Beyond Zoom Fatigue: Re-energize Yourself and Improve Learning
Posted: November 24, 2020 Filed under: behavior, computer, digital devices, educationj, health, posture, stress management | Tags: boredom, learning, mind-body, zoom fatigue 7 CommentsErik Peper and Amber Yang
“Instead of zoning out and being on my phone half the time. I felt more engaged in the class and like I was actually learning something.” -21 year old college student
Before the pandemic, roughly, two-thirds of all social interactions were face-to-face—and when the shelter-in-place order hit our communities, we were all faced with the task of learning how to engage virtually. The majority of students reported that taking online classes instead of in person classes is significantly more challenging. It is easier to be distracted and multitask online—for example, looking at Instagram, Facebook, Twitter, TikTok, texting, surfing the internet, responding to notifications, listening to music, or drifting to sleep. Hours of watching TV and/or streaming videos have conditioned many people to sit and take in information passively, which discourages them from actively responding or initiating. The information is rapidly forgotten when the next screen image or advertisement appears. Effectively engaging on Zoom requires a shift from passively watching and listening to being an active, creative participant.
Another barrier to virtual engagement is that communicating online does not engage all senses. A considerable amount of our communication is nonverbal—sounds, movement, visuals, physical structures, touch, and body language. Without these sensory cues, it can be difficult to feel socially connected on Zoom, Microsoft Teams, or Google Meet to sustain attention and to focus especially if there are many people in the class or meeting. Another challenge to virtual learning is that without the normal environment of a classroom, many students across the country are forced to learn in emotionally and/or physically challenging environments, which gets in the way of maintaining attention and focus. The Center for Disease Prevention (CDC) reported that anxiety disorder and depressive disorder have increased considerably in the United States during the COVID-19 pandemic (Leeb et al, 2020; McGinty et al, 2020). Social isolation, stay-at-home orders, and coping with COVID-19 are contributing factors affecting mental health especially for minority and ethnic youth. Stress, anxiety and depression can greatly affect students’ ability to learn and focus.
The task of teaching has also become more stressful since many students are not visible or appear still-faced and non-responsive. Teaching to non-responsive faces is significantly more stressful since the presenter receives no social feedback. The absence of social feedback during communication is extremely stressful. It is the basis of Trier Social stress test in which a person presents for five minutes to a group of judges who provide no facial or verbal feedback (Allen et al, 2016; Peper, 2020).
The Zoom experience especially in a large class can be a no win situation for the presenter and the viewer. To help resolve this challenge, we explored a strategy to increase student engagement and reduce social stress of the teacher. In this exploration, we asked students to rate their subjective energy level, attention and involvement during a Zoom conducted class. For the next Zoom class, they were asked to respond frequently with facial and body expressions to the presentation. For example, students would expressively shake their head no or yes and/or use facial expressions to signal to the teacher that they were engaged and listening. Other strategies included giving thumbs up or thumbs down, making sounds, and changing your body posture as a response to the presentation. Watch the superb non-judgmental instructions adapted for high school students by Amber Yang.
When college students purposely implement and increase their animated facial and body responses by 123% during Zoom classes, they report a significant increase in frequency of animation (ANOVA (F(1,70) = 30.66, p < .0001), energy level (ANOVA (F(1,70) = 28.96, p < .0001), attention (ANOVA (F(1,70) = 16.87, p = .0001) and involvement (ANOVA (F(1,69) = 10.70, p = .002) as compared just attending normally in class (see Figure 1).
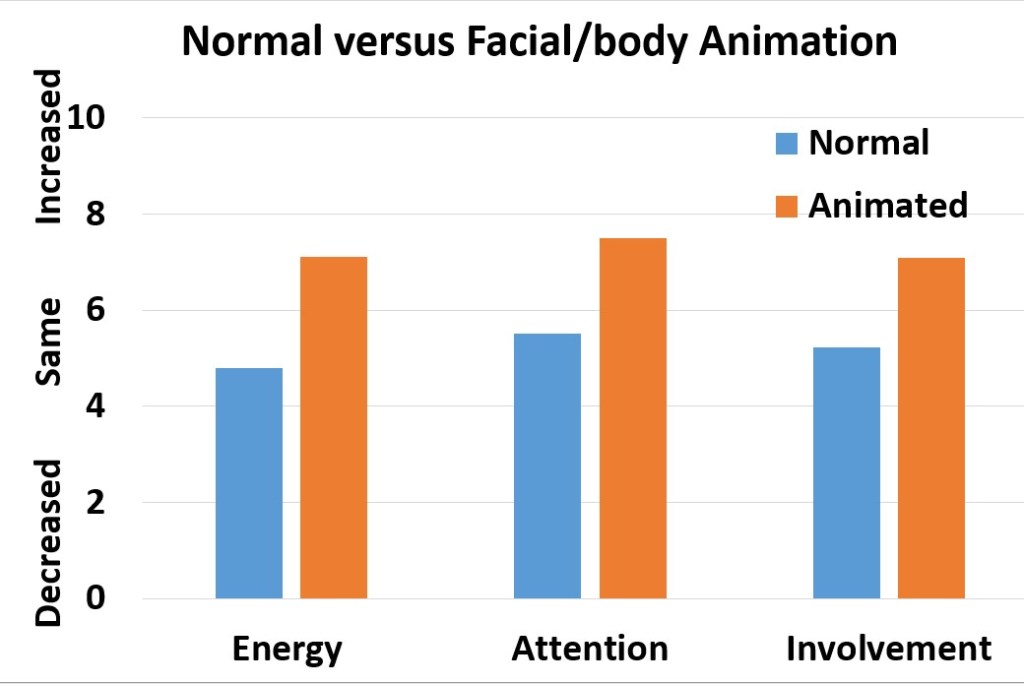
Figure 1. Change in subjective energy, attention and involvement when the students significantly increase their facial and body animation by 123 % as compared to their normal non-expressive class behavior (Peper & Yang, in press).
“I never realized how my expressions affected my attention. Class was much more fun” -22 year old college student
“I can see how paying attention and participation play a large role in learning material. After trying to give positive facial and body feedback I felt more focused and I was taking better notes and felt I was understanding the material a bit better.” –28 year old medical student
These quotes are a few of the representative reports by more than 80% of the students who observed that being animated and responsive helped them to stay present and learn much more easily and improve retention of the materials. For a few students, it was challenging to be animated as they felt shy, self-conscious and silly and kept wondering what other students would think of them.
Having students compare two different ways of being in Zoom class is a useful assignment since it allows students to discover that being animated and responsive with facial/body expression improves learning. So often we forget how our body impacts our thoughts and emotions. For example, when students were asked to sit in a slouched position, they reported that it was much easier to recall hopeless, helpless, powerless and defeated memories and more difficult to perform mental math in the slouched position. While in the upright position it was easier to access positive empowering memories and easier to perform mental math (Peper et al, 2017; Peper et al, 2018).
Experience how body posture affects emotional recall and feeling (adapted from Alda, 2018).
1) Stand up and configure your body in a position that signals defeat, hopelessness and depression (slouching with the head down). While holding this position, recall a memory of hopelessness and defeat. Notice any negative emotions that arise from this.
2) Shift and configure your body into a position that signals joy, happiness and success (standing tall, looking up with a smile). While holding this position, recall a memory of joy and happiness. Notice any positive emotions that arise from this.
3) Configure your body in a position that signals defeat, hopelessness and depression (slouching with the head down). While holding this position, recall a joy, happiness and success. Do not change your body position. End this configuration after holding it for a little while.
4) Shift and your body in a position that signals joy, happiness and success (standing tall, looking up with a smile). While holding this position, recall a memory of hopelessness and defeat. Do not change your body position. End this configuration after holding it for a little while.
When body posture and expression are congruent with the evoked emotion, it is almost always easier to experience the emotions. On the other hand, when the body posture expression is the opposite of the evoked emotion (e.g., the body in a positive empowered stance while recalling hopeless defeated memories) it is much more difficult to evoke and experience the emotion. This same concept applies to learning. When slouching and lying on the bed while in a Zoom class, it is much more difficult to stay present and not drift off. On the other hand, when sitting erect and upright and actively responding to the presentation, the body presence/posture invites the brain to focus for optimized learning.
Conclusion
In a Zoom environment, it is easy to slouch, drift away, and become non-responsive—which can exacerbate zoom fatigue symptoms and also decrease our capacity to learn, focus, and feel connected with the people around us. Take charge and actively participate in class by sitting up, maintaining an empowered posture, and using nonverbal facial and body expressions to communicate. The important concept is not how you show your animation, but that you actively participate within the constraints of your own limitations. For example, if a person is paralyzed the person will benefit if they do the experience internally even though their body may not show any expression. By engaging our soma we optimize our learning experience as we face the day-to-day challenges of the pandemic and beyond.
I noticed I was able to retain information better as well as enjoy the class more when I used facial-body responses. At times, where I would try to wonder off into bliss, I would catch myself and try to actively engage in the class with body movements even if there is no discussion. Animated face/body was a better learning experience. –21-year old college student.
References
Peper, E. (October 13, 2020). Breaking the social bond: The immobilized face. The Peper Perspective.
Peper, E., Wilson, V.E., Martin, M., Rosengard, E., & Harvey, R. (unpublished). Avoid Zoom fa
Tips to Reduce Zoom Fatigue
Posted: November 15, 2020 Filed under: behavior, computer, digital devices, ergonomics, Exercise/movement, health, laptops, Neck and shoulder discomfort, Pain/discomfort, self-healing, stress management, Uncategorized, vision 1 CommentAdapted from the book, TechStress: How Technology
is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics, by Erik Peper, Richard Harvey and Nancy Faass.



Peper, E., Harvey, R., & Faass, N. (2020), TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics. Berkeley, CA: North Atlantic Books.
Inna Khazan, PhD, interviews the authors of TechStress
Posted: August 18, 2020 Filed under: behavior, computer, digital devices, ergonomics, Evolutionary perspective, Exercise/movement, health, laptops, Neck and shoulder discomfort, Pain/discomfort, posture, stress management, Uncategorized, vision Leave a commentGo behind the screen and watch Inna Khazan, PhD, faculty member at Harvard Medical School and author of Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance, interview Erik Peper, PhD and Richard Harvey, PhD. coauthors of the new book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics.
Dr. Inna Khazan interviews Dr. Erik Peper about his new book Tech Stress. We talk about some of the ways in which technology overuse affects our health and what we can do about it.
Dr. Inna Khazan interviews Dr. Rick Harvey about his new book Tech Stress, the way technology overuse can affect adults and children, and what we can do about it.
Ways to reduce TechStress
Posted: August 13, 2020 Filed under: ADHD, behavior, computer, digital devices, emotions, ergonomics, Evolutionary perspective, Exercise/movement, health, Neck and shoulder discomfort, Nutrition/diet, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized 5 CommentsWe are excited about our book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics, that was published August 25, 2020.
Evolution shapes behavior — and as a species, we’ve evolved to be drawn to the instant gratification, constant connectivity, and the shiny lights, beeps, and chimes of our ever-present devices. In earlier eras, these hardwired evolutionary patterns may have set us up for success, but today they confuse our instincts, leaving us vulnerable and stressed out from fractured attention, missed sleep, skipped meals, aches, pains, and exhaustion and often addicted to our digital devices.
Tech Stress offers real, practical tools to avoid evolutionary pitfalls programmed into modern technology that trip us up. You will find a range of effective strategies and best practices to individualize your workspace, reduce physical strain, prevent sore muscles, combat brain drain, and correct poor posture. The book also provides fresh insights on reducing psychological stress on the job, including ways to improve communication with coworkers and family.
Although you will have to wait to have the book delivered to your home, you can already begin to implement ways to reduce physical discomfort, zoom/screen fatigue and exhaustion. Have a look the blogs below.
How evolution shapes behavior
How to optimize ergonomics
Cartoon ergonomics for working at the computer and laptop
Hot to prevent and reduce neck and shoulder discomfort
Why do I have neck and shoulder discomfort at the computer?
Relieve and prevent neck stiffness and pain
How to prevent screen fatigue and eye discomfort
Resolve Eyestrain and Screen Fatigue
How to improve posture and prevent slouching
“Don’t slouch!” Improve health with posture feedback
How to improve breathing and reduce stress
Anxiety, lightheadedness, palpitations, prodromal migraine symptoms? Breathing to the rescue!
How to protect yourself from EMF
Cell phone radio frequency radiation increases cancer risk

Available from: https://www.penguinrandomhouse.com/books/232119/tech-stress-by-erik-peper-phd/
Why do I have neck and shoulder discomfort at the computer?
Posted: July 23, 2020 Filed under: behavior, computer, digital devices, ergonomics, Exercise/movement, laptops, Neck and shoulder discomfort, Pain/discomfort, posture, Uncategorized 8 CommentsAdapted from the upcoming book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics, by Erik Peper, Richard Harvey and Nancy Faass.
While working in front of screens, many of us suffer from Zoom/screen fatigue, iNeck, shoulder and back discomfort, tired eyes, exhaustion and screen addiction (Peper, 2020; Fosslien & Duffy, 2020; So, Cheng & Szeto, 2017; Peper & Harvey, 2018). As we work, our shoulders and forearms tense and we are often not aware of this until someone mentions it. Many accept the discomfort and pain as the cost of doing work–not realizing that it may be possible to work without pain.
Observe how you and coworkers work at the computer, laptop or cellphone. Often we bring our noses close to the screen in order to the text more clearly and raise our shoulders when we perform data entry and use the mouse. This unaware muscle tension can be identified with physiological recording of the muscles electrical activity when they contract (electromyography) (Peper & Gibney, 2006; Peper, Harvey & Tylova, 2006). In most cases, when we rest our hands on our laps the muscle tension is low but the moment we even rest our hands on the keyboard or when we begin to type or mouse, our muscles may tighten, as shown in Figure 1. The muscle activity will also depend on the person’s stress level, ergonomic arrangement and posture.
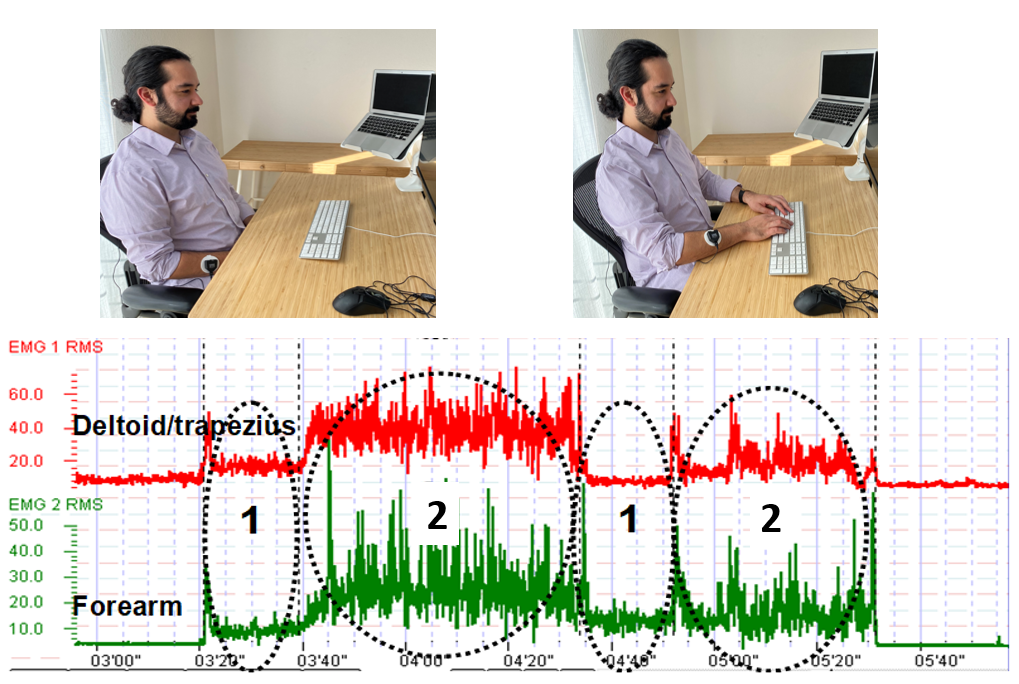 Figure 1. Muscle tension from the shoulder and forearm increased without any awareness when the person rested their hands on the keyboard (Rest Keyboard) and during typing and mousing. The muscles only relaxed when the hands were resting on their lap (Rest Lap) (reproduced by permission from Peper, Harvey, and Faass, 2020).
Figure 1. Muscle tension from the shoulder and forearm increased without any awareness when the person rested their hands on the keyboard (Rest Keyboard) and during typing and mousing. The muscles only relaxed when the hands were resting on their lap (Rest Lap) (reproduced by permission from Peper, Harvey, and Faass, 2020).
Stop reading from your screen and relax your shoulders. Did you feel them slightly drop and relax?
If you experienced this release of tension and relaxation in the shoulders, then you were tightening your shoulders muscles without awareness. It is usually by the end of the day that we experience stiffness and discomfort. Do the following exercise as guided by the video or described in the text below to experience how discomfort and pain develop by maintaining low-level muscle tension.
While sitting, lift your right knee two inches up so that the foot is about two inches away from the floor. Keep holding the knee up in this position. Did you notice your breathing stopped when you lifted your knee? Are you noticing increasing tension and discomfort or even pain? How much longer can you lift the knee up?
Let go, relax and observe how the discomfort dissipates.
Reasons for the discomfort
The discomfort occurred because your muscles were contracted, which inhibited the blood and lymph flow through the tissue. When your muscles contracted to lift your knee, the blood flow in those muscles was reduced. Only when your muscles relaxed could enough blood flow occur to deliver nutrients and oxygen as well as remove the waste products of metabolism (Wan et al, 2017). From a physiological perspective, muscles work most efficiently when they alternately contract and relax. For example, most people can walk without discomfort since their muscles contract and relax with each step. However, you could hold your knee up for a few minutes before experiencing discomfort in those same muscles.
How to prevent discomfort.
To prevent discomfort and optimize health, apply the same concept of alternating tensing and relaxing to your neck, shoulder, back and arm muscles while working. Every few minutes move your arms and shoulders and let them relax. Interrupt the static sitting position with movement. If you need reminders to get up and move your body during the workday or long periods sitting in front of a device, you can download and install the free app, StretchBreak.
For more information, read and apply the concepts described in our upcoming book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. The book explains why TechStress develops, why digital addiction occurs, and what you can do to prevent discomfort, improve health and enhance performance. Order the book from Amazon and receive it August 25th. Alternatively, sign up with the publisher and receive a 30% discount when the book is published August 25th. https://www.northatlanticbooks.com/shop/tech-stress/

References
Peper, E. & Gibney, K. H. (2006). Muscle Biofeedback at the Computer: A Manual to Prevent Repetitive Strain Injury (RSI) by Taking the Guesswork out of Assessment, Monitoring and Training. Amersfoort: The Netherlands: Biofeedback Foundation of Europe. ISBN 0-9781927-0-2. Free download of the the book: http://bfe.org/helping-clients-who-are-working-from-home/
Wan, J. J., Qin, Z., Wang, P. Y., Sun, Y., & Liu, X. (2017). Muscle fatigue: general understanding and treatment. Experimental & molecular medicine, 49(10), e384. https://doi.org/10.1038/emm.2017.194
Reduce initial dose of the virus and optimize your immune system
Posted: April 4, 2020 Filed under: behavior, health, stress management, Uncategorized | Tags: coronavirus, COVID-19, immune system, public health, technology 9 CommentsErik Peper and Richard Harvey
Adapted from:Peper, E. & Harvey, R. (September 13, 2020). Reduce Initial Dose of the Virus and Optimize Your Immune System. Townsend Letters-The Examiner of Alternative Medicine, 44. https://www.townsendletter.com/article/reduce-initial-dose-of-the-virus-and-optimize-your-immune-system/
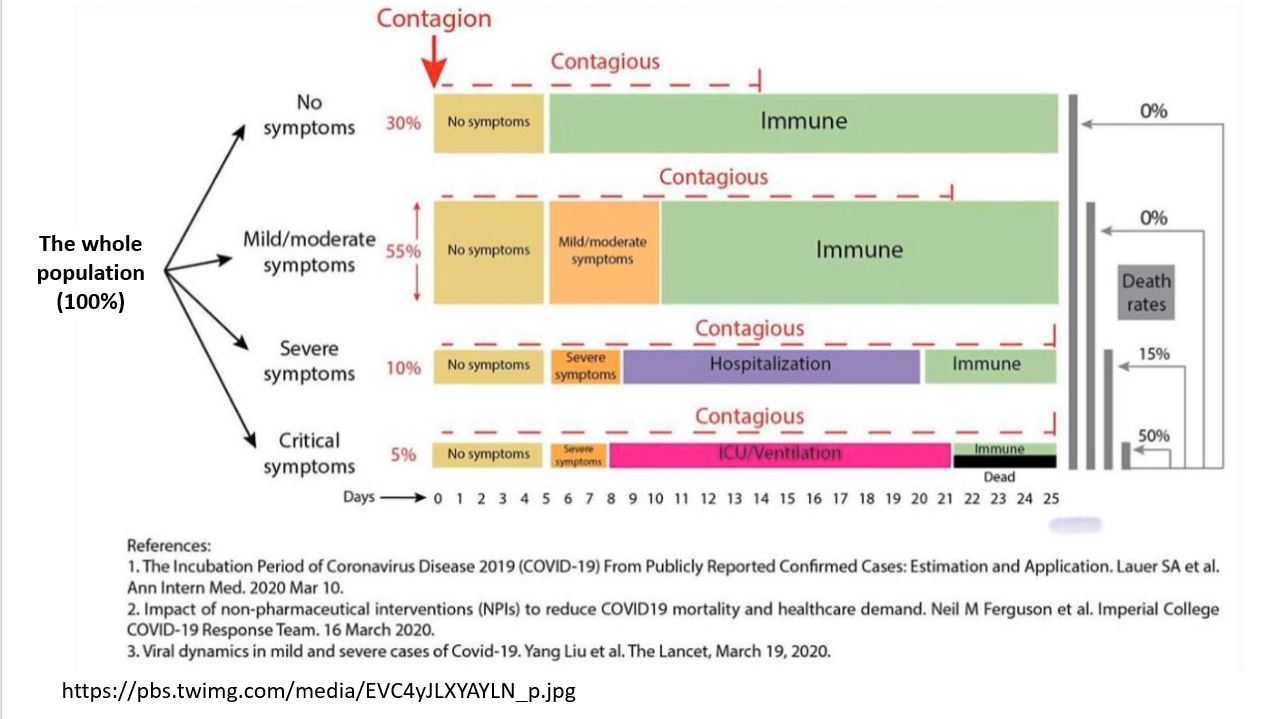
COVID-19 can sometimes overwhelm young and old immune systems and in some cases can result in ‘Severe Acute Respiratory Syndrome’ pneumonia and death (CDC, 2020). The risk is greater for older people, and people with serious heart conditions (e.g., heart failure, coronary artery disease, or cardiomyopathies), cancers, obesity, Type 2 diabetes, COPD, chronic kidney disease, hypertension, smoking, immune suppression or other health issues (CDC, 2020a) as well as young people who vape or smoke and those with immunological defects in type I and II interferon production (Gaiha, Cheng, & Halpern-Felsher, 2020; van der Made, 2020). As we age the immune system deteriorates (immunosenescence) that reduces the response of the adaptive immune system that needs to respond to the virus infection (Aw, Silva & Palmer, 2007; Osttan, Monti, Gueresi, et al., 2016). On the other hand, for young people and children the risk is very low and similar for Covid-19 as for seasonal influenza A and B in rates for hospitalization, admission to the intensive care unit, and mechanical ventilator ( Song et al, 2020).
Severity of disease may depend upon initial dose of the virus
In a brilliant article, How does the coronavirus behave inside a patient? We’ve counted the viral spread across peoples; now we need to count it within people, assistant professor of medicine at Columbia University and cancer physician Siddhartha Mukherjee points out that severity of the disease may be related to the initial dose of the virus. Namely, if you receive a very small dose (not too many virus particles), they will infect you; however, the body can activate its immune response to cope with the infection. The low dose exposure act similar to vaccination. If on the other hand you are exposed to a very high dose then your body is overwhelmed with the infection and is unable to respond effectively. Think of a forest fire. A small fire can easily be suppressed since there is enough time to upgrade the fire-fighting resources; however, during a fire-storm with multiple fires occurring at the same time, the fire-fighting resources are overwhelmed and there is not enough time to recruit outside fire-fighting resources.
As Mukherjee points out this dose exposure relationship with illness severity has a long history. For example, before vaccinations for childhood illnesses were available, a child who became infected at the playground usually experienced a mild form of the disease. However, the child’s siblings who were infected at home develop a much more severe form of the disease.
The child infected in the playground most likely received a relatively small dose of the virus over a short time period (viral concentration in the air is low). On the other hand, the siblings who were infected at home by their infected brother or sister received a high concentration of the virus over an extended period which initially overwhelmed their immune system. Higher virus concentration is more likely during the winter and in well insulated/sealed houses where the air is recirculated without going through HEPA or UV filters to sterilize the air. When there is no fresh air to decrease or remove the virus concentration, the risk of severity of illness may be higher (Heid, 2020).
The risk of becoming sick with COVID-19 can only occur if you are exposed to the coronavirus and the competency of your immune system. This can be expressed in the following equation. This equation suggests two strategies to reduce risk: reduce coronavirus load/exposure and strengthen the immune system.
This equation suggests two strategies to reduce risk: reduce coronavirus load/exposure and strengthen the immune system.
How to reduce the coronavirus load/dose of virus exposure
Assume that everyone is contagious even though they may appear healthy. Research suggests that people are already contagious before developing symptoms or are asymptomatic carriers who do not get sick and thereby unknowingly spread the virus (Furukawa, Brooks, Sobel, 2020). Dutch researchers have reported that, “The proportion of pre-symptomatic transmission was 48% for Singapore and 62% for Tianjin, China (Ganyani et al, 2020). Thus, the intervention to isolate people who have symptoms of COVID-19 (fever, dry cough, etc.) most likely will miss the asymptomatic carriers who may infect the community without awareness. Only if you have been tested, do you know if you been exposed or recovered from the virus. To reduce exposure to the virus, avoid the “Three C’s” — closed spaces with poor ventilation, crowded places and close contact—and do the following:
- Follow the public health guidelines:
-
- Social distance (physical distancing while continuing to offer social support)
- Wear a mask and gloves to reduce spreading the virus to others.
- Wash your hands with soap for at least 20 seconds.
- Avoid touching your face to prevent microorganisms and viruses to enter the body through mucosal surfaces of the nose mouth and eyes.
- Clean surfaces which could have been touched by other such as door bell, door knobs, packages.
- Avoid the person’s slipstream that may contain the droplets in the exhaled air. The purpose of social distancing is to have enough distance between you and another person so that the exhaled air of the other person would not reach you. The distance between people depends upon their activities and the direction of airflow.
In a simulation study, Professor Bert Blocken and his colleagues at KU Leuven and Eindhoven University of Technology reported that the plume of the exhaled air that potentially could contain the virus droplets could extend much more than 5 feet. It would depends upon the direction of the wind and whether the person is walking or jogging as show in Figure 1 (Blocken, 2020).

Figure 1. The plume of exhaled droplets that could contain the virus extends behind the person in their slipstream (photo from KU Leuven en TU Eindhoven).
The plume of exhaled droplets in the person’s slipstream may extend more than 15 feet while walking and more than 60 feet while jogging or bicycling. Thus. social distancing under these conditions is much more than 6 feet and it means avoiding their slipstream and staying much further away from the person.
- Increase fresh air to reduce virus concentration. The CDC recommends ventilation with 6 to 12 room air changes per hour for effective air disinfection (Nardell & Nathavitharana, 2020). By increasing the fresh outside air circulation, you dilute the virus concentration that may be shed by an infected asymptomatic or sick person (Qian & Zheng, 2018). Thus, if you are exposed to the virus, you may receive a lower dose and increase the probability that you experience a milder version of the disease. Almost all people who contract COVID-19 are exposed indoors to the virus. In the contact tracing study of 1245 confirmed cases in China, only a single outbreak of two people occurred in an outdoor environment (Qian et al, 2020). To increase fresh air (this assumes that outside air is not polluted), explore the following:
-
- Open the windows to allow cross ventilation through your house or work setting. One of the major reasons that the flu season spikes in the winter is that people congregate indoors to escape weather extremes. People keep their windows closed to conserve heat and reduce heating bill costs. Lack of fresh air circulation increases the viral density and risk of illness severity (Foster, 2014). See the superb graphic illustration by Bartzokas et al (Feb 26, 2021).in the New York Times of virus concentration in schools when the windows are opened. https://www.nytimes.com/interactive/2021/02/26/science/reopen-schools-safety-ventilation.html?smid=em-share
- Use an exhaust fans to ventilate a building. By continuously replacing the inside “stale” air with fresh outside air, the concentration of the virus in the air is reduced.
- Use High-efficiency particulate air (HEPA) air purifiers to filter the air within a room. These devices will filter out particles whose diameter is equal to 0.3 µ m. They will not totally filter out the virus; however, they will reduce it.
- Avoid buildings with recycled air unless the heating and air conditioning system (HAC) uses HEPA filters.
- Wear masks to protect other people and your community. The mask will reduce the shedding of the virus to others by people with COVID-19 or those who are asymptomatic carriers. This is superbly illustrated by Prather, Wang, & Schooley (2020) that not masking maximizes exposure, whereas universal masking results in the least exposure.

- Avoid long-term exposure to air pollution. People exposed to high levels of air pollution and fine particulate matter (PM2.5) are more at risk to develop chronic respiratory conditions and COVID-19 death rates. In the 2003 study of SARS, ecologic analysis conducted among 5 regions in China with 100 or more SARS cases showed that case fatality rate increased with the increment of air pollution index (Cui, Zhang, Froines, et al. , 2003). The higher the concentration of fine particulate matter (PM2.5), the higher the death rate (Conticini, Frediani, & Caro, 2020). As researchers, Xiao Wu, Rachel C. Nethery and colleagues (2020) from the Harvard T.H. Chan School of Public Health point out, “A small increase in long-term exposure to PM2.5 leads to a large increase in COVID-19 death rate, with the magnitude of increase 20 times that observed for PM2.5 and all cause mortality. The study results underscore the importance of continuing to enforce existing air pollution regulations to protect human health both during and after the COVID-19 crisis.“
- Breathe only through your nose. The nose filters, warms, moisturizes and slows the airflow so that airway irritation is reduced. Nasal breathing increases nitric oxide production that significantly increases oxygen absorption in the body. During inspiration through the nose the nitric oxide helps dilate the airways in your lungs and blood vessels (McKeown, 2016). More importantly for dealing with COVID-19, Nitric Oxide, produced and released inside the nasal cavities and the lining of the blood vessels, acts as an antiviral and a secondary strategy to protect against viral infections (Mehta, Ashkar & Mossman, 2012).
How to strengthen your immune system to fight the virus
The immune system is dynamic and many factors as well as individual differences affect its ability to fight the virus. It is possible that a 40 year-old person may have an immune systems that functions as a 70 year old, while some 70 year-olds have an immune system that function as a 40 year-old. Factors that contribute to immune competence include genetics, aging, previous virus exposure, and lifestyle (Lawton, 2020).
It is estimated that 70-80% mortality caused by Covid-19 occurred in people with comorbidity who are: over 65, male, lower socioeconomic status (SES), non white, overweight/obesity, cardiovascular heart disease, and immunocompromised. Although children comprised only a small percentage of the seriously ill patients, 83% of those children in the intensive care units had comorbidities and 60% were obese. The majority of contributing factors to comorbidities and obesity are the result of economic inequality and life style patterns such as the Western inflammatory diet (Shekerdemian et al, 2020; Zachariah, 2020; Pollan, 2020).
By taking charge of your lifestyle habits through an integrated approach, you may be able to strengthen your immune system (Alschuler et al, 2020; Lawton, 2020). The following tables, adapted from the published articles by Lawton (2020), Alschuler et al, (2020) and Jaffe (2020), list factors that support or decrease the immune system.
Factors that decrease immune competence

Factors that support immune competence
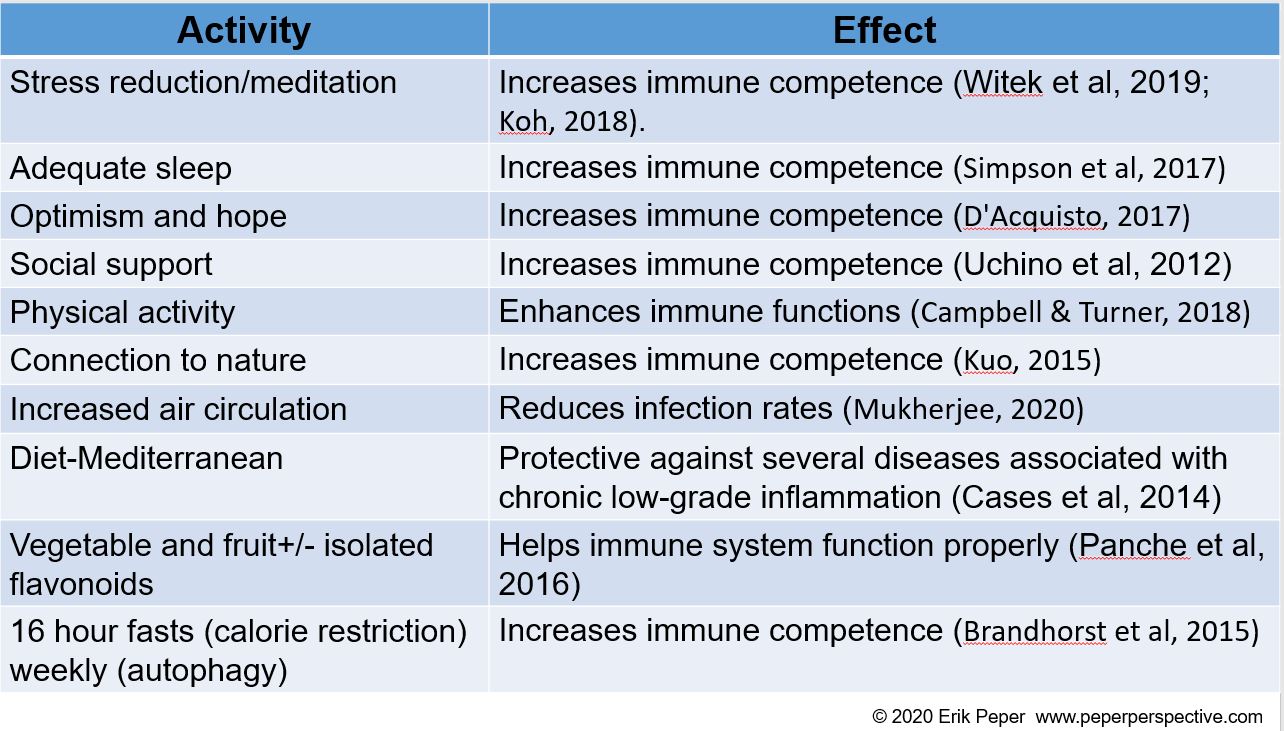
Phytochemicals and vitamins that support immune competence

REFERENCES
Abhanon, T. (2020 March 26). Practical tips how to keep yourself safe.
Foster, H. (2014 December 1). The reason for the season: why flu strikes in winter. SITN Science in the News.
Furukawa, N.W., Brooks, J.T., & Sobel, J. (2020, July). Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. [June3, 2020]. https://doi.org/10.3201/eid2607.201595
Ganyani, T., Kremer, C., Chen, D., Torneri, A, Faes, C., Wallinga, J., & Hensm N. (2020). Estimating the generation interval for COVID-19 based on symptom onset data doi:https://doi.org/10.1101/2020.03.05.20031815
Gaiha, S.M., Cheng, J. & Halpern-Felsher, B. (2020). Association between youth smoking, electronic cigarette use, and coronavirus disease 2019. Journal of Adolescent Health. Published online August 11, 2020. doi: https://doi.org/10.1016/j.jadohealth.2020.07.002
Heid, M. (2020-04-09). The Germ-Cleaning Power of an Open Window. Elemental by Medium.
BMJ Open, 11:e047474. http://dx.doi.org/10.1136/bmjopen-2020-047474
Jaffe, R. (2020). Reduce risk, boost immunity defense and repair abilities, and stay resilient. PERQUE Integrative Health.
Lawton, G. (2020). You’re only as young as your immune system. New Scientist, 245(3275), 44-48.
Lee, G. Y., & Han, S. N. (2018). The Role of Vitamin E in Immunity. Nutrients, 10(11), 1614.
Malaguarnera L. (2019). Influence of Resveratrol on the Immune Response. Nutrients, 11(5), 946.
Mukherjee, S. (2020). How does the coronavirus behave inside a patient? We’ve counted the viral spread across peoples; now we need to count it within people. The New Yorker, April 6, 2020.
Reduce TechStress at Home
Posted: March 19, 2020 Filed under: behavior, computer, digital devices, ergonomics, health, laptops, Neck and shoulder discomfort, Pain/discomfort, Uncategorized 8 CommentsAdapted from the book, Peper, E., Harvey, R., & Faass, (2020). Tech Stress: How Technology Is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.

Numerous people report that working at the computer at home is more tiring than working in the office. Although there are obvious advantages to working at home, there are also disadvantages (e.g., no space to work, challenging ergonomics, no escape from the family, lack of nonverbal cues used to communicate, less informal sharing at the water cooler, increased multitasking by working and having to take care of the children).
A major challenge is having a comfortable work space in your home. This may mean finding a place to put the computer, keyboard and screen. For some it is the kitchen table, desk in the corner of the bedroom, or coffee table while other it is in a totally separate room.
Incorrect ergonomic arrangement and stressed work style often increases neck, shoulder discomfort and aggravates eye strain and tiredness. Regardless how your digital work space is organized, implement the following life and work style suggestions and ergonomics recommendations to promote health.
LIFE AND WORK STYLE SUGGESTIONS
Take many, many, many breaks. Movement breaks will reduce the covert static tension that builds up as we sit in static positions and work at the computer.
- Every few minutes take a small break such as stand up and wiggle or role your shoulders. When performing the movements, stop looking at the screen and look around the room or out the window.
- Every 30 minutes get up walk around for and move your body. Use timers to notify you every 30 minutes to take a break (e.g., cellphone alarms or personal digital assistants such as Hey Google, Siri, or Alexa).
Improve vision.
- Take vision breaks to reduce eye fatigue.
- Every few minutes look away from the screen and into the far distance and blink. If at all possible look outside at green plants which relaxes the near vision induced tension.
- Blink and blink again. When working at the computer we reduce our blinking rate. Thus, blink each time you click on a new link, finishing entering a column of numbers, etc.
- Close your eyes by letting the eye lids drop down as you also relax your jaw. Imagine a hook on top of your head which is pulling your head upward and at the same time drop your shoulders.
- Reduce glare and bright backgrounds
- Arrange your computer screen at 90 degrees to the brightest light source.
- Have a darker background behind you when participating in video conferencing (e.g., Zoom, Skype, GoToMeeting, WhatsApp, FaceTime). Your face will be visible.
Regenerate
- When stressed remember to breathe. As you inhale let your stomach expand as you exhale let the air flow out slowly.
- Stop watching and listening to the negative news (check the news no more than once a day). Watch positive and humorous movies.
- Get fresh air, go for a walk, and be in the sun
- Reconnect with friends and share positive experiences.
- Remind yourself, that this too shall pass.
ERGONOMIC RECOMMENDATIONS: MAKE THE WORLD YOURS
Good ergonomics means adapting the equipment and environment to you and not the other way around. Optimizes the arrangement of the chair, desk, keyboard, mouse, camera, screen and yourself as shown in Figure 1.
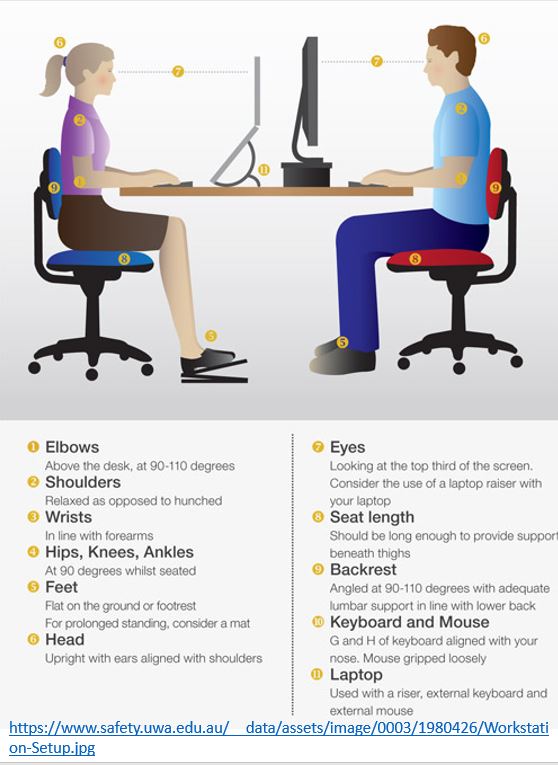
Figure 1. Recommended arrangement for working at the computer.
Arrange the laptop
The laptop is challenging because if your hands are at the right height for data entry on the keyboard, then you must look down to see the screen. If the screen at the right height, then you have to raise your hands to reach the keyboard. There are two solutions for this challenge.
- Use an external keyboard and mouse, then raise the laptop so that the top of the screen is at eye level. Use a laptop stand or a stack of books to raise the lap top.
- Use an external monitor for display, then use the laptop as your keyboard.
If these solutions are not possible, take many, many, many breaks to reduce the neck and shoulder stress.
Arrange the computer workstation
- Adjust the chair so that your forearms can rest on the table without raising your shoulders. This may mean sitting on a pillow. If the chair is then too high and your legs dangle, create a foot stool on which you can rest your feet.
- Adjust the monitor so that the top of the screen is at eye level. If the monitor is too low, raise it by putting some books underneath it.
- If possible, alternate standing and sitting while working.
RESOURCES
Book
Tech Stress: How Technology Is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics provides insight in how discomfort, symptoms and media addiction develops and what you can do about it. It incorporates the role of evolutionary traps, how biofeedback makes the unaware aware, experiential physical and cognitive practices, and ergonomic recommendations to optimize health and productivity. A must book for anyone using digital devices. Peper, E., Harvey, R., & Faass, (2020). Tech Stress: How Technology Is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
Ergonomic suggestions for working at the computer and laptop.
https://peperperspective.com/2014/09/30/cartoon-ergonomics-for-working-at-the-computer-and-laptop/
11 tips for working at home
How our digital world activates evolutionary response patterns.
https://peperperspective.com/2018/02/10/digital-addiction/
How posture affects health
https://peperperspective.com/2019/07/01/dont-slouch-improves-health-with-posture-feedback/
https://peperperspective.com/2019/05/21/relieve-and-prevent-neck-stiffness-and-pain/
https://peperperspective.com/2019/01/23/head-position-it-matters/
Coronavirus risk in context: How worried should you be?
Posted: March 7, 2020 Filed under: behavior, health, Uncategorized | Tags: coronavirus, COVID-19 9 CommentsThe coronavirus which causes coronavirus disease 2019 (COVID-19) appears to be a highly contagious disease. Some older people and those who are immune compromised are more at risk. The highest risk are for older people who already have cardiovascular, diabetes, respiratory disease, and hypertension. In addition, older men over 65 years are much more at risk; however, many are smokers who have a compromised pulmonary system. Previous meta analysis showed that smoking was consistently associated with higher risk of hospital admissions after influenza infection. Nevertheless, it is reasonable to assume that over time all most all of us will become exposed to the virus, a few will get very sick, and even fewer will die.
The preliminary data suggests that most people who become infected may not even know they are infectious. Make the assumption that everyone could be contagious unless tested for the virus or antibodies to the virus since people appear to be infectious for the first four days before experiencing symptoms.
The absolute risk that one would die of this disease is low although if you do become very sick it is more dangerous than the normal flu; however, the fear of this disease may be out of proportion compared to other health risks. For detailed analysis and graphic summaries see the updated research reports on the Coronavirus disease (COVID-19) by Our World in Data and Information is beautiful. These reports make data and research on the world’s largest problems understandable and accessible.
It is worthwhile to look at the absolute risk of COVID-19. To read that more than 332,000 people world wide have died in the last five months is terrifying especially with the increasing death rate in Europe and New York; however, it needs to be understood in context of the size of the population. The epicenter of this disease was Wuhan and Hubei Provence, China with a total population of about 60 million people. Each year about 427,200 people die in the Wuhan and Hubei Province (the annual death rate in China is 7.12 deaths per 1000 people). Without this new viral disease, about 71,200 people would have died during the same two month period. The question that has not been discussed is how much did the total death rate increase. Would it be possible that some of the people who died would have died of other natural causes such as the flu?
The World Health Organization (WHO) and governments around the world should be lauded for their attempt to reduce the spread of the virus. On March 6, 2020, the United States Congress allocated $8. billion dollars to fight and prevent the spread of COVID-19.
This funding will only partially prevent the spread of the virus because some people have no choice but to go to work when they are sick–they do not receive paid sick leave! This is true for about 30 percent of the American workers who have no coverage at work or the millions of self-employed workers (e.g. gig/freelance workers, waiters, cashiers, drivers, nannies, house cleaners).
To reduce the risk of the spreading COVID-19, anyone who feels sick or thinks they have been exposed, should receive paid sick leave so that they can stay home and self-isolate. The paid sick leave should be Federally funded and provide basic income for those whose income would be lost if they did not work. Although it is possible that a few people will cheat and take the paid sick leave when they are well, this is worth the risk to keep the rest of population healthy. To provide possible relief, at the moment the House and Senate are working on a greater than $2 trillion dollar stimulus package.
Personal and government responses to health risks are not always rational.
Funding for health and illness prevention is driven by politics. For example, gun violence results in more than 100,000 people being injured each year and more than 36,000 killed—an average of 100 per day. Gun violence is a much more virulent disease than COVID-19 and more than 1.7 million Americans have died from firearms since 1968.
The Federal Government response to this gun violence epidemic has been minimal. For the first time since 1996 did the 2020 federal budget include $25 million funding for the CDC and NIH to research reducing gun-related deaths and injuries.
It is clear that the government response does not always focuses its resources on what would reduce injury and death rates the most. Look at the difference in the national response to COVID-19 virus that has killed more than 120,000 people in the USA ($8.5 billion for the initial response and then $2 trillion stimulus package) as compared gun violence that kills 36,000 people a year in the USA ($25 million funding to study the causes of gun violence).
Be realistic about the actual risk of COVID-19 without succumbing to fear.
COVID-19 is a pandemic and I expect that 30% to 70% of us will be infected this year. Hopefully, in the next 18 months an effective vaccine will be developed. In the mean time, there is no known treatment, thus optimize health and reduce the exposure to the coronavirus.
- How to reduce exposure to the coronavirus
- Optimize your health and immune function by eating healthy, getting enough sleep, enjoying some exercise/movement and reducing stress.
- Increase social distance when with other people–greet people by staying separated by at least six feet or more from each other instead of a handshake or a kiss on the cheek.
- Wash your hands after touching surfaces that others may have touched or after going out for shopping, work, pleasure and/or meeting other people.
- Avoid touching your face especially your mouth, nose and eyes.
- Sanitize hard surfaces. Malia Jones, PhD, MPH points out that you can make your own inexpensive antimicrobial spray by mixing 1 part household bleach to 99 parts cold tap water. Spray this on surfaces and leave for 10-30 minutes. (Note: this is bleach. It will ruin your sofa).
- If you think you have the disease or have symptoms, contact your healthcare provider. Wear a mask and self-isolate to reduce spreading the virus to others.
- Increase fresh air circulation and avoid room that have poor ventilation.
- Reliable information about COVID-19
- World Health Organization (WHO): https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- Centers for Disease Control (CDC): https://www.cdc.gov/coronavirus/2019-ncov/about/index.html
- Graphic representation of the background of the COVID-19 infection and relationship to other diseases
- Summary of what is the corona virus: https://ourworldindata.org/coronavirus#citation
- Graphic representation of coronavirus in context to other diseases: https://informationisbeautiful.net/visualizations/covid-19-coronavirus-infographic-datapack/
- Accurate information on number of infections, new cases and deaths: https://www.worldometers.info/coronavirus/
To make sense of the danger of COVID-19, look at it in context to the flu. The risk is the greatest for people with co-morbidity (obesity, diabetes, emphysema, immune suppressed illnesses, and people who smoke and vape). While the risk for young people and children is no different for being infected with Covid-19 or influensa A and B in hospitalization rates, intensive care unit admission rates, and mechanical ventilator (Song et al. 2020). Depending upon the severity the flu, 9,000,000 to 45,000,000 people get sick from flu and between 12,000 to 61,000 die from its complications as shown below in Figure 1.
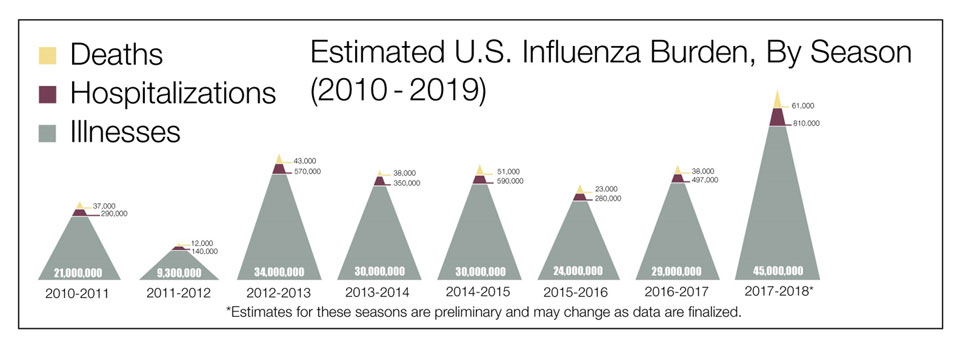 Figure 1. The estimated U.S. influenza burden by year (from: https://www.cdc.gov/flu/about/burden/index.html)
Figure 1. The estimated U.S. influenza burden by year (from: https://www.cdc.gov/flu/about/burden/index.html)


