Ensorcelled: Breaking the Digital Enchantment
Posted: October 7, 2025 Filed under: ADHD, attention, behavior, cellphone, computer, digital devices, education, emotions, healing, health, laptops, techstress, Uncategorized | Tags: anxiety, depression, health, human connection, life, loneliness, media addictdion, mental-health, storytelling 1 Comment
My mom called, “Stop playing on your computer and come for dinner!” I heard her, but I was way too into my game. It felt like I was actually inside it. I think I yelled “Yeah!” back, but I didn’t move.
A few seconds later, I was totally sucked into this awesome world where I was conquering other galaxies. My avatar was super powerful, and I was winning this crazy battle.
Then, all of a sudden, my mom came into my room and just turned off the computer. I was so mad. I was about to win! The real world around me felt boring and empty. I didn’t even feel hungry anymore. I didn’t say anything, I just wanted to go back to my game.
For some, the virtual world feels more real and exciting than the actual one. It can seem more vivid precisely because they have not yet tasted the full, multi-dimensional richness of real human connection, those moments when you feel seen, touched, and understood.
This theme comes vividly alive in my son Eliot Peper’s new novella, Ensorcelled. I am so proud of him. He has crafted a story in which a young boy, captured by the spell of the immersive digital world, discovers that real-life experiences carry far deeper meaning. I won’t give away the plot, but the story creates the experience, it doesn’t just tell it. It reminds us that meaning and belonging arise through genuine connection, not through screens. As Eliot writes, “Sometimes a story is the only thing that can save your life.” It’s a story everyone should read.
The effects of our immersive digital world
Our new world of digital media can take over the reality of actual experiences. It is no wonder that more young people feel stressed and have social anxiety when they have to make an actual telephone call instead of texting (Jin, 2025). They also experience a significant increase in anxiety and depression and feel more awkward initiating in-person social communication with others. The increase in mental health problems and social isolation affects predominantly those who are cellphone and social media natives; namely, those who started to use social media after Facebook was released in 2004 and the iPhone in 2007 (Braghieri et al., 2022).
Students who are most often on their phone whether streaming videos, scrolling, texting, watching YouTube, Instagram or TikTok, and more importantly responding to notifications from phones when they are socializing, report higher levels of loneliness, depression and anxiety as shown inf Figure 1 (Peper & Harvey 2018). They also report less positive feelings and energy when they communicate with each other online as compared to in person (Peper & Harvey, 2024).

Figure 1. The those with the highest phone use were the most lonely, depressed and anxious (Peper and Harvey, 2018).
Even students’ sexual activity has decreased in U.S. high-school from 2013 to 2023 and young adults (ages 18-44) from 2000-2018 (CDC, 2023; Ueda et al., 2020). Much of this may be due to the reality that adolescents have reduced face-to-face socializing (dating, parties, going out) while increasing their time on digital media (Twenge et al., 2019).
What to do
As a parent it often feels like a losing battle to pull your child, or even yourself, away from the intoxicating digital media, since the digital world is supercharged with AI-generated media. It is all aimed at capturing eyeballs (your attention and time), resulting reducing genuine human social connection. (Peper at al., 2020; Haidt, 2024). To change behavior is challenging and yet rewarding. If possible, implement the following (Peper at al., 2020; Twenge, 2025; Haidt, 2024):
- Create tech-free zones. Keep phones and devices out of bedrooms, the dinner table, and family gatherings. Make these spaces sacred for real connection.
- Avoid screens before bedtime. Turn off screens at least an hour before bed. Replace scrolling with quiet reflection, reading, or gentle stretching. Read or tell actual stories before bedtime.
- Explore why we turn to digital media. Before you open an app, ask: Why am I doing this? Am I bored, anxious, or avoiding something? Awareness shifts behavior.
- Provide unstructured time. Let yourself and your children be bored sometimes. Boredom sparks creativity, imagination, and self-discovery.
- Create shared experiences. Plan family activities that don’t involve screens—cooking, hiking, playing music, or simply talking. Real connection satisfies what digital media only mimics.
- Implement social support. Coordinate with other parents, friends, or colleagues to agree on digital limits. Shared norms make it easier to follow through.
- Model what you want your children to do. Children imitate what they see. When adults practice digital restraint, kids learn that real life matters more than screen life.
We have a choice.
We can set limits now and experience real emotional connection and growth or become captured, enslaved, and manipulated by the corporate creators, producers and sellers of media.
Read Ensorcelled. which uses storytelling, the traditional way to communicate concepts and knowledge. Read it, share it. It may change your child’s life and your own.

Available from
Signed copy by author: https://store.eliotpeper.com/products/ensorcelled
Paperback: https://www.amazon.com/Ensorcelled-Eliot-Peper/dp/1735016535/
Kindle: https://www.amazon.com/Ensorcelled-Eliot-Peper-ebook/dp/B0FLGQC3BS/
References
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022) http://dx.doi.org/10.2139/ssrn.3919760
CDC. (2023). Centers for Disease Control and Prevention. (2023). Youth Risk Behavior Survey: Data summary & trends report 2011–2021. U.S. Department of Health and Human Services. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
Haidt, J. (2024). The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness. New York: Penguin Press. https://www.amazon.com/Anxious-Generation-Rewiring-Childhood-Epidemic/dp/0593655036
Jin, B. (2025). Avoidance and Anxiety About Phone Calls in Young Adults: The Role of Social Anxiety and Texting Controllability. Communication Reports, 1–14. https://doi.org/10.1080/08934215.2025.2542562
Peper, E. & Harvey, R. (2018). Digital addiction: increased loneliness, depression, and anxiety. NeuroRegulation. 5(1),3–8. doi:10.15540/nr.5.1.3 5(1),3–8. http://www.neuroregulation.org/article/view/18189/11842
Peper, E. & Harvey, R. (2024). Smart phones affects social communication, vision, breathing, and mental and physical health: What to do! Townsend Letter-Innovative Health Perspectives, September 15, 2024. https://townsendletter.com/smartphone-affects-social-communication-vision-breathing-and-mental-and-physical-health-what-to-do/
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
Ueda, P., Mercer, C. H., Ghaznavi, C., & Herbenick, D. (2020). Trends in frequency of sexual activity and number of sexual partners among adults aged 18 to 44 years in the US, 2000–2018. JAMA Network Open, 3(6), e203833. https://doi.org/10.1001/jamanetworkopen.2020.3833
Twenge, J.M. (2025). 10 Rules for Raising Kids in a High-Tech World: How Parents Can Stop Smartphones, Social Media, and Gaming from Taking Over Their Children’s Lives. New York: Atria Books. https://www.amazon.com/Rules-Raising-Kids-High-Tech-World/dp/1668099993
Twenge, J. M., Spitzberg, B. H., & Campbell, W. K. (2019). Less in-person social interaction with peers among U.S. adolescents in the 21st century and links to loneliness. Journal of Social and Personal Relationships, 36(6), 1892-1913. https://doi.org/10.1177/0265407519836170
Grandmother Therapy: A Common-Sense Approach to Health and Wellness
Posted: July 24, 2024 Filed under: ADHD, attention, behavior, education, Evolutionary perspective, Exercise/movement, Nutrition/diet, Pain/discomfort, relaxation, self-healing | Tags: anxiety, depression, epilepsy, exhaustion, grandmother therapy, health, insomnia, life style change, mental-health, therapy 1 CommentErik Peper, PhD and Angelika Sadar, MA

In today’s fast-paced world, college students and young adults often struggle with various health issues. From anxiety and depression to ADHD and epilepsy, these challenges can significantly impact their daily lives. But what if the solution to many of these problems lies in something as simple as “Grandmother Therapy”?
What is Grandmother Therapy? Grandmother Therapy is all about going back to basics and establishing healthy lifestyle habits. It’s the common-sense approach that our grandmothers might have suggested: regular sleep patterns, balanced nutrition, increased social connections, and regular physical activity.
The Problem: Many college students:
- Skip breakfast before their first class
- Rely on fast food and sugary stimulants
- Have irregular sleep schedules
- Spend excessive time on gaming and social media
The Medical Approach: Often, the quick solution is medication:
- Depression? Take antidepressants.
- Insomnia? Use sleeping pills.
- Anxiety? Try anti-anxiety medication.
- ADHD? Prescribe Ritalin or similar drugs.
While these treatments may help manage symptoms, they often overlook the underlying lifestyle factors contributing to these issues.
The Grandmother Therapy Approach:
- Establish regular sleep patterns
- Adopt healthy eating habits
- Increase social connections
- Incorporate regular physical activity
- Reduce gaming and social media use
Case Study #1: The Power of Sleep
This illustrates the simple intervention of having a bedtime routine. A college student in a holistic health class complained that she was tired most of the time and had difficulty focusing her attention and continuously drifted off in class.
Here is her reported sleep schedule:
- last night I went to bed at 3am and woke up 7;
- the day before, I went to bed at 1pm and woke up at 6,
- two nights before, I went to bed at 4pm and woke up at 10 am.
Holistic treatment approach:
Set a sleep schedule: she was provided with information about the importance of having a regular pattern of sleep and waking. Namely, go to bed at the same time and get up 8 hours later. She agreed to do an experiment for a week to go to bed at 12 and wake up at 8m. To her surprise, she felt so much more energized and could pay attention in class during the week of the experiment.
Case Study #2: Beyond Seizures: A Holistic Approach to Treating Psychogenic Nonepileptic Seizures
This case study highlights the importance of a comprehensive, lifestyle-based approach to treating psychogenic nonepileptic seizures (PNES). It follows a 24-year-old male student initially diagnosed with intractable epilepsy, experiencing over 10 seizures per week that didn’t respond to medication.
Key points:
1. Initial misdiagnosis: Despite normal MRI and EEG results, the client was initially treated for epilepsy.
2. Limited assessment: Traditional medical evaluations focused solely on seizure descriptions and diagnostics, overlooking crucial lifestyle factors.
3. Comprehensive evaluation: A psychophysiological assessment revealed high sympathetic arousal, including rapid breathing, sweaty palms, and muscle tension.
4. Lifestyle factors: The client’s diet consisted of high-glycemic fast foods, excessive caffeine, alcohol, and daily marijuana use. He also had significant student debt and a history of abdominal surgery.
Holistic treatment approach:
– Dietary changes: Switching to unprocessed, low-glycemic foods and increasing vegetable and fruit intake
– Breathing techniques: Learning and practicing slow diaphragmatic breathing
– Stress management: Addressing underlying stressors and practicing relaxation techniques
– Supplements: Adding omega-3 and multivitamins to support brain health
Remarkable results: Within four months, the patient became seizure-free, reduced marijuana use significantly, and decreased medication dosage.
Summary
These cases underscore the potential of integrating lifestyle modifications and stress management techniques in treating attention, anxiety and even psychogenic nonepileptic seizures; offering hope for patients who don’t respond to traditional treatments alone. Before turning to medication or complex treatments, consider the power of Grandmother Therapy. By addressing fundamental lifestyle factors, we can often improve our health and well-being significantly. Remember, sometimes the most effective solutions are the simplest ones.
The Challenges of Simplicity: While Grandmother Therapy may seem straightforward, its simplicity can make it challenging to implement. It requires commitment and a willingness to change long-standing habits.
Implement many Life Style Changes at once: Recommending one change at the time is logical; however, participants will more likely experience rapid benefits and are more motivated to continue when they change multiple lifestyle factors at once.
Call to Action: Are you struggling with health issues? Try implementing some aspects of Grandmother Therapy in your life. Implement changes and see how they impact your overall well-being.
Please let us know your experience with implementing Grandmother Therapy.
See the following blogs for more background information
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods
Posted: June 30, 2024 Filed under: ADHD, attention, behavior, CBT, digital devices, education, emotions, Evolutionary perspective, health, mindfulness, neurofeedback, Nutrition/diet, Uncategorized | Tags: ADHD, anxiety, depression, diet, glyphosate, herbicide, herbicites, mental-health, neurofeedback, pesticides, supplements', ultraprocessed foods, vitamins 4 CommentsAdapted from: Peper, E. & Shuford, J. (2024). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods. NeuroRegulation, 11(2), 219–228. https://doi.org/10.15540/nr.11.2.219
Look at your hand and remember that every cell in your body including your brain is constructed out the foods you ingested. If you ingested inferior foods (raw materials to be built your physical structure), then the structure can only be inferior. If you use superior foods, you have the opportunity to create a superior structure which provides the opportunity for superior functioning. -Erik Peper
Summary
Mental health symptoms of attention deficit hyperactivity disorder (ADHD), Autism, anxiety and depression have increased over the last 15 years. An additional risk factor that may affect mental and physical health is the foods we eat. Even though, our food may look and even taste the same as compared to 50 years ago, it contains herbicide and pesticide residues and often consist of ultra-processed foods. These foods (low in fiber, and high in sugar, animal fats and additives) are a significant part of the American diet and correlate with higher levels of inattention and hyperactivity in children with ADHD. Due to affluent malnutrition, many children are deficient in essential vitamins and minerals. We recommend that before beginning neurofeedback and behavioral treatments, diet and lifestyle are assessed (we call this Grandmother therapy assessment). If the diet appears low in organic foods and vegetable, high in ultra-processed foods and drinks, then nutritional deficiencies should be assessed. Then the next intervention step is to reduce the nutritional deficiencies and implement diet changes from ultra-processed foods to organic whole foods. Meta-analysis demonstrates that providing supplements such as Vitamin D, etc. and reducing simple carbohydrates and sugars and eating more vegetables, fruits and healthy fats during regular meals can ameliorate the symptoms and promote health.
The previous article and blog, Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms, pointed out how the changes in bonding, screen time and circadian rhythms affected physical and mental health (Peper, 2023a; Peper, 2023b). However, there are many additional factors including genetics that may contribute to the increase is ADHD, autism, anxiety, depression, allergies and autoimmune illnesses (Swatzyna et al., 2018). Genetics contribute to the risk of attention deficit hyperactivity disorder (ADHD); since, family, twin, and adoption studies have reported that ADHD runs in families (Durukan et al., 2018; Faraone & Larsson, 2019). Genetics is in most cases a risk factor that may or may not be expressed. The concept underlying this blog is that genetics loads the gun and environment and behavior pulls the trigger as shown in Figure 1.

Figure 1. Interaction between Genetics and Environment
The pandemic only escalated trends that already was occurring. For example, Bommersbach et al (2023) analyzed the national trends in mental health-related emergency department visits among USA youth, 2011-2021. They observed that in the USA, Over the last 10 years, the proportion of pediatric ED visits for mental health reasons has approximately doubled, including a 5-fold increase in suicide-related visits. The mental health-related emergency department visits increased an average of 8% per year while suicide related visits increased 23.1% per year. Similar trends have reported by Braghieri et al (2022) from the National Survey on Drug Use and Health as shown in Figure 2.

Figure 2. Mental health trends in the United States by age group in 2008–2019. The data come from the National Survey on Drug Use and Health. Reproduced with permission from Braghieri, Luca and Levy, Ro’ee and Makarin, Alexey, Social Media and Mental Health (July 28, 2022) https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
The trends reported from this data shows an increase in mental health illnesses for young people ages 18-23 and 24-29 and no changes for the older groups which could be correlated with the release of the first iPhone 2G on June 29, 2007. Thus, the Covid 19 pandemic and social isolation were not THE CAUSE but an escalation of an ongoing trend. For the younger population, the cellphone has become the vehicle for personal communication and social connections, many young people communicate more with texting than in-person and spent hours on screens which impact sleep (Peper, 2023a). At the same time, there are many other concurrent factors that may contributed to increase of ADHD, autism, anxiety, depression, allergies and autoimmune illnesses.
Without ever signing an informed consent form, we all have participated in lifestyle and environmental changes that differ from that evolved through the process of evolutionary natural selection and promoted survival of the human species. Many of those changes in lifestyle are driven by demand for short-term corporate profits over long-term health of the population. As exemplified by the significant increase in vaping in young people as a covert strategy to increase smoking (CDC, 2023) or the marketing of ultra-processed foods (van Tulleken, 2023).
This post focusses how pesticides and herbicides (exposure to neurotoxins) and changes in our food negatively affects our health and well-being and is may be another contributor to the increase risk for developing ADHD, autism, anxiety and depression. Although our food may look and even taste the same compared to 50 years ago, it is now different–more herbicide and pesticide residues and is often ultra-processed. lt contains lower levels of nutrients and vitamins such as Vitamin C, Vitamin B2, Protein, Iron, Calcium and Phosphorus than 50 years ago (Davis et al, 2004; Fernandez-Cornejo et al., 2014). Non-organic foods as compared to organic foods may reduce longevity, fertility and survival after fasting (Chhabra et al., 2013).
Being poisoned by pesticide and herbicide residues in food
Almost all foods, except those labeled organic, are contaminated with pesticides and herbicides. The United States Department of Agriculture reported that “Pesticide use more than tripled between 1960 and 1981. Herbicide use increased more than tenfold (from 35 to 478 million pounds) as more U.S. farmers began to treat their fields with these chemicals” (Fernandez-Cornejo, et al., 2013, p 11). The increase in herbicides and pesticides is correlated with a significant deterioration of health in the United States (Swanson, et al., 2014 as illustrated in the following Figure 3.


Figure 3. Correlation between Disease Prevalence and Glyphosate Applications (reproduced with permission from Swanson et al., 2014.
Although correlation is not causation and similar relationships could be plotted by correlating consumption of ultra-refined foods, antibiotic use, decrease in physical activity, increase in computer, cellphone and social media use, etc.; nevertheless, it may suggest a causal relationship. Most pesticides and herbicides are neurotoxins and can accumulate in the person over time this could affect physical and mental health (Bjørling-Poulsen et al., 2008; Arab & Mostaflou, 2022). Even though the United States Environmental Protection Agency (EPA) has determined that the residual concentrations in foods are safe, their long-term safety has not been well established (Leoci & Ruberti, 2021). Other countries, especially those in which agribusiness has less power to affect legislation thorough lobbying, and utilize the research findings from studies not funded by agribusiness, have come to different conclusions…
For example, the USA allows much higher residues of pesticides such as, Round-Up, with a toxic ingredient glyphosate (0.7 parts per million) in foods than European countries (0.01 parts per million) (Wahab et al., 2022; EPA, 2023; European Commission, 2023) as is graphically illustrated in figure 4.

Figure 4: Percent of Crops Sprayed with Glyphosate and Allowable Glyphosate Levels in the USA versus the EU
The USA allows this higher exposure than the European Union even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbo et al., 2022). The negative effects most likely would be more harmful in a rapidly growing infant than for an adult. Most likely, some individuals are more vulnerable than others and are the “canary in mine.” They are the early indicators for possible low-level long-term harm. Research has shown that fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021). Also, organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010). We hypothesize this exposure is one of the co-factors that have contributed to the decrease in mental health of adults 18 to 29 years.
At the same time as herbicides and pesticides acreage usage has increased, ultra-processed food have become a major part of the American diet (van Tulleken, 2023). Eating a diet high in ultra-processed foods, low in fiber, high sugar, animal fats and additives has been associated with higher levels of inattention and hyperactivity in children with ADHD; namely, high consumption of sugar, candy, cola beverages, and non-cola soft drinks and low consumption of fatty fish were also associated with a higher prevalence of ADHD diagnosis (Ríos-Hernández et al., 2017).
In international studies, less nutritional eating behaviors were observed in ADHD risk group as compared to the normal group (Ryu et al., 2022). Artificial food colors and additives are also a public health issue and appear to increase the risk of hyperactive behavior (Arnold et al., 2012). In a randomized double-blinded, placebo controlled trial 3 and 8/9 year old children had an increase in hyperactive behavior for those whose diet included extra additives (McCann et al., 2007). The risk may occur during fetal development since poor prenatal maternal is a critical factor in the infants neurodevelopment and is associated with an increased probability of developing ADHD and autism (Zhong et al., 2020; Mengying et al., 2016).
Poor nutrition even affects your unborn grandchild
Poor nutrition not only affects the mother and the developing fetus through epigenetic changes, it also impacts the developing eggs in the ovary of the fetus that can become the future granddaughter (Wilson, 2015). At birth, the baby has all of her eggs. Thus, there is a scientific basis for the old wives tale that curses may skip a generation. Providing maternal support is even more important since it affects the new born and the future grandchild. The risk may even begin a generation earlier since the grandmother’s poor nutrition as well as stress causes epigenetic changes in the fetus eggs. Thus 50% of the chromosomes of the grandchild were impacted epigenetically by the mother’s and grandmother’s dietary and health status .
Highly processed foods
Highly refined foods have been processed to remove many of their nutrients. These foods includes white bread, white rice, pasta, and sugary drinks and almost all the fast foods and snacks. These foods are low in fiber, vitamins, and minerals, and they are high in sugars, unhealthy fats, and calories. In addition, additives may have been added to maximize taste and mouth feel and implicitly encourage addiction to these foods. A diet high in refined sugars and carbohydrates increases the risk of diabetes and can worsen the symptoms of ADHD, autism, depression, anxiety and increase metabolic disease and diabetes (Woo et al., 2014; Lustig, 2021; van Tulleken, 2023). Del-Ponte et al. (2019) noted that a diet high in refined sugar and saturated fat increased the risk of symptoms of ADHD, whereas a healthy diet, characterized by high consumption of fruits and vegetables, would protect against the symptoms.
Most likely, a diet of highly refined foods may cause blood sugar to spike and crash, which can lead to mood swings, irritability, anxiety, depression and cognitive decline and often labeled as “hangryness” (the combination of anger and hunger) (Gomes et al., 2023; Barr et al., 2019). At the same time a Mediterranean diet improves depression significantly more than the befriending control group (Bayles et al., 2022). In addition, refined foods are low in essential vitamins and minerals as well as fiber. Not enough fiber can slow down digestion, affect the human biome, and makes it harder for the body to absorb nutrients. This can lead to nutrient deficiencies, which can contribute to the symptoms of ADHD, autism, depression, and anxiety. Foods do impact our mental and physical health as illustrated by foods that tend to reduce depression (LaChance & Ramsey, 2018; MacInerney et al., 2017). By providing appropriate micronutrients such as minerals (Iron, Magnesium Zinc), vitamins (B6, B12, B9 and D), Omega 3s (Phosphatidylserine) and changing our diet, ADHD symptoms can be ameliorated.
Many children with ADHD, anxiety, depression are low on essential vitamins and minerals. For example, low levels of Omega-3 fatty acids and vitamin D may be caused by eating ultra-refined foods, fast foods, and drinking soft drink. At the same time, the children are sitting more in indoors in front of the screen and thereby have lower sun exposure that is necessary for the vitamin D production.
“Because of lifestyle changes and sunscreen use, about 42% of Americans are deficient in vitamin D. Among children between 1 to 11 years old, an estimated 15% have vitamin D deficiency. And researchers have found that 17% of adolescents and 32% of young adults were deficient in vitamin D.” (Porto and Abu-Alreesh, 2022).
Reduced sun exposure is even more relevant for people of color (and older people); since, their darker skin (increased melanin) protects them from ultraviolet light damage but at the same time reduces the skins production of vitamin D. Northern Europeans were aware of the link between sun exposure and vitamin D production. To prevent rickets (a disease caused by vitamin D deficiency) and reduce upper respiratory tract infections the children were given a tablespoon of cod liver oil to swallow (Linday, 2010). Cod liver oil, although not always liked by children, is more nutritious than just taking a Vitamin D supplements. It is a whole food and a rich source of vitamin A and D as well as containing a variety of Omega 3 fatty acids (eicosapentaenoic acid (EPA) (USDA, 2019).
Research studies suggest that ADHD can be ameliorated with nutrients, and herbs supplements (Henry & CNS, 2023). Table 1 summarizes some of the nutritional deficits observed and the reduction of ADHD symptoms when nutritional supplements were given (adapted from Henry, 2023; Henry & CNS, 2023).
| Nutritional deficits observed in people with ADHD | Decrease in ADHD symptoms with nutritional supplements |
| Vitamin D: In meta-analysis with a total number of 11,324 children, all eight trials reported significantly lower serum concentrations of 25(OH)D in patients diagnosed with ADHD compared to healthy controls. (Kotsi et al, 2019) | After 8 weeks children receiving vitamin D (50,000 IU/week) plus magnesium (6 mg/kg/day) showed a significant reduction in emotional problems as observed in a randomized, double blind, placebo-controlled clinical trial (Hemamy et al., 2021). |
| Iron: In meta-analysis lower serum ferritin was associated with ADHD in children (Wang et al., 2017) and the mean serum ferritin levels are lower in the children with ADHD than in the controls (Konofal et al., 2004). | After 12 weeks of supplementation with Iron (ferrous sulfate) in double-blind, randomized placebo-controlled clinical trial, clinical trials symptoms of in children with ADHD as compared to controls were reduced (Tohidi et al., 2021; Pongpitakdamrong et all, 2022). |
| Omega 3’s: Children with ADHD are more likely to be deficient in omega 3’s than children without ADHD (Chang et al., 2017). | Adding Omega-3 supplements to their diet resulted in an improvement in hyperactivity, impulsivity, learning, reading and short term memory as compared to controls in 16 randomized controlled trials including 1514 children and young adults with ADHD (Derbyshire, 2017) |
| Magnesium: In meta-analysis, subjects with ADHD had lower serum magnesium levels compared with to their healthy controls (Effatpahah et al., 2019) | 8 weeks of supplementation with Vitamin D and magnesium caused a significant decrease in children with conduct problems, social problems, and anxiety/shy scores (Hemamy et al., 2020). |
| Vitamin B2, B6, B9 and B12deficiency has been found in many patients with Attention Deficit and Hyperactivity Disorder (Landaas et al, 2016; Unal et al., 2019). | Vitamin therapy appears to reduce symptoms of ADHD and ASD (Poudineh et al., 2023; Unal et al., 2019). An 8 weeks supplementing with Vitamin B6 and magnesium decreased hyperactivity and hyperemotivity/aggressiveness. When supplementation was stopped, clinical symptoms of the disease reappeared in few weeks (Mousain-Bosc et al., 2006). |
Table 1. Examples of vitamin and mineral deficiencies associated with symptoms of ADHD and supplementation to reduction of ADHD symptoms.
Supplementation of vitamins and minerals in many cases consisted of more than one single vitamin or mineral. For an in-depth analysis and presentation, see the superb webinar by Henry & CNS (2023): https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback? (Henry & CNS, 2023).
Whole foods are more than the sum of individual parts (the identified individual constituents/nutrients). The process of digestion is much more complicated than ingesting simple foods with added vitamins or minerals. Digestion is the interaction of many food components (many of which we have not identified) which interact and affect the human biome. A simple added nutrient can help; however, eating whole organic foods it most likely be healthier. For example, whole-wheat flour is much more nutritious. Whole wheat is rich in vitamins B-1, B-3, B-5, riboflavin, folate well as fiber while refined white flour has been bleached and stripped of fiber and nutrients to which some added vitamins and iron are added.
Recommendation
When working with clients, follow Talib’s principles as outlined in Part 1 by Peper (2023) which suggests that to improve health first remove the unnatural which in this case are the ultra-processed foods, simple carbohydrates, exposure to pesticides and herbicides (Taleb, 2014). The approach is beneficial for prevention and treatment. This recommendation to optimize health is both very simple and very challenging. The simple recommendation is to eat only organic foods and as much variety as possible as recommended by Professor Michael Pollan in his books, Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules (Pollan, 2006; Pollan, 2011).
Do not eat foods that contain herbicides and pesticide residues or are ultra-processed. Although organic foods especially vegetable and fruits are often much more expensive, you have choice: You can pay more now to optimize health or pay later to treat disease. Be safe and not sorry. This recommendation is similar to the quote, “Let food be thy medicine and medicine be thy food,” that has been attributed falsely since the 1970s to Hippocrates, the Greek founder of western medicine (5th Century, BC) (Cardenas, 2013).
There are many factors that interfere with implementing these suggestions; since, numerous people live in food deserts (no easy access to healthy unprocessed foods ) or food swamps (a plethora of fast food outlets) and 54 million Americans are food insecure (Ney, 2022). In addition, we and our parents have been programmed by the food industry advertising to eat the ultra- processed foods and may no longer know how to prepare healthy foods such as exemplified by a Mediterranean diet. Recent research by Bayles et al (2022) has shown that eating a Mediterranean diet improves depression significantly more than the befriending control group. In addition, highly processed foods and snacks are omnipresent, often addictive and more economical.
Remember that clients are individuals and almost all research findings are based upon group averages. Even when the data implies that a certain intervention is highly successful, there are always some participants for whom it is very beneficial and some for whom it is ineffective or even harmful. Thus, interventions need to be individualized for which there is usually only very limited data. In most cases, the original studies did not identify the characteristics of those who were highly successful or those who were unsuccessful. In addition, when working with specific individuals with ADHD, anxiety, depression, etc. there are multiple possible causes.
Before beginning specific clinical treatment such as neurofeedback and/or medication, we recommend the following:
- “Grandmother assessment” that includes and assessment of screen time, physical activity, outdoor sun exposure, sleep rhythm as outlined in Part 1 by Peper (2023). Then follow-up with a dietary assessment that investigates the prevalence of organic/non organic foods, ingestion of fast foods, ultra-processed foods, soft drinks, high simple carbohydrate and sugar, salty/sugary/fatty snacks, fruits, vegetables, and eating patterns (eating with family or by themselves in front of screens). Be sure to include an assessment of emotional reactivity and frequency of irritability and “hangryness”.
- If the assessment suggest low level of organic whole foods and predominance of ultra- refined foods, it may be possible that the person is deficient in vitamins and minerals. Recommend that the child is tested for the vitamin deficiencies. If vitamin deficiencies identified, recommend to supplement the diet with the necessary vitamins and mineral and encourage eating foods that naturally include these substances (Henry & CNS, 2023). If there is a high level of emotional reactivity and “hangryness,” a possible contributing factor could be hypoglycemic rebound from a high simple carbohydrate (sugar) intake or not eating breakfast combined with hyperventilation (Engel et al., 1947; Barr et al., 2019). Recommend eliminating simple carbohydrate breakfast and fast food snacks and substitute organic foods that include complex carbohydrates, protein, fats, vegetables and fruit. Be sure to eat breakfast.
- Implement “Grandmother Therapy”. Encourage the family and child to change their diet to eating a whide variety of organic foods (vegetables, fruits, some fish, meat and possibly dairy) and eliminate simple carbohydrates and sugars. This diet will tend to reduce nutritional deficits and may eliminate the need for supplements.
- Concurrent with the stabilization of the physiology begin psychophysiological treatment strategies such as neurofeedback biofeedback and cognitive behavior therapy.
Relevant blogs
Author Disclosure
Authors have no grants, financial interests, or conflicts to disclose.
References
Arnold, L, Lofthouse, N., & Hurt, E. (2012). Artificial food colors and attention-deficit/hyperactivity symptoms: conclusions to dye for. Neurotherapeutics, 9(3), 599-609. https://doi.org/10.1007/s13311-012-0133-x
Arab, A. & Mostafalou, S. (2022). Neurotoxicity of pesticides in the context of CNS chronic diseases. International Journal of Environmental Health Research, 32(12), 2718-2755. https://doi.org/10.1080/09603123.2021.1987396
Barr, E.A., Peper, E., & Swatzyna, R.J. (2019). Slouched Posture, Sleep Deprivation, and Mood Disorders: Interconnection and Modulation by Theta Brain Waves. NeuroRegulation, 6(4), 181–189. https://doi.org/10.15540/nr.6.4.181
Bayes. J., Schloss, J., Sibbritt, D. (2022). The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND: A Mediterranean Diet in MEN with Depression” study): a randomized controlled trial. Am J Clin Nutr. 116(2), 572-580. https://doi.org/10.1093/ajcn/nqac106
Bjørling-Poulsen, M., Andersen, H.R. & Grandjean, P. Potential developmental neurotoxicity of pesticides used in Europe. Environ Health 7, 50 (2008). https://doi.org/10.1186/1476-069X-7-50
Bommersbach, T.J., McKean, A.J., Olfson, M., Rhee, T.G. (2023). National Trends in Mental Health–Related Emergency Department Visits Among Youth, 2011-2020. JAMA, 329(17):1469–1477. https://doi.org/10.1001/jama.2023.4809
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Cardenas, D. (2013). Let not thy food be confused with thy medicine: The Hippocratic misquotation. e-Spen Journal, 8(6), 3260-3262. https://doi.org/10.1016/j.clnme.2013.10.002
CDC, (2023). Quick Facts on the Risks of E-cigarettes for Kids, Teens, and Young Adults. CDC. Centers for Disease Control and Prevention. Accessed September 23, 2023. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html
Chang, J.C., Su, K.P., Mondelli, V. et al. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: a Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacol. 43, 534–545. https://doi.org/10.1038/npp.2017.160
Chhabra, R., Kolli, S., & Bauer, J.H. (2013). Organically Grown Food Provides Health Benefits to Drosophila melanogaster. PLoS ONE, 8(1): e52988. https://doi.org/10.1371/journal.pone.0052988
Davis, D. R., Epp, M. D., & Riordan, H. D. (2004). Changes in USDA food composition data for 43 garden crops, 1950 to 1999. Journal of the American College of Nutrition, 23(6), 669-682. https://doi.org/10.1080/07315724.2004.10719409
Derbyshire, E. (2017). Do Omega-3/6 Fatty Acids Have a Therapeutic Role in Children and Young People with ADHD? J Lipids. 6285218. https://doi.org/10.1155/2017/6285218
Del-Ponte, B., Quinte, G.C., Cruz, S., Grellert, M., & Santos, I. S. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): A systematic review and meta-analysis. Journal of Affective Disorders, 252, 160-173. https://doi.org/10.1016/j.jad.2019.04.061
Durukan, İ., Kara, K., Almbaideen, M., Karaman, D., & Gül, H. (2018). Alexithymia, depression and anxiety in parents of children with neurodevelopmental disorder: Comparative study of autistic disorder, pervasive developmental disorder not otherwise specified and attention deficit-hyperactivity disorder. Pediatrics International, 60(3), 247–253. https://doi.org/10.1111/ped.13510
Effatpanah, M., Rezaei, M., Effatpanah, H., Effatpanah, Z., Varkaneh, H.K., Mousavi. S.M., Fatahi, S., Rinaldi, G., & Hashemi, R. (2019). Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Res, 274, 228-234. https://doi.org/10.1016/j.psychres.2019.02.043
Engel, G.L., Ferris, E.B., & Logan, M. (1947). Hyperventilation; analysis of clinical symptomatology. Ann Intern Med, 27(5), 683-704. https://doi.org/10.7326/0003-4819-27-5-683
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians
Faraone, S.V. & Larsson, H. (2019). Genetics of attention deficit hyperactivity disorder. Mol Psychiatry, 24(4), 562-575. https://doi.org/10.1038/s41380-018-0070-0
Fernandez-Cornejo, J. Nehring, R, Osteen, C., Wechsler, S., Martin, A., & Vialou, A. (2014). Pesticide use in the U.S. Agriculture: 21 Selected Crops, 1960-2008. Economic Information Bulletin Number 123, United State Department of Agriculture. https://www.ers.usda.gov/webdocs/publications/43854/46734_eib124.pdf
Gomes, G. N., Vidal, F. N., Khandpur. N., et al. (2023). Association Between Consumption of Ultraprocessed Foods and Cognitive Decline. JAMA Neurol, 80(2),142–150. https://doi.org/10.1001/jamaneurol.2022.4397
Hemamy, M., Heidari-Beni, M., Askari, G., Karahmadi, M., & Maracy, M. (2020). Effect of Vitamin D and Magnesium Supplementation on Behavior Problems in Children with Attention-Deficit Hyperactivity Disorder. Int J Prev Med, 11(1), 4. https://doi.org/10.4103/ijpvm.IJPVM_546_17
Henry, K. (2023). An Integrative Medicine Approach to ADHD. Rupa Health. Accessed September 30, 2023. https://www.rupahealth.com/post/an-integrative-medicine-approach-to-adhd
Henry, K. & CNS, L.A. (2023). Natural treatments for ADHD. Webinar Presentation by IntegrativePractitioner.com and sponsored by Rupa Health, June 6, 2023 https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback?
Hemamy, M., Pahlavani, N., Amanollahi, A. et al. (2021). The effect of vitamin D and magnesium supplementation on the mental health status of attention-deficit hyperactive children: a randomized controlled trial. BMC Pediatr, 21, 178. https://doi.org/10.1186/s12887-021-02631-1
Konofal, E., Lecendreux, M., Arnulf, I., & Mouren, M. (2004). Iron Deficiency in Children With Attention-Deficit/Hyperactivity Disorder. Arch Pediatr Adolesc Med, 158(12), 1113–1115. https://doi.org/10.1001/archpedi.158.12.1113
Kotsi, E., Kotsi, E. & Perrea, D.N. (2019). Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): a meta-analysis. ADHD Atten Def Hyp Disord, 11, 221–232. https://doi.org/10.1007/s12402-018-0276-7
LaChance, L.R. & Ramsey, D. (2018). Antidepressant foods: An evidence-based nutrient profiling system for depression. World J Psychiatr, 8(3): 97-104. World J Psychiatr., 8(3): 97-104. https://doi.org/10.5498/wjp.v8.i3.97
Landaas, E.T., Aarsland, T.I., Ulvik, A., Halmøy, A., Ueland. P.M., & Haavik, J. (20166). Vitamin levels in adults with ADHD. BJPsych Open, 2(6), 377-384. https://doi.org/10.1192/bjpo.bp.116.003491
Linday, L.A. (2010). Cod liver oil, young children, and upper respiratory tract infections. J Am Coll Nutr, 29(6), 559-62. https://doi.org/10.1080/07315724.2010.10719894
Leoci, R. & Ruberti, M. (2021) Pesticides: An Overview of the Current Health Problems of Their Use. Journal of Geoscience and Environment Protection, 9, 1-20. https://doi.org/10.4236/gep.2021.98001
Lustig, R.H. (2021). Metaboical: The lure and the lies of processed food, nutrition, and modern medicine. New York: Harper Wave. https://www.amazon.com/Metabolical-processed-poisons-people-planet/dp/1529350077
MacInerney, E. K., Swatzyna, R. J., Roark, A. J., Gonzalez, B. C., & Kozlowski, G. P. (2017). Breakfast choices influence brainwave activity: Single case study of a 12-year-old female. NeuroRegulation, 4(1), 56–62. https://doi.org/10.15540/nr.4.1.56
McCann, D., Barrett, A., Cooper, A., Crumpler, D., Dalen, L., Grimshaw, K., et al. (2007). Food additives and hyperactive behavior in 3-year old and 8/9-year-old children in the community: a randomized, double-blinded, placebo-controlled trial. Lancet, 370(9598), 1560-1567. https://doi.org/10.1016/S0140-6736(07)61306-3
Mengying, L.I, Fallin, A, D., Riley,A., Landa, R., Walker, S.O., Silverstein, M., Caruso, D., et al. (2016). The Association of Maternal Obesity and Diabetes With Autism and Other Developmental Disabilities. Pediatrics, 137(2), e20152206. https://doi.org/10.1542/peds.2015-2206
Mousain-Bosc, M., Roche, M., Polge, A., Pradal-Prat, D., Rapin, J., & Bali, J.P. (2006). Improvement of neurobehavioral disorders in children supplemented with magnesium-vitamin B6. I. Attention deficit hyperactivity disorders. Magnes Res. 19(1), 46-52. https://pubmed.ncbi.nlm.nih.gov/16846100/#:~:text=In%20almost%20all%20cases%20of,increase%20in%20Erc%2DMg%20values.
Ney, J. (2022). Food Deserts and Inequality. Social Policy Data Lab. Updated: Jan 24, 2022. Accessed September, 23, 2023. https://www.socialpolicylab.org/post/grow-your-blog-community
Peper, E. (2023a). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. the peperperspective July 2, 2023. Accessed august 8, 2024, https://peperperspective.com/2023/07/04/reflections-on-the-increase-in-autism-adhd-anxiety-and-depression-part-1-bonding-screen-time-and-circadian-rhythms/
Peper, E. (2023b). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation, 10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Pollan, M. (2006). Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules. New York Penguin Press. https://www.amazon.com/Omnivores-Dilemma-Natural-History-Meals/dp/1594200823/ref=tmm_hrd_swatch_0?_
Pollan, M. (2011). Food rules. New York Penguin Press. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/B00VSBILFG/ref=tmm_hrd_swatch_0?
Pongpitakdamrong, A., Chirdkiatgumchai, V., Ruangdaraganon, N., Roongpraiwan, R., Sirachainan, N., Soongprasit, M., & Udomsubpayakul, U. (2022). Effect of Iron Supplementation in Children with Attention-Deficit/Hyperactivity Disorder and Iron Deficiency: A Randomized Controlled Trial. Journal of Developmental & Behavioral Pediatrics, 43(2), 80-86., https://doi.org/10.1097/DBP.0000000000000993
Porto, A. & Abu-Alreesh, S. (2022). Vitamin D for babies, children & adolescents. Health Living. Healthychildren.org. Accessed September 24, 2023. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/vitamin-d-on-the-double.aspx#
Poudineh, M., Parvin, S., Omidali, M., Nikzad, F., Mohammadyari, F., Sadeghi Poor Ranjbar, F., F., Nanbakhsh, S., & Olangian-Tehrani, S. (2023). The Effects of Vitamin Therapy on ASD and ADHD: A Narrative Review. CNS & Neurological Disorders – Drug Targets (Formerly Current Drug Targets – CNS & Neurological Disorders), (22), 5, 2023, 711-735. https://doi.org/10.2174/1871527321666220517205813
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Ríos-Hernández, A., Alda, J.A., Farran-Codina, A., Ferreira-García, E., & Izquierdo-Pulido, M. (2017). The Mediterranean Diet and ADHD in Children and Adolescents. Pediatrics, 139(2):e20162027. https://doi.org/10.1542/peds.2016-2027
Ryu, S.A., Choi, Y.J., An, H., Kwon, H.J., Ha, M., Hong, Y.C., Hong, S.J., & Hwang, H.J. (2022). Associations between Dietary Intake and Attention Deficit Hyperactivity Disorder (ADHD) Scores by Repeated Measurements in School-Age Children. Nutrients, 14(14), 2919. https://doi.org/10.3390/nu14142919
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Swanson, N.L., Leu, A., Abrahamson, J., & Wallet, B. (2014). Genetically engineered crops, glyphosate and the deterioration of health in the United States of America. Journal of Organic Systems, 9(2), 6-17. https://www.organic-systems.org/journal/92/JOS_Volume-9_Number-2_Nov_2014-Swanson-et-al.pdf
Swatzyna, R. J., Boutros, N. N., Genovese, A. C., MacInerney, E. K., Roark, A. J., & Kozlowski, G. P. (2018). Electroencephalogram (EEG) for children with autism spectrum disorder: Evidential considerations for routine screening. European Child & Adolescent Psychiatry, 28(5), 615–624. https://doi.org/10.1007/s00787-018-1225-x
Taleb, N. N. (2014). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. https://www.amazon.com/Antifragile-Things-That-Disorder-Incerto/dp/0812979680/ref=tmm_pap_swatch_0
Tohidi, S., Bidabadi, E., Khosousi, M.J., Amoukhteh, M., Kousha, M., Mashouf, P., Shahraki, T. (2021). Effects of Iron Supplementation on Attention Deficit Hyperactivity Disorder in Children Treated with Methylphenidate. Clin Psychopharmacol Neurosci, 19(4), 712-720. https://doi.org/10.9758/cpn.2021.19.4.712
Unal, D. Çelebi, F., Bildik,H.N., Koyuncu, A., & Karahan, S. (2019). Vitamin B12 and haemoglobin levels may be related with ADHD symptoms: a study in Turkish children with ADHD, Psychiatry and Clinical Psychopharmacology, 29(4), 515-519. https://doi.org/10.1080/24750573.2018.1459005
USDA. (2019). Fish oil, cod liver. FoodData Central. USDA U.S> Department of Agriculture. Published 4/1/2019. Accessed September 24, 2024. https://fdc.nal.usda.gov/fdc-app.html#/food-details/173577/nutrients
Van Tulleken, C. (2023). Ultra-Processed People. The Science Behind Food That Isn’t Food. New York: W.W. Norton & Company. https://www.amazon.com/Ultra-Processed-People-Science-Behind-Food/dp/1324036729/ref=asc_df_1324036729/?
Wahab, S., Muzammil, K., Nasir, N., Khan, M.S., Ahmad, M.F., Khalid, M., Ahmad, W., Dawria, A., Reddy, L.K.V., & Busayli, A.M. (2022). Advancement and New Trends in Analysis of Pesticide Residues in Food: A Comprehensive Review. Plants (Basel), 11(9), 1106. https://doi.org/10.3390/plants11091106
Wang. Y., Huang, L., Zhang, L., Qu, Y., & Mu, D. (2017). Iron Status in Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. PLoS One, 12(1):e0169145. https://doi.org/10.1371/journal.pone.0169145
Wilson, L. (2015). Mothers, beware: Your lifestyle choices will even affect your grandkids.
News Corp Australia Network. Accessed Jun 24, 2024. https://www.news.com.au/lifestyle/parenting/kids/mothers-beware-your-lifestyle-choices-will-even-affect-your-grandkids/news-story/3f326f457546cfb32af5c409f335fb56
Woo, H.D.,; Kim, D.W., Hong, Y.-S., Kim, Y.-M.,Seo, J.-H.,; Choe, B.M., Park, J.H.,; Kang, J.-W., Yoo, J.-H.,; Chueh, H.W., et al. (2014). Dietary Patterns in Children with Attention Deficit/Hyperactivity Disorder (ADHD). Nutrients, 6, 1539-1553. https://doi.org/10.3390/nu6041539
Zhong, C., Tessing, J., Lee, B.K., Lyall, K. Maternal Dietary Factors and the Risk of Autism Spectrum Disorders: A Systematic Review of Existing Evidence. Autism Res,13(10),1634-1658. https://doi.org/10.1002/aur.2402
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythm
Posted: July 4, 2023 Filed under: ADHD, behavior, computer, digital devices, education, emotions, Evolutionary perspective, health, laptops, screen fatigue, Uncategorized | Tags: anxiety, autism, bonding, circadian rhythms, depression, nature, still face experiment 10 Comments
Adapted from: Peper, E. Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation,10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Over the past two decades, there has been a significant increase in the prevalence of autism, Attention-Deficit/hyperactivity disorder (ADHD), anxiety, depression, and pediatric suicidal behavior. Autism rates have risen from 1 in 150 children in 2000 to 1 in 36 children in 2020 (CDC, 2023), while ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18-25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020), and depression rates for U.S. teens ages 12-17 have increased from 8% in 2007 to 13% in 2017 (Geiger & Davis, 2019; Walrave et al., 2022). Pediatric suicide attempts have also increased by 163% from 2009 to 2019 (Arakelyan et al., 2023), and during the COVID-19 pandemic, these rates have increased by more than 25% (WHO, 2022; Santomauro et al., 2021). In addition, the prevalence of these disorders has tripled for US adults during the pandemic compared to before (Ettman et al., 2020).
The rapid increase of these disorders is not solely due to improved diagnostic methods, genetic factors or the COVID-19 pandemic. The pandemic amplified pre-existing increasing trends. More likely, individuals who were at risk had their disorders triggered or amplified by harmful environmental and behavioral factors. Conceptually, Genetics loads the gun; epigenetics, behavior, and environment pull the trigger.
While behavioral strategies such as neurofeedback, Cognitive Behavior Therapy, biofeedback, meditation techniques, and pharmaceuticals can treat or ameliorate these disorders, the focus needs to be on risk reduction. In some ways, treatment can be likened to closing the barn doors after the horses have bolted.
Evolutionary perspective to reduce risk factors
Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto), provides an evolutionary perspective and offers simple rules of health by reducing risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, sugar, digital media).
- We do not need evidence of harm to claim that a drug or an unnatural procedure is dangerous. If evidence of harm does not exist, it does not mean harm does not exist.
- Only resort to medical techniques when the health payoff is very large (to save a life), exceeds its potential harm, such as incontrovertibly needed surgery or life-saving medicine (penicillin).
- Avoid the iatrogenics and negative side effects of prescribed medication.
Writer and scholar Taleb’s suggestions are reminiscent of the perspective described by the educator Joseph C. Pearce (1993) in his book, Evolution’s End. Pearce argued that modern lifestyles have negatively affected the secure attachment and bonding between caregivers and infants. The lack of nurturing and responsive caregiving in early childhood may lead to long-term emotional and psychological problems. He points out that we have radically adapted behaviors that differ from those that evolved over thousands of generations and that allowed us to thrive and survive. In the last 100 years, babies have often been separated from their mothers at birth or early infancy by being put in a nursery or separate room, limited or no breastfeeding with the use of formula, exposure to television for entertainment, lack of exploratory play outdoors, and the absence of constant caretakers in high-stress and unsafe environments.
As Pearce pointed out, “If you want true learning, learning that involves the higher frontal lobes – the intellectual, creative brain – then again, the emotional environment must be positive and supportive. This is because at the first sign of anxiety the brain shifts its functions from the high, prefrontal lobes to the old defenses of the reptilian brain… These young people need audio-vocal communication, nurturing, play, body movement, eye contact, sweet sounds and close heart contact on a physical level” (Mercogliano & Debus, 1999).
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past. The proposed recommendations are based upon Talib’s perspective that anything that was not part of our evolutionary past is probably harmful; thus, it is wise to remove the unnatural/unfamiliar and adopt the precautionary principle, which states that if evidence of harm does not exist, it does not mean harm does not exist (Kriebel et al., 2010).
This article is the first of a three-part series. Part 1 focuses on increasing reciprocal communication between infant and caretaker, reducing screen time, and re-establishing circadian rhythms; Part 2 focuses on reducing exposure to neurotoxins, eliminating processed foods, and supporting the human biome; and Part 3 focuses on respiration and movement.
Part 1- Increase bonding, reduce screen time, and re-establish circadian rhythms
Increase bonding between infant and caretaker
Infants develop emotional communication through reciprocal interactions with their caregivers, during which the caregiver responds to the infant’s expressions. When this does not occur, it can be highly stressful and detrimental to the infant’s development. Unfortunately, more and more babies are emotionally and socially isolated while their caregivers are focussed on, and captured by, the content on their digital screens. Moreover, infants and toddlers are entertained (babysat) by cellphones and tablets instead of dynamically interacting with their caretakers. Screens do not respond to the child’s expressions; the screen content is programmed to capture the infant’s attention through rapid scene changes. Without reciprocal interaction, babies often become stressed, as shown by the research of developmental psychologist Professor Edward Tronick, who conducted the “Still Face” experiment (Tronick & Beeghly, 2011; Weinberg et al, 2008).
The “Still Face” experiment illustrated what happens when caregivers are not responding to infants’ communication. The caregivers were asked to remain still and unresponsive to their babies, resulting in the infants becoming increasingly distressed and disengaged from their surroundings. Not only does this apply to infants but also to children, teenagers and older individuals. Watch the short Still Face experiment, which illustrates what happens when the caretaker is not responding to the infant’s communication.
Recommendation. Do not use cellphone and digital media while being with an infant in the first two years of life. It is important for caregivers to limit their cellphone use and prioritize reciprocal interactions with their infants for healthy emotional and psychological development.
Reduce screen time (television, social media, streaming videos, gaming)[1]
From an evolutionary perspective, screen time is an entirely novel experience. Television, computers, and cellphones are modern technologies that have significantly impacted infants’ and young people’s development. To grow, infants, toddlers, and children require opportunities to explore the environment through movement, touch, and play with others, which is not possible with screens. Research has shown that excessive screen time can negatively affect children’s motor development, attention span, socialization skills, and contribute to obesity and other health problems (Hinkley et al., 2014; Carson et al., 2016; Mark, 2023).
When four-year-olds watch fast-paced videos, they exhibit reduced executive functions and impulse control, which may be a precursor for ADHD, compared to children who engage in activities such as drawing (Lillard & Peterson, 2011; Mark, 2023).
Furthermore, excessive screen time and time spent on social media are causal in increasing depression in young adults-–as was discovered when Facebook became available at selected universities. Researchers compared the mental health of students at similar universities where Facebook was or was not available and observed how the students’ mental health changed when Facebook became available (Braghieri et al., 2022). Their research showed that “College-wide access to Facebook led to an increase in severe depression by 7% and anxiety disorders by 20%. In total, the negative effect of Facebook on mental health appeared to be roughly 20% the magnitude of what is experienced by those who lose their job” (Walsh, 2022).
Exposure to digital media has also significantly reduced our attention span from 150 seconds in 2004 to an average of 44 seconds in 2021. The shortening of attention span may contribute to the rise of ADHD and anxiety (Mark, 2022, p. 96).
Recommendations: Reduce time spent on social media, gaming, mindlessly following one link after the other, or watching episode after episode of streaming videos. Instead, set time limits for screen use, turn off notifications, and prioritize in-person interactions with friends, family and colleagues while engaging in collaborative activities. Encourage children to participate in physical and social activities and to explore nature.
To achieve this, follow the guidelines from the American Academy of Pediatrics’ recommendation on screen time (Council on Communications and Media, 2016), which suggest these limits on screen time for children of different age groups:
- Children under 18 months of age should avoid all screen time, except for video chatting with family and friends.
- Children aged 18-24 months should have limited screen time, and only when watched together with a caretaker.
- Children aged 2 to 5 years should have no more than one hour of screen time per day with parental supervision.
- For adolescents, screen and social media time should be limited to no more than an hour a day.
In our experience, when college students reduce their time spent on social media, streaming videos, and texting, they report that it is challenging; however, they then report an increase in well-being and performance over time (Peper et al., 2021). It may require more effort to provide children with actual experiential learning and entertainment than allowing them to use screens, but it is worthwhile. Having children perform activities and play outdoors–in a green nature environment–appears to reduce ADHD symptoms (Louv, 2008; Kuo & Taylor, 2004).
Reestablish circadian (daily) rhythms
Our natural biological and activity rhythms were regulated by natural light until the 19th century. It is hard to imagine not having light at night to read, to work on the computer, or to answer email. However, light not only illuminates, but also affects our physiology by regulating our biological rhythms. Exposure to light at night can interfere with the production of melatonin, which is essential for sleep. Insufficient sleep affects 30% of toddlers, preschoolers, and school-age children, as well as the majority of adolescents. The more media is consumed at bedtime, the more bedtime is delayed and total sleep time is reduced (Hale et al., 2018). Reduced sleep is a contributing factor to increased ADHD symptoms of inattention, hyperactivity and impulsivity (Cassoff et al., 2012).
Recommendations: Support the circadian rhythms. Avoid screen time one hour before bedtime. This will reduce exposure to blue light and reduce sympathetic arousal triggered by the content on the screen or reactions to social media and emails. Sleep in total darkness, and establish a regular bedtime and waking time to avoid “social jetlag,” which can negatively affect health and performance (Caliandro et al., 2021). Implement sleep hygiene strategies such as developing a bedtime ritual to improve sleep quality (Stager et al., 2023; Suni, 2023). Thus, go to bed and wake up at the same time each day, including weekends. Avoid large meals, caffeine, and alcohol before bedtime. Consistency is key to success.
Conclusion
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past, and explore strategies that support behaviors that have allowed the human being to thrive and survive. Improve clinical outcomes and optimize health by enhancing reciprocal communication interactions, reducing screen time and re-establishing the circadian rhythm.
References
Arakelyan, M., Freyleue, S., Avula, D., McLaren, J.L., O’Malley, A.J., & Leyenaar, J.K. (2023). Pediatric Mental Health Hospitalizations at Acute Care Hospitals in the US, 2009-2019. JAMA, 329(12), 1000–1011. https://doi.org/10.1001/jama.2023.1992
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Caliandro, R., Streng, A.A., van Kerkhof, L.W.M., van der Horst, G.T.J., & Chaves, I. (2021). Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients, 13(12), 4543. https://doi.org/10.3390/nu13124543
Carson, V., Tremblay, M.S., Chaput, J.P., & Chastin, S.F. (2016). Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab, 41(6 Suppl 3), S294-302. https://doi.org/10.1139/apnm-2016-0026
Cassoff, J., Wiebe, S.T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nat Sci Sleep, 4, 73-80. https://doi.org/10.2147/NSS.S31269
CDC. (2022). Attention-Deficit/hyperactivity disorder (ADHD): ADHD through the years. Centers for Disease Control and Prevention. Assessed March 27, 2023. https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. (2023). Data & Statistics on Autism Spectrum Disorder. CDC Centers for Disease Control and Prevention. Assessed March 25, 2023. https://www.cdc.gov/ncbddd/autism/data.html
Council on Communications and Media. (2016). Media and young minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M.,& Galea, S. (2020), Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Geiger, A.W. & Davis, L. (2019). A growing number of American teenagers-particularly girls-are facing depression. Pew Research Center. Accessed March 28, 2023.
Goodwin, R.D., Weinberger, A.H., Kim, J.H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. J Psychiatr Res. 130, 441-446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hale, L., Kirschen, G/W., LeBourgeois, M.K., Gradisar, M., Garrison, M.M., Montgomery-Downs, H., Kirschen, H., McHale, S.M., Chang, A.M., & Buxton, O.M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc Psychiatr Clin N Am, 27(2),229-245. https://doi.org/10.1016/j.chc.2017.11.014
Hinkley, T., Verbestel, V., Ahrens, W., Lissner, L., Molnár, D., Moreno, L.A., Pigeot, I., Pohlabeln, H., Reisch, L.A., Russo, P., Veidebaum, T., Tornaritis, M., Williams, G., De Henauw, S., De Bourdeaudhuij, I; IDEFICS Consortium. (2014). Early childhood electronic media use as a predictor of poorer well-being: a prospective cohort study. JAMA Pediatr,. May;168(5):485-92. https://doi.org/10.1001/jamapediatrics.2014.94
Kriebel, D., Tickner, J., Epstein, P., Lemons, J., Levins, R., Loechler, E.L., Quinn, M., Rudel, R., Schettler, T., Stoto, M. (2001). The precautionary principle in environmental science. Environ Health Perspect, 109(9):871-6. https://doi.org/10.1289/ehp.01109871
Kuo. F.E. & Taylor, A.F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 94(9),1580-6. https://doi.org/10.2105/ajph.94.9.1580
Lillard, A.S. & Peterson, J. The immediate impact of different types of television on young children’s executive function. Pediatrics, 128(4), 644-9. https://doi.org/10.1542/peds.2010-1919
Louv, R. (2008). Last Child in the Woods: Saving Our Children from Nature-Deficit Disorder. Algonquin Books. Chapel Hill, NC: Algonquin Books
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press.
Mercogliano, C. & Debus, K. (1999). Nurturing Heart-Brain Development Starting With Infants 1999 Interview with Joseph Chilton Pearce. Journal of Family Life, 5(1). https://www.michaelmount.co.za/nurturing-heart-brain-development-starting-with-infants-1999-interview-with-joseph-chilton-pearce/
Pearce, J.C. (1993). Evolutions’s End. New York: HarperOne.
Peper, E., Wilson, V., Martin, M., Rosegard, E., & Harvey, R. (2021). Avoid Zoom fatigue, be present and learn. NeuroRegulation, 8(1), 47–56. https://doi.org/10.15540/nr.8.1.47
Santomauro, D.F., Mantilla Herrera, A.M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D.M., Abbafati, C., Adolph, C., …. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(103121700-1712., https://doi.org/10.1016/S0140-6736(21)02143-7
Stager, L.M., Caldwell, A., Bates, C., & Laroche, H. (2023). Helping kids get the sleep they need. Society of Behavioral Medicine. Accessed March 29, 2023 https://www.sbm.org/healthy-living/helping-kids-get-the-sleep-they-need?gclid=Cj0KCQjww4-hBhCtARIsAC9gR3ZM7v9VSvqaFkLnceBOH1jIP8idiBIyQcqquk5y_RZaNdUjAR9Wpx4aAhTBEALw_wcB
Suni, E. (2023). Sleep hygiene- What it is, why it matters, and how to revamp your habits to get better nightly sleep. Sleep Foundation. Accessed March 29, 2023. https://www.sleepfoundation.org/sleep-hygiene
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto) Random House Publishing Group. (Kindle Locations 5906-5908).
Tronick, E. & Beeghly, M. (2011).Infants’ meaning-making and the development of mental health problems. Am Psychol, 66(2),107-19. https://doi.org/10.1037/a0021631
Walrave, R., Beerten, S.G., Mamouris, P. et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 23, 163 (2022). https://doi.org/10.1186/s12875-022-01769-w
Walsh, D. (2022 September 14). Study: Social media use linked to decline in mental health. MIT Management Ideas Made to Matter. Accessed March 28, 2023. https://mitsloan.mit.edu/ideas-made-to-matter/study-social-media-use-linked-to-decline-mental-health#:~:text=College%2Dwide%20access%20to%20Facebook,with%20either%20psychotherapy%20or%20antidepressants
Weinberg, M.K., Beeghly, M., Olson, K.L., & Tronick, E. (2008). A Still-face Paradigm for Young Children: 2½ Year-olds’ Reactions to Maternal Unavailability during the Still-face. J Dev Process, 3(1):4-22. https://pubmed.ncbi.nlm.nih.gov/22384309/
WHO (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. Assessed march 26, 2023. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
[1] The critique of social media does not imply that there are no benefits. If used judiciously, it is a powerful tool to connect with family and friends or access information.
Hope for insomnia, depression, anxiety, ADHD, exhaustion, and nasal congestion -Breathe light, slow and deep
Posted: July 9, 2022 Filed under: ADHD, behavior, Breathing/respiration, emotions, Exercise/movement, health, Pain/discomfort, relaxation, Uncategorized | Tags: allergies, anxiety, asthma, depression, hyperventilation, insomnia, nasal congestion, nose breathing Leave a commentAnxiety, depression, insomnia, exhaustion, ADHD, allergies, poor performance have all increased (Barendse et al., 2021; London & Landes, 2021; Peper et al, 2022a; Peper et al, 2022b; Vasileiadou et al, 2021). One of the unrecognized contributing factor is dysfunctional mouth breathing (McKeown, 2022). Improve health by learning to breathe in and out through the nose during the day and night. Listen to the inspiring presentation by Patrick McKeown, author of the superb book, The breathing cure-Develop new habits for a healthier, happier & long life (McKeown, 2022). In this presentation, he describes the science behind these disorders, the rationale for breathing light, slow and deep and offers simple breathing exercises to reduce symptoms and improve performance.
References
Barendse, M., Flannery, J., Cavanagh, C., Aristizabal, M., Becker, S. P., Berger, E., … & Pfeifer, J. (2021). Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID-19 pandemic: A collaborative of 12 samples from 3 countries. https://doi.org/10.31234/osf.io/hn7us
London, A.S. & Landes, S.D. (2021). Cohort Change in the Prevalence of ADHD Among U.S. Adults: Evidence of a Gender-Specific Historical Period Effect. Journal of attention disorders, 25(6), 771-782. https://doi.org/10.1177/1087054719855689
McKeown, P. (2022). The breathing cure-Develop new habits for a healthier, happier & long life. West Palm Beach, FL: Humanix Books.
Peper, E. (2022). Reduce anxiety. the peperperspective. https://peperperspective.com/2022/03/23/reduce-anxiety/
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022b). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Vasileiadou, S., Ekerljung, L., Bjerg, A., & Goksor, E. (2021). Asthma increased in young adults from 2008–2016 despite stable allergic rhinitis and reduced smoking. PLoS ONE, 16(6): e0253322. https://doi.org/10.1371/journal.pone.0253322
Evolutionary traps: How screens, digital notifications and gaming software exploits fundamental survival mechanisms
Posted: January 17, 2020 Filed under: ADHD, behavior, digital devices, emotions, Evolutionary perspective, Uncategorized | Tags: Aggression, CBT, depression, gaming, media, mental rehearsal 6 CommentsErik Peper and Richard Harvey
If athletes, psychologists, business executives, actors, students, politicians, job seekers and others use mental and actual rehearsal to improve their performances, would repeated watching of violent and aggressive streaming-videos, or playing hours and hours of first-shooter computer games be a form of rehearsal for aggressive behavior?
Arguably, mental and actual rehearsal is positively associated with improving health, such as preparing for an athletic competition or an academic exam and is negatively associated with health when playing aggressive, violent first-person shooter video games, or continuously watching aggressive or violent content on a variety of streaming platforms. Rehearsal–whether physical or in our imagination–impacts our health and performance in school, sports, therapy, politics, business and health. Choose to rehearse activities that improve health and well-being.
- Athletes use mental rehearsal to improve sports performance (Peper & Aita, 2017; Schenk & Miltenberger, 2019).
- Surgeons use mental rehearsal and actual practice to improve performance (Spiotta et al., 2018).
- Psychologists use cognitive behavioral therapy (CBT) rehearsal techniques to reduce anxiety and depression (Dobson & Dobson, 2018; Yamada et al, 2018; Cook, Mostazir, & Watkins, 2019)
- Successful business executives rehearse presentations before a staff meeting (Couch & Citrin, 2018).
- Actors and performers spend hours and days rehearsing their roles so that they portray and act it realistically during the performance .
- Students take practice exams so that they will perform better on the actual exam.
- Politicians, lawyers, and many others rehearse and practice being able to answer unexpected questions.
- Job seekers rehearse elevator pitches so that they transmit in a few words what is important
Mechanisms of rehearsal
Both mental and physical rehearsal strengthens neurochemical connections in the brain so that the rehearsed behaviors become more automated, fluid and unconscious. There is a saying in neurosciences, “Neurons that fire together wire together.” –the more you rehearse a task, the more those specific neurological pathways are strengthened, leading to automatic and efficient outcomes.
We now spend hours a day being exposed to digital displays on our phones, computers, gaming consoles and other digital devices, immersing ourselves in content reflecting life promoting, positive behavior and sometimes violent, negative behavior. Children and adults spend much of their free time looking at screens, texting, playing computer games, updating social media sites with moment by moment accounts of sometimes trivial activities, or going down the rabbit hole by following one hyperlinks after another. As we do this, we are unaware how much time has frittered away without actually doing anything productive. Below are some recent estimates of ‘daily active user’ minutes per day that uses a screen.
- Facebook about an hour per day
- Instagram just under an hour per day
- Texting about 45 minutes per day
- Internet browsing, about 45 minutes per day
- Snapchat, about 30 minutes per day
- Twitter, about 25 minutes per day
Adolescents interact with media for over 40 hours per week, or around 6 hours per day!
In spending much of our time with the screens, we rehearse a variety of physical body postures as well as a variety of cognitive and behavioral states that impact our physical, mental, emotional and social health. Many researchers have lamented the loss of some social skills that develop during physical face-to-face contact. The colloquial phrase, Use it or lose it, raises several questions about what is being lost when we spend so much of our waking time interacting with screens instead actually with other people?
It is almost impossible not to be distracted by the digital screen. The powerful audiovisual formats override our desire to do something different that some of us become enslaved to watching streaming videos, playing computer games or texting. Moreover, the ongoing visual and auditory notifications from our apps interrupts and/or capture our attention. Why is it difficult to turn away from visual or auditory stimuli? The answer has roots in our survival.
To attend to stimuli is an automatic evolutionary survival response. If we did not attend, we would not survive–Is the slight movement to the far right, just at the edge of our peripheral vision, a predator ready to attack?

Tiger in Kanha National Park, Madhya Pradesh, India
Each time a stimulus occurs, we need to check it out to see if it is friend or foe, safety or danger. The response is so automatic that we are unaware that we have reacted until after we have responded. We all have experienced this. When a computer screen or cellphone screen is held by the stranger next to us, we automatically look at their screen and we may even begin to read their emails. Although we know that peering at some else’s screen is not proper, we are still feel compelled to do it!
Similarly, screens displaying computer games and other media can capture or hijack our attention by the rapid scene changes, primarily because the content is programmed so we receive intermittent rewards for our responses. For example, the sound or visual notifications from our apps, cellphone messages, or social media trigger an impulse to scan the environment for information that may be critical to our survival. Even without receiving notifications, we may anticipate or project that there may be new information on our social media accounts, and sometimes we become disappointed when the interval between notifications is long. One student talking to another might say: “Don’t worry, they’ll respond; It’s only been 30 seconds.” Anticipating responses from the media can interrupt what we are otherwise doing. For example, rather than finish our work, we check for updates on social media, even though we probably know that there are no new important messages to which we would have to respond right away.
The mechanisms that help us survive by scanning our environment for predators may now become an evolutionary trap and is exploited to capture as many eyeballs as possible to increase market share, advertising revenue, and corporate bottom line.
We usually blame the individual for lack of self-control instead of blaming the designers of the digital apps, games and displays who have exploited this biological survival mechanism. We expect that children have voluntary control as their brains are developing–but how could they not react to the stimuli that for thousands of generations, helped them to survive. It is similar to asking children to have control and say “No” to fast foods and sweets. The foods that were previously necessary for survival represented by moderate amounts of ‘salt, fat, acid, heat and sweet’ tastes are often found in excess in our modern commercial or packaged ‘fast food nation’ making it likely that people may fall into an evolutionary trap related to what they eat.
Presently, high levels of exposure to violent and aggressive streaming videos and computer games can be harmful as they provide the practice to rehearse violence, killing and aggression mentally. It would be too strong a statement to assert that everyone who plays violent video games will become delinquent, criminal or homicidal in an extreme form of aggression. According to the American Psychological Association Task Force on Video Game Violence in 2017, it may be asserted that high frequency, long duration, high intensity interactions with violent video games or similar media content is highly associated with angry and aggressive thoughts, desensitization to violence, and decreases in empathy or helping others (Calvert et al., 2017). Some forms of social media interactions also lead to a form of social isolation, loneliness (phoneliness) (Christodoulou, G., Majmundar, A., Chou, C-P, & Pentz, M.A., 2020; Kardaras, 2017). Digital content requires the individual to respond to the digital stimuli, without being aware of the many verbal and nonverbal communication cues (facial expressions, gestures, tone of voice, eye contact, body language, posture, touch, etc) that are part of social communication (Remland, 2016). It is no wonder that more and more adolescents experience anxiety, depression, loneliness, and attention deficit disorders with a constant ‘digital diet’ that some have suggested include not only media, but junk food as well .
The negative impact of watching digital media was prescient by Jerry Mander, one of the leading visionaries of the 20th century, in his 1978 book, Four Arguments for the Elimination of Television, as well as by Joseph C. Pearce, author of books on human development and child development, in his 1993 book, Evolution’s End.
More recently, two superb books detail the harm that the digital revolution has brought, along with recommended strategies for how to use modern technologies wisely and live successfully in an e-world. We are not saying to avoid the beneficial parts of the digital age. We are saying to be aware how some material and digital platforms prey upon our evolutionary survival mechanisms. Unfortunately, most people —especially children– have not evolved skills to counter the negative impacts of some types of media exposure. It may take parental control and societal policies to mitigate the damage and enhance the benefits of the digital age. We highly recommend the following two books.
Glow Kids by Nicholas Kardaras, PhD describes the impact of excessive texting and computer gaming as well as strategies how to use digital media wisely
Deep Work by Cal Newport, PhD describes the impact of constant interruptions and offers rules for focused success in a distracted world.

References:
Kardaras, N. (2017). Glow Kids, New York: St. Martin’s Griffin
Newport, C. (2019). Deep Work. New York: Grand Central Publishing
Pearce, J. C. (1993). Evolution’s End. New York: Harper One
Posture affects memory recall and mood
Posted: November 25, 2017 Filed under: Exercise/movement, self-healing, stress management, Uncategorized | Tags: cognitive therapy, depression, empowerment, energy, helplessness, memory, mood, posture, power posture, somatics 5 CommentsThis blog has been reprinted from: Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45 (2), 36-41.
When I sat collapsed looking down, negative memories flooded me and I found it difficult to shift and think of positive memories. While sitting erect, I found it easier to think of positive memories. -Student participant
 The link between posture and mood is embedded in idiomatic phrases such as walking tall, standing proud, and an upstanding citizen, versus collapsed, defeated, or in a slump–Language suggests that posture and mood/emotions are connected. Slumped posture is commonly observed in depression (Canales et al., 2010; Michalak et al., 2009) and adapting an upright posture increases positive affect, reduces fatigue, and increases energy in people with mild to moderate depression (Wilkes et al., 2017; Peper & Lin, 2012).
The link between posture and mood is embedded in idiomatic phrases such as walking tall, standing proud, and an upstanding citizen, versus collapsed, defeated, or in a slump–Language suggests that posture and mood/emotions are connected. Slumped posture is commonly observed in depression (Canales et al., 2010; Michalak et al., 2009) and adapting an upright posture increases positive affect, reduces fatigue, and increases energy in people with mild to moderate depression (Wilkes et al., 2017; Peper & Lin, 2012).
This blog describes in detail our research study that demonstrated how posture affects memory recall (Peper et al, 2017). Our findings may explain why depression is increasing the more people use cell phones. More importantly, learning posture awareness and siting more upright at home and in the office may be an effective somatic self-healing strategy to increase positive affect and decrease depression.
Background
Most psychotherapies tend to focus on the mind component of the body-mind relationship. On the other hand, exercise and posture focus on the body component of the mind/emotion/body relationship. Physical activity in general has been demonstrated to improve mood and exercise has been successfully used to treat depression with lower recidivism rates than pharmaceuticals such as sertraline (Zoloft) (Babyak et al., 2000). Although the role of exercise as a treatment strategy for depression has been accepted, the role of posture is not commonly included in cognitive behavior therapy (CBT) or biofeedback or neurofeedback therapy.
The link between posture, emotions and cognition to counter symptoms of depression and low energy have been suggested by Wilkes et al. (2017) and Peper and Lin (2012), . Peper and Lin (2012) demonstrated that if people tried skipping rather than walking in a slouched posture, subjective energy after the exercise was significantly higher. Among the participants who had reported the highest level of depression during the last two years, there was a significant decrease of subjective energy when they walked in slouched position as compared to those who reported a low level of depression. Earlier, Wilson and Peper (2004) demonstrated that in a collapsed posture, students more easily accessed hopeless, powerless, defeated and other negative memories as compared to memories accessed in an upright position. More recently, Tsai, Peper, and Lin (2016) showed that when participants sat in a collapsed position, evoking positive thoughts required more “brain activation” (i.e. greater mental effort) compared to that required when walking in an upright position.
Even hormone levels also appear to change in a collapsed posture (Carney, Cuddy, & Yap, 2010). For example, two minutes of standing in a collapsed position significantly decreased testosterone and increased cortisol as compared to a ‘power posture,’ which significantly increased testosterone and decreased cortisol while standing. As Professor Amy Cuddy pointed out in herTechnology, Entertainment and Design (TED) talk, “By changing posture, you not only present yourself differently to the world around you, you actually change your hormones” (Cuddy, 2012). Although there appears to be controversy about the results of this study, the overall findings match mammalian behavior of dominance and submission. From my perspective, the concepts underlying Cuddy’s TED talk are correct and are reconfirmed in our research on the effect of posture. For more detail about the controversy, see the article by Susan Dominusin in the New York Times, “When the revolution came for Amy Cuddy,”, and Amy Cuddy’s response (Dominus, 2017;Singal and Dahl, 2016).
The purpose of our study is to expand on our observations with more than 3,000 students and workshop participants. We observed that body posture and position affects recall of emotional memory. Moreover, a history of self-described depression appears to affect the recall of either positive or negative memories.
Method
Subjects: 216 college students (65 males; 142 females; 9 undeclared), average age: 24.6 years (SD = 7.6) participated in a regularly planned classroom demonstration regarding the relationship between posture and mood. As an evaluation of a classroom activity, this report of findings was exempted from Institutional Review Board oversight.
Procedure
While sitting in a class, students filled out a short, anonymous questionnaire, which asked them to rate their history of depression over the last two years, their level of depression and energy at this moment, and how easy it was for them to change their moods and energy level (on a scale from 1–10). The students also rated the extent they became emotionally absorbed or “captured” by their positive or negative memory recall. Half of the students were asked to rate how they sat in front of their computer, tablet, or mobile device on a scale from 1 (sitting upright) to 10 (completely slouched).
Two different sitting postures were clearly defined for participants: slouched/collapsed and erect/upright as shown in Figure 1. To assume the collapsed position, they were asked to slouch and look down while slightly rounding the back. For the erect position, they were asked to sit upright with a slight arch in their back, while looking upward.
 Figure 1. Sitting in a collapsed position and upright position (photo by Jana Asenbrennerova). Reprinted by permission from Gorter and Peper (2011).
Figure 1. Sitting in a collapsed position and upright position (photo by Jana Asenbrennerova). Reprinted by permission from Gorter and Peper (2011).
After experiencing both postures, half the students sat in the collapsed position while the other half sat in the upright position. While in this position, they were asked to recall/evoke as many hopeless, helpless, powerless, or defeated memories as possible, one after the other, for 30 seconds.
After 30 seconds they were reminded to keep their same position and let go of thinking negative memories. They were then asked to recall/evoke only positive, optimistic, or empowering memories for 30 seconds.
They were then asked to switch positions. Those who were collapsed switched to sitting erect, and those who were erect switched to sitting collapsed. Then they were again asked to recall/evoke as many hopeless, helpless, powerless, or defeated memories as possible one after the other for 30 seconds. After 30 seconds they were reminded to keep their same position and again let go of thinking of negative memories. They were then asked to recall/evoke only positive, optimistic, or empowering memories for 30 seconds, while still retaining the second posture.
They then rated their subjective experience in recalling negative or positive memories and the degree to which they were absorbed or captured by the memories in each position, and in which position it was easier to recall positive or negative experiences.
Results
86% of the participants reported that it was easier to recall/access negative memories in the collapsed position than in the erect position, which was significantly different as determined by one-way ANOVA (F(1,430)=110.193, p < 0.01) and 87% of participants reported that it was easier to recall/access positive images in the erect position than in the collapsed position, which was significantly different as determined by one-way ANOVA (F(1,430)=173.861, p < 0.01) as shown in Figure 2.
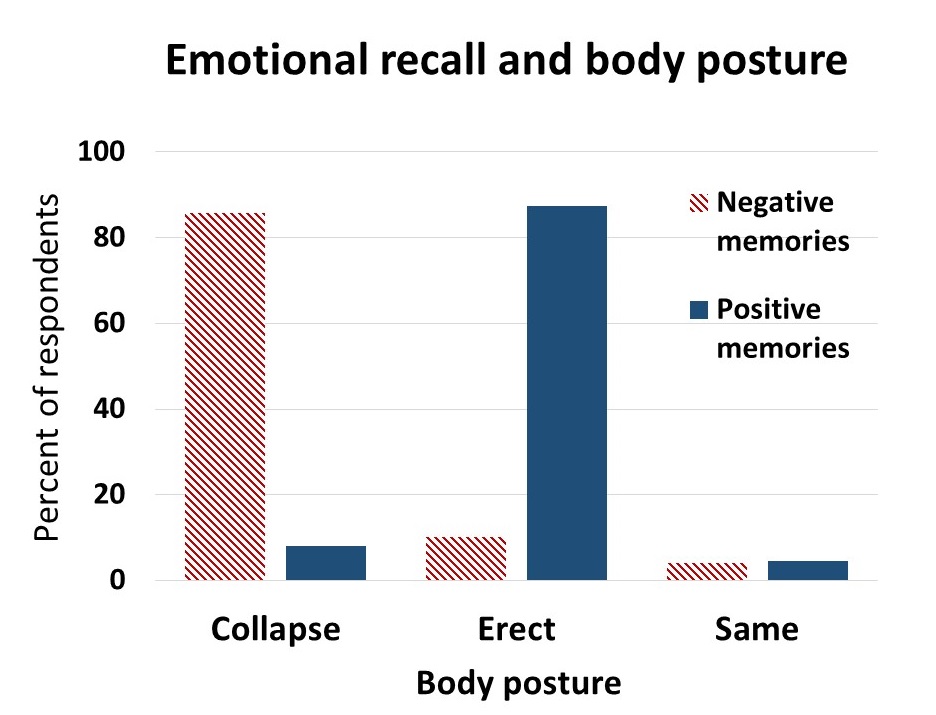 Figure 2. Percent of respondents who reported that it was easier to recall positive or negative memories in an upright or slouched posture.
Figure 2. Percent of respondents who reported that it was easier to recall positive or negative memories in an upright or slouched posture.
The difficulty or ease of recalling negative or positive memories varied depending on position as shown in Figure 3.
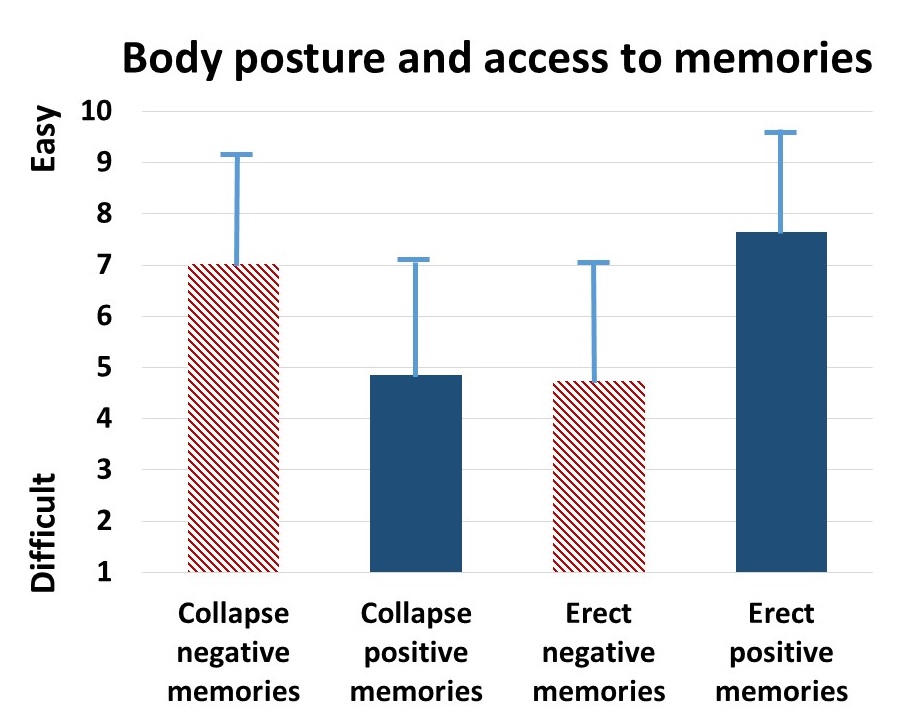 Figure 3. The relative subjective rating in the ease or difficulty of recalling negative and positive memories in collapsed and upright positions.
Figure 3. The relative subjective rating in the ease or difficulty of recalling negative and positive memories in collapsed and upright positions.
The participants with a high level of depression over the last two years (top 23% of participants who scored 7 or higher on the scale of 1–10) reported that it was significantly more difficult to change their mood from negative to positive (t(110) = 4.08, p < 0.01) than was reported by those with a low level of depression (lowest 29% of the participants who scored 3 or less on the scale of 1–10). It was significantly easier for more depressed students to recall/evoke negative memories in the collapsed posture (t(109) = 2.55, p = 0.01) and in the upright posture (t(110) = 2.41, p ≦0.05 he) and no significant difference in recalling positive memories in either posture, as shown in Figure 4.
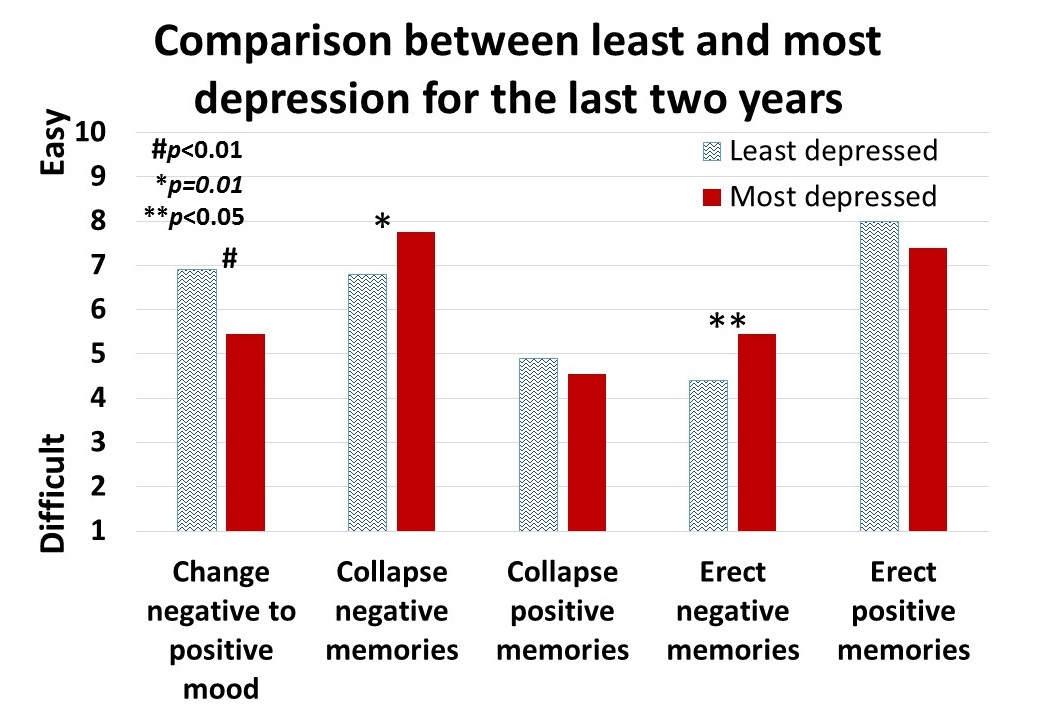 Figure 4. Differences is in memory access for participants with a history of least or most depression.
Figure 4. Differences is in memory access for participants with a history of least or most depression.
For all participants, there was a significant correlation (r = 0.4) between subjective energy level and ease with which they could change from negative to positive mood. There were no significance differences for gender in all measures except that males reported a significantly higher energy level than females (M = 5.5, SD = 3.0 and M = 4.7, SD = 3.8, respectively; t(203) = 2.78, p < 0.01).
A subset of students also had rated their posture when sitting in front of a computer or using a digital device (tablet or cell phone) on a scale from 1 (upright) to 10 (completely slouched). The students with the highest levels of depression over the last two years reporting slouching significantly more than those with the lowest level of depression over the last two years (M = 6.4, SD = 3.5 and M = 4.6, SD = 2.6; t(46) = 3.5, p < 0.01).
There were no other order effects except of accessing fewer negative memories in the collapsed posture after accessing positive memories in the erect posture (t(159)=2.7, p < 0.01). Approximately half of the students who also rated being “captured” by their positive or negative memories were significantly more captured by the negative memories in the collapsed posture than in the erect posture (t(197) = 6.8, p < 0.01) and were significantly more captured by positive memories in the erect posture than the collapsed posture (t(197) = 7.6, p < 0.01), as shown in Figure 5.
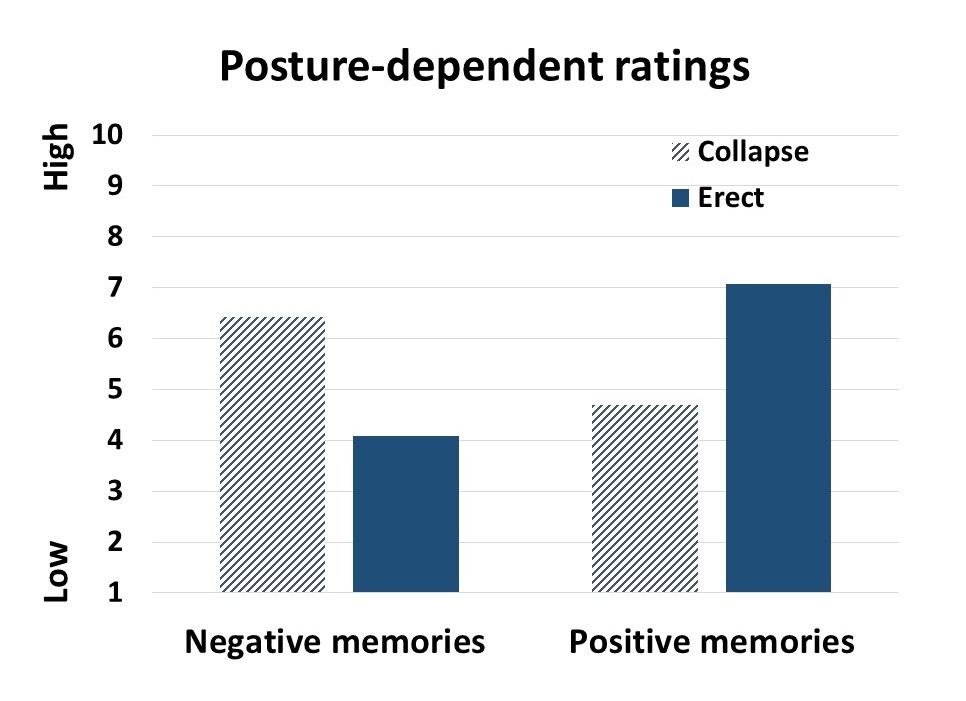 Figure 5. Subjective rating of being captured by negative and positive memories depending upon position.
Figure 5. Subjective rating of being captured by negative and positive memories depending upon position.
Discussion
Posture significantly influenced access to negative and positive memory recall and confirms the report by Wilson and Peper (2004). The collapsed/slouched position was associated with significantly easier access to negative memories. This is a useful clinical observation because ruminating on negative memories tends to decrease subjective energy and increase depressive feelings (Michi et al., 2015). When working with clients to change their cognition, especially in the treatment of depression, the posture may affect the outcome. Thus, therapists should consider posture retraining as a clinical intervention. This would include teaching clients to change their posture in the office and at home as a strategy to optimize access to positive memories and thereby reduce access or fixation on negative memories. Thus if one is in a negative mood, then slouching could maintain this negative mood while changing body posture to an erect posture, would make it easier to shift moods.
Physiologically, an erect body posture allows participants to breathe more diaphragmatically because the diaphragm has more space for descent. It is easier for participants to learn slower breathing and increased heart rate variability while sitting erect as compared to collapsed, as shown in Figure 6 (Mason et al., 2017).
 Figure 6. Effect of posture on respiratory breathing pattern and heart rate variability.
Figure 6. Effect of posture on respiratory breathing pattern and heart rate variability.
The collapsed position also tends to increase neck and shoulder symptoms This position is often observed in people who work at the computer or are constantly looking at their cell phone—a position sometimes labeled as the i-Neck.
Implication for therapy
In most biofeedback and neurofeedback training sessions, posture is not assessed and clients sit in a comfortable chair, which automatically causes a slouched position. Similarly, at home, most clients sit on an easy chair or couch, which lets them slouch as they watch TV or surf the web. Finally, most people slouch when looking at their cellphone, tablet, or the computer screen (Guan et al., 2016). They usually only become aware of slouching when they experience neck, shoulder, or back discomfort.
Clients and therapists are usually not aware that a slouched posture may decrease the client’s energy level and increase the prevalence of a negative mood. Thus, we recommend that therapists incorporate posture awareness and training to optimize access to positive imagery and increase energy.
References
Singal, J. and Dahl, M. (2016, Sept 30 ) Here Is Amy Cuddy’s Response to Critiques of Her Power-Posing Research. https://www.thecut.com/2016/09/read-amy-cuddys-response-to-power-posing-critiques.html
We thank Frank Andrasik for his constructive comments.
Exercise: Improve your health, mood, and cognitive function
Posted: July 22, 2017 Filed under: Uncategorized | Tags: depression, exercise, health, hypertension, mood, Sitting disease 1 CommentThrough millions of years, movement was part of our biological necessity.. Movement was necessary to hunt, to escape predators, to explore and to find a mate. Organisms developed a brain (nervous system) to coordinate movement as eloquently explain by neuroscientist Daniel Wolpert in his 2011 TED talk, The Real Reasons for Brains.
It is only recently that we limit movement by sitting, driving, taking the escalator, or controlling equipment that performs the actual physical labor. We interfere with our evolutionary developed physiology when we reduce or even eliminate movement for the sake of efficiency. Lack of movement, “sitting disease”, is a significant contributor and causal factor in illness. It also increases the stress response, negative mood and depression and reduces cognitive activity. Take charge and reduce illness when you integrate purposeful exercise (walking, running, dancing, etc.) into your life style.

Exercise is the most effective behavioral technique for self-regulation of mood in healthy people as summarized in the superb article, The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review, Dr. Julia C. Basso and Wendy A. Suzuki of the Center for Neural Science, New York University, New York, NY, USA. The robust research findings show that acute exercise improves mood, significantly reduces depression, tension, anger, fatigue, and confusion. In addition, acute exercise improves symptoms associated with psychological disorders such as depression, anxiety, schizophrenia, and post-traumatic stress disorder. Exercise decreases the risk of type 2 diabetes, coronary heart disease and stress-related blood pressure response by inhibiting the sympathetic nervous system response to stress. For a detailed summary, see the blogs, What is the best single thing we can do for our health and Healthy movement is the new aging.
Finally, the authors also review the relevant neurophysiological, and neurochemical processes that are affected by exercise. What is most interesting are the findings that “acute exercise primarily enhances executive functions dependent on the prefrontal cortex including attention, working memory, problem solving, cognitive flexibility, verbal fluency, decision making, and inhibitory control. These positive changes have been demonstrated to occur with very low to very high exercise intensities, with effects lasting for up to two hours after the end of the exercise bout.”
As the authors state, “We show that the three most consistent cognitive/behavioral effects of a single bout of exercise in humans are improved executive functions, enhanced mood states, and decreased stress levels.”
Even though the findings are clear that movement/exercise is a powerful “drug” to improve our health, most health professionals focus on sitting treatment and prescribing pharmaceutical agents. Possibly, a treatment session should start with fun physical exercise and followed by therapy. Remember, if you feel blah, have lower energy, feel frustrated or irritated, get up and move. Movement and exercise will change your mood. You will experience what Peper and Lin (2012), have shown that less than minute of skipping in place will significantly improve your subjective energy level and mood. Get up and skip in place, then observe how much better you feel. Then sit again read the article by Dr. Julia C. Basso and Wendy A. Suzuki, http://content.iospress.com/download/brain-plasticity/bpl160040?id=brain-plasticity%2Fbpl160040


 From:
From: 
