Integrative Medicine: NATO’s Task Force Report
Posted: January 24, 2016 Filed under: Uncategorized | Tags: CAM, complementary medicine, integrative medicine 1 CommentNorth Atlantic Treaty Organization’s Task Force Human Factors and Medicine (HFM)-195 has just published the results of their deliberations on integrative medicine interventions for military personal. The findings were published as NATO Special Edition-Integrative Medicine Interventions for Military Personnel in the October 2015 issue of Medical Acupuncture, 27(5). The individual articles range from historical perspectives to analysis of clinical applications of CAM. The individual articles can be downloaded – free of charge – from http://online.liebertpub.com/toc/acu/27/5.
The articles point out that the current health care system must adapt and include the utilization of complementary and alternative medicine (CAM). It is not main stream medicine versus CAM. It is how to integrate the best of both approaches and offer the most effective integrative medicine. The objectives of the report are:
- To improve health care systems and increase available treatment options for patients.
- To identify and to evaluate the various countries’ data on the utilization (rationale, frequency, accessibility) of CAM among Military personnel.
- To learn about the acceptability of CAM by the leadership of Military organizations, and review briefly the current regulatory and legal status of CAM utilization and its implementation.
- To explore NATO-wide implementation of selected CAM modalities (e.g., acupuncture, meditation/mindfulness programs, movement/yoga, biofeedback), with ongoing analysis of efficacy, cost-effectiveness, suitability, and acceptability.
- To develop acceptable terminology, regulatory policies, and educational literature.
- To expand perspectives and understanding of cross cultural initiatives and research project.
Look at the articles in the journal. It is a great resource.
Letting go of stress and worry*
Posted: January 15, 2016 Filed under: Uncategorized | Tags: mindfulness, stress management, visualization, worry 7 Comments One evening an old Cherokee told his grandson about a battle that goes on inside people. He said, “My son, the battle is between two wolves inside us all.”
One evening an old Cherokee told his grandson about a battle that goes on inside people. He said, “My son, the battle is between two wolves inside us all.”
“One is Evil – It is anger, envy, jealousy, sorrow, regret, greed, arrogance, self-pity, guilt, resentment, inferiority, lies, false pride, superiority, and ego.”
“The other is Good – It is joy, peace, love, hope, serenity, humility, kindness, benevolence, empathy, generosity, truth, compassion and faith.”
The grandson thought about it for a minute and then asked his grandfather: “Which wolf wins?”
The old Cherokee simply replied, “The one you feed.”
–Author and source unknown
Are you stressed and worrying what will happen? Are you thinking of all that could go wrong? Do you feel overwhelmed and anxious?
It is very challenging to let go of negative thoughts, images, memories and anticipations. These negative worries can be useful if they mobilize you towards active planning and action; however, in most cases, the thoughts continue to go around and around in our heads. The more we worry, the worse we feel. Often our shoulders and neck tighten and our stomach churns. The worries and concerns may become a pain in the neck and we no longer can stomach the stress.
Begin to take charge and realize that even though health and healing is not our control, we can contribute and support the healing process. Regardless how overwhelmed we are, begin with the basics. Start the day by respecting your body so that it can run well. It needs:
Proper fuel. Begin by having breakfast—not the sugar coated cereals or snack bars on the run—but an egg, oatmeal, and some fruit or other non-processed foods. Even when you think you do not have the time, fuel up your body so your body engine can work well. Drink only one cup of coffee with little sugar. Drink water or tea and avoid all soft drinks and any low calorie drinks. Remember that people who drink low calorie soft drinks increase their abdominal girth by three inches as compared to people who do not drink low calorie soft drinks (Fowler et al, 2015).
Follow-up with lunch and dinner, do not skip meals! Many of my college students do not eat breakfast or lunch before coming to class, as a group they are more reactive, anxious and perform significantly poorer on exams than the ones who do eat.
If you haven’t eaten, or eaten only high sugary snack foods an hour or two before, your blood sugar will lower and you become more reactive “Hangry” (the combination of hungry and angry). As the blood sugar drops, the brain reactivity pattern changes and you become much more impulsive (Peper et al, 2009).
Dynamic movement. The moment you do some movement your urge to snack, smoke, or ruminate is significantly reduced. When you begin physical movement (especially when you do not want to), the built up tension from the personal and interpersonal stress will decrease. You are completing the biological alarm reaction. When you physically move, you dissipate the fight/flight response and are shifting your body to a state of regeneration. As the alarm reaction response decreases, it becomes easier to do problem solving and abstract thinking. As long as you are in the alarm state, you tend to react defensively to the immediate events. Thus, when you feel uptight and stressed, take a hike. Walk up the stairs instead of taking the escalator, get off Muni one stop earlier and walk rapidly to your destination.
Positive and peaceful thoughts. Remember your thoughts, memories and images affect your body and vice versa. Experience how your thoughts effect your body. Have someone read the following to you. It takes only a few minutes.
Sit comfortably, and gently close your eyes and imagine a lemon. Notice the deep yellow color, and the two stubby ends. Imagine placing the lemon on a cutting board and cutting it in half with your favorite kitchen knife. Notice the pressure of the knife in your hand as you cut the lemon. Feel the drop of lemon juice against your skin. After cutting the lemon in half, put the knife down and pick up one half of the lemon.

As you look at it, notice the drops of juice glistening in the light, the half-cut seeds, the outer yellow rind, and the pale inner rind. Now get a glass and squeeze this half of lemon so the juice goes into the glass. As you squeeze, notice the pressure in your fingers and forearm. Feel droplets of lemon juice squirting against your skin. Smell the pungent, sharp fragrance. Now take the other half of lemon and squeeze the juice into the glass. Now take the glass in your hand. Feel the coolness of the glass and bring it to your lips. Feel the juice against your lips, and then sip the lemon juice. Taste the tart juice and swallow the lemon juice. Observe the pulp and seeds as you swallow (Adapted from Gorter and Peper, 2011).
What did you notice? As you imagined the lemon, did you notice that you experienced an increase in salivation, or that your mouth puckered? Almost everyone who does this exercise experiences some of these physical changes. The increase in salivation demonstrates that these thoughts and images have a direct effect on our bodies. Similarly, when we have thoughts of anger, resentment, frustration, or anxiety, they also affect our bodies. Unknowingly we may tighten our shoulders or our abdomen. We may unconsciously hold our breath or breathe shallowly. This response interferes with our ability to relax and heal. If this kind of tension is a constant habit, it reduces the body’s ability to regenerate.
Although we may dismiss our experience when we did the imagery exercise with an imaginary lemon—it was only an imaginary lemon, after all—it is fundamentally important. Every minute, every hour, every day, our bodies are subtly affected by thoughts, emotions, and images. Just as the image of the lemon caused us to salivate, our thoughts and emotions also cause physiological change.
What to do when consumed by worry. Although it seems impossible, you have a choice to focus on the negative or positive thoughts. When you feel stressed and overwhelmed, ask yourself, do I have control over this situation?
If “No”, acknowledge that you feel frustrated and stuck. Recognize you want to let it go and have no control. Ask yourself “does this thought serve any purpose or help me in any way” If not, let go of the thought and the sensations in your body” If there is a purpose or value act upon the thought (go feed the parking meter, make that call). Then do the following thought interrupting practice.
Sit up and make yourself tall on your sitz bones with your lower spine slightly arched at the same time look up and take a breath in. While inhaling, think of someone who loves you such as your grandmother an aunt. For that moment feel their love. Exhale softly while slightly smiling while still looking upward. As you exhale think of someone for whom you care for and wish them well.
Each time your brain begins to rehash that specific event, do not argue with it, do not continue with it, instead, initiate the thought interrupting practice. Many people report when they do this many, many, times a day, their energy, mood and productivity significantly increases. Initially it seems impossible, yet, the more you practice, the more the benefits occur.
If “yes,” make a list of all the things over which you have control and that need to be done. Acknowledge that this list appears overwhelming and you do not even know where to start. Begin by doing one small project. Remember, you do not have to finish it today. It is a start. And, if possible, share your list and challenge with friends or family members and ask them for support. The most important part is to move into action. Then, each time your brain worries, “I do not have enough time”, or “there is too much to do,” practice the thought interrupting practice.
Watch your thoughts; they become words.
Watch your words; they become actions.
Watch your actions; they become habits.
Watch your habits; they become character.
Watch your character; it becomes you
– Frank Outlaw (1977)
Reference:
Fowler, S. P., Williams, K., & Hazuda, H. P. (2015). Diet Soda Intake Is Associated with Long‐Term Increases in Waist Circumference in a Biethnic Cohort of Older Adults: The San Antonio Longitudinal Study of Aging. Journal of the American Geriatrics Society, 63(4), 708-715. http://onlinelibrary.wiley.com/doi/10.1111/jgs.13376/pdf
Peper, E., Harvey, R., Takabayashi, N., & Hughes, P. (2009). How to do clinical biofeedback in psychosomatic medicine: An illustrative brief therapy example for self-regulation. Japanese Journal of Biofeedback Research..36 (2), 1-16. https://biofeedbackhealth.files.wordpress.com/2011/01/howdoyouclinicalbiofeedback19.pdf
Gorter, R. & Peper, E. (2011). Fighting Cancer-A Non Toxic Approach to Treatment. Berkeley: North Atlantic: Random House. http://www.amazon.com/Fighting-Cancer-Nontoxic-Approach-Treatment-ebook/dp/B004C43GAQ/ref=sr_1_1?s=books&ie=UTF8&qid=1452923651&sr=1-1&keywords=fighting+cancer
Outlaw, F (1977). What They’re Saying Quote Page 7-B, San Antonio Light (NArch Page 28), Column 4, 1San Antonio, Texas, May 18, 1977 (NewspaperArchive).
*Adapted from: Peper, E. (2016). Legend of two wolves is a beacon across time for healthy thinking. Western Edition. January, pp 6, 8. http://thewesternedition.com/admin/files/magazines/WE-January-2016.pdf
Do medications work as promised? Ask questions!
Posted: January 13, 2016 Filed under: Uncategorized | Tags: antidepressants, medication, opiod, pharmaceuticals, risk-benefit, side effects, stress Leave a commentMedications can be beneficial and safe lives; however, some may not work as well as promised. In some cases, they may do more harm than good as illustrated by the following examples.
- There is weak or no evidence of effectiveness for the long term use of any opiod (morphine, fentanyl, oxycodone, methadone and hydrocodone) in the treatment of chronic pain (Perlin, 2015). As the Center for Disease Control and Prevention reports, “Since 1999, the amount of prescription painkillers prescribed and sold in the U.S. has nearly quadrupled, yet there has not been an overall change in the amount of pain that Americans report. Over prescribing leads to more abuse and more overdose deaths.” More than 16,000 people a year die from prescription drug overdose (CDC, 2016). For a superb discussion of the treatment of chronic pain, see the recently published book by Cindy Perlin, The truth about chronic pain treatments.
- Selective serotonin re-uptake inhibitor such as Paxil and Prozac (SSRI) are much less effective than promised by pharmaceutical companies. When independent researchers (not funded by pharmaceutical companies) re-analyzed the data from published and unpublished the studies, they found that the medication was no more effective than the placebo for the treatment of mild and moderate depression (Ioannidis, 2008; Le Noury et al, 2015). In addition, the SSRIs (paroxetine and Imipramine) in treatment of unipolar major depression in adolescence may cause significant harm which outweigh any possible benefits (Le Le Noury et al., 2015). On the other had, exercise appears as effective as antidepressants for reducing symptoms of mild to moderate depression (Cooney et al., 2013). Despite the questionable benefits of SSRI medications, pharmaceutic industry to posted $11.9 billion dollars in 2011 global sales (Perlin, 2015).
When medications are recommended, ask your provider the following questions (Robin, 1984; Gorter & Peper, 2011).
- Why are you prescribing the medication?
- What are the risks and negative side effects?
- Do the benefits outweigh the risks?
- How do I know when the medication is working?
- What will you do if the medication does not work?
- How many patients do you need to treat before one patient benefits?
- Can you recommend non-pharmaceutical options?
The important questions to ask are:
- How many patients need to be treated with the medication before one patient benefits?
- How many will experience negative side effects?
The data can be discouraging. As Daniel Levitin, neuroscientist at McGill University in Montreal and Dean at Minerva Schools in San Francisco, points out, it takes 300 people to take statins for one year before one heart attack, stroke or other serious event is prevented. However, 5% of all the people taken statins (the of drug of choice to lower cholesterol) will experience debilitating adverse effects such as severe muscle pain and gastrointestinal disorders. This means that you are 15 times more likely to suffer serious side effect than being helped by the drug. Nevertheless, the CDC reported that during 2011–2012, more than one-quarter (27.9%) of adults aged 40 and over used a prescription cholesterol-lowering medication (statins) (Gu, 2014).
Before making any medical decision when stressed, watch the superb 2015 TED London presentation by neuroscientist Daniel Levitin, How to think about making a decision under stress.
Reference:
CDC Center for Disease Control and Prevention (2016). Injury prevention & control: Prescription drug overdose. http://www.cdc.gov/drugoverdose/
Cooney, G.M., Dwan, K., Greig, C.A., Lawlor, D.A, Rimer, J., Waugh, F.R., McMurdo, M., & Mead, G. E.(2013). Exercise for depression. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No.: CD004366. DOI: 10.1002/14651858.CD004366.pub6.The Cochrane Library. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004366.pub6/epdf
Goter, R. & Peper, E. (2011). Fighting cancer: A nontoxic approach to treatment. Berkeley, CA: Noreth Atlantic Books.http://www.amazon.com/Fighting-Cancer-Nontoxic-Approach-Treatment/dp/1583942483/ref=sr_1_2_twi_pap_2?ie=UTF8&qid=1452715134&sr=8-2&keywords=gorter+and+peper
Gu, Q., Paulose-Ram, R., Burt, V.L., & Kit, B.K. (2014).Prescription Cholesterol-Lowering Medication Use in Adults Aged 40 and Over: United States, 2003–2012. NCHS Data Brief No. 177. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention National Center for Health Statistics.http://www.cdc.gov/nchs/data/databriefs/db177.pdf
Ioannidis, J. P. (2008). Effectiveness of antidepressants: an evidence myth constructed from a thousand randomized trials?. Philosophy, Ethics, and Humanities in Medicine, 3(1), 14. http://peh-med.biomedcentral.com/articles/10.1186/1747-5341-3-14
Le Noury, J., Nardo, J. M., Healy, D., Jureidini, J., Raven, M., Tufanaru, C., & Abi-Jaoude, E. (2015). Restoring Study 329: efficacy and harms of paroxetine and imipramine in treatment of major depression in adolescence. http://www.bmj.com/content/351/bmj.h4320.full
Levitin, D. (2015). How to stay calm when you know you’ be stressed. TEDGlobal London Talk http://www.ted.com/talks/daniel_levitin_how_to_stay_calm_when_you_know_you_ll_be_stressed
Perlin, C. (2015). The truth about chronic pain treatments. Delmar, NY: Morning Light Books, LLC. http://www.amazon.com/gp/product/B0160UEQB2/ref=dp-kindle-redirect?ie=UTF8&btkr=1
Robin, E.D. (1984). Matters of life & death: Risks vs. benefits of medical care. New York: W.H. Freeman and Company. http://www.amazon.com/Matters-Life-Death-Benefits-Medical/dp/071671681X/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=&sr=
Sharing gratitude
Posted: December 23, 2015 Filed under: Uncategorized | Tags: gratitude, healing, health, mind-body, stress management 4 CommentsIt was late in the afternoon and I was tired. A knock on my office door. One of my students came in and started to read to me from a card. “I want to thank you for all your help in my self-healing project…I didn’t know the improvements were possible for me in a span of 5 weeks…. I thank you so much for encouraging and supporting me…. I have taken back control of myself and continue to make new discoveries about my identity and find my own happiness and fulfillment.,,, Thank you so much.”
I was deeply touched and my eyes started to fill with tears. At that moment, I felt so appreciated. We hugged. My tiredness disappeared and I felt at peace.
This student had completed the daily self-healing practices . When the university students practice a sequence of daily self-healing exercises outlined in the book, Make Health Happen (Peper, Gibney & Holt, 2002), most report significant improvement in their health and well-being as shown in Figure 1 (Peper et al, 2014).
 Figure 1. Self-rating by students after completing a personal health improvement project over a period of four weeks (Bier, Peper, & Burke, 2005).
Figure 1. Self-rating by students after completing a personal health improvement project over a period of four weeks (Bier, Peper, & Burke, 2005).
The practice which students report impacts them profoundly and by which they experience a deepening connection and sense of agape (selfless unconditional caring and love) with another person is Sharing Gratitude.
Sharing Gratitude practice was adapted from Professor Martin Seligman’s 2004 TED presentation, The new era of positive psychology.
Take the opportunity during the holiday season to give joy to others. Just do the following:
- Remember someone who did something for you that impacted your life in a positive direction and whom you never properly thanked.
- Write a 300 word testimonial describing what the person did and how it positively impacted you.
- Visit the person and when you meet her/him, read the testimonial to her/him (if the person cannot be visited, use Skype so you can see and connect with each other).
Although it may seem awkward to read the testimonial, after you have done it, you most likely will feel closer and more deeply connected to the person. Moreover, the person to whom you read the testimonial, will feel deeply touched and both of your hearts will open.
For more background information, watch Professor Martin Seligman’s Ted presentation below.
References:
Bier, M., Peper, E., & Burke, A. (2005). Integrated Stress Management with Make Health Happen: Measuring the Impact through a 5-Month Follow-Up. Presented at the 36th Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract published in: Applied Psychophysiology and Biofeedback, 30(4), 400.
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt. ISBN-13: 978-0787293314
Peper, E., Lin, I-M, Harvey, R., Gilbert, M., Gubbala, P., Ratkovich, A., & Fletcher, F. (2014). Transforming chained behaviors: Case studies of overcoming smoking, eczema and hair pulling (trichotillomania). Biofeedback, 42(4), 154-160.
https://biofeedbackhealth.files.wordpress.com/2011/01/transforming-chained-behavior-published.pdf
Seligman, M. (2004). The new era of positive psychology. http://www.ted.com/index.php/talks/martin_seligman_on_the_state_of_psychology.html
Training Compassionate Presence
Posted: November 22, 2015 Filed under: Uncategorized | Tags: compassion, Dora Kunz, Energy healing, healing, Kawakami, Medicine, mindfulness, Muramatsu 3 Comments“Healing is best accomplished when art and science are conjoined, when body and spirit are probed together. Only when doctors can brood for the fate of a fellow human afflicted with fear and pain do they engage the unique individuality of a particular human being…a doctor thereby gains courage to deal with the pervasive uncertainties for which technical skill alone is inadequate. Patient and doctor then enter into a partnership as equals.
I return to my central thesis. Our health care system is breaking down because the medical profession has been shifting its focus away from healing, which begins with listening to the patient. The reasons for this shift include a romance with mindless technology.” Bernard Lown, MD, The Lost Art of Healing: Practicing Compassion in Medicine (1999)
I wanted to study with the healer and she instructed me to sit and observe, nothing more. She did not explain what she was doing, and provided no further instructions. Just observe. I did not understand. Yet, I continued to observe because she knew something, she did something that seemed to be associated with improvement and healing of many patients. A few showed remarkable improvement – at times it seemed miraculous. I felt drawn to understand. It was an unique opportunity and I was prepared to follow her guidance.

Three remarkable healers: Dora Kunz, Mitsumasa Kawakami and Norihiro Muramatsu.
The healer was remarkable. When she put her hands on the patient, I could see the patient’s defenses melt. At that moment, the patient seemed to feel safe, cared for, and totally nurtured. The patient felt accepted for just who she was and all the shame about the disease and past actions appeared to melt away. The healer continued to move her hands here and there and, every so often, she spoke to the client. Tears and slight sobbing erupted from the client. Then, the client became very peaceful and quiet. Eventually, the session was finished and the client expressed gratitude to the healer and reported that her lower back pain and the constriction around her heart had been released, as if a weight had been taken from her body.
How was this possible? I had so many questions to ask the healer: “What were you doing? What did you feel in your hands? What did you think? What did you say so softly to the client?” Yet, she did not help me understand how I could do this. The only instruction the healer kept giving me was to observe. Yes, she did teach me to be aware of the energy fields around the person and taught me how I could practice therapeutic touch (Kreiger, 1979; Kunz & Peper, 1995; Kunz & Krieger, 2004; Denison,2004; van Gelder & Chesley, F, 2015). But she was doing much more.
Sitting at the foot of the healer, observing for months, I often felt frustrated as she continued to insist that I just observe. How could I ever learn from this healer if she did not explain what I should do! Does the learning occur by activating my mirror neurons? Similar instructions are common in spiritual healing and martial arts traditions – the guru or mentor usually tells an apprentice to observe and be there. But how can one gain healing skills or spiritual healing abilities if you are only allowed to observe the process? Shouldn’t the healer be demonstrating actual practices and teaching skills?
After many sessions, I finally realized that the healer’s instruction to observe the healing was an indirect instruction. I began to learn how to be present without judging, to be present with compassion, to be present with total awareness in all senses, and to be present without frustration. The many hours at the foot of this master were not just wasted time. It eventually became clear that those hours of observation were important training and screening strategies used to insure that only those students who were motivated enough to master the discipline of non-judgmental observation, the discipline to be present and open to any experience, would continue to participate in the training process. It was training in compassionate mindfulness. Once apprentices achieved this state, they were ready to begin the work with clients and master the technical aspects of the specific healing art or spiritual practice.
A major component of the healing skill that relies on subtle energies is the ability to be totally present with the client without judgment (Peper, Gibney & Wilson, 2005; Peper, 2015). To be peaceful, caring, and present seems to create an energetic ambiance that sets stage, creates the space, for more subtle aspects of the healing interaction. This energetic ambiance is similar to feeling the love of a grandparent: feeling total acceptance from someone who just knows you are a remarkable human being. In the presence of a healer with such a compassionate presence, you feel safe, accepted, and engaged in a timeless state of mind, a state that promotes healing and regeneration as it dissolves long held defensiveness and fear-based habits of holding others at bay. This state of mind provides an opportunity for worries and unsettled emotions to dissipate. Feeling safe, accepted, and experiencing compassionate love supports the biological processes that nurture regeneration and growth.
How different this is from the more common experience with medical practitioners who sometimes have too little time to listen and to be with a patient. We might experience a medical provider as someone who may see us only as an illness (the cancer patient, the asthma patient) instead of recognizing us as a human being who happens to have an illness (a person with cancer or asthma). At times we can feel as though we are seen only as a series of numbers in a medical chart – yet we know we are more than that. People long to be seen. Often the medical provider interrupts with within the first 90 seconds with questions instead of listening. It becomes clear that the computerized medical record is more important than the human being seated there. Sometimes the patients can feel more fragmented and less safe, when they are not heard, not understood. In this rushed state, based upon “scientific data,” the health care provider may give a diagnosis without being aware of the emotional impact of the diagnosis.
As one 23 year old woman reported after being diagnosed with vulvodynia,”I cried immediately upon leaving the physician’s office. Even though he is an expert on the subject, I felt like I had no psychological support. I was on Gabapentin, and it made me very depressed. I thought to myself: Is my life, as I know it, over?” (Peper, Martinez Aranda, P., & Moss, 2015; Martinez Aranda, P. & Peper, E., 2015)
What was missing for this young woman was compassion and caring. Sometimes, the healthcare providers are unaware of the effect of their rushed behavior and lack of presence. They can issue a diagnosis based on the scientific data without recognizing the emotional impact on the person receiving it.
Sitting at the foot of the master healer is not wasted time when the apprentice learns how to genuinely attend to another with non-judgmental, compassionate presence. However, this requires substantial personal work. Possibly all allied healthcare providers should be required, or at least invited, to learn how to attain the state of mind that can enhance healing. Perhaps the practice of medicine could change if, as Bernard Lown wrote, the focus were once again on healing, “…which begins with listening to the patient.”
References
Denison, B. (2004). Touch the pain away: New research on therapeutic touch and persons with fibromyalgia syndrome. Holistic nursing practice, 18(3), 142-150.
Krieger, D. (1979). The therapeutic touch: How to use your hands to help or to heal. Vol. 15. Englewood Cliffs, NJ: Prentice-Hall.
Kunz, D. & Krieger, K. (2004). The spiritual dimension of therapeutic touch. Rochester, VT: Inner Traditions/Bear & Co.
Kunz, D., & Peper, E. (1995). Fields and their clinical implications. in Kunz, D.,(ed). Spiritual Aspects of the Healing Arts. Wheaton, ILL: Theosophical Pub House, 213-222.
Lown, B. (1999). The lost art of healing: Practicing compassion in medicine. New York, NY: Ballantine Books.
Martinez Aranda, P. & Peper, E. (2015). The healing of vulvodynia from the client’s perspective.
Peper, E. (2015). Towards the end of suffering: The contributions of integrating mind, body and spirit by Mr. Kawakami. In: Kawakami, M., Peper, E., & Kakigi, R. (2015). Cerebral investigation of a Yoga Master during Meditation-Findings from Collaborative Research. Fukuoka, Japan: Showado Publisher, 7-13.
Peper, E., Gibney, K. H. & Wilson, V. E. (2005). Enhancing Therapeutic Success–Some Observations from Mr. Kawakami: Yogi, Teacher, Mentor and Healer. Somatics. XIV (4), 18-21
Peper, E., Martinez Aranda, P., & Moss, E. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback, 43(2), 103-109.
Van Gelder, K & Chesley, F. (2015). A Most Unusual Life. Wheaton Ill: Theosophical Publishing House.
Notes:
- I thank Peter Parks for his superb editorial support and encouraging me to publish it.
- This blog was adapted the following two published articles, Peper, E. (2015). Compassionate Presence: Covert Training Invites Subtle Energies Insights. Subtle Energies Magazine, 26(2), 22-25; Peper, E. Sitting at the foot of the master-Covert training in compassionate presence. Somatics, 18(3), 46-47.
Less Medicine, More Health?
Posted: October 19, 2015 Filed under: Uncategorized | Tags: decision making, health, iatrogenic disease, medical testing, Medicine 1 CommentShould I get a body scan?
How aggressively should I lower my blood sugar level as I have type 2 diabetes?
I have no symptoms, should I get a routine mammogram?
I feel great, should I follow my doctor’s advice and have my annual physical?
These and hundreds of other questions often imply that the more medical care the better and healthier you will be. We assume that more care, more testing, the newer the drug, the more screening, etc. will prevent illness and promote health. In numerous cases this is not true! Although medical care can be superb for the treatment of acutely ill and injured, excessive use sometimes leads to harm.
In a superb book, Less Medicine, More Health, by Dr. H. Gilbert Welch, professor at Dartmouth Medical School and recognized expert on the effects of medical testing, the following seven basic assumptions underlying too much medical care are described in a readable and personable style.
- All risks can be lowered
- It’s always better to fix the problem
- Sooner is always better
- It never hurts to get more information
- Action is always better than inaction
- Newer is always better
- It’s all about avoiding death
Welch’s book explains the assumptions and the limitations of the assumption. Before assuming that the recommended medical procedures will improve your health—in some cases it will make you sicker—read his book, Less Medicine More Health.
Welch, H.G. (2015). Less Medicine, More Health. Boston: Beacon Press. ISBM 978-0-8070-7164-9
Resolving pelvic floor pain-A case report
Posted: September 25, 2015 Filed under: Breathing/respiration, Pain/discomfort, self-healing, stress management, Uncategorized | Tags: biofeedback, Breathing, electromyography, pain, posture, self-regulation, vulvodynia 10 CommentsAdapted from: Martinez Aranda, P. & Peper, E. (2015). The healing of vulvodynia from a client’s perspective. https://biofeedbackhealth.files.wordpress.com/2011/01/a-healing-of-vulvodynia-from-the-client-perspective-2015-06-15.pdf
It’s been a little over a year since I began practicing biofeedback and visualization strategies to overcome vulvodynia. Today, I feel whole, healed, and hopeful. I learned that through controlled and conscious breathing, I could unleash the potential to heal myself from chronic pain. Overcoming pain did not happen overnight; but rather, it was a process where I had to create and maintain healthy lifestyle habits and meditation. Not only am I thankful for having learned strategies to overcome chronic pain, but for acquiring skills that will improve my health for the rest of my life. –-24 year old woman who successfully resolved vulvodynia
Pelvic floor pain can be debilitating, and it is surprisingly common, affecting 10 to 25% of American women. Pelvic floor pain has numerous causes and names. It can be labeled as vulvar vestibulitis, an inflammation of vulvar tissue, interstitial cystitis (chronic pain or tenderness in the bladder), or even lingering or episodic hip, back, or abdominal pain. Chronic pain concentrated at the entrance to the vagina (vulva), is known as vulvodynia. It is commonly under-diagnosed, often inadequately treated, and can go on for months and years (Reed et al., 2007; Mayo Clinic, 2014). The discomfort can be so severe that sitting is uncomfortable and intercourse is impossible because of the extreme pain. The pain can be overwhelming and destructive of the patient’s life. As the participant reported,
I visited a vulvar specialist and he gave me drugs, which did not ease the discomfort. He mentioned surgical removal of the affected tissue as the most effective cure (vestibulectomy). I cried immediately upon leaving the physician’s office. Even though he is an expert on the subject, I felt like I had no psychological support. I was on Gabapentin to reduce pain, and it made me very depressed. I thought to myself: Is my life, as I know it, over?
Physically, I was in pain every single day. Sometimes it was a raging burning sensation, while other times it was more of an uncomfortable sensation. I could not wear my skinny jeans anymore or ride a bike. I became very depressed. I cried most days because I felt old and hopeless instead of feeling like a vibrant 23-year-old woman. The physical pain, combined with my negative feelings, affected my relationship with my boyfriend. We were unable to have sex at all, and because of my depressed status, we could not engage in any kind of fun. (For more details, read the published case report,Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report).
The four-session holistic biofeedback interventions to successfully resolved vulvodynia included teaching diaphragmatic breathing to transform shallow thoracic breathing into slower diaphragmatic breathing, transforming feelings of powerlessness and hopelessness to empowerment and transforming her beliefs that she could reduce her symptoms and optimize her health. The interventions also incorporated self-healing imagery and posture-changing exercises. The posture changes consisted of developing awareness of the onset of moving into a collapsed posture and use this awareness to shift to an erect/empowered postures (Carney, Cuddy, & Yap, 2010; Peper, 2014; Peper, Booiman, Lin, & Harvey, in press). Finally, this case report build upon the seminal of electromyographic feedback protocol developed by Dr. Howard Glazer (Glazer & Hacad, 2015) and the integrated relaxation protocol developed Dr. David Wise (Wise & Anderson, 2007).
Through initial biofeedback monitoring of the lower abdominal muscle activity, chest, and abdomen breathing patterns, the participant observed that when she felt discomfort or was fearful, her lower abdomen muscles tended to tighten. After learning how to sense this tightness, she was able to remind herself to breathe lower and slower, relax the abdominal wall during inhalation and sit or stand in an erect power posture.
The self-mastery approach for healing is based upon a functional as compared to a structural perspective. The structural perspective implies that the problem can only be fixed by changing the physical structure such as with surgery or medications. The functional perspective assumes that if you can learn to change your dysfunctional psychophysiological patterns the disorder may disappear.
The functional approach assumed that an irritation of the vestibular area might have caused the participant to tighten her lower abdomen and pelvic floor muscles reflexively in a covert defense reaction. In addition, ongoing worry and catastrophic thinking (“I must have surgery, it will never go away, I can never have sex again, my boyfriend will leave me”) also triggered the defense reaction—further tightening of her lower abdomen and pelvic area, shallow breathing, and concurrent increases in sympathetic nervous activation—which together activated the trigger points that lead to increased chronic pain (Banks et al, 1998).
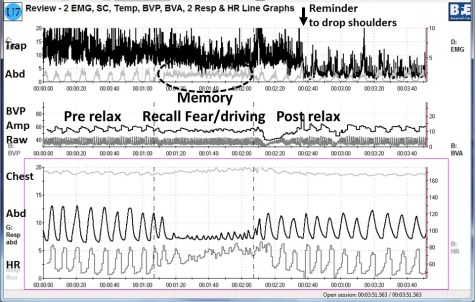
When the participant experienced a sensation or thought/worried about the pain, her body responded in a defense reaction by breathing in her chest and tightening the lower abdominal area as monitored with biofeedback. Anticipation of being monitored increased her shoulder tension, recalling the stressful memory increased lower abdominal muscle tension (pulling in the abdomen for protection), and the breathing became shallow and rapid as shown in Figure 1.
Figure 1. Physiological recording of pre-stressor relaxation, the recall of a fearful driving experience, and a post-stressor relaxation. The scalene to trapezius SEMG increased in anticipation while she recalled the experience, and then initially did not relax (from Peper, Martinez Aranda, & Moss, 2015).
This defense pattern became a conditioned response—initiating intercourse or being touched in the affected area caused the participant to tense and freeze up. She was unaware of these automatic protective patterns, which only worsened her chronic pain.
During the four sessions of training, the participant learned to reverse and interrupt the habitual defense reaction. For example, as she became aware of her breathing patterns she reported,
It was amazing to see on the computer screen the difference between my regular breathing pattern and my diaphragmatic breathing pattern. I could not believe I had been breathing that horribly my whole life, or at least, for who knows how long. My first instinct was to feel sorry for myself. Then, rather than practicing negative patterns and thoughts, I felt happy because I was learning how to breathe properly. My pain decreased from an 8 to alternating between a 0 and 3.
The mastery of slower and lower abdominal breathing within a holistic perspective resulted in the successful resolution of her vulvodynia. An essential component of the training included allowing the participant to feel safe, and creating hope by enabling her to experience a decrease in discomfort while doing a specific practice, and assisting her to master skills to promote self-healing. Instead of feeling powerless and believing that the only resolution was the removal of the affected area (vestibulectomy). The integrated biofeedback protocol offered skill mastery training, to promote self-healing through diaphragmatic breathing, somatic postural changes, reframing internal language, and healing imagery as part of a common sense holistic health approach.
For more details about the case report, download the published study, Peper, E., Martinez Aranda, P., & Moss, E. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback. 43(2), 103-109.
The participant also wrote up her subjective experience of the integrated biofeedback process in the paper, Martinez Aranda & Peper (2015). Healing of vulvodynia from the client perspective. In this paper she articulated her understanding and experiences in resolving vulvodynia which sheds light on the internal processes that are so often skipped over in published reports.
At the five year follow-up on May 29, 2019, she wrote:
“I am doing very well, and I am very healthy. The vulvodynia symptoms have never come back. It migrated to my stomach a couple of years after, and I still have a sensitive stomach. My stomach has gotten much, much better, though. I don’t really have random pain anymore, now I just have to be watchful and careful of my diet and my exercise, which are all great things!”
References
Banks, S. L., Jacobs, D. W., Gevirtz, R., & Hubbard, D. R. (1998). Effects of autogenic relaxation training on electromyographic activity in active myofascial trigger points. Journal of Musculoskeletal Pain, 6(4), 23-32. https://www.researchgate.net/profile/David_Hubbard/publication/232035243_Effects_of_Autogenic_Relaxation_Training_on_Electromyographic_Activity_in_Active_Myofascial_Trigger_Points/links/5434864a0cf2dc341daf4377.pdf
Carney, D. R., Cuddy, A. J., & Yap, A. J. (2010). Power posing brief nonverbal displays affect neuroendocrine levels and risk tolerance. Psychological Science, 21(10), 1363-1368. Available from: https://www0.gsb.columbia.edu/mygsb/faculty/research/pubfiles/4679/power.poses_.PS_.2010.pdf
Glazer, H. & Hacad, C.R. (2015). The Glazer Protocol: Evidence-Based Medicine Pelvic Floor Muscle (PFM) Surface Electromyography (SEMG). Biofeedback, 40(2), 75-79. http://www.aapb-biofeedback.com/doi/abs/10.5298/1081-5937-40.2.4
Martinez Aranda, P. & Peper, E. (2015). Healing of vulvodynia from the client perspective. Available from: https://biofeedbackhealth.files.wordpress.com/2011/01/a-healing-of-vulvodynia-from-the-client-perspective-2015-06-15.pdf
Mayo Clinic (2014). Diseases and conditions: Vulvodynia. Available at http://www.mayoclinic.org/diseases-conditions/vulvodynia/basics/definition/con-20020326
Peper, E. (2014). Increasing strength and mood by changing posture and sitting habits. Western Edition, pp.10, 12. Available from: http://thewesternedition.com/admin/files/magazines/WE-July-2014.pdf
Peper, E., Booiman, A., Lin, I, M.,& Harvey, R. (in press). Increase strength and mood with posture. Biofeedback.
Peper, E., Martinez Aranda, P., & Moss, E. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback. 43(2), 103-109. Available from: https://biofeedbackhealth.files.wordpress.com/2011/01/a-vulvodynia-treated-with-biofeedback-published.pdf
Reed, B. D., Haefner, H. K., Sen, A., & Gorenflo, D. W. (2008). Vulvodynia incidence and remission rates among adult women: a 2-year follow-up study. Obstetrics & Gynecology, 112(2, Part 1), 231-237. http://journals.lww.com/greenjournal/Abstract/2008/08000/Vulvodynia_Incidence_and_Remission_Rates_Among.6.aspx
Wise, D., & Anderson, R. U. (2006). A headache in the pelvis: A new understanding and treatment for prostatitis and chronic pelvic pain syndromes. Occidental, CA: National Center for Pelvic Pain Research.http://www.pelvicpainhelp.com/books/
Doctor Mike Evans: What’s the Best Diet? Healthy Eating 101
Posted: September 24, 2015 Filed under: Nutrition/diet, Uncategorized | Tags: diet, exercise, food, health 1 CommentA healthy diet is much more than just focusing on a single food. People focus so often on adding one type of food or eliminating another such as, “Don’t eat ice cream!”, “Eat chia seeds.” “No red meat.” In almost all cases, it is not just one thing, instead a healthy diet is embedded in awareness and healthy life style choices. Watch the superb common sense white board video presentation by Doctor Mike Evans, What’s the Best Diet? Healthy Eating 101. In this short presentation, he summarizes the best practices known. Implement his approach and your health will significantly improve.
Gut understanding-From salivating to pooping and all that is in between
Posted: August 16, 2015 Filed under: Uncategorized | Tags: allergy, antibiotics, bacteria, digestion, health, microbiome 4 CommentsEighty percent of all your cells in your body are bacteria and not human cells. Or is it that human beings are this mixture of beneficial bacteria and human cells? The majority of the bacteria live in our large intestines and contribute to our health and well-being. One of the hottest area in medicine and biology is the study of the human microbiome–understanding the role of the bacteria that co-habitate with us. The dynamic mixture of healthy and harmful bacteria can create illness or health and change our moods.
Ever wondered how food is digested, what foods do for you, what is a stomach ache, diarrhea or how defecation occurs? To understand our digestive tract from the mouth to the anus, from the first morsel of food entering our mouth to pooping is explained in superb readable book, Gut-The Inside Story of Our Body’s Most Underrated Oran, written by the German writer and scientist. Giulia Enders. It is a must read for anyone concerned about impact of cesarean birth, food allergies, eczema, ulcers, effect of antibiotics, constipation, farting, bloating, etc.For a fun summary, see Steve Palkin’s interview with Giulia Enders on YouTube.