Rethink the monies spent on cancer screening tests
Posted: November 24, 2023 Filed under: behavior, cancer, Evolutionary perspective, healing, health, Nutrition/diet, self-healing | Tags: breast canceer, Cancer screening, environmental toxins, Life style, mammography, organic foods Leave a commentErik Peper, PhD and Richard Harvey, PhD

Cancer screening tests are based upon the rational that early detection of fatal cancers enables earlier and more effective treatments (Kowalski, 2021), however, there is some controversy. Early screening may increase the risk of over diagnosis, treating false positives (people who did not have the cancer but the test indicates they have cancer) and potentially fatal treatment of cancers that would never progress to increase morbidity or mortality (Kowalski, 2021).
Today about $40 billion spent on colon cancer screening, $15 billion spent on breast cancer screening, and $4 billion spent on prostate cancer screening annually (CSPH, 2021). A question is raised whether the billions and billions of dollars spent on screening asymptomatic participants would be more wisely spent on promoting and supporting life style changes that reduce cancer risks and actually extend life span? That cancer screening is expensive does not mean no one should be screened. Instead, the argument is that the majority of healthcare dollars could be spent on health promotion practices and reserving screening for those people who are at highest risk for developing cancers.
What is the evidence that screening prolongs life?
Cancer screening tests appear correlated with preventing deaths since deaths due to cancers in the USA have decreased by about 28% from 1999 to 2020 (CDC, 2023a). Although cancer causes many of the deaths in the USA, overall life expectancy has increased by less than 1% from 1999 to 2020. If cancer screening were more effective, the life expectancy should have increased more because cancer is the second leading cause of death (CDC, 2023b). Consider also that deaths due to cancers may be coincident and or comorbid with other circumstances. For example, during the last four years, overall life expectancy in the USA has precipitously declined in part due to other causes of death such as the COVID pandemic and opioid overdose epidemic (Lewis, 2022). Decline in life expectancy in the USA has many contributing factors, including the ‘harms’ associated with cancer screening procedures. For example, perforations during colon cancer screening can lead to internal bleeding, or complications related to surgeries, radiotherapies or chemotherapies. Bretthauer et al., (2023) commented: “A cancer screening test may reduce cancer-specific mortality but fail to increase longevity if the harms for some individuals outweigh the benefits for others or if cancer-specific deaths are replaced by deaths from competing cause” (p. 1197).
Bretthauer et al. (2023) conducted a systematic review and meta-analysis of 18 long-term randomized clinical trials involving 2.1 million Individuals with more than nine years of follow-up reporting on all-cause mortality. They reported that“…this meta-analysis suggest that current evidence does not substantiate the claim that common cancer screening tests save lives by extending lifetime, except possibly for colorectal cancer screening with sigmoidoscopy.”
Following is a summary of Bretthauer et al. (2023) findings:
- The only cancer screening with a significant lifetime gain (approximately 3 months) was sigmoidoscopy.
- There was no significant difference between harms of screening and benefits of screening for:
- mammography
- prostate cancer screening
- FOBT (fecal occult blood test) screening every year or every other year
- lung cancer screening Pap test cytology for cervical cancer screening, no randomized clinical trials with cancer-specific or all-cause mortality end points and long term follow-up were identified.
Potential for loss or harm (e.g., iatrogenic and nosocomial) versus potential for benefit and extended life
More than 35 years ago a significant decrease in breast cancer mortality was observed after mammography was implemented. The correlation suggested a causal relationship that screening reduced mortality (Fracheboud, 2004). This correlation made logical sense since the breast cancer screening test identified cancers early which could then be treated and thereby would result in a decrease in mortality.
How much money is spent on screening that may correlate with unintended harms?
The annual total expenditure for cancer screening is estimated to be between $40-$50 billion annually (CSPH, 2021). Below are some of the estimated expenditures for common tests other than colorectal cancer screening, which arguably is costly; however, has potential benefits that outweigh potential harms.
- $10.37-13.94 billion for mammography to screen 50% of eligible women (Badal et al, 2023).
- $2-4 billion for prostate cancer (Ma et al., 2014)
- $1-2 billion for lung cancer (Taylor et al., 2022)
What is the correlation between initiation of mammography and decrease in breast cancer mortality?
The conclusion that mammography reduced breast cancer mortality was based upon studies without control groups; however, this relationship could be causal or synchronistic. The ambiguity of correlation or causation was resolved with the use of natural experimental control groups. Some European countries began screening 10 years earlier than other countries. Using statistical techniques such as propensity score matching when comparing the data from countries that initiated mammography screening early (Netherlands, Sweden and Northern Ireland) to countries that started screening 10 year later (Belgium, Norway and Republic of Ireland), the effectiveness of screening could be compared.
The comparisons showed no difference in the decrease of breast cancer mortality in countries that initiated breast cancer screening early or late. For example, there was no difference in the decrease of breast cancer mortality rates of women who lived in the Netherlands that started screening early versus those who lived in Belgium that began screening 10 years later, as is shown Figure 1 (Autier et al, 2011).
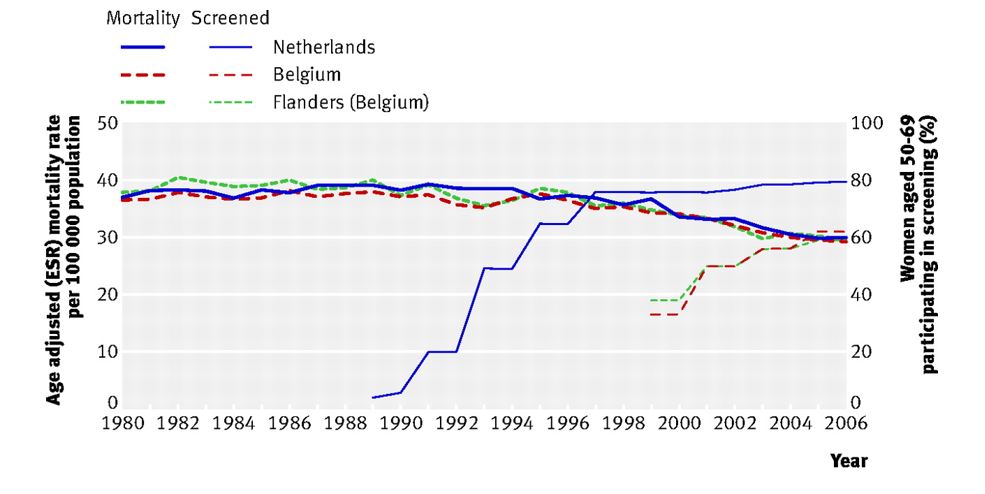
Figure 1. No difference in age adjust breast cancer mortality between the two adjacent countries even though breast cancer screening began ten years earlier in the Netherlands than in Belgium (graph reproduced from Autier et al, 2011).
The observations are similar when comparing neighboring countries: Sweden (early screening) to Norway (late screening) as well as Northern Ireland, UK (early screening) compared to the Republic of Ireland (late screening). The systematic comparisons showed that screening did not account for the decrease in breast cancer mortality. To what extent could the decrease in mortality be related to other factors such as better prenatal and early childhood diet and life style, improved nutrition, reduction in environmental pollutants, and other unidentified life style and environmental factors which improve immune competence?
A simplistic model to reduce the risk of cancers is described in the following equation (Gorter & Peper, 2011).

Cancer risk can be reduced, arguably by influencing risk factors that contribute to cancers as well as increasing factors to enhance immune competence. In the simple model above, ‘Cancer burden’ refers to the set of exposures that increase the odds of cancer formations. Categories include exposures to oncoviruses, environmental exposures (e.g., ionizing radiation, carcinogenic chemicals) as well as genetic (e.g., chromosomal aberrations, replication errors) and epigenetic factors (e.g., lifestyle categories related to eating, exercising, sleeping, and relaxing). In the model above, ‘Immune competence’ refers to a set of categories of immune functioning related to DNA repair, orderly cell death (i.e., processes of apoptosis), expected autophagy, as well as ‘metabolic rewiring,’ also called cellular energetics, that would allow the body to be able to reduce manage cancers from progressing (Fouad & Aanei, 2017) .
How do we examine the cancer burden/immune competence relationship?
Schmutzler et al., (2022) have suggested personalized and precision-medicine risk-adjusted cancer screening incorporating “… high-throughput “multi-omics” technologies comprising, among others, genomics, transcriptomics, and proteomics, which have led to the discovery of new molecular risk factors that seem to interact with each other and with non-genetic risk factors in a multiplicative manner.” The argument is that ‘profit-centered’ medicine could incorporate ‘multi-omics’ into risk-adjusted cancer screening as a way to reduce potential loss or harm due to other cancer screening procedures. Rather than simply screening for cancers using currently invasive or toxic procedures which may do more harm than good, consider more nuanced screening tests aimed at the so-called ‘hallmarks of cancer?’ For example, Hanahan (2022) suggests some technical targets for the multi-omics technologies. The following are some of the precision screening tests possible topersonalized medicine of 14 factors or processes related to:
- cells evading growth suppression
- non-mutational epigenetic reprogramming
- avoiding immune destruction
- enabling replicative immortality
- tumor-promoting inflammation
- polymorphic microbiomes
- activating invasion and metastasis
- inducing or accessing vasculature formation/angiogenesis
- cellular senescence
- genome instability and mutation
- resisting cell death
- deregulating cellular metabolism
- unlocking phenotypic plasticity
- sustaining proliferative signaling
Of the listed categories above, ‘phenotypic plasticity’ (cf. Feinberg, 2007; Gupta et al., 2019) suggests that lifestyle behaviors and environmental exposures play a role in cancer progression and regression.
Lifestyle and environmental factors can contribute to the development of cancers.
The 2008-2009 report from the President’s Cancer Panel appraised the National Cancer Program in accordance with the National Cancer Act of 1971 stated (Reuben, 2010):
“We have grossly underestimated the link between environmental toxins, plastics, chemicals, and cancer risk. It is estimated that 70 percent of all cancers were related to diet and environment “
Multiple research studies have shown that a healthy life style pattern is associated with decreased cancer risks and increased longevity. Lifestyle factors that have been documented to increase cancer risks in the United Kingdom (UK) as shown in figure 2.
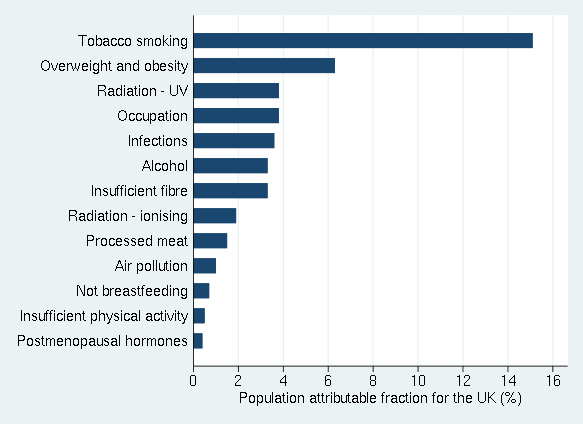
Figure 2. Percentages of cancer cases in the UK attributable to different exposures. Adapted from Brown et al., 2018 and reproduced by permission from Key et al., 2020.
Similar findings have been reported by Song et al. (2016) from the long term follow-up of 126901 adult health care professionals. People who never smoked, drank no alcohol or moderate alcohol (< 1 drink/d for women; < 2 drinks/d for men}, had a body-mass index (BMI) of at least 18.t but lower than 27.5, did weekly aerobic physical activity of at least 75 vigorous-intensity minutes or 150 150 moderate-intensity minutes compared to those who smoked, drank, had high BMI and did not exercise had nearly half the cancer death rate. Song et al (2016) concludes:
“…about 20% to 40% of carcinoma cases and about half of carcinoma deaths can be potentially prevented through lifestyle modification. Not surprisingly, these figures increased to 40% to 70% when assessed with regard to the population of US whites which has a much worse lifestyle pattern than other cohorts. Notably, approximately 80% to 90% of lung cancer deaths can be avoided if Americans adopted the lifestyle of the low-risk group, mainly by quitting smoking. For other cancers, a range of 10% to 70% of deaths can be prevented. These results provide strong support for the importance of environmental factors in cancer risk and reinforce the enormous potential of primary prevention for cancer control.”
Said another way, primary prevention should remain a priority for cancer control.
Given that many cancers are related to diet, environment and lifestyle, it is estimated that 50% of all cancers and cancer deaths could be prevented by modifying personal behavior. Thus, the monies spent on screening or even developing new treatments could better be spent on prevention along with implementing programs that promote a healthier environment, diet and personal behavior (AACR, 2011).
What can be done? Addressing systems not symptoms
From a ‘systems perspective,’ the first step is to reduce the cancer burden and carcinogenic agents that occur in our environment such environmental pollution (Turner et al., 2022). In many cases, governmental regulations that reduce cancer risk factors have been weakened, delayed, and contested for years through industry’s lobbying. It often takes more than 30 years after risk factors have been observed and documented before government regulations are successfully implemented, as exemplified in the battle over tobacco or, air pollution regulations related to particulates from burning fossil fuels (Stratton et al, 2001).
Sadly, we cannot depend upon governments or industries to implement regulations known to reduce cancer risks. More within our control is implementing lifestyle changes that enhance immune competence and promote health.
Implement a healthy life style that enhances immune competence and, supports health and well-being
Paraphrasing a trope of what some physicians may state: ‘Take two pills, and call me in the morning. Oh, and eat well, exercise, and get good rest.’ Broadly stated, the following are some controllable lifestyle behaviors that can decrease cancer risks and promotes health. Implementing environmental and lifestyle changes are very challenging because they are highly related to socio economic factors, cultural factors, industry push for profits over health, and self-care challenges since there are no immediate results experienced by behavior and lifestyle changes.
In many cases, the effects of harmful life-style and environment factors are only observed twenty or more years later (e.g., diabetes, lung cancer, cirrhosis of the liver). The individual does not experience immediate benefits of lifestyle changes thus it is more challenging to know that your healthy life style has an effect. The process is even more complex because in most cases it is not a single factor but the interaction of multiple factors (genetics, lifestyle, and environment). The complexity of causality so often conflicts with the simplistic research studies to identify only one isolated risk factor. Instead of waiting for the definitive governmental guidelines and regulations, adopt a ‘precautionary principle’ which means do not take an action when there is uncertainty about its potential harm (Goldstein, 2001). Do not wait for screening; instead, take charge of your health and implement as many of the following behaviors and strategies to enhance immune competence and thereby reduce cancer risks.
Eat organic foods, especially vegetable and fruits.
Many studies have suggested that eating organic foods and in particular more fruits and vegetable such as a Mediterranean diet is associated with increased health and longevity. Similarly, people who eat do not eat highly-processed or ultra-processed foods have better health status (Van Tulleken, 2023). For example, In the large prospective study of 68, 946 participants, adults who consumed the most organic fruits, vegetables, dairy products, meat and other foods had 25% fewer cancers when compared with adults who never ate organic food (Baudry et al., 2018; Rabin, 2018). Similarly, many studies have reported that those who adhere consistently to a Mediterranean diet have a significantly lower incidence of chronic diseases (such as cardiovascular diseases, diabetes, etc.) and cancers compared to those who do not adhere to a Mediterranean diet (Mentella et al., 2019).
Reduce environmental pollution exposure
Air pollution and the exposure to airborne carcinogens are a significant risk factor for cancers as illustrated by the increased cancer rates among smokers. In the USA, the reduction of smoking has significantly decreased the lung cancer deaths (US Department of Health and Human Services, 2014).
Increase movement and exercise
Many studies have documented that people who exercise regularly and are otherwise non–sedentary but are active their entire lives have the lowest risk for breast cancers and colon cancers. Women who exercise 3 hours a week or more have a 30-40% lower risk of developing breast cancer (NIH NCI, 2023). The NIH National Cancer Institute summary concludes that exercises also significantly benefited the following cancer survivors (NIH NCI, 2023):
- Breast cancer: In a 2019 systematic review and meta-analysis of observational studies, breast cancer survivors who were the most physically active had a 42% lower risk of death from any cause and a 40% lower risk of death from breast cancer than those who were the least physically active (Spei et al, 2019).
- Colorectal cancer: Evidence from multiple epidemiologic studies suggests that physical activity after a colorectal cancer diagnosis is associated with a 30% lower risk of death from colorectal cancer and a 38% lower risk of death from any cause (Patel et al., 2019).
- Prostate cancer: Limited evidence from a few epidemiologic studies suggests that physical activity after a prostate cancer diagnosis is associated with a 33% lower risk of death from prostate cancer and a 45% lower risk of death from any cause ((Patel et al., 2019).
- Implement stress management.
Chronic stress may reduce immune competence and increase the risk of cancers as well as hinders healing from cancer treatments (Dai et al., 2020). The results of numerous studies have shown that implementing stress management spractices uch as Cognitive-behavioral stress management (CBSM) improves mood and lowers distress during treatment and, is also associated with longer survival compared to control groups in the 8-15 year follow up (Stagl et al., 2015).
Respect your biological rhythm.
The International Agency for Research on Cancer (IARC) reports that, when the human circadian clock is disrupted, the likelihood of developing cancers, including lung cancers, intestinal cancers, and breast cancers, dramatically increases (Huang, et al., 2023). Go to bed at the same time and, have about 8 hours of sleep. As much as possible avoid night shifts at work along with frequent jet lag as that highly disrupts the circadian rhythm.
Increase social connections and be part of a social community
Absence of social support, feeling lonely and socially isolated tends reduces immune competence and increases cancer mortality risk while having more social support satisfaction is associated with lower mortality risks (Salazaor et al., 2023; Boen et al., 2018). Meta-analysis of 148 studies (308,849 participants) found that that on the average there is a 50% increased likelihood of survival for participants with stronger social relationships (Holt-Lunstad et al., 2010).
Live a life with meaning and purpose
Having meaning and purpose make each moment worth living and may contribute to improving immune function and possible cancer survival (LeShan, 1994; Rosenbaum & Rosenbaum, 2023).
Summary
The research suggests that cancer screening does not extend life span unless specifically performed for certain diagnostic purposes or, with individuals who are at high risk of developing cancers (e.g., have a genetic predisposition). Implementing self-care health behaviors that have been identified to promote health and increase lifespan. Implementing health behaviors is challenging since there is limited governmental and corporate support. Thus, take charge and implement a holistic self-care lifestyle that reduces cancer risk factors and supports health.
See also the following blogs:
References
AACR. (2011). AACR Cancer Progress Report 2011. American Association for Cancer Research. http://www.aacr.org/Uploads/DocumentRepository/2011CPR/2011_AACR_CPR_Text_web.pdf
American Cancer Society. (2021). History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms. Accessed November 11, 2023. https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/overview/chronological-history-of-acs-recommendations.html
Autier, P., Boniol, M., Gavin, A,, & Vatten, L.J. (2011) Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ. 343, d4411. https://doi.org/10.1136/bmj.d4411
Badal., K., Staib, J., Tice,J., Kim, M-O., Eklund, M., DaCosta Byfield, S., Catlett,K., Wilson,L., et al, (2023). Cost of breast cancer screening in the USA: Comparison of current practice, advocated guidelines, and a personalized risk-based approach. Journal of Clinical Oncology, 41: 16_suppl, 3 18917 :16_suppl, e18917. https://doi.org/10.1200/JCO.2023.41.16_suppl.e18917
Baudry, J., Assmann, K.E., Touvier, M., et al. (2018). Association of Frequency of Organic Food Consumption With Cancer Risk: Findings From the NutriNet-Santé Prospective Cohort Study. JAMA Intern Med, 178(12), 1597–1606. https://doi.org/10.1001/jamainternmed.2018.4357
Boen, C.E., Barrow, D..A, Bensen, J.T., Farnan, L., Gerstel, A., Hendrix, L.H., Yang, Y.C. (2018). Social Relationships, Inflammation, and Cancer Survival. Cancer. Epidemiol Biomarkers Prev, 27(5), 541-549. https://doi.org/10.1158/1055-9965.EPI-17-0836
Bretthauer M, Wieszczy P, Løberg M, et al. (2023). Estimated Lifetime Gained With Cancer Screening Tests: A Meta-Analysis of Randomized Clinical Trials. JAMA Intern Med. 183(11),1196–1203. https://doi.org/10.1001/jamainternmed.2023.3798Brown, K.F., Rumgay, H., Dunlop, C. et al. (2018). The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer, 118, 1130–1141. https://doi.org/10.1038/s41416-018-0029-6
CDC. (2023a). U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2022 submission data (1999-2020): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; released in November 2023. https://www.cdc.gov/cancer/dataviz
CDC. (2023b). Leading Causes of Death. National Center for health statistics, Centers for disease control and prevention. Accessed November 20, 2023. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
CSPH. (2021). Estimating annual expenditures for cancer screening in the United States. Center for Surgery and Public Health. Assessed November 14, 2023. https://csph.brighamandwomens.org/wp-content/uploads/2021/12/Estimating-Annual-Expenditures-for-Cancer-Screening-in-the-United-States.pdf
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., Li, X., Li, Y., Xiong. W., Li, G., Guo, C., & Zeng, Z. (2020). Chronic Stress Promotes Cancer Development. Front Oncol. 10, 1492. https://doi.org/10.3389/fonc.2020.01492
Feinberg, A. P. (2007). Phenotypic plasticity and the epigenetics of human disease. Nature, 447(7143), 433-440. https://doi.org/10.1038/nature05919
Fouad, Y. A., & Aanei, C. (2017). Revisiting the hallmarks of cancer. American journal of cancer research, 7(5), 1016. https://pubmed.ncbi.nlm.nih.gov/28560055/
Fracheboud, J. et al. (2004). Decreased rates of advanced breast cancer due to mammography screening in The Netherlands, British Journal of Cancer (2004) 91, 861–867. https://doi,org/10.1038/sj.bjc.6602075
Goldstein, B.D. (2001). The precautionary principle also applies to public health actions. Am J Public Health, 91(9),1358-61. https://doi.org/10.2105/ajph.91.9.1358
Gorter, R. & Peper, E. (2011). Fighting Cancer-A None Toxic Approach to Treatment. Berkeley: North Atlantic/New York: Random House. https://www.amazon.com/Fighting-Cancer-Nontoxic-Approach-Treatment/dp/1583942483
Gupta, P. B., Pastushenko, I., Skibinski, A., Blanpain, C., & Kuperwasser, C. (2019). Phenotypic plasticity: driver of cancer initiation, progression, and therapy resistance. Cell Stem Cell, 24(1), 65-78. https://doi.org/10.1016/j.stem.2018.11.011
Hanahan, Douglas. (2022): Hallmarks of cancer: new dimensions. Cancer discovery, 12(1), 31-46. https://doi.org/10.1158/2159-8290.CD-21-1059
Holt-Lunstad, J., Smith, T.B., & Layton, J.B. (2010). Social Relationships and Mortality Risk: A Meta-analytic Review, PLoS Med 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316
Huang, C., Zhang, C,, Cao, Y., Li, J., & Bi, F. (2023). Major roles of the circadian clock in cancer. Cancer Biol Med, 20(1):1–24. https://doi.org/10.20892/j.issn.2095-3941.2022.0474
Kalaf, J.M. (2014). Mammography: a history of success and scientific enthusiasm. Radiol Bras. 47(4):VII-VIII. https://doi.org/10.1590/0100-3984.2014.47.4e2
Key TJ, Bradbury KE, Perez-Cornago A, Sinha R, Tsilidis KK, Tsugane S. Diet, nutrition, and cancer risk: what do we know and what is the way forward? BMJ. 2020 Mar 5;368:m511. https://doi.org/10.1136/bmj.m511
Kowalski, A.E. (2021). Mammograms and mortality: How has the evidence evolved? J Econ Perspect, 35(2), 119-140. https://doi.org/10.1257/jep.35.2.119
LeShan, L. (1994). Cancer as a turning point. New York: Plume. https://www.amazon.com/Cancer-As-Turning-Point-Professionals/dp/0452271371
Lewis, T. (2022). The U.S. just lost 26 years’ worth of progress on life expectancy. Scientific American. October 17, 2022. Accessed November 11, 2023. https://www.scientificamerican.com/article/the-u-s-just-lost-26-years-worth-of-progress-on-life-expectancy/
Ma, X., Wang, R., Long, J.B., Ross, J.S., Soulos, P.R., Yu, J.B., Makarov, D.V., Gold, H.T. and Gross, C.P. (2014), The cost implications of prostate cancer screening in the Medicare population. Cancer, 120: 96-102. https://doi.org/10.1002/cncr.28373
Mentella, M.C., Scaldaferri, F., Ricci, C., Gasbarrini, A., & Miggiano, G.A.D. (2019). Cancer and Mediterranean Diet: A Review. Nutrients,11(9):2059. https://doi.org/10.3390/nu11092059
NIH NCI (2023). Physical Activity and Cancer. National Institutes of Health National Cancer Institute. Accessed November 18, 2023. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/physical-activity-fact-sheet
Patel, A,V., Friedenreich, C.M., Moore, S.C, et al. (2019). American College of Sports Medicine Roundtable Report on physical activity, sedentary behavior, and cancer prevention and control. Medicine and Science in Sports and Exercise, 51(11), 2391-2402. https://doi.org/10.1249/MSS.0000000000002117
Rabin, R.C. (2018). Can eating organic food lower your cancer risk? The New York Times. Oct 23, 2018. Accessed November 17, 2023. https://www.nytimes.com/2018/10/23/well/eat/can-eating-organic-food-lower-your-cancer-risk.html
Reuben, S.H. (2010). Reducing environmental cancer risk – What We Can Do Now. The President’s Cancer Panel Report. Washington, D.C: U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES, National Institutes of Health, National Cancer Institute. https://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp08-09rpt/PCP_Report_08-09_508.pdf
Rosenbaum, E. H. & Rosenbaum, I.R. (2023) The Will to Live. Stanford Center for Integrative Medicine. Surviving Cancer. Accessed November 23, 2023. https://med.stanford.edu/survivingcancer/cancers-existential-questions/cancer-will-to-live.html
Salazar, S.M.D.C., Dino, M.J.S., & Macindo, J.R.B. (2023). Social connectedness and health-related quality of life among patients with cancer undergoing chemotherapy: a mixed method approach using structural equation modelling and photo-elicitation. J Clin Nurs. Published online March 9, 2023. https://doi.org/10.1111/jocn.16675
Schmutzler, R. K., Schmitz-Luhn, B., Borisch, B., Devilee, P., Eccles, D., Hall, P., … & Woopen, C. (2022). Risk-adjusted cancer screening and prevention (RiskAP): complementing screening for early disease detection by a learning screening based on risk factors. Breast Care, 17(2), 208-223. https://doi.org/10.1159/000517182
Song, M., & Giovannucci, E. (2016). Preventable incidence and mortality of carcinoma associated with lifestyle factors among white adults in the United States. JAMA Ooncology, 2(9), 1154-1161. https://doi.org/10.1001/jamaoncol.2016.0843
Spei, M.E., Samoli, E., Bravi, F., et al. (2019). Physical activity in breast cancer survivors: A systematic review and meta-analysis on overall and breast cancer survival. Breast, 44,144-152. https://doi.org/10.1016/j.breast.2019.02.001
Stagl, J.M., Lechner, S.C., Carver, C.S. et al. (2015). A randomized controlled trial of cognitive-behavioral stress management in breast cancer: survival and recurrence at 11-year follow-up. Breast Cancer Res Treat, 154, 319–328. https://doi.org/10.1007/s10549-015-3626-6
Stratton, K., Shetty, P., Wallace, R., et al., eds. (2001). Institute of Medicine (US) Committee to Assess the Science Base for Tobacco Harm Reduction. Washington (DC): National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK222369/
Tailor, T.D,, Bell, S., Fendrick, A.M., & Carlos, R.C. (2022) Total and Out-of-Pocket Costs of Procedures After Lung Cancer Screening in a National Commercially Insured Population: Estimating an Episode of Care. J Am Coll Radiol. 19(1 Pt A), 35-46. https://doi.org/10.1016/j.jacr.2021.09.015
Turner, M.C., Andersen, Z.J., Baccarelli, A., Diver, W.R., Gapstur, S.M., Pope, C.A 3rd, Prada, D., Samet, J., Thurston, G., & Cohen, A. (2020). Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J Clin, 10.3322/caac.21632. https://doi.org/10.3322/caac.21632
US Department of Health and Human Services (2014). The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: :
US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. https://aahb.org/Resources/Pictures/Meetings/2014-Charleston/PPT%20Presentations/Sunday%20Welcome/Abrams.AAHB.3.13.v1.o.pdf
Van Tulleken, C. (2023). Ultra-processed people. The science behind food that isn’t food. New Yoerk: W.W. Norton & Company. https://www.amazon.com/gp/product/1324036729/ref=ox_sc_act_title_1?smid=ATVPDKIKX0DER&psc=1
Eat what grows in season
Posted: December 14, 2021 Filed under: health, Nutrition/diet, self-healing | Tags: food, herbicide, organic foods, pesticides Leave a commentAndrea Castillo and Erik Peper

We are what we eat. Our body is synthesized from the foods we eat. Creating the best conditions for a healthy body depends upon the foods we ingest as implied by the phrase, Let food be thy medicine, attributed to Hippocrates, the Greek founder of western medicine (Cardenas, 2013). The foods are the building blocks for growth and repair. Comparing our body to building a house, the building materials are the foods we eat, the architect’s plans are our genetic coding, the care taking of the house is our lifestyle and the weather that buffers the house is our stress reactions. If you build a house with top of the line materials and take care of it, it will last a life time or more. Although the analogy of a house to the body is not correct since a house cannot repair itself, it is a useful analogy since repair is an ongoing process to keep the house in good shape. Our body continuously repairs itself in the process of regeneration. Our health will be better when we eat organic foods that are in season since they have the most nutrients.
Organic foods have much lower levels of harmful herbicides and pesticides which are neurotoxins and harmful to our health (Baker et al., 2002; Barański, et al, 2014). Crops have been organically farmed have higher levels of vitamins and minerals which are essential for our health compared to crops that have been chemically fertilized (Peper, 2017),
Even seasonality appears to be a factor. Foods that are outdoor grown or harvested in their natural growing period for the region where it is produced, tend to have more flavor that foods that are grown out of season such as in green houses or picked prematurely thousands of miles away to allow shipping to the consumer. Compare the intense flavor of small strawberry picked in May from the plant grown in your back yard to the watery bland taste of the great looking strawberries bought in December.
The seasonality of food
It’s the middle of winter. The weather has cooled down, the days are shorter, and some nights feel particularly cozy. Maybe you crave a warm bowl of tomato soup so you go to the store, buy some beautiful organic tomatoes, and make yourself a warm meal. The soup is… good. But not great. It is a little bland even though you salted it and spiced it. You can’t quite put your finger on it, but it feels like it’s missing more tomato flavor. But why? You added plenty of tomatoes. You’re a good cook so it’s not like you messed up the recipe. It’s just—missing something.
That something could easily be seasonality. The beautiful, organic tomatoes purchased from the store in the middle of winter could not have been grown locally, outside. Tomatoes love warm weather and die when days are cooler, with temperatures dropping to the 30s and 40s. So why are there organic tomatoes in the store in the middle of cold winters? Those tomatoes could’ve been grown in a greenhouse, a human-made structure to recreate warmer environments. Or, they could’ve been grown organically somewhere in the middle of summer in the southern hemisphere and shipped up north (hello, carbon emissions!) so you can access tomatoes year-round.
That 24/7 access isn’t free and excellent flavor is often a sacrifice we pay for eating fruits and vegetables out of season. Chefs and restaurants who offer seasonal offerings, for example, won’t serve bacon, lettuce, tomato (BLT) sandwiches in winter. Not because they’re pretentious, but because it won’t taste as great as it would in summer months. Instead of winter BLTs, these restaurants will proudly whip up seasonal steamed silky sweet potatoes or roasted brussels sprouts with kimchee puree.
When we eat seasonally-available food, it’s more likely we’re eating fresher food. A spring asparagus, summer apricot, fall pear, or winter grapefruit doesn’t have to travel far to get to your plate. With fewer miles traveled, the vitamins, minerals, and secondary metabolites in organic fruits and vegetables won’t degrade as much compared to fruits and vegetables flown or shipped in from other countries. Seasonal food tastes great and it’s great for you too.
If you’re curious to eat more of what’s in season, visit your local farmers market if it’s available to you. Strike up a conversation with the people who grow your food. If farmers markets are not available, take a moment to learn what is in season where you live and try those fruits and vegetables next time to go to the store. This Seasonal Food Guide for all 50 states is a great tool to get you started.
Once you incorporate seasonal fruits and vegetables into your daily meals, your body will thank you for the health boost and your meals will gain those extra flavors. Remember, you’re not a bad cook: you just need to find the right seasonal partners so your dinners are never left without that extra little something ever again.
Sign up for Andrea Castillo’s Seasonal, a newsletter that connects you to the Bay Area food system, one fruit and vegetable at a time. Andrea is a food nerd who always wants to know the what’s, how’s, when’s, and why’s of the food she eats.
References
Baker, B.P., Benbrook, C.M., & Groth III, E., & Lutz, K. (2002). Pesticide residues in conventional, integrated pest management (IPM)-grown and organic foods: insights from three US data sets. Food Additives and Contaminants, 19(5) http://www.tandfonline.com/doi/abs/10.1080/02652030110113799
Barański, M., Średnicka-Tober, D., Volakakis, N., Seal, C., Sanderson, R., Stewart, G., . . . Leifert, C. (2014). Higher antioxidant and lower cadmium concentrations and lower incidence of pesticide residues in organically grown crops: A systematic literature review and meta-analyses. British Journal of Nutrition, 112(5), 794-811. https://doi.org/10.1017/S0007114514001366
Cardenas, E. (2013). Let not thy food be confused with thy medicine: The Hippocratic misquotation,e-SPEN Journal, I(6), e260-e262. https://doi.org/10.1016/j.clnme.2013.10.002
Peper, E. (2017). Yes, fresh organic food is better! the peper perspective. https://peperperspective.com/2017/10/27/yes-fresh-organic-food-is-better/
Yes, fresh organic food is better!
Posted: October 27, 2017 Filed under: Nutrition/diet, self-healing | Tags: farming, Holistic health, longevity, non-organic foods, nutrition, organic foods, pesticides 6 Comments
Is it really worthwhile to spent more money on locally grown organic fruits and vegetables than non-organic fruits and vegetables? The answer is a resounding “YES!” Organic grown foods have significantly more vitamins, antioxidants and secondary metabolites such as phenolic compounds than non-organic foods. These compounds provide protective health benefits and lower the risk of cancer, cardiovascular disease, type two diabetes, hypertension and many other chronic health conditions (Romagnolo & Selmin, 2017; Wilson et al., 2017; Oliveira et al., 2013; Surh & Na, 2008). We are what we eat–we can pay for it now and optimize our health or pay more later when our health has been compromised.
The three reasons why fresh organic food is better are:
- Fresh foods lengthen lifespan.
- Organic foods have more vitamins, minerals, antioxidants and secondary metabolites than non-organic foods.
- Organic foods reduce exposure to harmful neurotoxic and carcinogenic pesticide and herbicides residues.
Background
With the advent of chemical fertilizers farmers increased crop yields while the abundant food became less nutritious. The synthetic fertilizers do not add back all the necessary minerals and other nutrients that the plants extract from the soil while growing. Modern chemical fertilizers only replace three components–Nitrogen, Phosphorus and Potassium–of the hundred of components necessary for nutritious food. Nitrogen (N) which promotes leaf growth; Phosphorus (P which development of roots, flowers, seeds, fruit; and Potassium (K) which promotes strong stem growth, movement of water in plants, promotion of flowering and fruiting. These are great to make the larger and more abundant fruits and vegetables; however, the soil is more and more depleted of the other micro-nutrients and minerals that are necessary for the plants to produce vitamins and anti-oxidants. Our industrial farming is raping the soils for quick growth and profit while reducing the soil fertility for future generations. Organic farms have much better soils and more soil microbial activity than non-organic farm soils which have been poisoned by pesticides, herbicides, insecticides and chemical fertilizers (Mader, 2002; Gomiero et al, 2011). For a superb review of Sustainable Vs. Conventional Agriculture see the web article: https://you.stonybrook.edu/environment/sustainable-vs-conventional-agriculture/
1. Fresh young foods lengthen lifespan. Old foods may be less nutritious than young food. Recent experiments with yeast, flies and mice discovered that when these organisms were fed old versus young food (e.g., mice were diets containing the skeletal muscle of old or young deer), the organisms’ lifespan was shortened by 18% for yeast, 13% for flies, and 13% for mice (Lee et al., 2017). Organic foods such as potatoes, bananas and raisins improves fertility, enhances survival during starvation and decreases long term mortality for fruit flies(Chhabra et al, 2013). See Live longer, enhance fertility and increase stress resistance: Eat organic foods. https://peperperspective.com/2013/04/21/live-longer-enhance-fertility-and-increase-stress-resistance-eat-organic-foods/
In addition, eating lots of fruits and vegetables decreases our risk of dying from cancer and heart disease. In a superb meta-analysis of 95 studies, Dr. Dagfinn Aune from the School of Public Health, Imperial College London, found that people who ate ten portions of fruits and vegetable per day were a third less likely to die than those who ate none (Aune et al, 2017). Thus, eat lots of fresh and organic fruits and vegetables from local sources that is not aged because of transport.
2. Organic foods have more vitamins, minerals, antioxidants and secondary metabolites than non-organic foods. Numerous studies have found that fresh organic fruits and vegetables have more vitamins, minerals, antioxidants, and secondary metabolites than non-organic ones. For example, organic tomatoes contain 57 per cent more vitamin C than non-organic ones (Oliveira et al 2013) or organic milk has more beneficial polyunsaturated fats non-organic milk (Wills, 2017; Butler et al, 2011). Over the last 50 years key nutrients of fruits and vegetables have declined. In a survey of 43 crops of fruits and vegetables, Davis, Epp, & Riordan, (2004) found a significant decrease of vitamins and minerals in foods grown in the 1950s as compared to 1999 as shown in Figure 1 (Lambert, 2015).
Figure 1. Change in vitamins and minerals from 1950 to 1999. From: Davis, D. R., Epp, M. D., & Riordan, H. D. (2004). Changes in USDA food composition data for 43 garden crops, 1950 to 1999. Journal of the American College of Nutrition, 23(6), 669-682.
3, Organic foods reduce exposure to harmful neurotoxic and carcinogenic pesticide and herbicides residues. Even though, the United States Department of Agriculture (USDA) and the United States Environmental Protection Agency (EPA) state that pesticide residues left in or on food are safe and non-toxic and have no health consequences, I have my doubts! Human beings accumulate pesticides just like tuna fish accumulates mercury—frequent ingesting of very low levels of pesticide and herbicide residue may result in long term harmful effects and these long term risks have not been assessed. Most pesticides are toxic chemicals and were developed to kill agricultural pests — living organisms. Remember human beings are living organisms. The actual risk for chronic low level exposure is probably unknown; since, the EPA pesticide residue limits are the result of a political compromise between scientific findings and lobbying from agricultural and chemical industries (Portney, 1992). Organic diets expose consumers to fewer pesticides associated with human disease (Forman et al, 2012).
Adopt the precautionary principle which states, that if there is a suspected risk of herbicides/pesticides causing harm to the public, or to the environment, in the absence of scientific consensus, the burden of proof that it is not harmful falls on those recommending the use of these substances (Read & O’Riordan, 2017). Thus, eat fresh locally produced organic foods to optimize health.
References
Butler, G. Stergiadis, s., Seal, C., Eyre, M., & Leifert, C. (2011). Fat composition of organic and conventional retail milk in northeast England. Journal of Dairy Science. 94(1), 24-36.http://dx.doi.org/10.3168/jds.2010-3331
Davis, D. R., Epp, M. D., & Riordan, H. D. (2004). Changes in USDA food composition data for 43 garden crops, 1950 to 1999. Journal of the American College of Nutrition, 23(6), 669-682. http://www.chelationmedicalcenter.com/!_articles/Changes%20in%20USDA%20Food%20Composition%20Data%20for%2043%20Garden%20Crops%201950%20to%201999.pdf
Lambert, C. (2015). If Food really better from the farm gate than super market shelf? New Scientist.228(3043), 33-37.
Oliveira, A.B., Moura, C.F.H., Gomes-Filho, E., Marco, C.A., Urban, L., & Miranda, M.R.A. (2013). The Impact of Organic Farming on Quality of Tomatoes Is Associated to Increased Oxidative Stress during Fruit Development. PLoS ONE, 8(2): e56354. https://doi.org/10.1371/journal.pone.0056354
Read, R. and O’Riordan, T. (2017). The Precautionary Principle Under Fire. Environment-Science and policy for sustainable development. September-October. http://www.environmentmagazine.org/Archives/Back%20Issues/2017/September-October%202017/precautionary-principle-full.html
Romagnolo, D. F. & Selmin, O.L. (2017). Mediterranean Diet and Prevention of Chronic Diseases. Nutr Today. 2017 Sep;52(5):208-222. doi: 10.1097/NT.0000000000000228. https://www.ncbi.nlm.nih.gov/pubmed/29051674
Wills, A. (2017). There is evidence organic food is more nutritious. New Scientist,3114, p53.
Wilson, L.F., Antonsson, A., Green, A.C., Jordan, S.J., Kendall, B.J., Nagle, C.M., Neale, R.E., Olsen, C.M., Webb, P.M., & Whiteman, D.C. (2017). How many cancer cases and deaths are potentially preventable? Estimates for Australia in 2013. Int J Cancer. 2017 Oct 6. doi: 10.1002/ijc.31088. https://www.ncbi.nlm.nih.gov/pubmed/28983918
Live longer, enhance fertility and increase stress resistance: Eat organic foods
Posted: April 21, 2013 Filed under: Nutrition/diet, Uncategorized | Tags: diet, fertility, organic foods, pesticide, stress 5 CommentsHealth food advocates have long claimed that organic foods are better for your health because they have more nutrients and fewer pesticides than non organic or genetically modified grown foods. On the other hand, the USDA and agribusiness tend to claim that organically grown foods have no additional benefits. Until now, much of the published research appeared inconclusive and meta-analysis appeared to indicate that there are no health benefits from organic as compared to non organic foods although organic foods did reduce eczema in infants (Dangour et al, 2010).
Food studies that have demonstrated no benefits of organic farmed foods as compared to non-organic or genetically modified crops should be viewed with skepticism since many of these studies have been funded directly or indirectly by agribusiness. On the other hand, independently funded research studies have tended to demonstrate that organic foods are more beneficial than non-organic foods. Sadly, the United States Department of Agriculture (USDA) and agribusiness are highly interdependent as the USDA both regulates and promotes agricultural products. On the one hand the USDA’s mission is “To expand economic opportunity through innovation, helping rural America to thrive; to promote agriculture production” and on the other hand “Enhance food safety by taking steps to reduce the prevalence of food borne hazards from farm to table, improving nutrition and health by providing food assistance and nutrition education and promotion. (For more discussion on the conflict of interest between agribusiness and the USDA, see Michael Pollan’s superb books, The Omnivore’s Dilemma: A Natural History of Four Meals and In Defense of Food: An Eater’s Manifest).
Historically, most nutritional studies have investigated the nutritional difference or pesticide residue between organic and non-organically farmed. Many studies have shown that organic grown foods have significantly lower pesticide residues than non organic foods (Baker et al, 2002; Luc, 2006). Even though agribusiness and the USDA tend to state that the pesticide residues left in or on the food are safe and non-toxic and have no health consequences, I have my doubts. Human beings accumulate pesticides just like tuna fish accumulates mercury—frequent ingesting of very low levels of pesticides residue may result in long term harmful effects. One way to measure if there is an effect of organic, non organic or genetically modified grown foods or residual pesticides is to do a long term follow up and measure the impact over the lifespan of the organism. This is difficult with human beings; since, it would take 50 or more years to observe the long term effects. Nevertheless, the effects of organically grown foods versus non-organically grown foods upon lifespan, fertility and stress resistance has now been demonstrated with fruit flies.
The elegant research by Chhabra R, Kolli S, Bauer JH (2013) showed that when fruit flies were fed either organic bananas, potatoes, soy or raisins, they demonstrated a significant increase in longevity, fertility and stress resistance as compared to eating non-organic bananas, potatoes, soy and raisins. In this controlled study, the outcome data is stunning. Below are some of their results reproduced from their article, “Organically Grown Food Provides Health Benefits to Drosophila melanogaster.”
Figure 1. Longevity of D. melanogaster fed organic diets. Survivorship curves of female fruit flies fed diets made from extracts of potatoes, raisins, bananas or soybeans (grey: conventional food; black: organic food; statistically significant changes (p,0.005) are indicated by asterisks).Median survival times of flies on conventional and organics food sources, respectively, are: potatoes: 16 and 22 days (,38% longevity increase,p,0.0001); soybeans: 8 and 14 days (,75% longevity increase, p,0.0001).doi:10.1371/journal.pone.0052988.g001. Reproduced from Chhabra R, Kolli S, Bauer JH (2013).
Figure 2. Daily egg-laying of flies exposed to organic diets. Egg production of flies fed the indicated food was determined daily. Shown are the averages of biological replicates; error bars represent the standard deviation (grey: conventional food; black: organic food; statistically significant changes (p,0.005) are indicated by asterisks; p,0.0001 for all food types). doi:10.1371/journal.pone.0052988.g002. Reproduced from Chhabra R, Kolli S, Bauer JH (2013).
Figure 3. Starvation tolerance of flies raised on organic diets. Survivorship curves of female flies raised for 10 days on the indicated food sources. Flies were then transferred to starvation media and dead flies were counted twice daily (grey: conventional food; black: organic food; statistically significant changes (p,0.005) are indicated by asterisks). Median survival times of flies on conventional and organics food sources, respectively, are: potatoes: 6 and 24 hours (p,0.0001); bananas: 24 and 48 hours (p,0.0001). doi:10.1371/journal.pone.0052988.g003. Reproduced from Chhabra R, Kolli S, Bauer JH (2013)
This elegant study demonstrated the cumulative impact of organic versus non-organic food source upon survival fitness. It demonstrated that non-organic foods decreased the overall health of the organism which may be due to the lower levels of essential nutrients, presence of pesticides or genetic modified factors.
The take home message of their research is: If you are concerned about your health, want to live healthier and longer, improve fertility and resist stress, eat organically grown fruits and vegetable. Although this research was done with fruit flies and human beings are not fruit flies since we eat omnivorously, it may still be very relevant especially for children. As children grow the ingestion of non-organic foods may cause a very low level nutrient malnutrition coupled with an increased exposure to pesticides. The same concept can be extended to meats and fish. Eat only meat from free ranging animals that have been fed organic grown foods and not been given antibiotics or hormones to promote growth.
Bon appétit
.References
Baker, B.P., Benbrook, C.M., & Groth III, E., & Lutz, K. (2002). Pesticide residues in conventional, integrated pest management (IPM)-grown and organic foods: insights from three US data sets. Food Additives and Contaminants, 19(5) http://www.tandfonline.com/doi/abs/10.1080/02652030110113799
Chhabra R, Kolli S, Bauer JH (2013) Organically Grown Food Provides Health Benefits to Drosophila melanogaster. PLoS ONE 8(1): e52988. doi:10.1371/journal.pone.0052988 http://www.plosone.org/article/info:doi%2F10.1371%2Fjournal.pone.0052988
Dangour, A.D., Lock, K., Hayter, A., Aikenhead, A., Allen, E., Uauy, R. (2010). Nutrition related health effects of organic foods: a systematic review. Am J Clin Nutr, 92,203–210. http://ajcn.nutrition.org/content/92/1/203.short
Luc, C., Toepel, K., Irish, R., Fenske, R.A., Barr, D.B., & Bravo, R. (2006). Organic Diets Significantly Lower Children’s Dietary Exposure to Organophosphorus Pesticides. Environ Health Perspect, 114(2), 260–263. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1367841/
Pollan, M. (2009). In Defense of Food: An Eater’s Manifesto. New York: Penguin Press. ISBN: 978-0143114963
Pollan, M. (2006). The Omnivore’s Dilemma: A Natural History of Four Meals. New York: Penguin Press. ISBN: 1594200823


