic. These neurophysiological mechanisms of the soothing with the calming analgesic effects of oxytocin have been characterized in detail by Xin, et al. (2017).
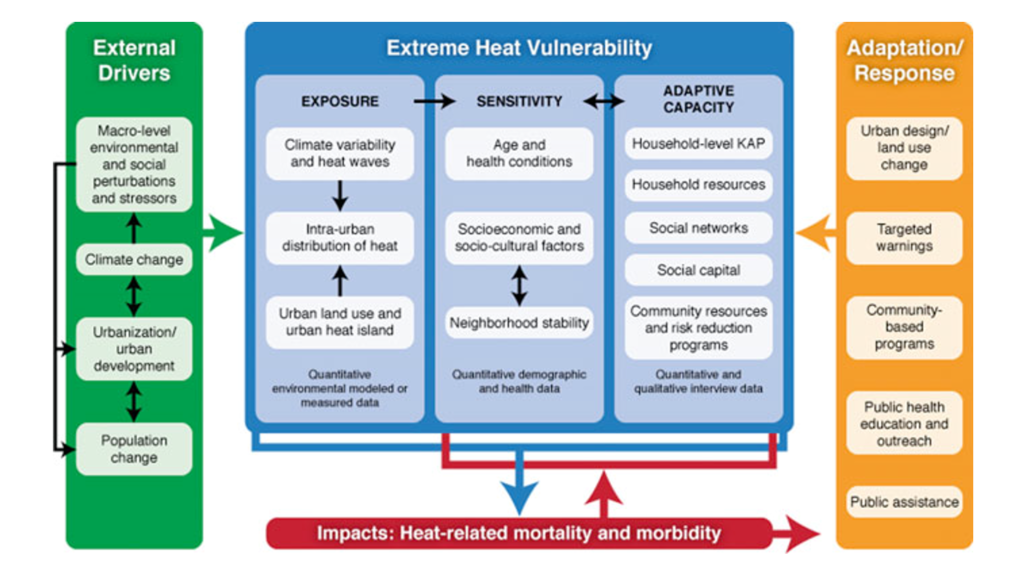
The most common response is a fight/flight/freeze stress response that is mediated by excitatory hormones such as adrenalin and inhibitory neurotransmitters such as gamma amino butyric acid (GABA). There is a long history of fight/flight/freeze stress response research, which is beyond the scope of this blog with major theories and terms such as interior milleau (Bernard, 1872); homeostasis and fight/flight (Cannon, 1929); general adaptation syndrome (Selye, 1951); polyvagal theory (Porges, 1995); and, allostatic load (McEwen, 1998). A simplified way to start a discussion about stress reactions begins with the fight/flight stress response. When stressed our defense reactions are triggered. Our sympathetic nervous system becomes activated our mind and body stereotypically responds as illustrated in Figure 1.
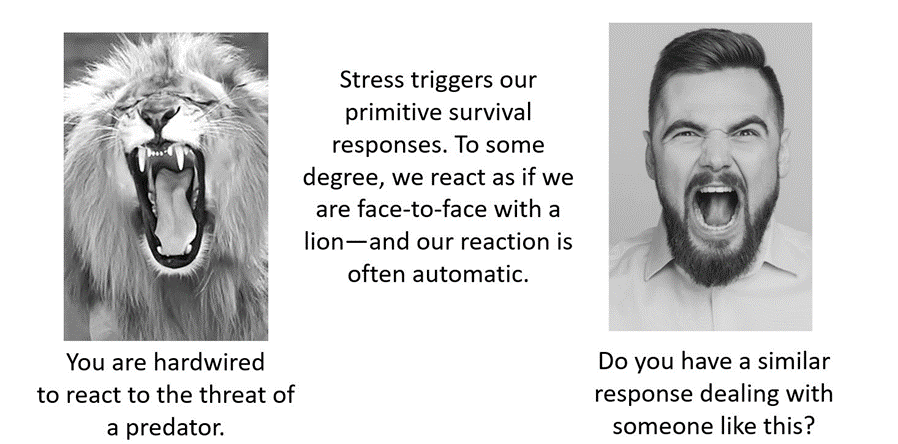
Figure 1. An intense confrontation tends to evoke a stress response (reproduced from Peper et al., 2020).
The flight/fight response triggers a cascade of stress hormones or neurotransmitters (e.g., hypothalamus-pituitary-adrenal cascade) and produces body changes such as the heart pounding, quicker breathing, an increase in muscle tension and sweating. Our body mobilizes itself to protect itself from danger. Our focus is on immediate survival and not what will occur in the future (Porges, 2021; Sapolsky, 2004). It is as if we are facing an angry lion—a life-threatening situation—and we feel threatened and unsafe.
Rather than sitting still, a quick effective strategy is to interrupt this fight/flight response process by completing the alarm reaction such as by moving our muscles (e.g., simulating a fight or flight behavior) before continuing with slower breathing or other self-soothing strategies. Many people have experienced their body tension is reduced and they feel calmer when they do vigorous exercise after being upset, frustrated or angry. Similarly, athletes often have reported that they experience reduced frequency and/or intensity of negative thoughts after an exhausting workout (Thayer, 2003; Liao et al., 2015; Basso & Suzuki, 2017).
Becoming aware of the escalating cascades of physical, behavioral and psychological responses to a stressor is the first step in interrupting the escalating process. After becoming aware, reduce the body’s arousal and change the though patterns using any of the techniques described in this blog. The self-regulation skills presented in this blog are ideally over-learned and automated so that these skills can be rapidly implemented to shift from being stressed to being calm. Examples of skills that can shift from sympathetic neervous system overarousal to parasympathetic nervous system calm include techniques of autogenic traing (Schulz & Luthe, 1959), the quieting reflex developed by Charles Stroebel in 1985 or more recently rescue breathing developed by Richard Gevirtz (Stroebel, 1985; Gevirtz, 2014; Peper, Gibney & Holt, 2002; Peper & Gibney, 2003).
Concepts underlying the rescue techniques
- Psychophysiological principle: “Every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, conscious or unconscious, and conversely, every change in the mental-emotional state, conscious or unconscious, is accompanied by an appropriate change in the physiological state” (Green et al. 1970, p. 3).
- Posture evokes memories and feelings associated with the position. When the body posture is erect and tall while looking slightly up. It is easier to evoke empowering, positive thoughts and feelings. When looking down it is easier to evoke hopeless, helpless and powerless thoughts and feelings (Peper et al., 2017).
- Healing occurs more easily when relaxed and feeling safe. Feeling safe and nurtured enhances the parasympathetic state and reduces the sympathetic state. Use memory recall to evoke those experiences when you felt safe (Peper, 2021).
- Interrupting thoughts is easier with somatic movement than by redirecting attention and thinking of something else without somatic movement.
- Focus on what you want to do not want to do. Attempting to stop thinking or ruminating about something tends to keeps it present (e.g., do not think of pink elephants. What color is the elephant? When you answer, “not pink,” you are still thinking pink). A general concept is to direct your attention (or have others guide you) to something else (Hilt & Pollak, 2012; Oded, 2018; Seo, 2023).
- Skill mastery takes practice and role rehearsal (Lally et al., 2010; Peper & Wilson, 2021).
- Use classical conditioning concepts to facilitate shifting states. Practice the skills and associate them with an aroma, memory, sounds or touch cues. Then when you the situation occurs, use these classical conditioned cues to facilitate the regeneration response (Peper & Wilson, 2021).
Rescue techniques
Coping When Highly Stressed and Agitated
- Complete the alarm/defense reaction with physical activity (Be careful when you do these physical exercises if you have back, hip, knee, or ankle problems).
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Check whether the situation is actually a threat. If yes, then do anything to get out of immediate danger (yell, scream, fight, run away, or dial 911).
- If there is no actual physical threat, then leave the situation and perform vigorous physical activity to complete your alarm reaction, such as going for a run or walking quickly up and down stairs. As you do the exercise, push yourself so that the muscles in your thighs are aching, which focusses your attention on the sensations in your thighs. In our experience, an intensive run for 20 minutes quiets the brain while it often takes 40 minutes when walking somewhat quickly.
- After recovering from the exhaustive exercise, explore new options to resolve the conflict.
- Complete the alarm/defense reaction and evoke calmness with the S.O.S™ technique (Oded, 2023)
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Squat against a wall (similar to the wall-sit many skiers practice). While tensing your arms and fists as shown in Figure 2, gaze upward because it is more difficult to engage in negative thinking while looking upwards. If you continue to ruminate, then scan the room for object of a certain color or feature to shift visual attention and be totally present on the visual object.
- Do this set of movements for 7 to 10 seconds or until you start shaking. Than stand up and relax hands and legs. While standing, bounce up and down loosely for 10 to 15 seconds as you become aware of the vibratory sensations in your arms and shoulders, as shown in Figure 3.

Figure 2.Defense position wall-sit to tighten muscles in the protective defense posture (Oded, 2023). Figure 3. Bouncing up and down to loosen muscles ((Oded, 2023).
- Acknowledge you have reacted and have chosen to interrupt your automatic response. Swing your arms back and forth for 20 seconds. Allow the arms to swing freely as illustrated in Figure 4.

Figure 4. Swinging the arms to loosen the body and spine (Oded, 2023).
- Rest and ground. Lie on the floor and put your calves and feet on a chair seat so that the psoas muscle can relax, as illustrated in Figure 5. Allow yourself to be totally supported by the floor and chair. Be sure there is a small pillow under your head and put your hand on your abdomen so that you can focus on abdominal breathing.

Figure 5. Lying down to allow the psoas muscle to relax and feel grounded (Oded, 2023).
- While lying down, imagine a safe place or memory and make it as real as possible. It is often helpful to listen to a guided imagery or music. The experience can be enhanced if cues are present that are associated with the safe place, such as pictures, sounds, or smells. Continue to breathe effortlessly at about six breaths per minute. If your attention wanders, bring it back to the memory or to the breathing. Allow yourself to rest for 10 minutes.
In most cases, thoughts stop and the body’s parasympathetic activity becomes dominant as the person feels safe and calm. Usually, the hands warm and the blood volume pulse amplitude increases as an indicator of feeling safe, as shown in Figure 6.

Figure 6. Blood volume pulse increases as the person is relaxing, feels safe and calm.
Coping When You Can’t Get Away (adapted from Peper, Harvey & Faass, 2020)
In many cases, it is difficult or embarrassing to remove yourself from the situation when you are stressed out such as at work, in a business meeting or social gathering.
- Become aware that you have reacted.
- Excuse yourself for a moment and go to a private space, such as a restroom. Going to the bathroom is one of the only acceptable social behaviors to leave a meeting for a short time.
- In the bathroom stall, do the 5-minute Nyingma exercise, which was taught by Tarthang Tulku Rinpoche in the tradition of Tibetan Buddhism, as a strategy for thought stopping (see Figure 7). Stand on your toes with your heels touching each other. Lift your heels off the floor while bending your knees. Place your hands at your sides and look upward. Breathe slowly and deeply (e.g., belly breathing at six breaths a minute) and imagine the air circulating through your legs and arms. Do this slow breathing and visualization next to a wall so you can steady yourself if necessary to keep balance. Stay in this position for 5 minutes or longer. Do not straighten your legs—keep squatting despite the discomfort. In a very short time, your attention is captured by the burning sensation in your thighs. Continue. After 5 minutes, stop and shake your arms and legs.
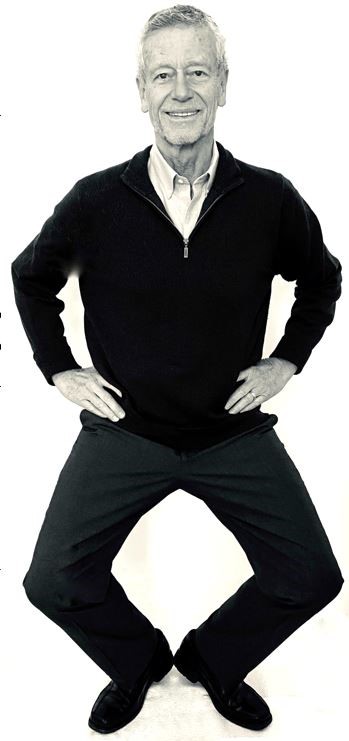
Figure 7. Stressor squat Nyingma exercise (reproduced from Peper et al., 2020).
- Follow this practice with slow abdominal breathing to enhance the parasympathetic response. Be sure that the abdomen expands as the inhalation occurs. Breathe in and out through the nose at about six breaths per minute.
- Once you feel centered and peaceful, return to the room.
- After this exercise, your racing thoughts most likely will have stopped and you will be able to continue your day with greater calm.
What to do When Ruminating, Agitated, Anxious or Depressed
(adapted from Peper, Harvey, & Hamiel, 2019).
- Shift your position by sitting or standing erect in a power position with the back of the head reaching upward to the ceiling while slightly gazing upward. Then sniff quickly through nose, hold and again sniff quickly then very slowly exhale. Be sure as you exhale your abdomen constricts. Then sniff again as your abdomen gets bigger, hold, and sniff one more time letting the abdomen get even bigger. Then, very slow, exhale through the nose to the internal count of six (adapted from Balban et al., 2023). When you sniff or gasp, your racing thoughts will stop (Peper et al., 2016).
- Continue with box breathing (sometimes described as tactical breathing or battle breathing) by exhaling slowly through your nose for 4 seconds, holding your breath for 4 seconds, inhaling slowly for 4 seconds through your nose, holding your breath for 4 seconds and then repeating this cycle of breathing for a few minutes (Röttger et al., 2021; Balban et al., 2023). Focusing your attention on performing the box breathing makes it almost impossible to think of anything else. After a few minutes, follow this with slow effortless diaphragmatic breathing at about six breaths per minute. While exhaling slowly through your nose, look up and when you inhale imagine the air coming from above you. Then as you exhale, imagine and feel the air flowing down and through your arms and legs and out the hands and feet.
- While gazing upward, elicit a positive memory or a time when you felt safe, powerful, strong and/or grounded. Make the positive memory as real as possible.
- Implement cognitive strategies such as reframing the issue, sending goodwill to the person, seeing the problem from the other person’s point of view, and ask is this problem worth dying over (Peper, Harvey, & Hamiel, 2019).
What to Do When Thoughts Keep Interrupting
Practice humming or toning. When you are humming or toning, your focus is on making the sound and the thoughts tend to stop. Generally, breathing will slow down to about six breaths per minute (Peper, Pollack et al., 2019). Explore the following:
- Box breathing (Röttger et al., 2021; Balban et al., 2023)
- Humming also known as bee breath (Bhramari Pranayama) (Abishek et al., 2019; Yoga, 2023) – Allow the tongue to rest against the upper palate, sit tall and erect so that the back of the head is reaching upward to the ceiling, and inhale through your nose as the abdomen expands. Then begin humming while the air flows out through your nose, feel the vibration in the nose, face and throat. Let humming last for about 7 seconds and then allow the air to blow in through the nose and then hum again. Continue for about 5 minutes.
- Toning – Inhale through your nose and then vocalize a single sound such as Om. As you vocalize the lower sound, feel the vibration in your throat, chest and even going down to the abdomen. Let each toning exhalation last for about 6 to 7 seconds and then inhale through your nose. Continue for about 5 minutes (Peper, al., 2019).
Many people report that after practice these skills, they become aware that they are reacting and are able to reduce their automatic reaction. As a result, they experience a significant decrease in their stress levels, fewer symptoms such as neck and holder tension and high blood pressure, and they feel an increase in tranquility and the ability to communicate effectively.
Practicing these skills does not resolve the conflicts; they allow you to stop reacting automatically. This process allows you a time out and may give you the ability to be calmer, which allows you to think more clearly. When calmer, problem solving is usually more successful. As phrased in a popular meme, “You cannot see your reflection in boiling water. Similarly, you cannot see the truth in a state of anger. When the waters calm, clarity comes” (author unknown).

Boiling water (photo modified from: https://www.facebook.com/photo/?fbid=388991500314839&set=a.377199901493999)
Below are additional resources that describe the practices. Please share these resources with friends, family and co-workers.
Stressor squat instructions
Toning instructions
Diaphragmatic breathing instructions
Reduce stress with posture and breathing
Conditioning
References
Abishek, K., Bakshi, S. S., & Bhavanani, A. B. (2019). The efficacy of yogic breathing exercise bhramari pranayama in relieving symptoms of chronic rhinosinusitis. International Journal of Yoga, 12(2), 120–123. https://doi.org/10.4103/ijoy.IJOY_32_18
Balban, M. Y., Neri, E., Kogon, M. M., Weed, L., Nouriani, B., Jo, B., Holl, G., Zeitzer, J. M., Spiegel, D., Huberman, A. D. (2023). Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Reports Medicine, 4(1), 10089. https://doi.org/10.1016/j.xcrm.2022.100895
Basso, J. C. & Suzuki, W. A. (2017). The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plast, 2(2), 127–152. https://doi.org/10.3233/BPL-160040
Bernard, C. (1872). De la physiologie générale. Paris: Hachette livre. https://www.amazon.ca/PHYSIOLOGIE-GENERALE-BERNARD-C/dp/2012178596
Cannon, W. B. (1929). Organization for Physiological Homeostasis. Physiological Reviews, 9, 399–431. https://doi.org/10.1152/physrev.1929.9.3.399
Cohen, L. & Lansing, A. H. (2021). The tend and befriend theory of stress: Understanding the biological, evolutionary, and psychosocial aspects of the female stress response. In: Hazlett-Stevens, H. (eds), Biopsychosocial Factors of Stress, and Mindfulness for Stress Reduction. pp. 67–81, Springer, Cham. https://doi.org/10.1007/978-3-030-81245-4_3
Gevirtz, R. (2014). HRV Training and its Importance – Richard Gevirtz, Ph.D., Pioneer in HRV Research & Training. Thought Technology. Accessed December 29, 2023. https://www.youtube.com/watch?v=9nwFUKuJSE0
Green, E. E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological. Journal of Transpersonal Psychology, 2, 1–26. https://atpweb.org/jtparchive/trps-02-70-01-001.pdf
Hilt, L. M., & Pollak, S. D. (2012). Getting out of rumination: comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165.
https://doi.org/10.1007/s10802-012-9638-3
Lally, P., VanJaarsveld, C. H., Potts, H. W., & Wardle, J. (2010). How habits are formed: Modelling habit formation the real world. European Journal of Social Psychology, 40, 998–1009. https://doi.org/10.1002/ejsp.674
Liao, Y., Shonkoff, E. T., & Dunton, G. F. (2015). The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology. 6, 1975. https://doi.org/10.3389/fpsyg.2015.01975
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44.
https://doi.org/10.1111/j.1749-6632.1998.tb09546.x
Oded, Y. (2018). Integrating mindfulness and biofeedback in the treatment of posttraumatic stress disorder. Biofeedback, 46(2), 37-47. https://doi.org/10.5298/1081-5937-46.02.03
Oded, Y. (2023). Personal communication. S.O.S 1™ technique is part of the Sense Of Safety™ method. www.senseofsafety.co
Peper, E. (2021). Relive memory to create healing imagery. Somatics, XVIII(4), 32–35.https://www.researchgate.net/publication/369114535_Relive_memory_to_create_healing_imagery
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., & Gibney, K.H. (2003). A teaching strategy for successful hand warming. Somatics. XIV(1), 26–30. https://www.researchgate.net/publication/376954376_A_teaching_strategy_for_successful_hand_warming
Peper, E., Harvey, R., & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153–160. https://doi.org/10.15540/nr.6.3.153
Peper, E., Lee, S., Harvey, R., & Lin, I-M. (2016). Breathing and math performance: Implication for performance and neurotherapy. NeuroRegulation, 3(4), 142–149. http://dx.doi.org/10.15540/nr.3.4.142
Peper, E., Lin, I-M, Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128–133. https://www.neuroregulation.org/article/view/19345/13263
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 9(2), 46–49. https://doi.org/10.5298/1081-5937-49-2-04
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology, 32(4), 301–318. https://doi.org/10.1111/j.1469-8986.1995.tb01213.x
Porges, S.W. (2021) Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry, 20(2),296-298. Porges SW. Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry. 2021 Jun;20(2):296-298. https://doi.org10.1002/wps.20871
Röttger, S., Theobald, D. A., Abendroth, J., & Jacobsen, T. (2021). The effectiveness of combat tactical breathing as compared with prolonged exhalation. Applied Psychophysiology and Biofeedback, 46, 19–28. https://doi.org/10.1007/s10484-020-09485-w
Sapolsky, R. (2004). Why zebras don’t get ulcers (3rd ed.). New York:Holt. https://www.amazon.com/Why-Zebras-Dont-Ulcers-Third/dp/0805073698/
Schultz, J. H., & Luthe, W. (1959). Autogenic training: A psychophysiologic approach to psychotherapy. Grune & Stratton. https://www.google.com/books/edition/Autogenic_Training/y8SwQgAACAAJ?hl=en
Selye, H. (1951). The general-adaptation-syndrome. Annual Review of Medicine, 2(1), 327–342. https://doi.org/10.1146/annurev.me.02.020151.001551
Seo, H. (2023). How to stop ruminating. The New York Times. Accessed January 3, 2024. https://www.nytimes.com/2023/02/01/well/mind/stop-rumination-worry.html
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-quieting-reflex-Charles-Stroebel/dp/0425085066
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A. R., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. https://doi.org/10.1037/0033-295X.107.3.411
Thayer, R. E. (2003). Calm energy: How people regulate mood with food and exercise. Oxford University Press. https://www.amazon.com/Calm-Energy-People-Regulate-Exercise/dp/0195163397
Xin, Q., Bai, B., & Liu, W. (2017). The analgesic effects of oxytocin in the peripheral and central nervous system. Neurochemistry International, 103, 57–64. https://doi.org/10.1016/j.neuint.2016.12.021
Yoga, N. (2023). This simple breath practice is scientifically proven to calm your mind. The nomadic yogi. Accessed December 31, 2023. https://www.leahsugerman.com/blog/bhramari-pranayama-humming-bee-breath#
Reduce the risk for colds and flu and superb science podcasts
Posted: January 24, 2024 Filed under: attention, behavior, education, Evolutionary perspective, Exercise/movement, healing, health, Nutrition/diet, self-healing, stress management, Uncategorized, vision | Tags: colds, darkness, flu, influenza, light 1 Comment
What can we do to reduce the risk of catching a cold or the flu? It is very challenging to make sense out of all the recommendations found on internet and the many different media site such as X(Twitter), Facebook, Instagram, or TikTok. The following podcasts are great sources that examine different topics that can affect health. They are in-depth presentations with superb scientific reasoning.
Huberman Lab podcasts discusses science and science based tools for everyday life. https://www.hubermanlab.com/podcast. Select your episode and they are great to listen to on your cellphone.
THE PODCAST episode, How to prevent and treat cold and flu, is outstanding. Skip the long sponsor introductdion and start listening at the 6 minute point. In this podcast, Professor Andrew Huberman describes behavior, nutrition and supplementation-based tools supported by peer-reviewed research to enhance immune system function and better combat colds and flu. I also dispel common myths about how the cold and flu are transmitted and when you and those around you are contagious. I explain if common preventatives and treatments such as vitamin C, zinc, vitamin D and echinacea work. I also highlight other compounds known to reduce contracting and duration of colds and flu. I discuss how to use exercise and sauna to bolster the immune response. This episode will help listeners understand how to reduce the chances of catching a cold or flu and help people recover more quickly from and prevent the spread of colds and flu.
PODCAST, ScienceVS, is an outstanding podcast series that takes on fads, trends, and opinionated mob to find out what’s fact, what’s not, and what’s somewhere in between. Select your episode and listen.
Link: https://gimletmedia.com/shows/science-vs/episodes#show-tab-picker
PODCAST episode, The Journal club podcast and Youtube, presentation from Huberman Lab is a example of outstanding scientific reasoning. In this presentation, Professor Andrew Huberman and Dr. Peter Attia (author of Outlive: The Science and Art of Longevity) discuss two peer-reviewed scientific papers in-depth. The first discussion explores the role of bright light exposure during the day and dark exposure during the night and its relationship to mental health. The second paper explores a novel class of immunotherapy treatments to combat cancer.
Rethink the monies spent on cancer screening tests
Posted: November 24, 2023 Filed under: behavior, cancer, Evolutionary perspective, healing, health, Nutrition/diet, self-healing | Tags: breast canceer, Cancer screening, environmental toxins, Life style, mammography, organic foods Leave a commentErik Peper, PhD and Richard Harvey, PhD

Cancer screening tests are based upon the rational that early detection of fatal cancers enables earlier and more effective treatments (Kowalski, 2021), however, there is some controversy. Early screening may increase the risk of over diagnosis, treating false positives (people who did not have the cancer but the test indicates they have cancer) and potentially fatal treatment of cancers that would never progress to increase morbidity or mortality (Kowalski, 2021).
Today about $40 billion spent on colon cancer screening, $15 billion spent on breast cancer screening, and $4 billion spent on prostate cancer screening annually (CSPH, 2021). A question is raised whether the billions and billions of dollars spent on screening asymptomatic participants would be more wisely spent on promoting and supporting life style changes that reduce cancer risks and actually extend life span? That cancer screening is expensive does not mean no one should be screened. Instead, the argument is that the majority of healthcare dollars could be spent on health promotion practices and reserving screening for those people who are at highest risk for developing cancers.
What is the evidence that screening prolongs life?
Cancer screening tests appear correlated with preventing deaths since deaths due to cancers in the USA have decreased by about 28% from 1999 to 2020 (CDC, 2023a). Although cancer causes many of the deaths in the USA, overall life expectancy has increased by less than 1% from 1999 to 2020. If cancer screening were more effective, the life expectancy should have increased more because cancer is the second leading cause of death (CDC, 2023b). Consider also that deaths due to cancers may be coincident and or comorbid with other circumstances. For example, during the last four years, overall life expectancy in the USA has precipitously declined in part due to other causes of death such as the COVID pandemic and opioid overdose epidemic (Lewis, 2022). Decline in life expectancy in the USA has many contributing factors, including the ‘harms’ associated with cancer screening procedures. For example, perforations during colon cancer screening can lead to internal bleeding, or complications related to surgeries, radiotherapies or chemotherapies. Bretthauer et al., (2023) commented: “A cancer screening test may reduce cancer-specific mortality but fail to increase longevity if the harms for some individuals outweigh the benefits for others or if cancer-specific deaths are replaced by deaths from competing cause” (p. 1197).
Bretthauer et al. (2023) conducted a systematic review and meta-analysis of 18 long-term randomized clinical trials involving 2.1 million Individuals with more than nine years of follow-up reporting on all-cause mortality. They reported that“…this meta-analysis suggest that current evidence does not substantiate the claim that common cancer screening tests save lives by extending lifetime, except possibly for colorectal cancer screening with sigmoidoscopy.”
Following is a summary of Bretthauer et al. (2023) findings:
- The only cancer screening with a significant lifetime gain (approximately 3 months) was sigmoidoscopy.
- There was no significant difference between harms of screening and benefits of screening for:
- mammography
- prostate cancer screening
- FOBT (fecal occult blood test) screening every year or every other year
- lung cancer screening Pap test cytology for cervical cancer screening, no randomized clinical trials with cancer-specific or all-cause mortality end points and long term follow-up were identified.
Potential for loss or harm (e.g., iatrogenic and nosocomial) versus potential for benefit and extended life
More than 35 years ago a significant decrease in breast cancer mortality was observed after mammography was implemented. The correlation suggested a causal relationship that screening reduced mortality (Fracheboud, 2004). This correlation made logical sense since the breast cancer screening test identified cancers early which could then be treated and thereby would result in a decrease in mortality.
How much money is spent on screening that may correlate with unintended harms?
The annual total expenditure for cancer screening is estimated to be between $40-$50 billion annually (CSPH, 2021). Below are some of the estimated expenditures for common tests other than colorectal cancer screening, which arguably is costly; however, has potential benefits that outweigh potential harms.
- $10.37-13.94 billion for mammography to screen 50% of eligible women (Badal et al, 2023).
- $2-4 billion for prostate cancer (Ma et al., 2014)
- $1-2 billion for lung cancer (Taylor et al., 2022)
What is the correlation between initiation of mammography and decrease in breast cancer mortality?
The conclusion that mammography reduced breast cancer mortality was based upon studies without control groups; however, this relationship could be causal or synchronistic. The ambiguity of correlation or causation was resolved with the use of natural experimental control groups. Some European countries began screening 10 years earlier than other countries. Using statistical techniques such as propensity score matching when comparing the data from countries that initiated mammography screening early (Netherlands, Sweden and Northern Ireland) to countries that started screening 10 year later (Belgium, Norway and Republic of Ireland), the effectiveness of screening could be compared.
The comparisons showed no difference in the decrease of breast cancer mortality in countries that initiated breast cancer screening early or late. For example, there was no difference in the decrease of breast cancer mortality rates of women who lived in the Netherlands that started screening early versus those who lived in Belgium that began screening 10 years later, as is shown Figure 1 (Autier et al, 2011).
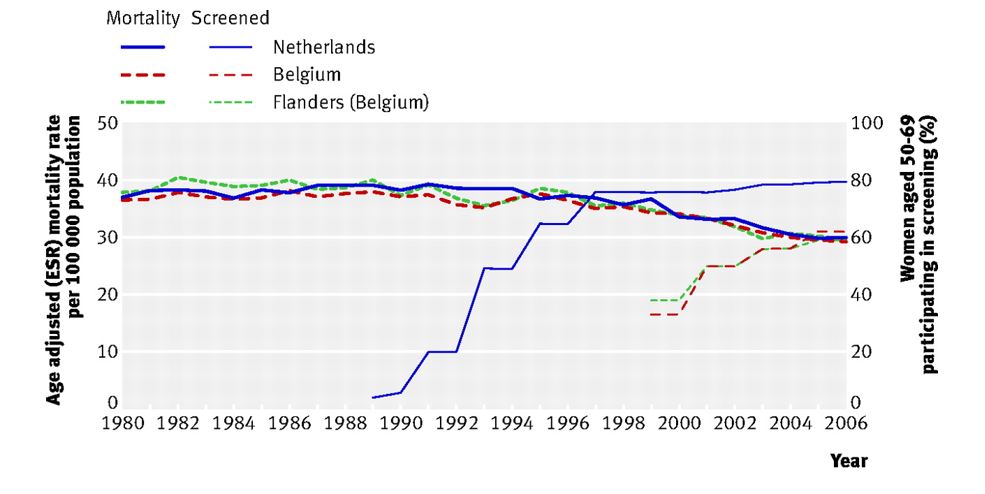
Figure 1. No difference in age adjust breast cancer mortality between the two adjacent countries even though breast cancer screening began ten years earlier in the Netherlands than in Belgium (graph reproduced from Autier et al, 2011).
The observations are similar when comparing neighboring countries: Sweden (early screening) to Norway (late screening) as well as Northern Ireland, UK (early screening) compared to the Republic of Ireland (late screening). The systematic comparisons showed that screening did not account for the decrease in breast cancer mortality. To what extent could the decrease in mortality be related to other factors such as better prenatal and early childhood diet and life style, improved nutrition, reduction in environmental pollutants, and other unidentified life style and environmental factors which improve immune competence?
A simplistic model to reduce the risk of cancers is described in the following equation (Gorter & Peper, 2011).

Cancer risk can be reduced, arguably by influencing risk factors that contribute to cancers as well as increasing factors to enhance immune competence. In the simple model above, ‘Cancer burden’ refers to the set of exposures that increase the odds of cancer formations. Categories include exposures to oncoviruses, environmental exposures (e.g., ionizing radiation, carcinogenic chemicals) as well as genetic (e.g., chromosomal aberrations, replication errors) and epigenetic factors (e.g., lifestyle categories related to eating, exercising, sleeping, and relaxing). In the model above, ‘Immune competence’ refers to a set of categories of immune functioning related to DNA repair, orderly cell death (i.e., processes of apoptosis), expected autophagy, as well as ‘metabolic rewiring,’ also called cellular energetics, that would allow the body to be able to reduce manage cancers from progressing (Fouad & Aanei, 2017) .
How do we examine the cancer burden/immune competence relationship?
Schmutzler et al., (2022) have suggested personalized and precision-medicine risk-adjusted cancer screening incorporating “… high-throughput “multi-omics” technologies comprising, among others, genomics, transcriptomics, and proteomics, which have led to the discovery of new molecular risk factors that seem to interact with each other and with non-genetic risk factors in a multiplicative manner.” The argument is that ‘profit-centered’ medicine could incorporate ‘multi-omics’ into risk-adjusted cancer screening as a way to reduce potential loss or harm due to other cancer screening procedures. Rather than simply screening for cancers using currently invasive or toxic procedures which may do more harm than good, consider more nuanced screening tests aimed at the so-called ‘hallmarks of cancer?’ For example, Hanahan (2022) suggests some technical targets for the multi-omics technologies. The following are some of the precision screening tests possible topersonalized medicine of 14 factors or processes related to:
- cells evading growth suppression
- non-mutational epigenetic reprogramming
- avoiding immune destruction
- enabling replicative immortality
- tumor-promoting inflammation
- polymorphic microbiomes
- activating invasion and metastasis
- inducing or accessing vasculature formation/angiogenesis
- cellular senescence
- genome instability and mutation
- resisting cell death
- deregulating cellular metabolism
- unlocking phenotypic plasticity
- sustaining proliferative signaling
Of the listed categories above, ‘phenotypic plasticity’ (cf. Feinberg, 2007; Gupta et al., 2019) suggests that lifestyle behaviors and environmental exposures play a role in cancer progression and regression.
Lifestyle and environmental factors can contribute to the development of cancers.
The 2008-2009 report from the President’s Cancer Panel appraised the National Cancer Program in accordance with the National Cancer Act of 1971 stated (Reuben, 2010):
“We have grossly underestimated the link between environmental toxins, plastics, chemicals, and cancer risk. It is estimated that 70 percent of all cancers were related to diet and environment “
Multiple research studies have shown that a healthy life style pattern is associated with decreased cancer risks and increased longevity. Lifestyle factors that have been documented to increase cancer risks in the United Kingdom (UK) as shown in figure 2.
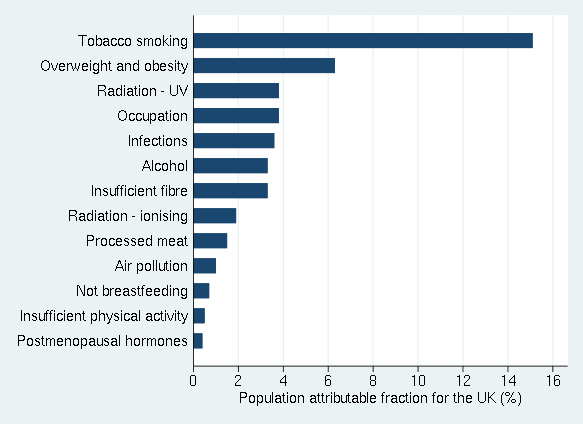
Figure 2. Percentages of cancer cases in the UK attributable to different exposures. Adapted from Brown et al., 2018 and reproduced by permission from Key et al., 2020.
Similar findings have been reported by Song et al. (2016) from the long term follow-up of 126901 adult health care professionals. People who never smoked, drank no alcohol or moderate alcohol (< 1 drink/d for women; < 2 drinks/d for men}, had a body-mass index (BMI) of at least 18.t but lower than 27.5, did weekly aerobic physical activity of at least 75 vigorous-intensity minutes or 150 150 moderate-intensity minutes compared to those who smoked, drank, had high BMI and did not exercise had nearly half the cancer death rate. Song et al (2016) concludes:
“…about 20% to 40% of carcinoma cases and about half of carcinoma deaths can be potentially prevented through lifestyle modification. Not surprisingly, these figures increased to 40% to 70% when assessed with regard to the population of US whites which has a much worse lifestyle pattern than other cohorts. Notably, approximately 80% to 90% of lung cancer deaths can be avoided if Americans adopted the lifestyle of the low-risk group, mainly by quitting smoking. For other cancers, a range of 10% to 70% of deaths can be prevented. These results provide strong support for the importance of environmental factors in cancer risk and reinforce the enormous potential of primary prevention for cancer control.”
Said another way, primary prevention should remain a priority for cancer control.
Given that many cancers are related to diet, environment and lifestyle, it is estimated that 50% of all cancers and cancer deaths could be prevented by modifying personal behavior. Thus, the monies spent on screening or even developing new treatments could better be spent on prevention along with implementing programs that promote a healthier environment, diet and personal behavior (AACR, 2011).
What can be done? Addressing systems not symptoms
From a ‘systems perspective,’ the first step is to reduce the cancer burden and carcinogenic agents that occur in our environment such environmental pollution (Turner et al., 2022). In many cases, governmental regulations that reduce cancer risk factors have been weakened, delayed, and contested for years through industry’s lobbying. It often takes more than 30 years after risk factors have been observed and documented before government regulations are successfully implemented, as exemplified in the battle over tobacco or, air pollution regulations related to particulates from burning fossil fuels (Stratton et al, 2001).
Sadly, we cannot depend upon governments or industries to implement regulations known to reduce cancer risks. More within our control is implementing lifestyle changes that enhance immune competence and promote health.
Implement a healthy life style that enhances immune competence and, supports health and well-being
Paraphrasing a trope of what some physicians may state: ‘Take two pills, and call me in the morning. Oh, and eat well, exercise, and get good rest.’ Broadly stated, the following are some controllable lifestyle behaviors that can decrease cancer risks and promotes health. Implementing environmental and lifestyle changes are very challenging because they are highly related to socio economic factors, cultural factors, industry push for profits over health, and self-care challenges since there are no immediate results experienced by behavior and lifestyle changes.
In many cases, the effects of harmful life-style and environment factors are only observed twenty or more years later (e.g., diabetes, lung cancer, cirrhosis of the liver). The individual does not experience immediate benefits of lifestyle changes thus it is more challenging to know that your healthy life style has an effect. The process is even more complex because in most cases it is not a single factor but the interaction of multiple factors (genetics, lifestyle, and environment). The complexity of causality so often conflicts with the simplistic research studies to identify only one isolated risk factor. Instead of waiting for the definitive governmental guidelines and regulations, adopt a ‘precautionary principle’ which means do not take an action when there is uncertainty about its potential harm (Goldstein, 2001). Do not wait for screening; instead, take charge of your health and implement as many of the following behaviors and strategies to enhance immune competence and thereby reduce cancer risks.
Eat organic foods, especially vegetable and fruits.
Many studies have suggested that eating organic foods and in particular more fruits and vegetable such as a Mediterranean diet is associated with increased health and longevity. Similarly, people who eat do not eat highly-processed or ultra-processed foods have better health status (Van Tulleken, 2023). For example, In the large prospective study of 68, 946 participants, adults who consumed the most organic fruits, vegetables, dairy products, meat and other foods had 25% fewer cancers when compared with adults who never ate organic food (Baudry et al., 2018; Rabin, 2018). Similarly, many studies have reported that those who adhere consistently to a Mediterranean diet have a significantly lower incidence of chronic diseases (such as cardiovascular diseases, diabetes, etc.) and cancers compared to those who do not adhere to a Mediterranean diet (Mentella et al., 2019).
Reduce environmental pollution exposure
Air pollution and the exposure to airborne carcinogens are a significant risk factor for cancers as illustrated by the increased cancer rates among smokers. In the USA, the reduction of smoking has significantly decreased the lung cancer deaths (US Department of Health and Human Services, 2014).
Increase movement and exercise
Many studies have documented that people who exercise regularly and are otherwise non–sedentary but are active their entire lives have the lowest risk for breast cancers and colon cancers. Women who exercise 3 hours a week or more have a 30-40% lower risk of developing breast cancer (NIH NCI, 2023). The NIH National Cancer Institute summary concludes that exercises also significantly benefited the following cancer survivors (NIH NCI, 2023):
- Breast cancer: In a 2019 systematic review and meta-analysis of observational studies, breast cancer survivors who were the most physically active had a 42% lower risk of death from any cause and a 40% lower risk of death from breast cancer than those who were the least physically active (Spei et al, 2019).
- Colorectal cancer: Evidence from multiple epidemiologic studies suggests that physical activity after a colorectal cancer diagnosis is associated with a 30% lower risk of death from colorectal cancer and a 38% lower risk of death from any cause (Patel et al., 2019).
- Prostate cancer: Limited evidence from a few epidemiologic studies suggests that physical activity after a prostate cancer diagnosis is associated with a 33% lower risk of death from prostate cancer and a 45% lower risk of death from any cause ((Patel et al., 2019).
- Implement stress management.
Chronic stress may reduce immune competence and increase the risk of cancers as well as hinders healing from cancer treatments (Dai et al., 2020). The results of numerous studies have shown that implementing stress management spractices uch as Cognitive-behavioral stress management (CBSM) improves mood and lowers distress during treatment and, is also associated with longer survival compared to control groups in the 8-15 year follow up (Stagl et al., 2015).
Respect your biological rhythm.
The International Agency for Research on Cancer (IARC) reports that, when the human circadian clock is disrupted, the likelihood of developing cancers, including lung cancers, intestinal cancers, and breast cancers, dramatically increases (Huang, et al., 2023). Go to bed at the same time and, have about 8 hours of sleep. As much as possible avoid night shifts at work along with frequent jet lag as that highly disrupts the circadian rhythm.
Increase social connections and be part of a social community
Absence of social support, feeling lonely and socially isolated tends reduces immune competence and increases cancer mortality risk while having more social support satisfaction is associated with lower mortality risks (Salazaor et al., 2023; Boen et al., 2018). Meta-analysis of 148 studies (308,849 participants) found that that on the average there is a 50% increased likelihood of survival for participants with stronger social relationships (Holt-Lunstad et al., 2010).
Live a life with meaning and purpose
Having meaning and purpose make each moment worth living and may contribute to improving immune function and possible cancer survival (LeShan, 1994; Rosenbaum & Rosenbaum, 2023).
Summary
The research suggests that cancer screening does not extend life span unless specifically performed for certain diagnostic purposes or, with individuals who are at high risk of developing cancers (e.g., have a genetic predisposition). Implementing self-care health behaviors that have been identified to promote health and increase lifespan. Implementing health behaviors is challenging since there is limited governmental and corporate support. Thus, take charge and implement a holistic self-care lifestyle that reduces cancer risk factors and supports health.
See also the following blogs:
References
AACR. (2011). AACR Cancer Progress Report 2011. American Association for Cancer Research. http://www.aacr.org/Uploads/DocumentRepository/2011CPR/2011_AACR_CPR_Text_web.pdf
American Cancer Society. (2021). History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms. Accessed November 11, 2023. https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/overview/chronological-history-of-acs-recommendations.html
Autier, P., Boniol, M., Gavin, A,, & Vatten, L.J. (2011) Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ. 343, d4411. https://doi.org/10.1136/bmj.d4411
Badal., K., Staib, J., Tice,J., Kim, M-O., Eklund, M., DaCosta Byfield, S., Catlett,K., Wilson,L., et al, (2023). Cost of breast cancer screening in the USA: Comparison of current practice, advocated guidelines, and a personalized risk-based approach. Journal of Clinical Oncology, 41: 16_suppl, 3 18917 :16_suppl, e18917. https://doi.org/10.1200/JCO.2023.41.16_suppl.e18917
Baudry, J., Assmann, K.E., Touvier, M., et al. (2018). Association of Frequency of Organic Food Consumption With Cancer Risk: Findings From the NutriNet-Santé Prospective Cohort Study. JAMA Intern Med, 178(12), 1597–1606. https://doi.org/10.1001/jamainternmed.2018.4357
Boen, C.E., Barrow, D..A, Bensen, J.T., Farnan, L., Gerstel, A., Hendrix, L.H., Yang, Y.C. (2018). Social Relationships, Inflammation, and Cancer Survival. Cancer. Epidemiol Biomarkers Prev, 27(5), 541-549. https://doi.org/10.1158/1055-9965.EPI-17-0836
Bretthauer M, Wieszczy P, Løberg M, et al. (2023). Estimated Lifetime Gained With Cancer Screening Tests: A Meta-Analysis of Randomized Clinical Trials. JAMA Intern Med. 183(11),1196–1203. https://doi.org/10.1001/jamainternmed.2023.3798Brown, K.F., Rumgay, H., Dunlop, C. et al. (2018). The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer, 118, 1130–1141. https://doi.org/10.1038/s41416-018-0029-6
CDC. (2023a). U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2022 submission data (1999-2020): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; released in November 2023. https://www.cdc.gov/cancer/dataviz
CDC. (2023b). Leading Causes of Death. National Center for health statistics, Centers for disease control and prevention. Accessed November 20, 2023. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
CSPH. (2021). Estimating annual expenditures for cancer screening in the United States. Center for Surgery and Public Health. Assessed November 14, 2023. https://csph.brighamandwomens.org/wp-content/uploads/2021/12/Estimating-Annual-Expenditures-for-Cancer-Screening-in-the-United-States.pdf
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., Li, X., Li, Y., Xiong. W., Li, G., Guo, C., & Zeng, Z. (2020). Chronic Stress Promotes Cancer Development. Front Oncol. 10, 1492. https://doi.org/10.3389/fonc.2020.01492
Feinberg, A. P. (2007). Phenotypic plasticity and the epigenetics of human disease. Nature, 447(7143), 433-440. https://doi.org/10.1038/nature05919
Fouad, Y. A., & Aanei, C. (2017). Revisiting the hallmarks of cancer. American journal of cancer research, 7(5), 1016. https://pubmed.ncbi.nlm.nih.gov/28560055/
Fracheboud, J. et al. (2004). Decreased rates of advanced breast cancer due to mammography screening in The Netherlands, British Journal of Cancer (2004) 91, 861–867. https://doi,org/10.1038/sj.bjc.6602075
Goldstein, B.D. (2001). The precautionary principle also applies to public health actions. Am J Public Health, 91(9),1358-61. https://doi.org/10.2105/ajph.91.9.1358
Gorter, R. & Peper, E. (2011). Fighting Cancer-A None Toxic Approach to Treatment. Berkeley: North Atlantic/New York: Random House. https://www.amazon.com/Fighting-Cancer-Nontoxic-Approach-Treatment/dp/1583942483
Gupta, P. B., Pastushenko, I., Skibinski, A., Blanpain, C., & Kuperwasser, C. (2019). Phenotypic plasticity: driver of cancer initiation, progression, and therapy resistance. Cell Stem Cell, 24(1), 65-78. https://doi.org/10.1016/j.stem.2018.11.011
Hanahan, Douglas. (2022): Hallmarks of cancer: new dimensions. Cancer discovery, 12(1), 31-46. https://doi.org/10.1158/2159-8290.CD-21-1059
Holt-Lunstad, J., Smith, T.B., & Layton, J.B. (2010). Social Relationships and Mortality Risk: A Meta-analytic Review, PLoS Med 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316
Huang, C., Zhang, C,, Cao, Y., Li, J., & Bi, F. (2023). Major roles of the circadian clock in cancer. Cancer Biol Med, 20(1):1–24. https://doi.org/10.20892/j.issn.2095-3941.2022.0474
Kalaf, J.M. (2014). Mammography: a history of success and scientific enthusiasm. Radiol Bras. 47(4):VII-VIII. https://doi.org/10.1590/0100-3984.2014.47.4e2
Key TJ, Bradbury KE, Perez-Cornago A, Sinha R, Tsilidis KK, Tsugane S. Diet, nutrition, and cancer risk: what do we know and what is the way forward? BMJ. 2020 Mar 5;368:m511. https://doi.org/10.1136/bmj.m511
Kowalski, A.E. (2021). Mammograms and mortality: How has the evidence evolved? J Econ Perspect, 35(2), 119-140. https://doi.org/10.1257/jep.35.2.119
LeShan, L. (1994). Cancer as a turning point. New York: Plume. https://www.amazon.com/Cancer-As-Turning-Point-Professionals/dp/0452271371
Lewis, T. (2022). The U.S. just lost 26 years’ worth of progress on life expectancy. Scientific American. October 17, 2022. Accessed November 11, 2023. https://www.scientificamerican.com/article/the-u-s-just-lost-26-years-worth-of-progress-on-life-expectancy/
Ma, X., Wang, R., Long, J.B., Ross, J.S., Soulos, P.R., Yu, J.B., Makarov, D.V., Gold, H.T. and Gross, C.P. (2014), The cost implications of prostate cancer screening in the Medicare population. Cancer, 120: 96-102. https://doi.org/10.1002/cncr.28373
Mentella, M.C., Scaldaferri, F., Ricci, C., Gasbarrini, A., & Miggiano, G.A.D. (2019). Cancer and Mediterranean Diet: A Review. Nutrients,11(9):2059. https://doi.org/10.3390/nu11092059
NIH NCI (2023). Physical Activity and Cancer. National Institutes of Health National Cancer Institute. Accessed November 18, 2023. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/physical-activity-fact-sheet
Patel, A,V., Friedenreich, C.M., Moore, S.C, et al. (2019). American College of Sports Medicine Roundtable Report on physical activity, sedentary behavior, and cancer prevention and control. Medicine and Science in Sports and Exercise, 51(11), 2391-2402. https://doi.org/10.1249/MSS.0000000000002117
Rabin, R.C. (2018). Can eating organic food lower your cancer risk? The New York Times. Oct 23, 2018. Accessed November 17, 2023. https://www.nytimes.com/2018/10/23/well/eat/can-eating-organic-food-lower-your-cancer-risk.html
Reuben, S.H. (2010). Reducing environmental cancer risk – What We Can Do Now. The President’s Cancer Panel Report. Washington, D.C: U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES, National Institutes of Health, National Cancer Institute. https://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp08-09rpt/PCP_Report_08-09_508.pdf
Rosenbaum, E. H. & Rosenbaum, I.R. (2023) The Will to Live. Stanford Center for Integrative Medicine. Surviving Cancer. Accessed November 23, 2023. https://med.stanford.edu/survivingcancer/cancers-existential-questions/cancer-will-to-live.html
Salazar, S.M.D.C., Dino, M.J.S., & Macindo, J.R.B. (2023). Social connectedness and health-related quality of life among patients with cancer undergoing chemotherapy: a mixed method approach using structural equation modelling and photo-elicitation. J Clin Nurs. Published online March 9, 2023. https://doi.org/10.1111/jocn.16675
Schmutzler, R. K., Schmitz-Luhn, B., Borisch, B., Devilee, P., Eccles, D., Hall, P., … & Woopen, C. (2022). Risk-adjusted cancer screening and prevention (RiskAP): complementing screening for early disease detection by a learning screening based on risk factors. Breast Care, 17(2), 208-223. https://doi.org/10.1159/000517182
Song, M., & Giovannucci, E. (2016). Preventable incidence and mortality of carcinoma associated with lifestyle factors among white adults in the United States. JAMA Ooncology, 2(9), 1154-1161. https://doi.org/10.1001/jamaoncol.2016.0843
Spei, M.E., Samoli, E., Bravi, F., et al. (2019). Physical activity in breast cancer survivors: A systematic review and meta-analysis on overall and breast cancer survival. Breast, 44,144-152. https://doi.org/10.1016/j.breast.2019.02.001
Stagl, J.M., Lechner, S.C., Carver, C.S. et al. (2015). A randomized controlled trial of cognitive-behavioral stress management in breast cancer: survival and recurrence at 11-year follow-up. Breast Cancer Res Treat, 154, 319–328. https://doi.org/10.1007/s10549-015-3626-6
Stratton, K., Shetty, P., Wallace, R., et al., eds. (2001). Institute of Medicine (US) Committee to Assess the Science Base for Tobacco Harm Reduction. Washington (DC): National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK222369/
Tailor, T.D,, Bell, S., Fendrick, A.M., & Carlos, R.C. (2022) Total and Out-of-Pocket Costs of Procedures After Lung Cancer Screening in a National Commercially Insured Population: Estimating an Episode of Care. J Am Coll Radiol. 19(1 Pt A), 35-46. https://doi.org/10.1016/j.jacr.2021.09.015
Turner, M.C., Andersen, Z.J., Baccarelli, A., Diver, W.R., Gapstur, S.M., Pope, C.A 3rd, Prada, D., Samet, J., Thurston, G., & Cohen, A. (2020). Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J Clin, 10.3322/caac.21632. https://doi.org/10.3322/caac.21632
US Department of Health and Human Services (2014). The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: :
US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. https://aahb.org/Resources/Pictures/Meetings/2014-Charleston/PPT%20Presentations/Sunday%20Welcome/Abrams.AAHB.3.13.v1.o.pdf
Van Tulleken, C. (2023). Ultra-processed people. The science behind food that isn’t food. New Yoerk: W.W. Norton & Company. https://www.amazon.com/gp/product/1324036729/ref=ox_sc_act_title_1?smid=ATVPDKIKX0DER&psc=1
TechStress: Building Healthier Computer Habits
Posted: August 30, 2023 Filed under: ADHD, behavior, biofeedback, Breathing/respiration, cognitive behavior therapy, computer, digital devices, education, emotions, ergonomics, Evolutionary perspective, Exercise/movement, health, laptops, Neck and shoulder discomfort, Pain/discomfort, posture, screen fatigue, stress management, Uncategorized, vision, zoom fatigue | Tags: cellphone, fatigue, gaming, mobile devices, screens 2 CommentsBy Erik Peper, PhD, BCB, Richard Harvey, PhD, and Nancy Faass, MSW, MPH
Adapted by the Well Being Journal, 32(4), 30-35. from the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics by Erik Peper, Richard Harvey, and Nancy Faass.

Every year, millions of office workers in the United States develop occupational injuries from poor computer habits—from carpal tunnel syndrome and tension headaches to repetitive strain injury, such as “mouse shoulder.” You’d think that an office job would be safer than factory work, but the truth is that many of these conditions are associated with a deskbound workstyle.
Back problems are not simply an issue for workers doing physical labor. Currently, the people at greatest risk of injury are those with a desk job earning over $70,000 annually. Globally, computer-related disorders continue to be on the rise. These conditions can affect people of all ages who spend long hours at a computer and digital devices.
In a large survey of high school students, eighty-five percent experienced tension or pain in their neck, shoulders, back, or wrists after working at the computer. We’re just not designed to sit at a computer all day.
Field of Ergonomics
For the past twenty years, teams of researchers all over the world have been evaluating workplace stress and computer injuries—and how to prevent them. As researchers in the fields of holistic health and ergonomics, we observe how people interact with technology. What makes our work unique is that we assess employees not only by interviewing them and observing behaviors, but also by monitoring physical responses.
Specifically, we measure muscle tension and breathing, in the moment, in real-time, while they work. To record shoulder pain, for example, we place small sensors over different muscles and painlessly measure the muscle tension using an EMG (electromyograph)—a device that is employed by physicians, physical therapists, and researchers. Using this device, we can also keep a record of their responses and compare their reactions over time to determine progress.
What we’ve learned is that people get into trouble if their muscles are held in tension for too long. Working at a computer, especially at a stationary desk, most people maintain low-level chronic tension for much of the day. Shallow, rapid breathing is also typical of fine motor tasks that require concentration, like data entry.
Muscle tension and breathing rate usually increase during data entry or typing without our awareness.
When these patterns are paired with psychological pressure due to office politics or job insecurity, the level of tension and the risk of fatigue, inflammation, pain, or injury increase. In most cases, people are totally unaware of the role that tension plays in injury. Of note, the absolute level of tension does not predict injury—rather, it is the absence of periodic rest breaks throughout the day that seems to correlate with future injuries.
Restbreaks
All of life is the alternation between movement and rest, inhaling and exhaling, sleeping and waking. Performing alternating tasks or different types of activities and movement is one way to interrupt the couch potato syndrome—honoring our evolutionary background.
Our research has confirmed what others have observed: that it’s important to be physically active, at least periodically, throughout the day. Alternating activity and rest recreate the pattern of our ancestors’ daily lives. When we alternate sedentary tasks with physical activity, and follow work with relaxation, we function much more efficiently. In short, move your body more.
Better Computer Habits: Alternate Periods of Rest and Activity
As mentioned earlier, our workstyle puts us out of sync with our genetic heritage. Whether hunting and gathering or building and harvesting, our ancestors alternated periods of inactivity with physical tasks that required walking, running, jumping, climbing, digging, lifting, and carrying, to name a few activities. In contrast, today many of us have a workstyle that is so immobile we may not even leave our desk for lunch.
As health researchers, we have had the chance to study workstyles all over the world. Back pain and strain injuries now affect a large proportion of office workers in the US and in high-tech firms worldwide. The vast majority of these jobs are sedentary, so one focus of the research is on how to achieve a more balanced way of working.
A recent study on exercise looked at blood flow to the brain. Researchers Carter and colleagues found that if people sit for four hours on the job, there’s a significant decrease in blood flow to the brain. However, if every thirty or forty minutes they get up and move around for just two minutes, then brain blood flow remains steady. The more often you interrupt sitting with movement, the better.
It may seem obvious that to stay healthy, it’s important to take breaks and be physically active from time to time throughout the day. Alternating activity and rest recreate the pattern of our ancestors’ daily lives. The goal is to alternate sedentary tasks with physical activity and follow work with relaxation. When we keep this type of balance going, most people find that they have more energy, are more productive, and can be more effective.
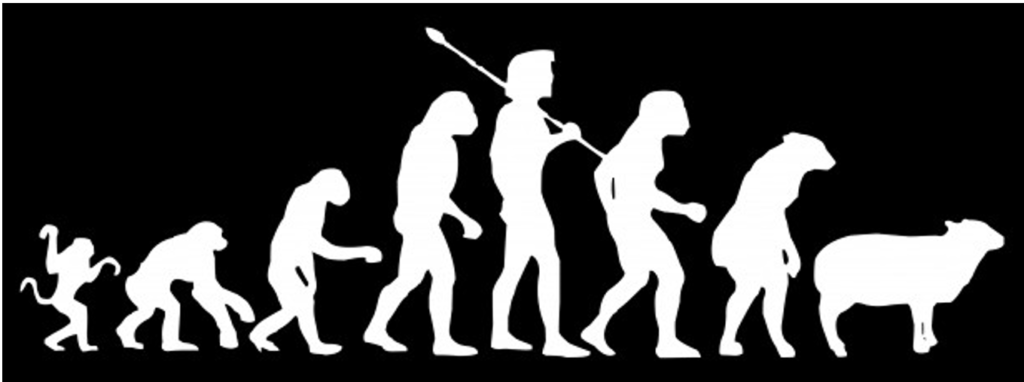
Genetics: We’re Hardwired Like Ancient Hunters
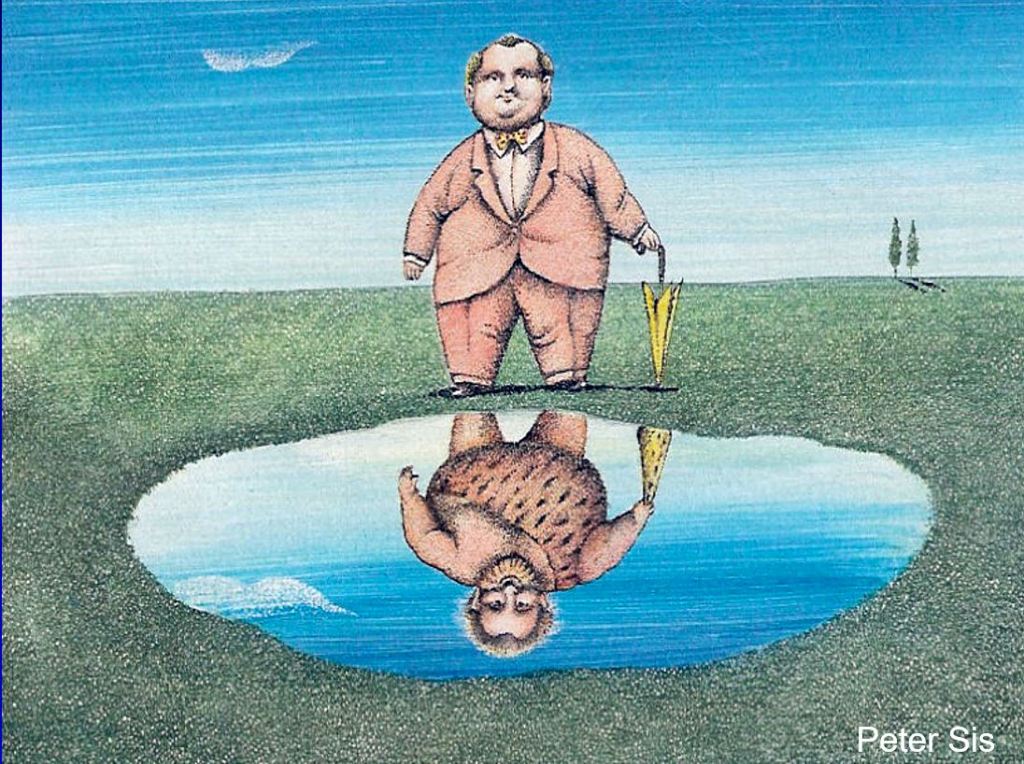
Despite a modern appearance, we carry the genes of our forebearers—for better and for worse. (Art courtesy of Peter Sis). Reproduced from Peper, E., Harvey, R., & Faass (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
In the modern workplace, most of us find ourselves working indoors, in small office spaces, often sitting at a computer for hours at a time. In fact, the average Westerner spends more than nine hours per day sitting indoors, yet we’re still genetically programmed to be physically active and spend time outside in the sunlight most of the day, like the nomadic hunters and gatherers of forty thousand years ago.
Undeniably, we inherently conserve energy in order to heal and regenerate. This aspect of our genetic makeup also helps burn fewer calories when food is scarce. Hence the propensity for lack of movement and sedentary lifestyle (sitting disease).
In times of famine, the habit of sitting was essential because it reduced calorie expenditure, so it enabled our ancestors to survive. In a prehistoric world with a limited food supply, less movement meant fewer calories burned. Early humans became active when they needed to search for food or shelter. Today, in a world where food and shelter are abundant for most Westerners, there is no intrinsic drive to initiate movement.
It is also true that we have survived as a species by staying active. Chronic sitting is the opposite of our evolutionary pattern in which our ancestors alternated frequent movement while hunting or gathering food with periods of rest. Whether they were hunters or farmers, movement has always been an integral aspect of daily life. In contrast, working at the computer—maintaining static posture for hours on end—can increase fatigue, muscle tension, back strain, and poor circulation, putting us at risk of injury.
Quit a Sedentary Workstyle
Almost everyone is surprised by how quickly tension can build up in a muscle, and how painful it can become. For example, we tend to hover our hands over the keyboard without providing a chance for them to relax. Similarly, we may tighten some of the big muscles of our body, such as bracing or crossing our legs.
What’s needed is a chance to move a little every few minutes—we can achieve this right where we sit by developing the habit of microbreaks. Without regular movement, our muscles can become stiff and uncomfortable. When we don’t take breaks from static muscle tension, our muscles don’t have a chance to regenerate and circulate oxygen and necessary nutrients.
Build a variety of breaks into your workday:
- Vary work tasks
- Take microbreaks (brief breaks of less than thirty seconds)
- Take one-minute stretch breaks
- Fit in a moving break
Varying Work Tasks
You can boost physical activity at work by intentionally leaving your phone on the other side of the desk, situating the printer across the room, or using a sit-stand desk for part of the day. Even a few minutes away from the desk makes a difference, whether you are hand delivering documents, taking the long way to the bathroom, or pacing the room while on a call.
When you alternate the types of tasks and movement you do, using a different set of muscles, this interrupts the contractions of muscle fibers and allows them to relax and regenerate. Try any of these strategies:
- Alternate computer work with other activities, such as offering to do a coffee run
- Schedule walking meetings with coworkers
- Vary keyboarding and hand movements
Ultimately, vary your activities and movements as much as possible. By changing your posture and making sure you move, you’ll find that your circulation and your energy improve, and you’ll experience fewer aches and pains. In a short time, it usually becomes second nature to vary your activities throughout the day.
Experience It: “Mouse Shoulder” Test
You can test this simple mousing exercise at the computer or as a simulation. If you’re at the computer, sit erect with your hand on the mouse next to the keyboard. To simulate the exercise, sit with erect posture as if you were in front of your computer and hold a small object you can use to imitate mousing.
With the mouse (or a sham mouse), simulate drawing the letters of your name and your street address, right to left. Be sure each letter is very small (less than half an inch in height). After drawing each letter, click the mouse.
As part of the exercise, draw the letters and numbers as quickly as possible for ten to fifteen seconds. What did you observe? In almost all cases, you may note that you tightened your mousing shoulder and your neck, stiffened your trunk, and held your breath. All this occurred without awareness while performing the task. Over time, this type of muscle tension can contribute to discomfort, soreness, pain, or eventual injury.
Microbreaks
If you’ve developed an injury—or have chronic aches and pains—you’ll probably find split-second microbreaks invaluable. A microbreak means taking brief periods of time that last just a few seconds to relax the tension in your wrists, shoulders, and neck.
For example, when typing, simply letting your wrists drop to your lap for a few seconds will allow the circulation to return fully to help regenerate the muscles. The goal is to develop a habit that is part of your routine and becomes automatic, like driving a car. To make the habit of microbreaks practical, think about how you can build the breaks into your workstyle. That could mean a brief pause after you’ve completed a task, entered a column of data, or before starting typing out an assignment.
For frequent microbreaks, you don’t even need to get up—just drop your hands in your lap or shake them out, move your shoulders, and then resume work. Any type of shaking or wiggling movement is good for your circulation and kind of fun.
In general, a microbreak may be defined as lasting one to thirty seconds. A minibreak may last roughly thirty seconds to a few minutes, and longer large-movement breaks are usually greater than a few minutes. Popular microbreaks:
- Take a few deep breaths
- Pause to take a sip of water
- Rest your hands in your lap
- Stretch
- Let your arms drop to your sides
- Shake out your hands (wrists and fingers)
- Perform a quick shoulder or neck roll
Often, we don’t realize how much tension we’ve been carrying until we become more mindful of it. We can raise our awareness of excess tension—this is a learned skill—and train ourselves to let go of excess muscle tension. As we increase our awareness, we’re able to develop a new, more dynamic workstyle that better fits our goals and schedule.
One-Minute Stretch Breaks

We all benefit from a brief break, even with the best of posture (left). One approach is to totally release your muscles (middle). That release can be paired with a series of brief stretches (right). Reproduced from Peper, E., Harvey, R., & Faass (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
The typical mini-stretch break lasts from thirty seconds to a few minutes, and ideally you want to take them several times per hour. Similar to microbreaks, mini-stretch breaks are especially important for people with an injury or those at risk of injury. Taking breaks is vital, especially if you have symptoms related to computer stress or whenever you’re working long hours at a sedentary job. To take a stretch break:
Begin with a big stretch, for example, by reaching high over your head then drop your hands in your lap or to your sides.
Look away from the monitor, staring at near and far objects, and blink several times. Straighten your back and stretch your entire backbone by lifting your head and neck gently, as if there were an invisible string attached to the crown of your head.
Stretch your mind and body. Sitting with your back straight and both feet flat on the floor, close your eyes and listen to the sounds around you, including the fan on the computer, footsteps in the hallway, or the sounds in the street.
Breathe in and out over ten seconds (breathe in for four or five seconds and breathe out for five or six seconds), making the exhale slightly longer than the inhale. Feel your jaw, mouth, and tongue muscles relax. Feel the back and bottom of the chair as your body breathes all around you. Envision someone in your mind’s eye who is kind and reassuring, who makes you feel safe and loved, and who can bring a smile to your face inwardly or outwardly.
Do a wiggling movement. When you take a one-minute break, wiggling exercises are fast and easy, and especially good for muscle tension or wrist pain. Wiggle all over—it feels good, and it’s also a great way to improve circulation.
Building Exercise and Movement into Every Day
Studies show that you get more benefit from exercising ten to twenty minutes, three times a day, than from exercising for thirty to sixty minutes once a day. The implication is that doing physical activities for even a few minutes can make a big difference.
Dunstan and colleagues have found that standing up three times an hour and then walking for just two minutes reduced blood sugar and insulin spikes by twenty-five percent.Fit in a Moving Break
Fit in a Moving Break
Once we become conscious of muscle tension, we may be able to reverse it simply by stepping away from the desk for a few minutes, and also by taking brief breaks more often. Explore ways to walk in the morning, during lunch break, or right after work. Ideally, you also want to get up and move around for about five minutes every hour.
Ultimately, research makes it clear that intermittent movement, such as brief, frequent stretching throughout the day or using the stairs rather than elevator, is more beneficial than cramming in a couple of hours at the gym on the weekend. This explains why small changes can have a big impact—it’s simply a matter of reminding yourself that it’s worth the effort.
Workstation Tips
Your ability to see the display and read the screen is key to reducing neck and eye strain. Here are a few strategic factors to remember:
Monitor height: Adjust the height of your monitor so the top is at eyebrow level, so you can look straight ahead at the screen.
Keyboard height: The keyboard height should be set so that your upper arms hang straight down while your elbows are bent at a 90-degree angle (like the letter L) with your forearms and wrists held horizontally.
Typeface and font size: For email, word processing, or web content, consider using a sans serif typeface. Fonts that have fewer curved lines and flourishes (serifs) tend to be more readable on screen.
Checking your vision: Many adults benefit from computer glasses to see the screen more clearly. Generally, we do not recommend reading glasses, bifocals, trifocals, and progressive lenses as they tend to allow clear vision at only one focal length. To see through the near-distance correction of the lens requires you to tilt your head back. Although progressive lenses allow you to see both close up and at a distance, the segment of the lens for each focal length is usually too narrow for working at the computer.
Wearing progressive lenses requires you to hold your head in a fixed position to be in focus. Yet you may be totally unaware that you are adapting your eye and head movements to sustain your focus. When that is the case, most people find that special computer glasses are a good solution.
Consider computer glasses if you must either bring your nose to the screen to read the text, wear reading glasses and find that their focal length is inappropriate for the monitor distance, wear bi- or trifocal glasses, or are older than forty.
Computer glasses correct for the appropriate focal distance to the computer. Typically, monitor distance is about twenty-three to twenty-eight inches, whereas reading glasses correct for a focal length of about fifteen inches. To determine your individual, specific focal length, ask a coworker to measure the distance from the monitor to your eyes. Provide this personal focal distance at the eye exam with your optometrist or ophthalmologist and request that your computer glasses be optimized for that distance.
Remembering to blink: As we focus on the screen, our blinking rate is significantly reduced. Develop the habit of blinking periodically: at the end of a paragraph, for example, or when sending an email.
Resting your eyes: Throughout the day, pause and focus on the far distance to relax your eyes. When looking at the screen, your eyes converge, which can cause eyestrain. Each time you look away and refocus, that allows your eyes to relax. It’s especially soothing to look at green objects such as a tree that can be seen through a window.
Minimizing glare: If the room is lit with artificial light, there may be glare from your light source if the light is right in front of you or right behind you, causing reflection on your screen. Reflection problems are minimized when light sources are at a 90-degree angle to the monitor (with the light coming from the side). The worst situations occur when the light source is either behind or in front of you.
An easy test is to turn off your monitor and look for reflections on the screen. Everything that you see on the monitor when it’s turned off is there when you’re working at the monitor. If there are bright reflections, they will interfere with your vision. Once you’ve identified the source of the glare, change the location of the reflected objects or light sources, or change the location of the monitor.
Contrast: Adjust the light contrast in the room so that it is neither too bright nor too dark. If the room is dark, turn on the lights. If it is too bright, close the blinds or turn off the lights. It is exhausting for your eyes to have to adapt from bright outdoor light to the lighting of your computer screen. You want the light intensity of the screen to be somewhat similar to that in the room where you’re working. You also do not want to look from your screen to a window lit by intense sunlight.
Don’t look down at phone: According to Kenneth Hansraj, MD, chief of spine surgery at New York Spine Surgery and Rehabilitation Medicine, pressure on the spine increases from about ten pounds when you are holding your head erect, to sixty pounds of pressure when you are looking down. Bending forward to look at your phone, your head moves out of the line of gravity and is no longer balanced above your neck and spine. As the angle of the face-forward position increases, this intensifies strain on the neck muscles, nerves, and bones (the vertebrae).
The more you bend your neck, the greater the stress since the muscles must stretch farther and work harder to hold your head up against gravity. This same collapsed head-forward position when you are seated and using the phone repeats the neck and shoulder strain. Muscle strain, tension headaches, or neck pain can result from awkward posture with texting, craning over a tablet (sometimes referred to as the iPad neck), or spending long hours on a laptop.
A face-forward position puts as much as sixty pounds of pressure on the neck muscles and spine.
Repetitive strain of neck vertebrae (the cervical spine), in combination with poor posture, can trigger a neuromuscular syndrome sometimes diagnosed as thoracic outlet syndrome. According to researchers Sharan and colleagues, this syndrome can also result in chronic neck pain, depression, and anxiety.
When you notice negative changes in your mood or energy, or tension in your neck and shoulders, use that as a cue to arch your back and look upward. Think of a positive memory, take a mindful breath, wiggle, or shake out your shoulders if you’d like, and return to the task at hand.
Strengthen your core: If you find it difficult to maintain good posture, you may need to strengthen your core muscles. Fitness and sports that are beneficial for core strength include walking, sprinting, yoga, plank, swimming, and rowing. The most effective way to strengthen your core is through activities that you enjoy.
Final Thoughts
If these ideas resonate with you, consider lifestyle as the first step. We need to build dynamic physical activity into our lives, as well as the lives of our children. Being outside is usually an uplift, so choose to move your body in natural settings whenever possible, whatever form that takes. Being outside is the factor that adds an energetic dimension. Finally, share what you learn, and help others learn and grow from your experiences.
If you spend time in front of a computeror using a mobile device, read the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. It provides practical, easy-to-use solutions for combating the stress and pain many of us experience due to technology use and overuse. The book offers extremely helpful tips for ergonomic use of technology, it
goes way beyond that, offering simple suggestions for improving muscle health that seem obvious once you read them, but would not have thought of yourself: “Why didn’t I think of that?” You will learn about the connection between posture and mood, reasons for and importance of movement breaks, specific movements you can easily perform at your desk, as well as healthier ways to utilize technology in your everyday life.
Additional resources
Are food companies responsible for the epidemic in diabetes, cancer, dementia and chronic disease and do their products need to be regulated like tobacco? Is it time for a class action suit?
Posted: July 15, 2023 Filed under: behavior, cancer, Evolutionary perspective, health, Nutrition/diet, self-healing | Tags: dementia, diabetes, diet, high fructose corn syrup, mortality, obsity, smoking, sugar, ultra-processed foods, UPF 2 CommentsAdapted from: Peper, E. & Harvey, R. (2024). Are Food Companies Responsible for the Epidemic in Diabetes, Cancer, Dementia and Chronic Disease and Do Their Products Need to Be Regulated Like Tobacco? Is It Time for a Class Action Suit? Thownsend Letter-the examiner of alternative medicine. https://www.townsendletter.com/e-letter-26-ultra-processed-foods-and-health-issues/
Erik Peper, PhD and Richard Harvey, PhD

Why are one third of young Americans becoming obese and at risk for diabetes?
Why are heart disease, cancer, and dementias occurring earlier and earlier? Is it genetics, environment, foods, or lifestyle?
Is it individual responsibility or the result of the quest for profits by agribusiness and the food industry?
Like the tobacco industry that sells products regulated because of their public health dangers, is it time for a class action suit against the processed food industry? The argument relates not only to the regulation of toxic or hazardous food ingredients (e.g., carcinogenic or obesogenic chemicals) but also to the regulation of consumer vulnerabilities. Addressing vulnerabilities to tobacco products include regulations such as how cigarette companies may not advertise their products for sale within a certain distance from school grounds.
Is it time to regulate nationally the installation of vending machines on school grounds selling sugar-sweetened beverages? Students have sensitivity to the enticing nature of advertised, and/or conveniently available consumable products such as ‘fast foods’ that are highly processed (e.g., packaged, preserved and practically imperishable). Whereas ‘processed foods’ have some nutritive value, and may technically pass as ‘nutritious’ food, the quality of processed ‘nutrients’ can be called into question. For the purpose of this blog other important questions to raise relate to ingredients which, alone or in combination, may contribute to the onset of or, the acceleration of a variety of chronic health outcomes related to various kinds of cancers, cardiovascular diseases, and diabetes.
It may be an over statement to suggest that processed food companies are directly responsible for the epidemic in diabetes, cancer, dementia and chronic disease and need to be regulated like tobacco. On the other hand, processed food companies should become much more regulated than they are now.
More than 80 years ago, smoking was identified as a significant factor contributing to lung cancer, heart disease and many other disorders. In 1964 the Surgeon Generals’ report officially linked smoking to deaths of cancer and heart disease (United States Public Health Service, 1964). Another 34 years pased before California prohibited smoking in restaurants in 1998 and, eventually inside all public buildings. The harms of smoking tobacco products were well known, yet many years passed with countless deaths and suffering which could have been prevented before regulation of tobacco products took place. Reviewing historical data there is about a 20 year delay (e.g., a whole generation) before death rates decrease in relation to when regulations became effective and smoking rates decreased, as shown in figure 1.
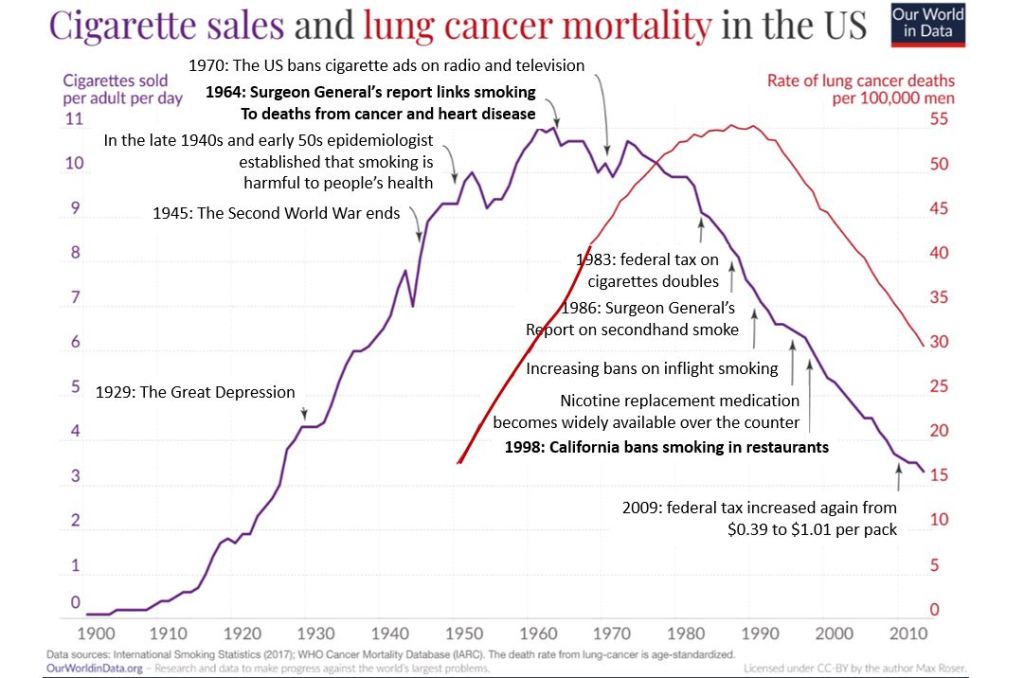
Figure 1. The relationship between smoking and lung cancer. Reproduced by permission from Roser, M. (2021). Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data.
During those interim years before government actions limited smoking more effectively, tobacco companies hid data regarding the harmful effects of smoking. Arguably, the ‘Big Tobacco’ industry paid researchers to publish data which could confuse readers about tobacco product harm. There is evidence of some published articles suggesting that the harm of cigarette smoking was a hoax– all for the sake of boosting corporate profits (Bero, 2005).
Now we are experiencing a similar problem with the processed food industry. It has been suggested that alongside smoking and vaping, opioid use, a sedentary ‘couch potato’ lifestyle, and lack of exercise, ultra-processed food (UPF) that we eat severely affects our health.
Ultra-processed foods, which for many constitutes a majority of calories ranging from 55% to over 80% of the food they eat, contain chemical additives that trick the tastebuds, mouth and eventually our brain to desire those processed foods and eat more of them (Srour et al., 2022).
What are ultra-processed foods? Any foods that your great grandmother would not recognize as food. This includes all soft drinks, highly processed chips, additives, food coloring, stabilizers, processed proteins, etc. Even oils such as palm oil, canola oil, or soybean are ultra processed since they heated, highly processed with phosphoric acid to remove gums and waxes, neutralized with chemicals, bleached, and deodorized with high pressure steam (van Tulleken, 2023).
The data is clear! Since the 1970s obesity and inflammatory disease have exploded after ultra-processed foods became the constituents of the modern diet as shown in figure 2.
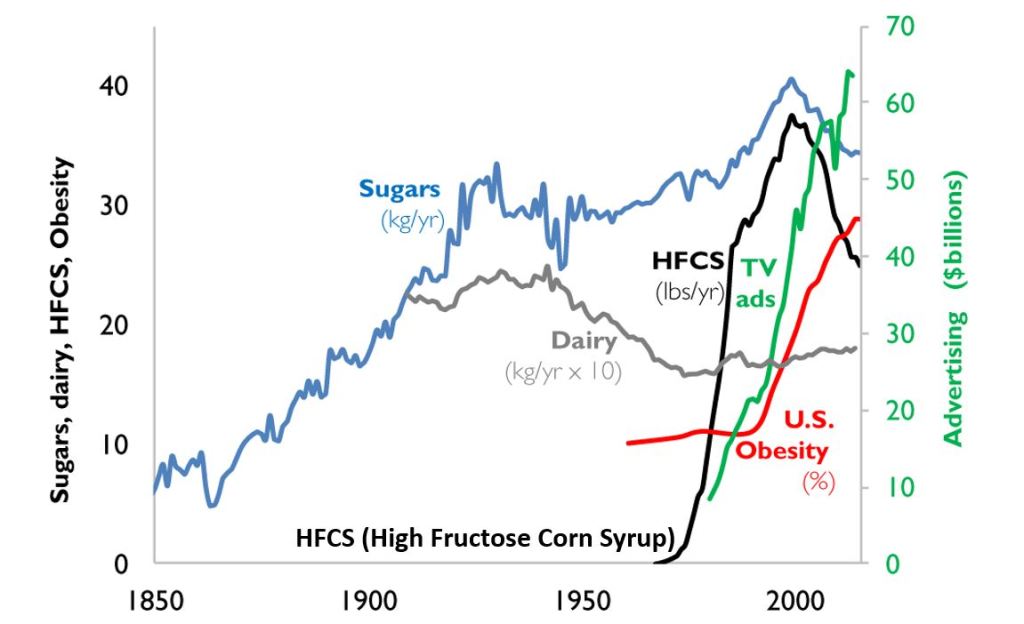
Figure 2. A timeline from 1850 to 2000 reflects the increase in use of refined sugar and high fructose corn syrup (HFCS) to the U.S. diet, together with the increase in U.S. obesity rate. The data for sugar, dairy and HFCS consumption per capita are from USDA Economic Research Service (Johnson et al., 2009) and reflects historical estimates before 1967 (Guyenet et al., 2017). The obesity data (% of U.S. adult population) are from the Robert Wood Johnson Foundation’s Trust for America’s Health. (stateofobesity.org). Total U.S. television advertising data are from the World Advertising Research Center (www.warc.com). The vertical measure (y–axis) for kilograms per year (kg/yr) on the left covers all data except advertising expenditures, which uses the vertical measure for advertising on the right. Reproduced by permission from Bentley et al, 2018.
This graph clearly shows a close association between the years that high fructose corn syrups (HFCS) were introduced into the American diet and an increase in TV advertising with corresponding increase in obesity. HFCS is an ultra-processed food and is a surrogate marker for all other ultra-processed foods. The best interpretation is that ultra-processed foods, which often contain HFCS, are a causal factor of the increase in obesity, and diabetes and in turn are risk factors for heart disease, cancers and dementias.
Ultra-processed foods are novel from an evolutionary perspective.
The human digestive system has only recently encountered sources of calories which are filled with so many unnatural chemicals, textures and flavors. Ultra-processed foods have been engineered, developed and product tested to increase the likelihood they are wanted by consumers and thereby increase sales and profits for the producers. These foods contain the ‘right amount’ processed materials to evoke the taste, flavor and feel of desired foods that ‘trick’ the consumer it eat them because they activate evolutionary preference for survival. Thus, these ultra-processed foods have become an ‘evolutionary trap’ where it is almost impossible not to eat them. We eat the food because it capitalized on our evolutionary preferences even though doing so is ultimately harmful for our health (for a detailed discussion on evolutionary traps, see Peper, Harvey & Faass, 2020).
An example is a young child wanting the candy while waiting with her parents at the supermarket checkout line. The advertised images of sweet foods trigger the cue to eat. Remember, breast milk is sweet and most foods in nature that are sweet in taste, provide calories for growth and survival and are not harmful. Calories are essential of growth. Thus, we have no intrinsic limit on eating sweets unlike foods that taste bitter.
As parents, we wish that our children (and even adults) have self-control and no desire to eat the candy or snacks that is displayed at eye level (eye candy) especially while waiting at the cashier. When reflecting about food advertising and the promotion of foods that are formulated to take advantage of ‘evolutionary traps’, who is responsible? Is it the child, who does not yet have the wisdom and self-control or, is it the food industry that ultra-processes the foods and adds ingredients into foods which can be harmful and then displays them to trigger an evolutionary preference for food that have been highly processed?
Every country that has adapted the USA diet of ultra-processed foods has experienced similar trends in increasing obesity, diabetes, cardiovascular disease, etc. The USA diet is replacing traditional diets as illustrated by the availability of Coca-Cola. It is sold in over 200 countries and territories (Coca-Cola, 2023).
An increase in ultra-processed foods by 10 percent was associated with a 25 percent increase in the risk of dementia and a 14 per cent increase in the risk of Alzheimers’s (Li et al., 2022). More importantly, people who eat the highest proportion of their diet in ultra-processed foods had a 22%-62% increased risk of death compared to the people who ate the lowest proportion of processed foods (van Tulleken, 2023). In the USA, counties with the highest food swamp scores (the availability of fast food outlets in a county) had a 77% increased odds of high obesity-related cancer mortality (Bevel et al., 2023). The increase risk has also been observed for cardiovascular disease, coronary heart disease, cerebrovascular disease and all cause mortality as is shown in figure 3 (Srour et al., 2019; Rico-Campà et al., 2019).
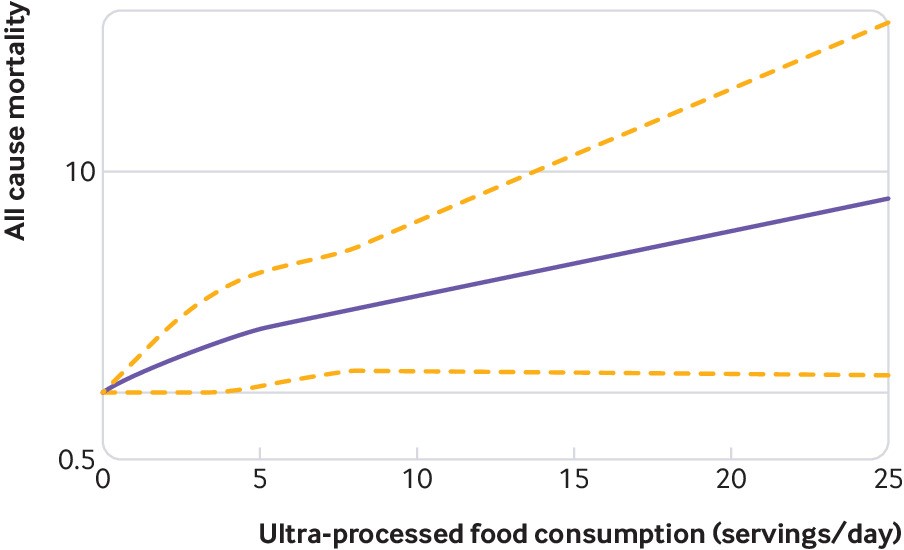
Figure 3. Association between consumption of ultra-processed foods and all cause mortality. Reproduced from Rico-Campà et al, 2019.
The harmful effects of UPF holds up even when correcting for the amount of sugars, carbohydrates or fats in the diet and controlling for socio economic variables.
The logic that underlies this perspective is based upon the writing by Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto). He provides an evolutionary perspective and offers broad and simple rules of health as well as recommendations for reducing UPF risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, added sugars, textured proteins, gums, stabilizers (guar gum, sodium alginate), emulsifiers (mono-and di-glycerides), modified starches, dextrose, palm stearin, and fats, colors and artificial flavoring or other ultra-processed food additives).
What can we do?
The solutions are simple and stated by Michael Pollan in his 2007 New York Times article, “Eat food. Not too much. Mostly Plants.” Eat foods that your great grandmother would recognize as foods (Pollan, 2009). Do not eat any of the processed foods that fill a majority of a supermarket’s space.
- Buy only whole organic natural foods and prepare them yourself.
- Request that food companies only buy and sell non-processed foods.
- Demand government action to tax ultra-processed food and limit access to these foods. In reality, it is almost impossible to expect people to choose healthy, organic foods when they are more expensive and not easily available in the American ‘food swamps and deserts’ (the presence of many fast food outlets or the absence of stores that have fresh produce and non-processed foods). We do have a choice. We can spend more money now for organic, health promoting foods or, pay much more later to treat illness related to UPF.
- It is time to take our cues from the tobacco wars that led to regulating tobacco products. We may even need to start class action suits against producers and merchants of UPF for causing increased illness and premature morbidity.
For more background information and the science behind this blog, read, the book, Ultra-processed people, by Chris van Tulleken.
Look at the following blogs for more background information.
References
Bentley, R.A., Ormerod, P. & Ruck, D.J. (2018). Recent origin and evolution of obesity-income correlation across the United States. Palgrave Commun 4, 146. https://doi.org/10.1057/s41599-018-0201-x
Bero, L. A. (2005). Tobacco Industry Manipulation of Research. Public Health Reports (1974-), 120(2), 200–208. http://www.jstor.org/stable/20056773
Bevel, M.S., Tsai, M., Parham, A., Andrzejak, S.E., Jones, S., & Moore, J.X. (2023). Association of Food Deserts and Food Swamps With Obesity-Related Cancer Mortality in the US. JAMA Oncol. 9(7), 909–916. https://doi.org/10.1001/jamaoncol.2023.0634
Coca-Cola. (2023). More on Coca-Cola. Accessed July 14, 2023. https://www.coca-cola.co.uk/our-business/faqs/how-many-countries-sell-coca-cola-is-there-anywhere-in-the-world-that-doesnt
Johnson, R.K., Appel, L.J., Brands, M., Howard, B.V., Lefevre, M., Lustig, R.H., Sacks, F., Steffen, L.M., & Wylie–Rosett, J. (2009). Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation, 120(10), 1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Li, H., Li, S., Yang, H., et al, 2022. Association of ultraprocessed food consumption with the risk of dementia: a prospective cohort study. Neurology, 99, e1056-1066. https://doi.org/10.1212/WNL.0000000000200871
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books, pp 18-22, 151. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/ref=sr_1_1?crid=1U9Y82YO4DKKP&keywords=erik+peper&qid=1689372466&sprefix=erik+peper%2Caps%2C187&sr=8-1
Pollan, M. (2007). Unhappy meals. The New York Times Magazine. https://www.nytimes.com/2007/01/28/magazine/28nutritionism.t.html
Pollan, M. (2009). Food Rules: An Eater’s Manual. New York: Penguin Books. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/014311638X/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1689373484&sr=8-2
Rico-Campà, A., Martínez-González, M. A., Alvarez-Alvarez, I., de Deus Mendonça, R., Carmen de la Fuente-Arrillaga, C., Gómez-Donoso, C., & Bes-Rastrollo, M. (2019). Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ; 365: l1949 https://doi.org/10.1136/bmj.l1949
Roser, M. (2021).Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data. Assessed July 13, 2023. https://ourworldindata.org/smoking-big-problem-in-brief
Srour, B., Fezeu, L.K., Kesse-Guyot, E.,Alles, B., Mejean, C…(2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé) BMJ,365:l1451. https://doi.org/10.1136/bmj.l1451
Srour, B., Kordahi, M. C., Bonazzi, E., Deschasaux-Tanguy, M., Touvier, M., & Chassaing, B. (2022). Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. The Lancet Gastroenterology & Hepatology. https://doi.org/10.1016/S2468-1253(22)00169-8
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. (Kindle Locations 5906-5908). https://www.amazon.com/Antifragile-Things-Disorder-ANTIFRAGILE-Hardcover/dp/B00QOJ6MLC/ref=sr_1_4?crid=3BISYYG0RPGW5&keywords=Antifragile%3A+Things+That+Gain+from+Disorder+%28Incerto%29&qid=1689288744&s=books&sprefix=antifragile+things+that+gain+from+disorder+incerto+%2Cstripbooks%2C158&sr=1-4
Van Tulleken, C. (2023). Ultra-processed people. The science behind food that isn’t food. New Yoerk: W.W. Norton & Company. https://www.amazon.com/gp/product/1324036729/ref=ox_sc_act_title_1?smid=ATVPDKIKX0DER&psc=1
United States Public Health Service. (1964). The 1964 Report on Smoking and Health. United States. Public Health Service. Office of the Surgeon General. https://profiles.nlm.nih.gov/spotlight/nn/catalog?f%5Bexhibit_tags%5D%5B%5D=smoking
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythm
Posted: July 4, 2023 Filed under: ADHD, behavior, computer, digital devices, education, emotions, Evolutionary perspective, health, laptops, screen fatigue, Uncategorized | Tags: anxiety, autism, bonding, circadian rhythms, depression, nature, still face experiment 3 Comments
Adapted from: Peper, E. Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation,10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Over the past two decades, there has been a significant increase in the prevalence of autism, Attention-Deficit/hyperactivity disorder (ADHD), anxiety, depression, and pediatric suicidal behavior. Autism rates have risen from 1 in 150 children in 2000 to 1 in 36 children in 2020 (CDC, 2023), while ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18-25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020), and depression rates for U.S. teens ages 12-17 have increased from 8% in 2007 to 13% in 2017 (Geiger & Davis, 2019; Walrave et al., 2022). Pediatric suicide attempts have also increased by 163% from 2009 to 2019 (Arakelyan et al., 2023), and during the COVID-19 pandemic, these rates have increased by more than 25% (WHO, 2022; Santomauro et al., 2021). In addition, the prevalence of these disorders has tripled for US adults during the pandemic compared to before (Ettman et al., 2020).
The rapid increase of these disorders is not solely due to improved diagnostic methods, genetic factors or the COVID-19 pandemic. The pandemic amplified pre-existing increasing trends. More likely, individuals who were at risk had their disorders triggered or amplified by harmful environmental and behavioral factors. Conceptually, Genetics loads the gun; epigenetics, behavior, and environment pull the trigger.
While behavioral strategies such as neurofeedback, Cognitive Behavior Therapy, biofeedback, meditation techniques, and pharmaceuticals can treat or ameliorate these disorders, the focus needs to be on risk reduction. In some ways, treatment can be likened to closing the barn doors after the horses have bolted.
Evolutionary perspective to reduce risk factors
Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto), provides an evolutionary perspective and offers simple rules of health by reducing risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, sugar, digital media).
- We do not need evidence of harm to claim that a drug or an unnatural procedure is dangerous. If evidence of harm does not exist, it does not mean harm does not exist.
- Only resort to medical techniques when the health payoff is very large (to save a life), exceeds its potential harm, such as incontrovertibly needed surgery or life-saving medicine (penicillin).
- Avoid the iatrogenics and negative side effects of prescribed medication.
Writer and scholar Taleb’s suggestions are reminiscent of the perspective described by the educator Joseph C. Pearce (1993) in his book, Evolution’s End. Pearce argued that modern lifestyles have negatively affected the secure attachment and bonding between caregivers and infants. The lack of nurturing and responsive caregiving in early childhood may lead to long-term emotional and psychological problems. He points out that we have radically adapted behaviors that differ from those that evolved over thousands of generations and that allowed us to thrive and survive. In the last 100 years, babies have often been separated from their mothers at birth or early infancy by being put in a nursery or separate room, limited or no breastfeeding with the use of formula, exposure to television for entertainment, lack of exploratory play outdoors, and the absence of constant caretakers in high-stress and unsafe environments.
As Pearce pointed out, “If you want true learning, learning that involves the higher frontal lobes – the intellectual, creative brain – then again, the emotional environment must be positive and supportive. This is because at the first sign of anxiety the brain shifts its functions from the high, prefrontal lobes to the old defenses of the reptilian brain… These young people need audio-vocal communication, nurturing, play, body movement, eye contact, sweet sounds and close heart contact on a physical level” (Mercogliano & Debus, 1999).
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past. The proposed recommendations are based upon Talib’s perspective that anything that was not part of our evolutionary past is probably harmful; thus, it is wise to remove the unnatural/unfamiliar and adopt the precautionary principle, which states that if evidence of harm does not exist, it does not mean harm does not exist (Kriebel et al., 2010).
This article is the first of a three-part series. Part 1 focuses on increasing reciprocal communication between infant and caretaker, reducing screen time, and re-establishing circadian rhythms; Part 2 focuses on reducing exposure to neurotoxins, eliminating processed foods, and supporting the human biome; and Part 3 focuses on respiration and movement.
Part 1- Increase bonding, reduce screen time, and re-establish circadian rhythms
Increase bonding between infant and caretaker
Infants develop emotional communication through reciprocal interactions with their caregivers, during which the caregiver responds to the infant’s expressions. When this does not occur, it can be highly stressful and detrimental to the infant’s development. Unfortunately, more and more babies are emotionally and socially isolated while their caregivers are focussed on, and captured by, the content on their digital screens. Moreover, infants and toddlers are entertained (babysat) by cellphones and tablets instead of dynamically interacting with their caretakers. Screens do not respond to the child’s expressions; the screen content is programmed to capture the infant’s attention through rapid scene changes. Without reciprocal interaction, babies often become stressed, as shown by the research of developmental psychologist Professor Edward Tronick, who conducted the “Still Face” experiment (Tronick & Beeghly, 2011; Weinberg et al, 2008).
The “Still Face” experiment illustrated what happens when caregivers are not responding to infants’ communication. The caregivers were asked to remain still and unresponsive to their babies, resulting in the infants becoming increasingly distressed and disengaged from their surroundings. Not only does this apply to infants but also to children, teenagers and older individuals. Watch the short Still Face experiment, which illustrates what happens when the caretaker is not responding to the infant’s communication.
Recommendation. Do not use cellphone and digital media while being with an infant in the first two years of life. It is important for caregivers to limit their cellphone use and prioritize reciprocal interactions with their infants for healthy emotional and psychological development.
Reduce screen time (television, social media, streaming videos, gaming)[1]
From an evolutionary perspective, screen time is an entirely novel experience. Television, computers, and cellphones are modern technologies that have significantly impacted infants’ and young people’s development. To grow, infants, toddlers, and children require opportunities to explore the environment through movement, touch, and play with others, which is not possible with screens. Research has shown that excessive screen time can negatively affect children’s motor development, attention span, socialization skills, and contribute to obesity and other health problems (Hinkley et al., 2014; Carson et al., 2016; Mark, 2023).
When four-year-olds watch fast-paced videos, they exhibit reduced executive functions and impulse control, which may be a precursor for ADHD, compared to children who engage in activities such as drawing (Lillard & Peterson, 2011; Mark, 2023).
Furthermore, excessive screen time and time spent on social media are causal in increasing depression in young adults-–as was discovered when Facebook became available at selected universities. Researchers compared the mental health of students at similar universities where Facebook was or was not available and observed how the students’ mental health changed when Facebook became available (Braghieri et al., 2022). Their research showed that “College-wide access to Facebook led to an increase in severe depression by 7% and anxiety disorders by 20%. In total, the negative effect of Facebook on mental health appeared to be roughly 20% the magnitude of what is experienced by those who lose their job” (Walsh, 2022).
Exposure to digital media has also significantly reduced our attention span from 150 seconds in 2004 to an average of 44 seconds in 2021. The shortening of attention span may contribute to the rise of ADHD and anxiety (Mark, 2022, p. 96).
Recommendations: Reduce time spent on social media, gaming, mindlessly following one link after the other, or watching episode after episode of streaming videos. Instead, set time limits for screen use, turn off notifications, and prioritize in-person interactions with friends, family and colleagues while engaging in collaborative activities. Encourage children to participate in physical and social activities and to explore nature.
To achieve this, follow the guidelines from the American Academy of Pediatrics’ recommendation on screen time (Council on Communications and Media, 2016), which suggest these limits on screen time for children of different age groups:
- Children under 18 months of age should avoid all screen time, except for video chatting with family and friends.
- Children aged 18-24 months should have limited screen time, and only when watched together with a caretaker.
- Children aged 2 to 5 years should have no more than one hour of screen time per day with parental supervision.
- For adolescents, screen and social media time should be limited to no more than an hour a day.
In our experience, when college students reduce their time spent on social media, streaming videos, and texting, they report that it is challenging; however, they then report an increase in well-being and performance over time (Peper et al., 2021). It may require more effort to provide children with actual experiential learning and entertainment than allowing them to use screens, but it is worthwhile. Having children perform activities and play outdoors–in a green nature environment–appears to reduce ADHD symptoms (Louv, 2008; Kuo & Taylor, 2004).
Reestablish circadian (daily) rhythms
Our natural biological and activity rhythms were regulated by natural light until the 19th century. It is hard to imagine not having light at night to read, to work on the computer, or to answer email. However, light not only illuminates, but also affects our physiology by regulating our biological rhythms. Exposure to light at night can interfere with the production of melatonin, which is essential for sleep. Insufficient sleep affects 30% of toddlers, preschoolers, and school-age children, as well as the majority of adolescents. The more media is consumed at bedtime, the more bedtime is delayed and total sleep time is reduced (Hale et al., 2018). Reduced sleep is a contributing factor to increased ADHD symptoms of inattention, hyperactivity and impulsivity (Cassoff et al., 2012).
Recommendations: Support the circadian rhythms. Avoid screen time one hour before bedtime. This will reduce exposure to blue light and reduce sympathetic arousal triggered by the content on the screen or reactions to social media and emails. Sleep in total darkness, and establish a regular bedtime and waking time to avoid “social jetlag,” which can negatively affect health and performance (Caliandro et al., 2021). Implement sleep hygiene strategies such as developing a bedtime ritual to improve sleep quality (Stager et al., 2023; Suni, 2023). Thus, go to bed and wake up at the same time each day, including weekends. Avoid large meals, caffeine, and alcohol before bedtime. Consistency is key to success.
Conclusion
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past, and explore strategies that support behaviors that have allowed the human being to thrive and survive. Improve clinical outcomes and optimize health by enhancing reciprocal communication interactions, reducing screen time and re-establishing the circadian rhythm.
References
Arakelyan, M., Freyleue, S., Avula, D., McLaren, J.L., O’Malley, A.J., & Leyenaar, J.K. (2023). Pediatric Mental Health Hospitalizations at Acute Care Hospitals in the US, 2009-2019. JAMA, 329(12), 1000–1011. https://doi.org/10.1001/jama.2023.1992
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Caliandro, R., Streng, A.A., van Kerkhof, L.W.M., van der Horst, G.T.J., & Chaves, I. (2021). Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients, 13(12), 4543. https://doi.org/10.3390/nu13124543
Carson, V., Tremblay, M.S., Chaput, J.P., & Chastin, S.F. (2016). Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab, 41(6 Suppl 3), S294-302. https://doi.org/10.1139/apnm-2016-0026
Cassoff, J., Wiebe, S.T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nat Sci Sleep, 4, 73-80. https://doi.org/10.2147/NSS.S31269
CDC. (2022). Attention-Deficit/hyperactivity disorder (ADHD): ADHD through the years. Centers for Disease Control and Prevention. Assessed March 27, 2023. https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. (2023). Data & Statistics on Autism Spectrum Disorder. CDC Centers for Disease Control and Prevention. Assessed March 25, 2023. https://www.cdc.gov/ncbddd/autism/data.html
Council on Communications and Media. (2016). Media and young minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M.,& Galea, S. (2020), Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Geiger, A.W. & Davis, L. (2019). A growing number of American teenagers-particularly girls-are facing depression. Pew Research Center. Accessed March 28, 2023.
Goodwin, R.D., Weinberger, A.H., Kim, J.H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. J Psychiatr Res. 130, 441-446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hale, L., Kirschen, G/W., LeBourgeois, M.K., Gradisar, M., Garrison, M.M., Montgomery-Downs, H., Kirschen, H., McHale, S.M., Chang, A.M., & Buxton, O.M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc Psychiatr Clin N Am, 27(2),229-245. https://doi.org/10.1016/j.chc.2017.11.014
Hinkley, T., Verbestel, V., Ahrens, W., Lissner, L., Molnár, D., Moreno, L.A., Pigeot, I., Pohlabeln, H., Reisch, L.A., Russo, P., Veidebaum, T., Tornaritis, M., Williams, G., De Henauw, S., De Bourdeaudhuij, I; IDEFICS Consortium. (2014). Early childhood electronic media use as a predictor of poorer well-being: a prospective cohort study. JAMA Pediatr,. May;168(5):485-92. https://doi.org/10.1001/jamapediatrics.2014.94
Kriebel, D., Tickner, J., Epstein, P., Lemons, J., Levins, R., Loechler, E.L., Quinn, M., Rudel, R., Schettler, T., Stoto, M. (2001). The precautionary principle in environmental science. Environ Health Perspect, 109(9):871-6. https://doi.org/10.1289/ehp.01109871
Kuo. F.E. & Taylor, A.F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 94(9),1580-6. https://doi.org/10.2105/ajph.94.9.1580
Lillard, A.S. & Peterson, J. The immediate impact of different types of television on young children’s executive function. Pediatrics, 128(4), 644-9. https://doi.org/10.1542/peds.2010-1919
Louv, R. (2008). Last Child in the Woods: Saving Our Children from Nature-Deficit Disorder. Algonquin Books. Chapel Hill, NC: Algonquin Books
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press.
Mercogliano, C. & Debus, K. (1999). Nurturing Heart-Brain Development Starting With Infants 1999 Interview with Joseph Chilton Pearce. Journal of Family Life, 5(1). https://www.michaelmount.co.za/nurturing-heart-brain-development-starting-with-infants-1999-interview-with-joseph-chilton-pearce/
Pearce, J.C. (1993). Evolutions’s End. New York: HarperOne.
Peper, E., Wilson, V., Martin, M., Rosegard, E., & Harvey, R. (2021). Avoid Zoom fatigue, be present and learn. NeuroRegulation, 8(1), 47–56. https://doi.org/10.15540/nr.8.1.47
Santomauro, D.F., Mantilla Herrera, A.M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D.M., Abbafati, C., Adolph, C., …. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(103121700-1712., https://doi.org/10.1016/S0140-6736(21)02143-7
Stager, L.M., Caldwell, A., Bates, C., & Laroche, H. (2023). Helping kids get the sleep they need. Society of Behavioral Medicine. Accessed March 29, 2023 https://www.sbm.org/healthy-living/helping-kids-get-the-sleep-they-need?gclid=Cj0KCQjww4-hBhCtARIsAC9gR3ZM7v9VSvqaFkLnceBOH1jIP8idiBIyQcqquk5y_RZaNdUjAR9Wpx4aAhTBEALw_wcB
Suni, E. (2023). Sleep hygiene- What it is, why it matters, and how to revamp your habits to get better nightly sleep. Sleep Foundation. Accessed March 29, 2023. https://www.sleepfoundation.org/sleep-hygiene
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto) Random House Publishing Group. (Kindle Locations 5906-5908).
Tronick, E. & Beeghly, M. (2011).Infants’ meaning-making and the development of mental health problems. Am Psychol, 66(2),107-19. https://doi.org/10.1037/a0021631
Walrave, R., Beerten, S.G., Mamouris, P. et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 23, 163 (2022). https://doi.org/10.1186/s12875-022-01769-w
Walsh, D. (2022 September 14). Study: Social media use linked to decline in mental health. MIT Management Ideas Made to Matter. Accessed March 28, 2023. https://mitsloan.mit.edu/ideas-made-to-matter/study-social-media-use-linked-to-decline-mental-health#:~:text=College%2Dwide%20access%20to%20Facebook,with%20either%20psychotherapy%20or%20antidepressants
Weinberg, M.K., Beeghly, M., Olson, K.L., & Tronick, E. (2008). A Still-face Paradigm for Young Children: 2½ Year-olds’ Reactions to Maternal Unavailability during the Still-face. J Dev Process, 3(1):4-22. https://pubmed.ncbi.nlm.nih.gov/22384309/
WHO (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. Assessed march 26, 2023. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
[1] The critique of social media does not imply that there are no benefits. If used judiciously, it is a powerful tool to connect with family and friends or access information.
Mouth breathing and tongue position: a risk factor for health
Posted: June 8, 2023 Filed under: ADHD, behavior, Breathing/respiration, cognitive behavior therapy, Evolutionary perspective, healing, health, Nutrition/diet, self-healing, Uncategorized | Tags: babies, breastfeedging, development, infants, jaw, mouth breathing, neurocognitive develoment, nose breathing, sleep, tongue-tie Leave a commentErik Peper, PhD, BCB and Ron Swatzyna, PhD, LCSW, BCB, BCN
Adapted from: Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512

Breathing usually occurs without awareness unless there are problems such as asthma, emphysema, allergies, or viral infections. Infant and child development may affect how we breathe as adults. This blog discusses the benefits of nasal breathing, factors that contribute to mouth breathing, how babies’ breastfeeding and chewing decreases the risk of mouth breathing, recommendations that parents may implement to support healthy development of a wider palate, and the embedded video presentation, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development, by Karindy Ong, MA, CCC-SLP, CFT, .
Benefits of nasal breathing
Breathing through the nose filters, humidifies, warms, or cools the inhaled air as well as reduces the air turbulence in the upper airways. In addition, the epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation. Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. This slower breathing also facilitates sympathetic parasympathetic balance and reduces airway irritation.
Mouth breathing
Some people breathe predominantly through their mouth although nose breathing is preferred and health promoting. Mouth breathing negatively impacts the ability to perform during the day as well as affect our cognitions and mood (Nestor, 2020). It contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded mis-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
One recommendation to reduce mouth breathing is to tape the mouths closed with mouth tape (McKeown, 2021). Using mouth tape while sleeping bolsters nose breathing and may help people improve sleep, reduce snoring, and improves alertness when awake (Lee et al, 2022).
Experience how mouth breathing affects the throat and upper airway
Inhale quickly, like a gasp, as much air as possible through your open mouth. Exhale letting the air flow out through your mouth. Repeat once more.
Inhale quickly as much air through the nose, then exhale by allow the airflow out through the nose. Repeat once more.
What did you observe? Many people report that rapidly inhaling through the mouth causes the back of the throat and even upper airways to feel drier and irritated. This does not occur when inhaling through the nose. This simple experiment illustrates how habitual mouth breathing may irritate the airways.
Developmental behavior that contributes to mouth breathing
The development of mouth breathing may begin right at birth when the mouth, tongue, jaw and nasal area are still developing. The arch of the upper palate forms the roof of the oral cavity that separates the oral and nasal cavities. When the palate and jaw narrows, the arch of the palate increases and pushes upwards into the nasal area. This reduces space in the nasal cavity for the air to flow and obstructs nasal breathing. The highly vaulted palate is not only genetically predetermined but also by how we use our tongue and jaw from birth. The highly arched palate is only a recent anatomical phenomena since the physical structure of the upper palate and jaw from the pre- industrial era was wider (less arched upper palate) than many of our current skulls (Kahn & Ehrlich, 2018).
The role of the tongue in palate development
After babies are born, they breastfeed by sucking with the appropriate tongue movements that help widen the upper palate and jaw. On the other hand, when babies are bottle fed, the tongue tends to move differently which causes the cheek to pull in and the upper palate to arch which may create a high narrow upper palate and making the jaw narrower. There are many other possible factors that could cause mouth breathing such as tongue-tie (ankyloglossia), septal deviation, congenital malformation, enlarged adenoids and tonsils (Aden tonsillar hyperplasia), inflammatory diseases such as allergic rhinitis (Trabalon et al, 2012). Whatever the reasons, the result of the impoverished tongue movement and jaw increases the risk for having a higher arched upper palate that impedes nasal breathing and contributes to habitual mouth breathing.
The forces that operate on the mouth, jaw and palate during bottle feeding may be similar to when you suck on straw and the cheeks coming in with the face narrowing. The way the infants are fed will change the development of the physical structure that may result in lifelong problems and may contribute to developing a highly arched palate with a narrow jaw and facial abnormalities such as long face syndrome (Tourne, 1990).
To widen the upper palate and jaw, the infant needs to chew, chew and tear the food with their gums and teeth. Before the industrialization of foods, children had to tear food with their teeth, chew fibrous foods or gnaw at the meat on bones. The chewing forces allows the jaw to widen and develop so that when the permanent teeth are erupting, they would more likely be aligned since there would be enough space–eliminating the need for orthodontics. On the other hand, when young children eat puréed and highly processed soft foods (e.g., cereals soaked in milk, soft breads), the chewing forces are not powerful enough to encourage the widening of the palate and jaw.
Although the solution in adults can be the use of mouth tape to keep the mouth closed at night to retrain the breathing pattern, we should not wait until we have symptoms. The focus needs to be on prevention. The first step is an assessment whether the children’s tongue can do its job effectively or limited by tongue-tie and the arch of the palate. These structures are not totally fixed and can change depending on our oral habits. The field of orthodontics is based upon the premise that the physical structure of the jaw and palate can be changed, and teeth can be realigned by applying constant forces with braces.
Support healthy development of the palate and jaw
Breastfeed babies (if possible) for the first year of life and do NOT use bottle feeding. When weaning, provide chewable foods (fruits, vegetable, roots, berries, meats on bone) that was traditionally part of our pre-industrial diet. These foods support in infants’ healthy tongue and jaw development, which helps to support the normal widening of the palate to provide space for nasal breathing.
Provide fresh organic foods that children must tear and chew. Avoid any processed foods which are soft and do not demand chewing. This will have many other beneficial health effects since processed foods are high in simple carbohydrates and usually contain color additives as well as traces of pesticides and herbicides. The highly processed foods increase the risk of developing depression, type 2 diabetes, inflammatory disease, and colon cancer (Srour et al., 2019).
Sadly, the USA allows much higher residues of pesticide and herbicides that act as neurotoxins than are allowed in by the European Union. For example, the acceptable level of the herbicide glyphosate (Round-Up) is 0.7 parts per million in the USA while in the acceptable level is 0.01 parts per million in European countries (Tano, 2016; EPA, 2023; European Commission, 2023). The USA allows this higher exposure even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbò et al., 2022).
The negative effects of herbicides and pesticides are harmful for growing infants. Even fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021) and organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010).
To implement these basic recommendations are very challenging. It means the mother has to breastfeed her infant during the first year of life. This is often not possible because of socioeconomic inequalities; work demands and medical complications. It also goes against the recent cultural norm that fathers should participate in caring for the baby by giving the baby a bottle of stored breast milk or formula.
From our perspective, women who give birth must have a year paid maternity leave to provide their infants with the best opportunity for health (e.g., breast-feeding, emotional bonding, and reduced financial stress). As a society, we have the option to pay the upfront cost now by providing a year- long maternity leave to mothers or later pay much more costs for treating chronic conditions that may have developed because we did not support the natural developmental process of babies.
Relevance to the field of neurofeedback and biofeedback
Clinicians often see clients, especially children with diagnostic labels such as ADHD who have failed to respond to numerous psychotherapies and pharmacotherapies. In the recent umbrella review and meta-analytic evaluation of recent meta-analyses, Leichsenring et al. (2022) found only small benefits overall for both types of intervention. They suggest that a paradigm shift in research seems to be required to achieve further progress in resolving mental health issues. As the past director of National Institute of Health, Dr. Thomas Insel pointed out that the Diagnostic and Statistical Manual of Mental Disorders (DSM) is not a valid instrument and should be a big wake up call for all of us to think outside the box (Insel, 2009). One factor that starts right at birth is the oral cavity development by dysfunctional tongue movements.
We want to make all of you aware of a serious issue in children that you may come across. For those of us who work with children children, we need to ask their parents about the following: tongue-tie, mouth breathing, bedwetting, high-vaulted palate, thumb sucking, abnormal eating issues, apraxia, dysarthria, and hypotonia. Research suggests that the palates of these children are so arched that the tongue cannot do its job effectively, causing multiple issues which may be related.
Please view the webinar from May 17, 2023. Presented by Karindy Ong, MA, CCC-SLP, CFT, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development. The presentation explains the developmental process of the role the tongue plays and how it contributes to nasal breathing. Please pass it on to others who may have interest.
References
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians.
Insel, T.R. (2009). Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry, 66(2), 128-133. https://doi.org/10.1001/archgenpsychiatry.2008.540
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lee, Y.C., Lu, C.T., Cheng, W.N., & Li, H.Y. (2022).The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare (Basel), 10(9), 1755. https://doi.org/10.3390/healthcare10091755
Leichsenring, F., Steinert, C., Rabung, S. and Ioannidis, J.P.A. (2022), The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry, 21: 133-145. https://doi.org/10.1002/wps.20941
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath/dp/0593191358/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1686191995&sr=8-1
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Srour, B. et al. (2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé).BMJ, 365. https://doi.org/10.1136/bmj.l1451
Tano, B. (2016). The Layman’s Guide to Integrative Immunity. Integrative Medical Press. https://www.amazon.com/Laymans-Guide-Integrative-Immunity-Discover/dp/0983419299/_
Tourne, L.P. (1990). The long face syndrome and impairment of the nasopharyngeal airway. Angle Orthod, 60(3):167-76. https://doi.org/10.1043/0003
Trabalon, M. & Schaal, B. (2012). It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr, 207605. https://doi.org/10.1155/2012/207605
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Biofeedback, posture and breath: Tools for health
Posted: December 1, 2022 Filed under: ADHD, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, computer, digital devices, education, emotions, ergonomics, Evolutionary perspective, Exercise/movement, healing, health, laptops, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, screen fatigue, self-healing, stress management, Uncategorized, vision, zoom fatigue 2 CommentsTwo recent presentations that that provide concepts and pragmatic skills to improve health and well being.
How changing your breathing and posture can change your life.
In-depth podcast in which Dr. Abby Metcalf, producer of Relationships made easy, interviews Dr. Erik Peper. He discusses how changing your posture and how you breathe may result in major improvement with issues such as anxiety, depression, ADHD, chronic pain, and even insomnia! In the presentation he explain how this works and shares practical tools to make the changes you want in your life.
How to cope with TechStress
A wide ranging discussing between Dr. Russel Jaffe and Dr Erik that explores the power of biofeedback, self-healing strategies and how to cope with tech-stress.
These concepts are also explored in the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics. You may find this book useful as we spend so much time working online. The book describes the impacts personal technology on our physical and emotional well-being. More importantly, “Tech Stress” provides all of the basic tools to be able not only to survive in this new world but also thrive in it.
Additiona resources:
Gonzalez, D. (2022). Ways to improve your posture at home.