Hope for teens with pain
Posted: August 31, 2019 Filed under: behavior, health, Pain/discomfort, relaxation, self-healing, stress management, Uncategorized | Tags: adolescents, teenagers 3 CommentsErik Peper, PhD and Rachel Zoffness, PhD*
KM was 14 years old when he came to my (Zoffness) office for treatment. He’d been diagnosed with migraine and cyclical vomiting syndrome and had been in bed for about 3 years. He had long, unwashed hair; was a sickly, pasty white; and rocked himself back and forth from the pain. He’d seen 15 doctors and had been prescribed 30 medications, including occipital nerve injections and Thorazine. Nothing had worked. Like most teens with chronic pain, KM was depressed, stressed, and terrified he’d never get his life back.
We started Cognitive Behavioral Therapy (CBT), beginning with pain neuroscience education. This involved teaching KM and his family how pain works in the brain, and how thoughts, emotions, physical sensations and behaviors work together to trigger and maintain flares. He then learned a variety of cognitive, behavioral and mind-body techniques to help manage and change pain. His parents received parent-training to support him behind the scenes. After a few weeks of treatment, KM was able to get out of bed and walk to the corner mailbox. After a few more weeks, he was able to walk his dog to the dog park and get a haircut. Within a few months he was jogging around the block, then running. As his functioning increased, his brain desensitized and his body strengthened, his pain started to recede. Gradually he returned to school and social relationships, eventually rejoining his soccer team. I attended his high school graduation a year ago. He got onstage and told the audience that, if you’d told him 4 years ago that he’d graduate high school, he’d never have believed you. He is currently in college, successfully managing his pain, living his important life.
Chronic pain (CP) in teens can be devastating. Teens are already tasked with managing the turbulence of hormone changes, social stress, academic stress, social media, family dynamics, and developing autonomy and independence. CP impacts not only the teen, but also the entire family. Because CP is framed as a biomedical problem, it is frequently treated with opioids and other minimally-helpful (and sometimes harmful) medications. Opioids are ineffective for long-term treatment of chronic pain, and are only useful in acute crises or to control pain at the end of life (Dowell, 2016; King et al, 2011).
Although we typically think of chronic pain as an issue primarily affecting adults coping with issues such as post-surgical pain and arthritis, CP affects up to 1 in 3 youth in the USA – more than 10 million children and teens (Friedrichsdorf, 2016; ). Pain impacts self-esteem, hope, and functioning, relegating teens to their beds and denying them normal educations and healthy social interactions. Like adults, teens often feel powerless and blamed. In a superb workbook, The Chronic Pain & Illness Workbook for Teens, psychologist Rachel Zoffness describes what pain is; how pain is constructed by the brain; how mind, body and emotions interact to affect pain; and offers a sequence of assessments and practices to reduce pain and improve health in language children and teens can easily understand. The approach combines cognitive behavioral therapy (CBT) with imagery, mindfulness, breathing, handwarming with biofeedback, and somatic practices (Turk & Gatchel, 2018; Peper, Gibney, & Holt, 2002).
This simple graphic of the pain cycle is helpful to clients (see Fig. 1).

Fig 1. CBT Pain Cycle
The pragmatic practices in this book offer tools and guided instructions that any child or teen can use for themselves, with parents, or with health providers. Therapists can use and adapt these activities with their clients of all ages. Although these scientifically-supported pain management techniques are written for teens, they can equally be used with adults. Below are two of many different practices described in the book that are useful for chronic pain.
Practice 1: Assessment: What sets off your pain?
The first step is to help youth identify factors that “trigger” – or set off – their pain. It’s helpful to define a trigger as a difficult emotion, situation, or event that causes pain to increase. Difficult situations and events of all kinds – biological, social, etc (situational triggers) can trigger difficult thoughts and emotions (cognitive and emotional triggers), and vice versa. For example, Adam was recovering from back surgery (situational trigger), got into a big fight with his sister about the car (situational trigger), and became angry and frustrated (emotional trigger). He felt the anger in his body, his muscles got hot and tight, and his back started spasming. Gina is an example of the reverse. She believed that nothing could cure her fibromyalgia (cognitive trigger), which made her feel depressed and hopeless (emotional trigger). She stayed home for weeks on end without school, friends, or distractions (situational trigger), and started feeling worse.
We can help youth with pain by asking:
- What emotions trigger your pain?
- Frustration
- Anger
- Stress
- Anxiety
- Loneliness
- Sadness
- What situations trigger your pain?
- Not getting enough sleep
- Arguing with family members
- Inflammation after physical therapy
- Missing fun events because you’re sick
- Thinking about upcoming exams
- Doctor’s appointments and hospital visits
Sometimes, the teen needs to keep a log for a week to identify the situations or triggers related to the pain. Once these have been identified then the teen can explore strategies to reduce the negative reactivity triggered by the emotions or situations.
Practice 2: Changing the voice of pain (Note: this is a summary of a longer activity)
One technique we use in CBT for chronic pain is identifying and tracking cognitive distortions, also known as “thinking traps.” I (Zoffness) call these traps “Pain Voice.” This is the catastrophic, pessimistic, critical, and negative voice that tells us awful, worrisome things, particularly about our pain or health.
For example:
Pain Voice pretends she can predict the future, and says it’s going to be terrible. She says: “You’ll never get better. Nothing will ever help you.” But since she can’t predict the future (who can?), Pain Voice is a liar! Pain Voice is also very bossy about what you can and can’t do: “You can’t see your friends this week,” or “You can’t go for a bike ride, and you definitely can’t have any fun.” Science teaches us that negative thoughts increase pain by turning up the brain’s “pain dial,” so we must make sure not to listen to or believe them. To stop Pain Voice, we first catch negative thoughts.
As soon as you learn how to recognize Pain Voice, you gain the power to change negative thoughts into more helpful “Wise Voice” thoughts. One way to bust Pain Voice is to start tracking your negative thoughts. First, list these critical, self-defeating, catastrophic Pain Voice thoughts. Notice if they’re helpful or harmful. Then check and question them, thoughtfully determining whether they’re the truth or a trap. Next, gather evidence as to why Pain Voice might be wrong by asking yourself, is this thought a fact? What evidence do I have that this thought might not be true? What else might happen other than what I’m predicting? Write out your Wise Voice responses, and use them to fight back every time you hear Pain Voice!
Jason’s example: Jason had terrible, daily back pain and hadn’t gone outside in 6 weeks. His friends texted, inviting him to watch a movie. Immediately he heard the thought, “I can’t go, I’m broken. If I leave my house my pain will spike and I won’t be able to function.” He recognized this as his Pain Voice and knew he had to fight back. He sat down with his worksheet and filled in the answers: yes, the thoughts were harmful, not helpful, and they were trying to trap him! He examined the evidence and wrote the Wise Voice thought, “This negative prediction is not a fact, it’s a trap. I’ve had back pain for 2 years, and sometimes going out and seeing friends actually reduces my pain.” Tuning into his Wise Voice gave him the strength to get the social support and distraction he needed to feel a little better! He went to his friend’s house, watched movies, ate popcorn, giggled, and had a great time. For the first time in 6 weeks, his pain went down. An example of his log is shown in table 1.
|
Situation |
Pain Voice |
Helpful or Harmful? |
Trap or Truth |
Wise Voice |
| Returning to school after missing 3 weeks | If I go back to school, I’ll be so far behind that I won’t understand anything the teacher is talking about. | Harmful | Trap | This negative prediction is not a fact. I’m smart and competent, I’ll probably understand some things. Last time I was behind, I made up the work and everything was fine. |
|
Pain flare-up
|
I can’t handle this! | Harmful | Trap | This negative prediction is not a fact. I’ve had 42 pain flare-ups this year, and I handled all of them. I’ve proven that I’m strong and resilient. There is a 0% chance I can’t handle this. |
Table 1. Example from Jason’s log
Summary: There is hope for youth with chronic pain. Interventions like CBT, mindfulness, biofeedback and other mind-body approaches are scientifically-supported and have evidence of effectiveness. Adhering to the biopsychosocial model – targeting biological, psychological and social factors – is proven to be the most effective treatment for chronic pain across conditions and ages. For more information, see Rachel Zoffness’ book, The chronic pain & illness workbook for teens, for pragmatic treatment practices and user-friendly pain education.

References
*Dr. Rachel Zoffness is a pain psychologist, consultant, writer and educator in Northern California’s East Bay specializing in chronic pain and illness.
Do self-healing first
Posted: May 27, 2019 Filed under: behavior, Breathing/respiration, emotions, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, Nutrition/diet, Pain/discomfort, placebo, relaxation, self-healing, stress management, surgery, Uncategorized 2 Comments
“I am doing very well, and I am very healthy. The vulvodynia symptoms have never come back. Also,my stomach (gastrointestinal discomfort) has gotten much, much better. I don’t really have random pain anymore, now I just have to be watchful and careful of my diet and my exercise, which are all great things!” —A five-year follow-up report from a 28-year-old woman who had previously suffered from severe vulvodynia (pelvic floor pain).
Numerous clients and students have reported that implementing self-healing strategies–common sense suggestions often known as “grandmother’s therapy”—significantly improves their health and find that their symptoms decreased or disappeared (Peper et al, 2014). These educational self-healing approaches are based upon a holistic perspective aimed to reduce physical, emotional and lifestyle patterns that interfere with healing and to increase those life patterns that support healing. This may mean learning diaphragmatic breathing, doing work that give you meaning and energy, alternating between excitation and regeneration, and living a life congruent with our evolutionary past.
If you experience discomfort/symptoms and worry about your health/well-being, do the following:
- See your health professional for diagnosis and treatment suggestions.
- Ask what are the benefits and risks of treatment.
- Ask what would happen if you if you first implemented self-healing strategies before beginning the recommended and sometimes invasive treatment?
- Investigate how you could be affecting your self-healing potential such as:
- Lack of sleep
- Too much sugar, processed foods, coffee, alcohol, etc.
- Lack of exercise
- Limited social support
- Ongoing anger, resentment, frustration, and worry
- Lack of hope and purpose
- Implement self-healing strategies and lifestyle changes to support your healing response. In many cases, you may experience positive changes within three weeks. Obviously, if you feel worse, stop and reassess. Keep a log and monitor what you do so that you can record changes.
This self-healing process has often been labeled or dismissed as the “placebo effect;” however, the placebo effect is the body’s natural self-healing response (Peper & Harvey, 2017). It is impressive that many people report feeling better when they take charge and become active participants in their own healing process. A process that empowers and supports hope and healing. When participants change their life patterns, they often feel better. Their health worries and concerns become reminders/cues to initiate positive action such as:
- Practicing self-healing techniques throughout the day (e.g., diaphragmatic breathing, self-healing imagery, meditation, and relaxation)
- Eating organic foods and eliminating processed foods
- Incorporating daily exercise and movement activities
- Accepting what is and resolving resentment, anger and fear
- Taking time to regenerate
- Resolving stress
- Focusing on what you like to do
- Be loving to yourself and others
For suggestions of what to do, explore some of the following blogs that describe self-healing practices that participants implemented to improve or eliminate their symptoms.
Acid reflux (GERD) https://peperperspective.com/2018/10/04/breathing-reduces-acid-reflux-and-dysmenorrhea-discomfort/
Dyspareunia https://peperperspective.com/2017/03/19/enjoy-sex-breathe-away-the-pain/
Epilepsy https://peperperspective.com/2013/03/10/epilepsy-new-old-treatment-without-drugs/
Irritability/hangry https://peperperspective.com/2017/10/06/are-you-out-of-control-and-reacting-in-anger-the-role-of-food-and-exercise/
Hot flashes and premenstrual symptoms https://peperperspective.com/2015/02/18/reduce-hot-flashes-and-premenstrual-symptoms-with-breathing/
Internet addiction https://peperperspective.com/2018/02/10/digital-addiction/
Irritable bowel syndrome (IBS) https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/
Math and test anxiety https://peperperspective.com/2018/07/03/do-better-in-math-dont-slouch-be-tall/
Neck stiffness https://peperperspective.com/2017/04/06/freeing-the-neck-and-shoulders/
Neck tension https://peperperspective.com/2019/05/21/relieve-and-prevent-neck-stiffness-and-pain/
Posture and mood https://peperperspective.com/2017/11/28/posture-and-mood-implications-and-applications-to-health-and-therapy/
Psoriasis https://peperperspective.com/2013/12/28/there-is-hope-interrupt-chained-behavior/
Surgery https://peperperspective.com/2018/03/18/surgery-hope-for-the-best-but-plan-for-the-worst/
Trichotillomania (hair pulling) https://peperperspective.com/2015/03/07/interrupt-chained-behaviors-overcome-smoking-eczema-and-hair-pulling/
Vulvodynia https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
References
Relieve and prevent neck stiffness and pain
Posted: May 21, 2019 Filed under: behavior, Exercise/movement, health, Neck and shoulder discomfort, Pain/discomfort, posture, Uncategorized | Tags: muscle tension, neck pain, neck stiffness, vision 6 CommentsIs your neck stiff, uncomfortable and painful?
When driving is it more difficult to turn your head?
Neck and shoulder pain affect more than 30% of people (Fejer et al, 2006; Cohen, 2015). This blog explores some strategies to reduce or prevent neck stiffness and discomfort and suggests practices to reduce discomfort and increase flexibility if you already are uncomfortable.
Shifts in posture may optimize neck flexibility
In our modern world, we frequently engage in a forward head position while looking at electronic devices or typing on computers. Prolonged smart phone usage has the potential to negatively impact posture and breathing functions (Jung et al., 2016) since we tilt our head down to look at the screen. Holding the head in a forward position, as displayed in Figure 1, can result in muscle tension in the spine, neck, and shoulders.
 Fig 1. Forward head and neck posture in comparison to a neutral spine. Source: https://losethebackpain.com/conditions/forward-head-posture/
Fig 1. Forward head and neck posture in comparison to a neutral spine. Source: https://losethebackpain.com/conditions/forward-head-posture/
Whenever you bring your head forward to look at the screen or tilt it down to look at your cellphone, your neck and shoulder muscles tighten and your breathing pattern become more shallowly. The more the head is forward, the more difficulty is it to rotate your head as is describe in the blog, Head position, it matters! (Harvey et al, 2018). Over time, the head forward position may lead to symptoms such as headaches and backpain. On the other hand, when we shift to an aligned upright position throughout the day, we create an opportunity to relieve this tension as shown in Figure 2.
 Figure 2. EMG and respiration recording from a subject sitting with a forward head position and a neutral, aligned head position. The neck and shoulder muscle tension was recorded from the right trapezius and left scalene muscles (Mason et all, unpublished). .
Figure 2. EMG and respiration recording from a subject sitting with a forward head position and a neutral, aligned head position. The neck and shoulder muscle tension was recorded from the right trapezius and left scalene muscles (Mason et all, unpublished). .
The muscle tension recorded from scalene and trapezius muscles (neck and shoulder) in Figure 2 shows that as the head goes forward or tilts down, the muscle tension significantly increases. In most cases participants are totally unware that their neck tightens. It is only after looking at the screen or focus our eyes until the whole day that we notice discomfort in the late afternoon.
Experience this covert muscle tension pattern in the following video, Sensing neck muscle tension-The eye, head, and neck connection.
Interrupt constant muscle tension
One possible reason why we develop the stiffness and discomfort is that we hold the muscles contracted for long time in static positions. If the muscle can relax frequently, it would significantly reduce the probability of developing discomfort. Experience this concept of interrupting tension practice by practicing the following:
- Sit on a chair and lift your right foot up one inch up from the floor. Keep holding it up? For some people, as soon as five seconds, they will experience tightening and the onset of discomfort and pain in the upper thigh and hip.
How long could you hold your foot slight up from the floor? Obviously, it depends on your motivation, but most people after one minute want to put the foot down as the discomfort become more intense. Put the foot down and relax. Notice the change is sensation and for some it takes a while for the discomfort to fade out.
- The reason for the discomfort is that the function of muscle is to move a joint and then relax. If tightening and relaxation occurs frequently, then there is no problem
- Repeat the same practice except lift the foot, relax and drop it down and repeat and repeat. Many people can easily do this for hours when walking.
What to do to prevent neck and shoulder stiffness.
Interrupt static muscle neck tension by moving your head neck and shoulder frequently while looking at the screen or performing tasks. Explore some of the following:
- Look away from the screen, take a breath and as you exhale, wiggle your head light heartedly as if there is a pencil at reaching from the top of your head to the ceiling and you are drawing random patterns on the ceiling. Keep breathing make the lines in all directions.
- Push the chair back from the desk, roll your right shoulder forward, up and back let it drop down and relax. Then roll you left shoulder forward up and back and drop down and relax. Again, be sure to keep breathing.
- Stand up and skip in place with your hands reaching to the ceiling so that when your right foot goes up you reach upward with your left hand toward the ceiling while looking at your left hand. Then, as your left foot goes up your reach upward to the ceiling with your right hand and look at your right hand. Smile as you are skipping in place.
- Install a break reminder program on your computer such as Stretch Break to remind you to stretch and move.
- Learn how to sit and stand aligned and how to use your body functionally such as with the Gokhale Method or the Alexander Technique (Gokhale, 2013; Peper et al, in press, Vineyard, 2007).
- Learn awareness and control neck and shoulder muscle tension with muscle biofeedback. For practitioners certified in biofeedback BCB, see https://certify.bcia.org/4dcgi/resctr/search.html
- Become aware of your collapsed and slouching wearing a posture feedback device such as UpRight Go on your upper back. This device provides vibratory feedback every time you slouch and reminds you to interrupt slouching and be upright and alighned.
Arrange your computer screen and keyboard so that the screen is at eye level instead of having to reach forward or look down. Similarly, hold your cell phone so that it is at eye level as shown in Figure 3 and 4.
 Figure 3. Slouching forward to see the laptop screen can be avoided by using an external keyboard, mouse and desktop riser. Reproduced by permission from www.backshop.nl
Figure 3. Slouching forward to see the laptop screen can be avoided by using an external keyboard, mouse and desktop riser. Reproduced by permission from www.backshop.nl

Figure 4. Avoid the collapsed while looking down at a cell phone by resting the arms on a backpack or purse and keeping the spine and head alighned. Photo of upright position reproduced with permission from Imogen Ragone, https://imogenragone.com/
Check vision
If you are squinting, bringing your nose to the screen, or if the letters are too small or blurry, have your eyes checked to see if you need computer glasses. Generally do not use bifocals or progressive glasses as they force you to tilt your head up or down to see the material at a specific focal length. Other options included changing the display size on screen by making the text and symbols larger may allow you see the screen without bending forward. Just as your muscle of your neck, your eyes need many vision breaks. Look away from the screen out of the window at a distant tree or for a moment close your eyes and breathe.
What to do if you have stiffness and discomfort
My neck was stiff and it hurt the moment I tried to look to the sides. I was totally surprised that I rapidly increased my flexibility and reduced the discomfort when I implemented the following two practices.
Begin by implementing the previous described preventative strategies. Most important is to interrupt static positions and do many small movement breaks. Get up and wiggle a lot. Look at the blog, Freeing the neck and shoulder, for additional practices.
Then, practice the following exercises numerous times during the day to release neck and shoulder tension and discomfort. While doing these practices exhale gently when you are stretching. If the discomfort increases, stop and see your health professional.
REFERENCES
Cohen, S.P. (2015). Epidemiology, Diagnosis, and Treatment of Neck Pain. Mayo Clinic Proceedings, 90 (2), 284-299. https://doi.org/10.1016/j.mayocp.2014.09.008
Fejer, R., Kyvik, K.Ohm, & Hartvigesen, J. (2006). The prevalence of neck pain in the world population: a systematic critical review of the literature. European Spine Journal, 15(6), 834-848. https://doi.org/10.1007/s00586-004-0864-4
Gokhale, E. (2013). 8 Steps to a Pain-Free Back. Pendo Press.
Harvey, R., Peper, E., Booiman, A., Heredia Cedillo, A., & Villagomez, E. (2018). The effect of head and neck position on head rotation, cervical muscle tension and symptoms. Biofeedback. 46(3), 65–71.
Mason, L., Peper, E., Harvey, R., & Hernandez, W. (unpublished). Healing headaches. Does success sustain over time?
Peper, E., Krüger, B., Gokhale, E., & Harvey, R. (in press). Comparing Muscle Activity and Spine Shape in Various Sitting Styles. Biofeedback.
Vineyar, M. (2007). How You Stand, How You Move, How You Live: Learning the Alexander Technique to Explore Your Mind-Body Connection and Achieve Self-Mastery. Boston: Da Capo Lifelong Books.
Optimize success: Enrich treatment with placebo-the body’s own natural healing response*
Posted: May 2, 2019 Filed under: behavior, health, Pain/discomfort, placebo, surgery, Uncategorized 2 CommentsWhen randomized controlled studies of pharmaceuticals or surgery find that the treatment is no more effective than the placebo, the authors conclude that surgery or drugs have no therapeutic value (Moseley et al, 2002; Jonas et al, 2015). Even though the patients may have gotten better, the researchers often do not explore questions such as, why did some of the patients improve just with the placebo treatment; what are the components of the placebo process; and, how can clinicians integrate placebo components into their practice to enhance the body’s own natural healing response.
To explore these topics further, listen to Shankar Vedantam’s outstanding podcast, A Dramatic Cure, from the NPR program, Hidden Brain-A conversation about life’s unseen patterns. Also, read the background materials on the website https://www.npr.org/2019/04/29/718227789/all-the-worlds-a-stage-including-the-doctor-s-office
 Placebo effects can be a powerful healing strategy as demonstrated by numerous research studies that have persuasively explored the central features of the placebo effect. The research has found that the more dramatic and impressive the procedure, the more powerful the placebo effect. For example, branded medicine with brightly colored packaging is more effective than generic medicine in plain boxes, an injection of a saline or sugar solution is more effective than taking a sugar pill, and placebo surgery is more effective than simply receiving an injection (Branthwaite & Cooper, 1981; Colloca & Benedetti, 2005). For a detailed exploration of placebo, nocebo and the important role of active placebo, see the blog, How effective is treatment? The importance of active placebos.
Placebo effects can be a powerful healing strategy as demonstrated by numerous research studies that have persuasively explored the central features of the placebo effect. The research has found that the more dramatic and impressive the procedure, the more powerful the placebo effect. For example, branded medicine with brightly colored packaging is more effective than generic medicine in plain boxes, an injection of a saline or sugar solution is more effective than taking a sugar pill, and placebo surgery is more effective than simply receiving an injection (Branthwaite & Cooper, 1981; Colloca & Benedetti, 2005). For a detailed exploration of placebo, nocebo and the important role of active placebo, see the blog, How effective is treatment? The importance of active placebos.
To see the effect of the placebo in action, watch the well-known British stage hypnotist and illusionist, Derren Brown’s video, Fear and Faith (https://www.youtube.com/watch?v=hfDlfhHVvTY). He magically weaves together a narrative that addresses the powerful influences of the natural, physical, and clinical environment and language used during a ‘therapeutic’ interaction. He shows how the influences of role modeling, the words that increase hope, trust and social compliance, and other covert factors promote healing. It uses the cover of a drug trial to convince various members of the public to overcome their fears using a placebo medicine called “Rumyodin” (which is a made-up name of a fake pharmaceutical) and demonstrates that the limits of experience are the limits of your belief.
This blog post serves as a reminder to ask ourselves as educators and therapists, ‘what can I do to include placebo enhancing components into my practice so that my clinical and educational outcomes are more effective?’ Explore ways to optimize your clinical environment, language use during ‘therapeutic’ interactions, and role modeling to increase hope, trust and social compliance and thereby optimize your clients’ own natural healing response.
Watch the video: Fear and Faith
References:
*I thank Richard Harvey, PhD., for his constructive feedback and James Fadiman, PhD., for reminding me to reframe the term placebo into “the body’s natural healing response.”
Anxiety, lightheadedness, palpitations, prodromal migraine symptoms? Breathing to the rescue!
Posted: March 24, 2019 Filed under: behavior, Breathing/respiration, emotions, health, Pain/discomfort, relaxation, Uncategorized | Tags: anxiety, aura, diaphragmatic breathing, dizzyness, light headedness, migraine, prodrome, symptom prescription 7 Comments
I quickly gasped twice and a sharp pain radiated up my head and into my eye. I shifted to slow breathing and it faded away.
I felt anxious and became aware of my heart palpitations at the end of practicing 70% exhalation for 30 seconds. I was very surprised how quickly my anxiety was triggered when I changed my breathing pattern.
Breathing is the body/mind/emotion/spirit interface which is reflected in our language with phrases such as a sigh of relief, all choked up, breathless, full of hot air, waiting with bated breath, inspired or expired, all puffed up, breathing room, or it takes my breath away. The colloquial phrases reflect that breathing is more than gas exchange and may have the following effects.
- Changes the lymph and venous blood return from the abdomen (Piller, Leduc, & Ryan, 2006). The downward movement of the diaphragm with the corresponding expansion of the abdomen occurs during inhalation as well as slight relaxation of the pelvic floor. The constriction of the abdomen and slight tightening of the pelvic floor causing the diaphragm to go upward and allows exhalation. This dynamic movement increases and decreases internal abdominal and thoracic pressures and acts a pump to facilitate the venous and lymph return from the abdomen. In many people this dynamic pumping action is reduced because the abdomen does not expand during inhalation as it is constricted by tight clothing (designer jean syndrome), holding the abdomen in to maintain a slim self-image, tightening the abdomen in response to fear, or the result of learned disuse to reduce pain from abdominal surgery, gastrointestinal disorders, or abdominal insults (Peper et al, 2015).
- Increases spinal disk movement. Effortless diaphragmatic breathing is a whole body process and associated with improved functional movement (Bradley, & Esformes, 2014). The spine slightly flexes when we exhale and extends when we inhale which allows dynamic disk movement unless we sit in a chair.
- Communicates our emotional state as our breathing patterns reflect our emotional state. When we are anxious or fearful the breath usually quickens and becomes shallow while when we relax the breath slows and the movement is more in the abdomen (Homma, & Masoka, 2008).
- Evokes, maintains, inhibits symptoms or promotes healing. Breathing changes our physiology, thoughts and emotions. When breathing slowly to about 6 breaths a minute, it may enhance heart rate variability and thereby increase sympathetic and parasympathetic balance (Lehrer & Gevirtz, 2014; Moss & Shaffer, 2017).
Can breathing trigger symptoms?
A fifty-five year old woman asked for suggestions what she could do to prevent the occurrence of episodic prodrome and aura symptoms of visual disturbances and problems in concentration that would signal the onset of a migraine. In the past, she had learned to control her migraines with biofeedback; however, she now experienced these prodromal sensation more and more frequently without experiencing the migraine. As she was talking, I observed that she was slightly gasping before speaking with shallow rapid breathing in her chest.
To explore whether breathing pattern may contribute to evoke, maintain or amplify symptoms, the following two behavioral breathing challenges can suggest whether breathing is a factor: Rapid fearful gasping or 70% exhalation.
Behavioral breathing challenge: Rapid fearful gasping
Take a rapid fearful gasp when inhaling as if your feel scared or fearful. Let the air really quickly come in and repeat two or three times as described in the video. Then describe what you experienced.
If you became aware of the onset of a symptom or that the symptom intensified, then your dysfunctional breathing patterns (e.g., gasping, breath holding or shallow chest breathing) may contribute to development or maintenance of these symptoms. For many people when they gasp–a big rapid inhalation as if they are terrified–it may evoke their specific symptom such as a pain sensation in the back of the eye, slight pain in the neck, blanking out, not being able to think clearly, tightness and stiffness in their back, or even an increase in achiness in their joints (Peper et al, 2016).
To reduce or avoid triggering the symptom, breathe diaphragmatically without effort; namely each time you gasp, hold your breath or breathe shallowly, shift to effortless diaphragmatic breathing.
The above case of the woman with the prodromal migraine symptoms, she experienced visual disturbances and fuzziness in her head after the gasping. This experience allowed her to realize that her breathing style could be a contributing in triggering her symptoms. When she then practiced slow diaphragmatic breathing for a few breaths her symptoms disappeared. Hopefully, if she replaces gasping and shallow breathing with effortless diaphragmatic breathing then there is a possibility that her symptoms may no longer occur.
Behavioral breathing challenge: 70% exhalation
While sitting, breathe normally for a minute. Now change your breathing pattern so that you exhale only 70% or your previous inhaled air. Each time you exhale, exhale only 70% of the inhaled volume. If you need to stop, just stop, and then return to this breathing pattern again by exhaling only 70 percent of the inhaled volume of air. After 30 seconds, let go and breathe normally as guided by the video clip. Observe what happened?
In our research study with 35 volunteers, almost all participants experienced an increase in arousal and symptoms such as lightheadedness, dizziness, anxiety, breathless, neck and shoulder tension after 30 seconds of incomplete exhalation as shown in Figure 1 and Table 1 (Peper and MacHose, 1993).
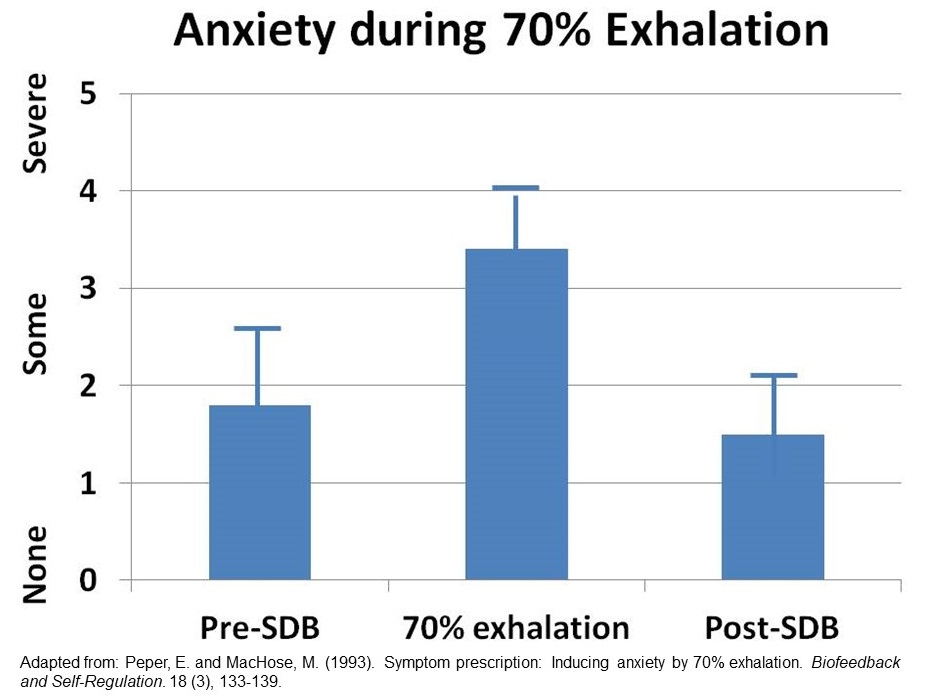
Figure 1. Increase in anxiety evoked by 70% exhalation.

Table 1. Symptoms experienced after exhalation 70%.
Although these symptoms may be similar to those evoked by hyperventilation and overbreathing, they are probably not caused by the reduction of end-tidal carbon dioxide (CO2). The apparent decrease in end-tidal PCO2 is cause by the room air mixing with the exhaled air and not a measure of end-tidal CO2 (Peper and Tibbets, 1992). Most likely the symptoms are associated by the shallow breathing that occurs when we were scared or terrified.
People who have a history of anxiety, panic, nervousness and tension as compared to those who report low anxiety tend to report more symptoms when exhaling 70% of inhaled air for 30 seconds. If this practice evoked symptoms, then changing the breathing patterns to slower diaphragmatic breathing may be a useful self-regulation strategy to optimize health.
These two behavior breathing challenges are useful demonstrations for students and clients that breathing patterns can influence symptoms. By experiencing ON and OFF control over their symptoms with breathing, the person now knows that breathing can affect their health and well being.
BLOGS WITH INSTRUCTIONS FOR LEARNING EFFORTLESS DIAPHRAGMATIC BREATHING
https://peperperspective.com/2017/11/17/breathing-to-improve-well-being/
https://peperperspective.com/2018/10/04/breathing-reduces-acid-reflux-and-dysmenorrhea-discomfort/
https://peperperspective.com/2015/02/18/reduce-hot-flashes-and-premenstrual-symptoms-with-breathing/
https://peperperspective.com/2017/03/19/enjoy-sex-breathe-away-the-pain/
REFERENCES
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Frontiers in Psychology, 5
Head position, it matters!*
Posted: January 23, 2019 Filed under: behavior, digital devices, Exercise/movement, health, Neck and shoulder discomfort, Pain/discomfort, posture, Uncategorized 5 CommentsThe blog has been adapted from our published article, Harvey, R., Peper, E., Booiman, A., Heredia Cedillo, A., & Villagomez, E. (2018). The effect of head and neck position on head rotation, cervical muscle tension and symptoms. Biofeedback. 46(3), 65–71.

Why is it so difficult to turn your head to see what is behind you?
How come so many people feel pressure in the back of the head or have headaches after working on the computer?
Your mother may have been right when she said, “Sit up straight! Don’t slouch!” Sitting slouched and collapsed is the new norm as digital devices force us to slouch or tilt our head downward. Sometimes we scrunch our neck to look at the laptop screen or cellphone. This collapsed position also contributes to an increased in musculoskeletal dysfunction (Nahar & Sayed, 2018). The more you use a screen for digital tasks, the more you tend to have head-forward posture, especially when the screens are small (Kang, Park, Lee, Kim, Yoon, & Jung, 2012). In addition, the less time children play outside and the more time young children watch the screen, the more likely will they become near sighted and need to have their vision corrected (Sherwin et al, 2012). In addition, the collapsed head forward position unintentionally decreases subjective energy level and may amplify defeated, helpless, hopeless thoughts and memories (Bader, 2015; Peper & Lin, 2012; Tsai, Peper, & Lin, 2016; Peper et al, 2017).
Explore the following two exercises to experience how the head forward position immediately limits head rotation and how neck scrunching can rapidly induce back of the head pressure and headaches.
Exercise 1. Effect of head forward position on neck rotation
Sit at the edge of the chair and bring your head forward, then rotate your head to the right and to the left and observe how far you can rotate. Then sit erect with the crown of the head reaching towards the ceiling and again rotate your head from right to left and observe how far you can rotate as shown in Figure 1.
 Figure 1. Head-erect versus head-forward position.
Figure 1. Head-erect versus head-forward position.
What did you experience?
Most likely your experience is similar to the 87 students (Mean Age = 23.6 years) who participated in this classroom activity designed to bring awareness of the effect of head and neck position on symptoms of muscle tension. 92.0% of the students reported that is was much easier to rotate their head and could rotate further during the head-erect position as compared to the head-forward position (see Figure 2).
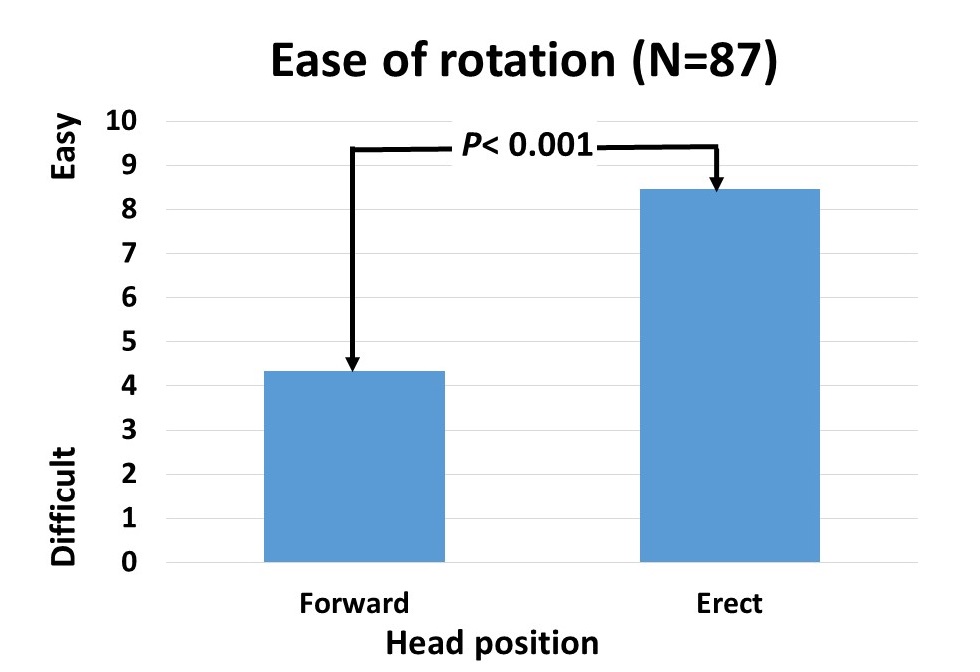 Figure 2. Self-report of ease of head rotation.
Figure 2. Self-report of ease of head rotation.
What does this mean?
Almost all participants were surprised that the head forward position restricted head rotation as well as reduced peripheral awareness (Fernandez-de-Las-Penas et al., 2006). The collapsed head forward may directly affect personal safety; since, it reduces peripheral awareness while walking, biking or driving a car. In addition, when the head is forward, the cervical vertebrae are in a more curved position compared to the erect head with the normal cervical curve (Kang et al., 2012). This means that in the head-forward position, the pressure on the vertebrae and the intervertebral disc is elevated compared to the preferred position with a stretched neck. This increases the risk of damage to the vertebrae and intervertebral disc (Kang et al, 2012). It also means that the muscles that hold the head in the forward position have to work much harder.
Be aware that of factors that contribute to a head-forward position.
- Sitting in a car seat in which the headrest pushes the head forward. Solutions: Tilt the headrest back or put pillow in your back from your shoulders to your pelvis to move your body slightly forward.
- If you wear a bun or ponytail, the headrest (car, airplane seat, or chair) will often push your head forward. This causes a change of the head to a more forward position and it becomes a habit without the person even knowing it. Solution: Place a pillow in your back to move your body forward or loosen the bun or ponytail.
- Difficulty reading the text on the digital screen. The person automatically cranes their head forward to read the text. Solutions: Have your eyes checked and, if necessary, wear computer-reading glasses; alternatively, increase the font size and reduce glare.
- Working on a laptop and looking down on the screen. Solutions: Detachable keyboard and laptop on a stand to raise screen to eye level as shown in Figure 3.
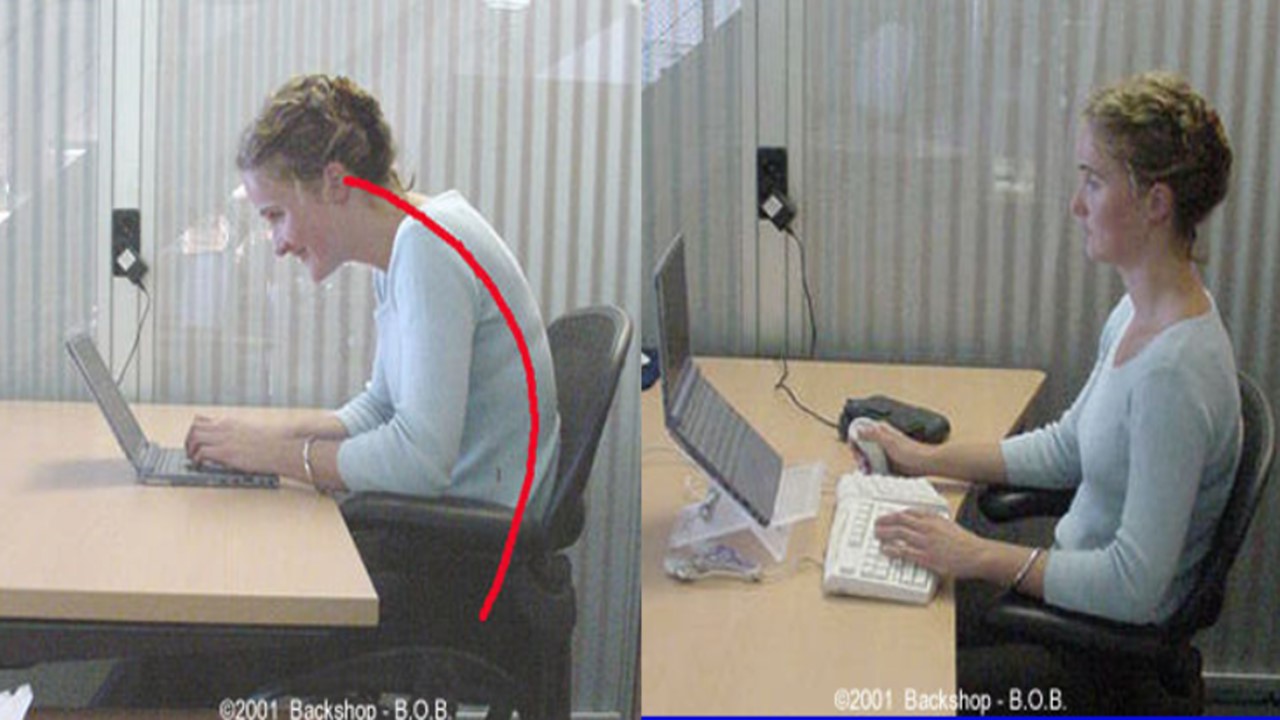
Figure 3. Trying to read the laptop screen, which causes the head to go forward as compared to raising the screen and using an external keyboard. Reproduced by permission from www.backshop.nl
- Being tired or exhausted encourages the body to collapse and slouch and increases the muscle tension in the upper cervical region. You can explore the effect of tiredness that causes slouching and head-forward position during the day by observing the following if you drive a car.
In the morning, adjust your rear mirror and side mirrors. Then at the end of the day when you sit in the car, you may note that you may need to readjust your inside rear mirror. No, the mirror didn’t change of position during the day by itself—you slouched unknowingly. Solutions: Take many breaks during the day to regenerate, install stretch break reminders, or wear an UpRight Go posture feedback device to remind you when you begin to slouch (Peper, Lin & Harvey, 2017).
Exercise 2: Effect of neck scrunching on symptom development
Sit comfortably and your nose forward and slightly. While the head is forward tighten your neck as if your squeezing the back of the head downward into the shoulders and hold this contracted neck position for 20 seconds. Let go and relax.
What did you experience?
Most likely your experience was similar to 98.4% of the 125 college students who reported a rapid increase in discomfort after neck scrunching as shown in Figure 4.
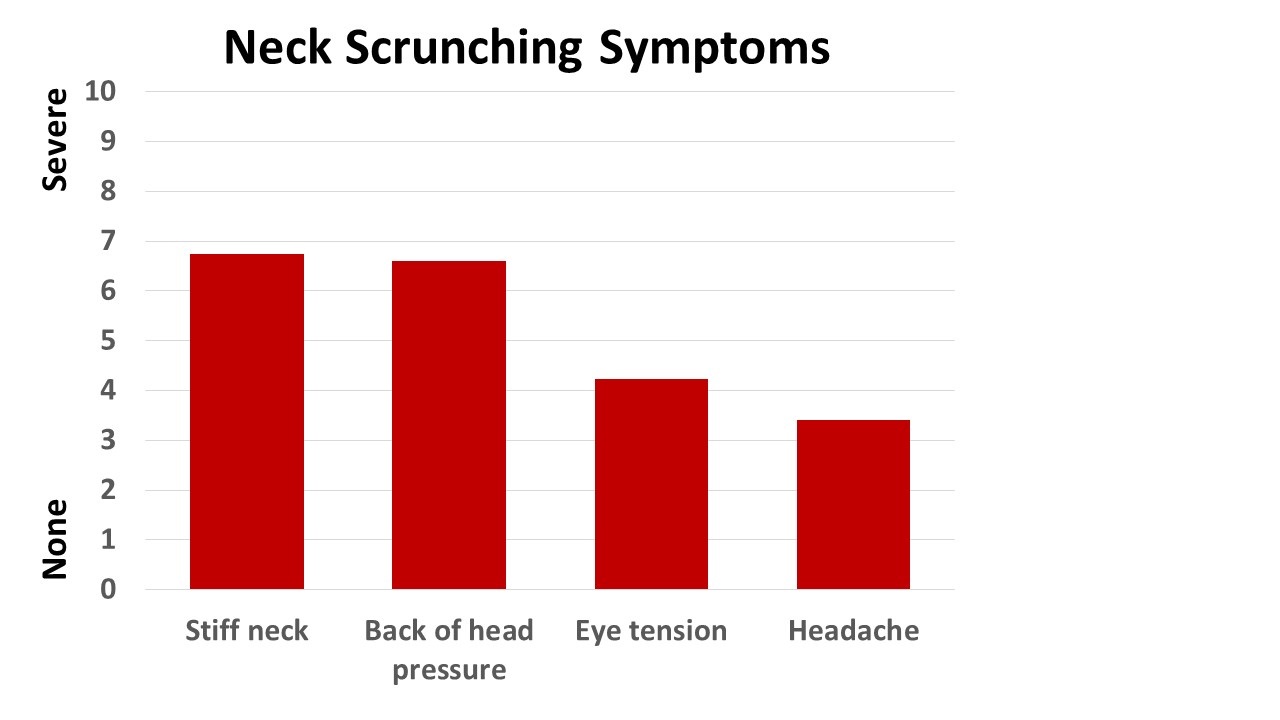 Figure 4. Symptoms induced by 30 seconds of neck scrunching.
Figure 4. Symptoms induced by 30 seconds of neck scrunching.
During scrunching there was a significant increase in the cervical and trapezius sEMG activity recorded from 12 volunteers as shown in Figure 5. Figure 5. Change in cervical and trapezius sEMG during head forward and neck scrunching.
Figure 5. Change in cervical and trapezius sEMG during head forward and neck scrunching.
What does this mean?
Nearly all participants were surprised that 30 seconds of neck scrunching would rapidly increase induce discomfort and cause symptoms. This experience provided motivation to identify situations that evoked neck scrunching and avoid those situations or change the ergonomics that induced the neck scrunching. If you experience headaches or neck discomfort, scrunching could be a contributing factor.
Factors that contribute to neck scrunching and discomfort.
- Bringing your head forward to see the text or graphics more clearly. There may be multiple causes such as blurred vision, tiny text font size, small screen and ergonomic factors. Possible solutions. Have your eyes checked and if appropriate wear computer-reading glasses. Increase the text font size or use a large digital screen. Reduce glare and place the screen at the appropriate height so that the top of the screen is no higher than your eyebrows.
- Immobility and working in static position for too long a time period. Possible solutions. Interrupt your static position with movements every few minutes such as stretching, standing, and wiggling.
Conclusion
These two experiential practices are “symptom prescription practices” that may help you become aware that head position contributes to symptoms development. For example, if you suffer from headaches or neck and backaches from computer work, check your posture and make sure your head is aligned on top of your neck–as if held by an invisible thread from the ceiling and take many movement breaks.The awareness may help you to identify situations that cause these dysfunctional body patterns that could cause symptoms. By inhibiting these head and neck patterns, you may be able to reduce or avoid discomfort. Just as a picture is worth a thousand words, self-experience through feeling and seeing is believing.
REFERENCES
Bader, E. E. (2015). The Psychology and Neurobiology of Mediation. Cardozo J. Conflict Resolution, 17, 363.
Fernandez-de-Las-Penas, C., Alonso-Blanco, C., Cuadrado, M. L., & Pareja, J. A. (2006). Forward head posture and neck mobility in chronic tension-type headache: A blinded, controlled study. Cephalalgia, 26(3), 314-319.
Kang, J. H., Park, R. Y., Lee, S. J., Kim, J. Y., Yoon, S. R., & Jung, K. I. (2012). The effect of the forward head posture on postural balance in long time computer based worker. Annals of rehabilitation medicine, 36(1), 98-104.
Lee, M. Y., Lee, H. Y., & Yong, M. S. (2014). Characteristics of cervical position sense in subjects with forward head posture. Journal of physical therapy science, 26(11), 1741-1743. https://doi.org/10.1589/jpts.26.1741
Nahar, S., & Sayed, A. (2018). Prevalence of musculoskeletal dysfunction in computer science students and analysis of workstation characteristics-an explorative study. International Journal of Advanced Research in Computer Science, 9(2), 21-27. https://doi.org/10.26483/ijarcs.v9i2.5570
Peper, E., & Lin, I. M. (2012). Increase or decrease depression: How body postures influence your energy level. Biofeedback, 40(3), 125-130
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41.
Peper, E., Lin, I-M, & Harvey, R. (2017). Posture and mood: Implications and applications to therapy. Biofeedback.35(2), 42-48.
Sherwin, J.C., Reacher, M.H., Keogh, R.H., Khawaja, A.P, Mackey, D.A., & Foster, P.J. (2012). The Association between Time Spent Outdoors and Myopia in Children and Adolescents: A Systematic Review and Meta-analysis. Ophthalmology, 119(10), 2141-2151. https://doi.org/10.1016/j.ophtha.2012.04.020
Tsai, H. Y., Peper, E., & Lin, I. M. (2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23-27.
*This blog was adapted from our published article, The blog has been adapted from our research article, Harvey, R., Peper, E., Booiman, A., Heredia Cedillo, A., & Villagomez, E. (2018). The effect of head and neck position on head rotation, cervical muscle tension and symptoms. Biofeedback. 46(3), 65–71.
Today is a new day-a new beginning
Posted: December 31, 2018 Filed under: behavior, health, Pain/discomfort, self-healing, Uncategorized | Tags: dance, hope, joy, pain, regenration, spinal injury 3 CommentsIn a world of turmoil, it is often challenging to think that tomorrow can be different and better. Yet, each day is an opportunity to accept whatever happened in the past and look forward to the unfolding present. So often, we anticipate that the future will be the same or worse especially if we feel depressed, suffer from ongoing pain, chronic illness, family or work stress, etc. At those moments, we forget that yesterday’s memories may contribute to how we experience and interpret the future. Most of us do not know what the future will bring, thus be open to new opportunities for growth and well-being. For the New Year, adapt a daily ritual that I learned from a remarkable healer Dora Kunz.
Each morning when you get out of bed, take a few slow deep breaths. Then think of someone who you feel loved by and makes you smile whether your grandmother, aunt or dog. Then when you get up and put your feet on the ground, say out loud, “Today is a new day- a new beginning.”
Watch the following two videos of people for whom the future appeared hopeless and yet had the courage to transcend their limitations and offer inspiration and joy.
Janine Shepherd: A broken body isn’t a broken person. Cross-country skier Janine Shepherd hoped for an Olympic medal — until she was hit by a truck during a training bike ride. She shares a powerful story about the human potential for recovery. Her message: you are not your body, and giving up old dreams can allow new ones to soar.
Ma Li and Zhai Xiaowei: Hand in Hand. This is a video of a broadcast that originally aired on China’s English-language CCTV channel 9 during a modern dance competition in Beijing, China in 2007. This very unique couple–she without an arm, he without a leg–was one of the finalists among 7000 competitors in the 4th CCTV national dance competition. It is the first time a handicapped couple had ever entered the competition. They won the silver medal and became an instant national hit. The young woman, in her 30’s, was a dancer who had trained since she was a little girl. Later in life, she lost her entire right arm in an automobile accident and fell into a state of depression for a few years. After rebounding, she decided to team with a young man who had lost his leg in a farming accident as a boy and who was completely untrained in dance. After a long and sometimes agonizing training regimen, this is the result. The dance is performed by Ma Li (馬麗) and Zhai Xiaowei (翟孝偉). The music “Holding Hands” is composed by San Bao and choreographed by Zhao Limin.
Breathing reduces acid reflux and dysmenorrhea discomfort
Posted: October 4, 2018 Filed under: Breathing/respiration, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: acid reflux, dysmenorrhea, gastroesophageal reflux disease, GERD, menstrual cramps, PMS 14 CommentsPublished as: Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
“Although difficult and going against my natural reaction to curl up in the response to my cramps, I stretched out on my back and breathed slowly so that my stomach got bigger with each inhalation. My menstrual pain slowly decreased and disappeared.
“For as long as I remember, I had stomach problems and when I went to doctors, they said, I had acid reflux. I was prescribed medication and nothing worked. The problem of acid reflux got really bad when I went to college and often interfered with my social activities. After learning diaphragmatic breathing so that my stomach expanded instead of my chest, I am free of my symptoms and can even eat the foods that previously triggered the acid reflux.”
In the late 19th earlier part of the 20th century many women were diagnosed with Neurasthenia. The symptoms included fatigue, anxiety, headache, fainting, light headedness, heart palpitation, high blood pressure, neuralgia and depression. It was perceived as a weakness of the nerves. Even though the diagnosis is no longer used, similar symptoms still occur and are aggravated when the abdomen is constricted with a corset or by stylish clothing (see Fig 1).

Figure 1. Wearing a corset squeezes the abdomen.
The constricted waist compromises the functions of digestion and breathing. When the person inhales, the abdomen cannot expand as the diaphragm is flattening and pushing down. Thus, the person is forced to breathe more shallowly by lifting their ribs which increases neck and shoulder tension and the risk of anxiety, heart palpitation, and fatigue. It also can contribute to abdominal discomfort since abdomen is being squeezed by the corset and forcing the abdominal organs upward. It was the reason why the room on top of stairs in the old Victorian houses was call the fainting room (Melissa, 2015).
During inhalation the diaphragm flattens and attempts to descend which increases the pressure of the abdominal content. In some cases this causes the stomach content to be pushed upward into the esophagus which could result in heart burn and acid reflux. To avoid this, health care providers often advice patients with acid reflux to sleep on a slanted bed with the head higher than their feet so that the stomach content flows downward. However, they may not teach the person to wear looser clothing that does not constrict the waist and prevent designer jean syndrome. If the clothing around the waist is loosened, then the abdomen may expand in all directions in response to the downward movement of the diaphragm during inhalation and not squeeze the stomach and thereby pushing its content upward into the esophagus.
Most people have experienced the benefits of loosening the waist when eating a large meal. The moment the stomach is given the room to spread out, you feel more comfortable. If you experienced this, ask yourself, “Could there be a long term cost of keeping my waist constricted?” A constricted waist may be as harmful to our health as having the emergency brake on while driving for a car.
We are usually unaware that shallow rapid breathing in our chest can contribute to symptoms such as anxiety, neck and shoulder tension, heart palpitations, headaches, abdominal discomfort such as heart burn, acid reflux, irritable bowel syndrome, dysmenorrhea and even reduced fertility (Peper, Mason, & Huey, 2017; Domar, Seibel, & Benson, 1990).
Assess whether you are at risk for faulty breathing
Stand up and observe what happens when you take in a big breath and then exhale. Did you feel taller when you inhaled and shorter/smaller when you exhaled?
If the answer is YES, your breathing pattern may compromise your health. Most likely when you inhaled you lifted your chest, slightly arched your back, tightened and raised your shoulders, and lifted your head up while slightly pulling the stomach in. When you exhaled, your body relaxed and collapsed downward and even the stomach may have relaxed and expanded. This is a dysfunctional breathing pattern and the opposite of a breathing pattern that supports health and regeneration as shown in figure 2.

Figure 2. Incorrect and correct breathing. Source unknown.
Observe babies, young children, dogs, and cats when they are peaceful. The abdomen is what moves during breathing. While breathing in, the abdomen expands in all 360 degrees directions and when breathing out, the abdomen constricts and comes in. Similarly when dogs or cats are lying on their sides, their stomach goes up during inhalation and goes down during exhalation.
Many people tend to breathe shallowly in their chest and have forgotten—or cannot– allow their abdomen and lower ribs to widen during inhalation (Peper et al, 2016). These factors include:
- Constriction by the modern corset called “Spanx” to slim the figure or by wearing tight fitting pants. In either case the abdominal content is pushed upward and interferes with normal healthy breathing.
- Maintaining a slim figure by pulling the abdomen (I will look fat when my stomach expands; I will suck it in).
- Avoiding post-surgical abdominal pain by inhibiting abdominal movement. Numerous patients have unknowingly learned to shallowly breathe in their chest to avoid pain at the site of the incision of the abdominal surgery such as for hernia repair or a cesarean operation. This dysfunctional breathing became the new normal unless they actively practice diaphragmatic breathing.
- Slouching as we sit or watch digital screens or look down at our cell phone.
Observe how slouching affects the space in your abdomen.
When you shift from an upright erect position to a slouched or protective position the distance between your pubic bone and the bottom of the sternum (xiphoid process) is significantly reduced.
- Tighten our abdomen to protect ourselves from pain and danger as shown in Figure 3.

Figure 3. Erect versus collapsed posture. There is less space for the abdomen to expand in the protective collapsed position. Reproduced by permission from Clinical Somatics (http://www.clinicalsomatics.ie/).
Regardless why people breathe shallowly in their chest or avoid abdominal and lower rib movement during breathing, by re-establishing normal diaphragmatic breathing many symptoms may be reduced. Numerous students have reported that when they shift to diaphragmatic breathing which means the abdomen and lower ribs expand during inhalation and come in during exhalation as shown in Figure 4, their symptoms such as acid reflux and menstrual cramp significantly decrease.

Figure 4. Diaphragmatic breathing. Reproduced from: www.devang.house/blogs/thejob/belly-breathing-follow-your-gut.
Reduce acid reflux
A 21-year old student, who has had acid reflux (GERD-gastroesophageal reflux diseases) since age 6, observed that she only breathed in her chest and that there were no abdominal movements. When she learned and practiced slower diaphragmatic breathing which allowed her abdomen to expand naturally during inhalation and reduce in size during exhalation her symptoms decreased. The image she used was that her lungs were like a balloon located in her abdomen. To create space for the diaphragm going down, she bought larger size pants so that her abdominal could spread out instead of squeezing her stomach (see Figure 5).

Figure 5. Hydraulic model who inhaling without the abdomen expanding increases pressure on the stomach and possibly cause stomach fluids to be pushed into the esophagus.
She practiced diaphragmatic breathing many times during the day. In addition, the moment she felt stressed and tightened her abdomen, she interrupted this tightening and re-established abdominal breathing. Practicing this was very challenging since she had to accept that she would still be attractive even if her stomach expanded during inhalation. She reported that within two weeks her symptom disappeared and upon a year follow-up she has had no more symptoms. In the video she describes her experiences of integrate breathing and awareness into daily life.
We have also use this similar approach to successfully overcome irritable bowel syndrome see: https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/
Take control of menstrual cramps
Numerous college students have reported that when they experience menstrual cramps, their natural impulse is to curl up in a protective cocoon. If instead they interrupted this natural protective pattern and lie relaxed on their back with their legs straight out and breathe diaphragmatically with their abdomen expanding and going upward during inhalation, they report a 50 percent decrease in discomfort (Gibney & Peper, 2003). For some the discomfort totally disappears when they place a warm pad on their lower abdomen and focused on breathing slowly about six breaths per minute so that the abdomen goes up when inhaling and goes down when exhaling. At the same time, they also imagine that the air would flow like a stream from their abdomen through their legs and out their feet while exhaling. They observed that as long as they held their abdomen tight the discomfort including the congestive PMS symptoms remained. Yet, the moment they practice abdominal breathing, the congestion and discomfort is decreased. Most likely the expanding and constricting of the abdomen during the diaphragmatic breathing acts as a pump in the abdomen to increase the lymph and venous blood return and improve circulation.
Conclusion
Breathing is the body-mind bridge and offers hope for numerous disorders. Slower diaphragmatic breathing with the corresponding abdomen movement at about six breaths per minute may reduce autonomic dysregulation. It has profound self-healing effects and may increase calmness and relaxation. At the same time, it may reduce heart palpitations, hypertension, asthma, anxiety, and many other symptoms.
References
DeVault, K.R. & Castell, D.O. (2005). Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The American Journal of Gastroenterology, 100, 190-200.
Domar, A.D., Seibel, M.M., & Benson, H. (1990). The Mind/Body Program for Infertility: a new behavioral treatment approach for women with infertility. Fertility and sterility, 53(2), 246-249.
Gibney, H.K. & Peper, E. (2003). Taking control: Strategies to reduce hot flashes and premenstrual mood swings. Biofeedback, 31(3), 20-24.
Johnson, L.F. & DeMeester, T.R. (1981). Evaluation of elevation of the head of the bed, bethanechol, and antacid foam tablets on gastroesophageal reflux. Digestive Diseases Sciences, 26, 673-680. https://www.ncbi.nlm.nih.gov/pubmed/7261830
Melissa. (2015). Why women fainted so much in the 19th century. May 20, 2015. Donloaded October 2, 1018. http://www.todayifoundout.com/index.php/2015/05/women-fainted-much-19th-century/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. (45-4)
Stanciu, C. & Bennett, J.R.. (1977). Effects of posture on gastro-oesophageal reflux. Digestion, 15, 104-109. https://www.karger.com/Article/Abstract/197991
Family or work? The importance of value clarification
Posted: May 4, 2018 Filed under: Breathing/respiration, mindfulness, Neck and shoulder discomfort, Pain/discomfort, relaxation, stress management, Uncategorized | Tags: meaning, regeneration, relaxation, respiration, stress management, values clarification 1 CommentRichard Harvey, PhD and Erik Peper, PhD

In a technologically modern world, many people have the option of spending 24 hours a day/ 7 days a week continuously interacting via telephone, text, work and personal emails or internet websites and various social media platforms such as Facebook, What’s App, Instagram, Twitter, LinkedIn and Snapchat. How many people do we know who work too many hours, watch too many episodes on digital screens, commute too many hours, or fill loneliness with online versions of retail therapy? In the rush of work-a-day survival as well as being nudged and bombarded with social media notifications, or advertisements for material goods, we forget to nurture meaningful friendships and family relationships (Peper and Harvey, 2018). The following ‘values clarification’ practice may help us identify what is most important to us and help keep sight of those things that are most relevant in our lives (Hofmann, 2008; Knott, Ribar, & Duson, 1989; Twohig & Crosby, 2009;. Peper, 2014).
Give yourself about 12 minutes of uninterrupted time to do this practice. Do this practice by yourself, in a group, or with family and friends. Have a piece of paper ready. Be guided by the two video clips at the end of the blog. Begin with the Touch Relaxation and Regeneration Practice to relax and let go of thoughts and worries, then follow it with the Value Clarification Practice.
Touch Relaxation and Regeneration Practice
Turn off your cell phone and let other know not to interrupt for the next 12 minutes, then engage in the following six-minute relaxation exercise. If your attention wanders during the practice, then bring your attention back to the various sensations in your body.
- Sit comfortably, then lift your arms from your lap, holding them parallel to the floor and tighten your arms while making a fist in each hand. While holding your fists tightly closed, keep breathing for a total of 10 seconds before dropping the arms to your lap while you relax all of your muscles. Attend for 20 seconds to the changing sensations in arms and hands as they relax. If your attention wanders bring it back to the sensations in your arm and hands.
- Tighten your buttock muscles and bend your ankles so that the toes move upwards in a direction towards your knees. Keep breathing and hold your toes upwards for 10 seconds and then let the toes move down to the floor, letting go and relaxing all the muscles of the lower trunk and legs. Feel your knees widening and feel your buttock muscles relaxing. Continue attending to the body and muscle sensations for the next 20 seconds. If your attention wanders bring it back to the sensations in your body.
- Tighten your whole body by pressing your knees together, lifting your arms up from your lap, making a fist and wrinkling your face. Hold the tension while continuing to breath for 10 seconds. Let go and relax and feel the whole body sinking and relaxing and being supported by the chair for the next 20 seconds.
- Bring your right hand to your left shoulder. Over the next 10 seconds, inhale for three or four seconds and as you exhale for five or six seconds, with your right hand stroke down your left arm from your shoulder to past your hand. Imagine that the exhaled air is flowing through your arm and out your hand. Repeat at least once more.
- Bring your left hand to your right shoulder. Inhale for three or four seconds and as you exhale for five or six seconds with your left hand stroke down your right arm from your shoulder to past your hand. Imagine that the exhaled air is flowing through your arm and out your hand. Repeat at least once more.
- Bring both hands to the sides of your hips. Inhale for three or four seconds and as you exhale for five or six seconds stroke your legs with your hands from the hips to the ankles. Imagine that the exhaled air is flowing through your legs and out your feet. Repeat a least once more.
- Close your eyes and inhale for three or four seconds, then hold your breath for seven seconds slowly exhale for eight seconds. Imagine as you exhale the air flowing through your arms and out your hands and through your legs and out your feet. Continue breathing easily and slowly such as inhaling for three or four seconds, and out for five to seven seconds. If your attention wanders just bring it back to the sensations going down your arms and legs. Feel the relaxation and peacefulness.
- Take another deep breath and then stretch and continue with the Value Clarification
Value Clarification Practice
Get the paper and pen and do the following Value Clarification Practice.
- Quickly (e.g. 30-60 seconds) list the 10 most important things in your life. For the activity to work, the list must contain 10 important things that may be concrete or abstract, ranging from material things such as a smart phone or a car to immaterial things such as family, love, god, health… If you need to, break up a larger category into smaller pieces. For example, if one item on the list is family, and you only have seven items on the list, assuming you have a family of four, then identify separate family members in order to complete a list of 10 important things.
- To start off, in only 10 seconds, please cross off three items from the list, then explain why you removed those three. If done in a group of people turn to the person explain why you made these choices.
- Next, in only 10 seconds, please cross off three more, then explain why you kept what you kept. If done in a group of people turn to the person explain why you made these choices.
- Finally, in only 10 seconds, please cross off three more, then reveal the one most important thing on your list. Share your choice for the item you kept and how you felt while crossing items from the list or keeping them.
- When engaging with this type of values clarification practice, please remind yourself and others that the items on the list were never gone, they are always in your life to the extent that you can honor the presence of those things in your life.
We have done these exercises with thousands of student and adults. The most common final item on the list is family or an individual family member. Sometimes, categories such as health or god appear, however it is extremely rare that material items make it to the final round. For example, no one would report that their last item is their job, their bank account, their house, or their smart phone. It is common that people have difficulty choosing the last item on their list, often taking more than 10 seconds to choose. For example, they find that they cannot choose between eliminating individual family members. For those who find the activity too difficult, remind them that the exercise is voluntary and meant as a ‘thought experiment’ which they may stop at any time.
Reflect how much of your time is spent nurturing what is most important to you? In many cases we feel compelled to finish some employment priorities instead of making time for nurturing our family relationship. And when we become overwhelmed with work demands, we retreat to sooth our difficulties by checking our email or browsing social media rather than supporting the family connections that are so important to us.
Organize an action plan to honor and support your commitment to the items on your list that you value the most. If possible let other people know what you are doing.
- Describe in detail what you will do in real life and in real time in service to honor and support your relationships with the things that you value.
- Describe in detail what you will do, when you will do it, with whom you will do it, at what time you will do it, and anticipate what will get in the way of doing it. For example, how will you resolve any conflicts between what you plan and what you actually do when there is not enough time to carry out your plans?
- Schedule a time during the following week for feedback about your plans to honor and support the things you value.
Summary
Many people experience that it is challenging to make time to honor and support their primary values given the ongoing demands of daily living. To be congruent with our values means making ongoing choices such as listening and sharing experiences with your partner versus binging on videos or, using your smartphone for answering email or texting instead of watching your child play ball.
The values you previously identified are similar to those identified by patients who are in hospice and dying. For them as they look back on their lives, the five most common regret are (Ware, 2009; Ware, 2012):
- I wish I’d the courage to live a life true to myself, not the life others expected of me.
- I wish I hadn’t worked so hard.
- I wish I had the courage to express my feelings.
- I wish I had stayed in touch with my friends.
- I wish I had let myself be happier.
Take the time to plan actions that support your identified values. Feel free to watch the following videos that guide you through the activities described here.
References
Hofmann, S.G. (2008). Acceptance and commitment therapy: New wave or Morita therapy?. Clinical Psychology: Science and Practice, 15(4), 280-285. https://doi.org/10.1111/j.1468-2850.2008.00138.x
Knott, J.E., Ribar, M.C. & Duson, B.M. (1989). Thanatopics: Activities and Exercises for Confronting Death, Lexington Books: Lexington, MA. https://www.amazon.com/Thanatopics-Activities-Exercise-Confronting-Death/dp/066920871X
Peper, E. (October 19, 2014). Choices-Creating meaningful days. https://peperperspective.com/2014/10/19/choices-creating-meaningful-days/
Peper, E. & Harvey, R. (2018). Digital addiction: increased loneliness, depression, and anxiety. NeuroRegulation. 5(1),3–8. doi:10.15540/nr.5.1.3 http://www.neuroregulation.org/article/view/18189/11842
Twohig, M.P. & Crosby, J.M. (2009). Values clarification. In: O’Donohue & W.T., Fisher, J.E., Eds. Cognitive behavior therapy: applying empirically supported techniques in your practice. Wiley: Hoeboken, N.J., p. 681-686.
Ware, B. (2009). Regrets of the dying. https://bronnieware.com/blog/regrets-of-the-dying/
Ware, B. (2012). The top five regrets of dying: A life transformed by the dearly departing. Hay House. ISBN: 978-1401940652
Surgery: Hope for the best and plan for the worst!
Posted: March 18, 2018 Filed under: Pain/discomfort, placebo, self-healing, stress management, surgery, Uncategorized | Tags: anesthesia, hernia, iatrogenic illness, technology, urinary retention 20 CommentsAdapted from: Peper, E. Surviving and preventing medical errors. (2019). Townsend Letter-The Examiner of Alternative Medicine. 429, 63-69. https://townsendletter.com/surviving-and-preventing-medical-errors-peper/
The purpose of this blog is to share what I have learned from a cascade of medical errors that happen much more commonly than surgeons, hospitals, or health care providers acknowledge and is the third leading cause of death in the US (Makary, M.A. & Daniel, M., 2016). My goal here is to provide a few simple recommendations to reduce these errors.

It is now two years since my own surgery—double hernia repair by laparoscopy. The recovery predicted by my surgeon, “In a week you can go swimming again,” turned out to be totally incorrect.
Six weeks after the surgery, I was still lugging a Foley catheter with a leg collection bag that drained my bladder. I had swelling due to blood clots in the abdominal area around my belly button, severe abdominal cramping, and at times, overwhelming spasms. For six weeks my throat was hoarse following the intubation. Instead of swimming, hiking, walking, working, and making love with my wife, I was totally incapacitated, unable to work, travel, or exercise. I had to lie down every few hours to reduce the pain and the spasms.
Instead of going to Japan for a research project, I had to cancel my trip. Rather than teaching my class at the University, I had another faculty member teach for me. I am a fairly athletic guy—I swim several times a week, bike the Berkeley hills, and hiked. Yet after the surgery, I avoided even walking in order to minimize the pain. I moved about as if I were crippled. Now two years later, I finally feel healthy again.
How come my experiences were not what the surgeon promised?
All those who cared for me during this journey were compassionate individuals, committed to doing their best, including the emergency staff, the nurses, my two primary physicians, my surgeon, and my urologist. However, given the personal, professional, and economic cost to me and my family, I feel it is important to assess where things went wrong. The research literature makes it clear that my experience was by no means unique, so I have summarized some of the most important factors that contributed to these unexpected complications, following “simple arthroscopic surgery.”
- Underestimating the risk. Although the surgeon suggested that the operation would be very low risk with no complications, the published research data does not support his optimistic statement and misrepresented the actual risk. Complications for laparoscopic surgery range from 15% to as high as 38% or higher, depending on the age of the patient and how well they do with general anesthesia (Vigneswaran et al, 2015; Neumayer et al, 2004; Perugini & Callery, 2001). Experienced surgeons who have done more than 250 laparoscopic surgeries have a lower complication rate. However, a 2011 Cochran review points out that there is theoretically a higher risk that intra-abdominal organs will be injured during a laparoscopic procedure (Sauerland, 2011). In addition, bilateral laparoscopic hernia repair has significantly higher risk than single sided laparoscopic hernia repair for post-operative urinary retention (Blair et al, 2016). My experience is not an outlier–it is more common.
- Inappropriate post-operative procedures. In my case I was released directly after waking up from general anesthesia without checking to determine whether I could urinate or not. The medical staff and facility should never have released me, since older males have a 30% or higher probability that urinary retention will occur after general anesthesia. However, it was a Friday afternoon and the staff probably wanted to go home since the facility closes at 5:30 pm. This landed me in the Emergency Room.
- Medical negligence. In my case the surgeon recommended that I have my bladder in the emergency room emptied and then go home. That was not sufficient, and my body still was not working properly, requiring a second visit to the ER and the insertion of a Foley catheter. Following the second ER visit, the surgeon removed the catheter in his office in the late afternoon and did not check to determine whether I could urinate or not. This resulted in a third ER visit.
- Medical error. On my third visit to the emergency room, the nurse made the error of inflating the Foley catheter balloon when it was in the urethra (rather than the bladder) which caused tearing and bleeding of the urethra and possible irritation to the prostate.
- Drawbacks of the ER as the primary resource for post-surgical care. Care is not scheduled for the patient’s needs, but rather based on a triage system. In my case I had to wait sometimes two hours or more until a catheter could be inserted. The wait kept increasing the urine volume which expanded and irritated the bladder further.
- A medical system that does not track treatment outcomes. Without good follow-up and long-term data, no one is accountable or responsible.
- A reimbursement system that rewards lower up-front costs. The system favors quick outpatient surgeries without factoring in the long-term costs and harm of the type I experienced.
Assuming the best and not planning for the worst.
Can I trust the health care provider’s statement that the procedure is low risk and that the recovery will go smoothly?
The typical outcome of a medical procedure or surgery may be significantly worse than generally reported by hospitals or medical staff. In many cases there is no systematic follow-up nor data on outcomes and complications, thus no one knows the actual risks.
In the United States medical error results in at least 98,000 unnecessary deaths each year and 1,000,000 excess injuries (Weingart et al, 2000; Khon et al, 2000). The Institute of Medicine reported in 2012 that one-third of hospitalized patients are harmed during their stay (Ferguson, 2012; Institute of Medicine, 2012).
One should also be intelligently skeptical about positive claims for any specific study—it is important to know whether the study has been replicated with other populations and not just a particular group of patients.
To quote Dr. Marcia Angell (2009), the first woman editor of the highly respected New England Journal of Medicine, “It is simply no longer possible to believe much of the clinical research that is published, or to rely on the judgment of trusted physicians or authoritative medical guidelines. I take no pleasure in this conclusion, which I reached slowly and reluctantly over my two decades as an editor of The New England Journal of Medicine.”
The evidence for many procedures and medications is surprisingly limited
- Research studies frequently select specific subsets of patients. They may exclude many patients who have other co-morbidities.
- Clinical trials may demonstrate statistical significance without providing clinically meaningful results. For example, between 2009 and 2013 all most all cancer drugs that were approved for treatment in Europe showed upon follow-up no clear evidence that they improved survival or quality of life for patients (Davis et al, 2017; Kim & Prasad, 2015).
- Pharmaceuticals are tested only against a passive placebo. In some cases, the patient’s positive response may actually be the placebo effect, due to physical sensations induced by the medication or its side effects, thus inspiring hope that the drug is working (Peper and Harvey, 2017).
- Negative side effects are significantly underreported. The data depend on self-report by both the patient and the health care provider.
Many published studies on the positive clinical outcome of pharmaceuticals are suspect. As Dr. Richard Horton (2015), Editor-in-Chief of The Lancet, wrote in 2015, “A lot of what is published is incorrect … much of the scientific literature, perhaps half, may simply be untrue. Afflicted by studies with small sample sizes, tiny effects, invalid exploratory analyses, and flagrant conflicts of interest, together with an obsession for pursuing fashionable trends of dubious importance, science has taken a turn towards darkness.”
Most studies, including those on surgery, lack long-term follow-up.
The apparent short-term benefits may be not beneficial in the long term or may even be harmful. For example, doctors and patients are convinced that SSRIs (serotonin re-uptake inhibitors—antidepressants such as Paxil and Prozac) are beneficial, with resulting global sales in 2011 of $11.9 billion. However, when all the research data were pooled, metanalysis showed that these drugs are no more effective than placebo for the treatment of mild to moderate depression and increase suicides significantly among young adults (Fournier et all, 2010; Kirsch, 2014).
Consider long-term follow-up in my case: the surgeon will report a successful surgery, despite the fact that it took me almost two years to recover fully. (I did not die during surgery and left in seemingly good shape.). Although I called him numerous times for medical guidance during my complications, the outpatient surgical facility will report no complications since I was not transferred from that facility during the surgery to a hospital for continuing care. My insurance carrier that paid the majority of the medical bills recorded the invoices as separate unrelated events: one surgery/one bill, but three separate bills for the emergency room, an additional visit to my primary care physician to check my abdomen when my surgeon did not return my call, and the ongoing invoices from the urologist. They all reported success because the iatrogenic events were not linked to the initial procedure in the data base.
In my case, following surgery, I had to go to the emergency room on three separate occasions due to post-operative urinary retention, placing me at risk of permanent detrusor muscle damage. For more than 18 months, I was under the care of a urologist.
Over the past two years, my symptoms have included gastrointestinal inflammation, spasms, and abdominal bulging, which are only now disappearing. Even my posture has changed. I am now working to reverse the automatic flexing at the hips and leaning forward which I covertly learned to reduce the abdominal discomfort. This level of discomfort and dysfunction are new to me. Reading the research on laparoscopy, I realized that excessive internal bruising, large hematomas, and internal adhesions are fairly common with this type of surgery. However, soft tissue injuries are difficult to confirm with imaging techniques.
My complications were also a direct result of inappropriate post-surgical recommendations and treatment. The symptoms were further compounded by faulty patient discharge procedures performed by the outpatient surgical facility. Since this was my first general anesthesia, I had no idea that I would be one of the people whose outcome were not what the surgeon had predicted. Thus, hope for the best, but plan for the worst.
SCHEDULING MEDICAL PROCEDURES
The following are recommendations may help reduce post-surgical or medical procedure complications.
- Schedule elective medical procedures or surgery early the morning and in the middle of the week. Do not schedule procedures on Mondays, Fridays, or in the afternoon. Procedures performed in the afternoon have significant increase in complications and errors. Anesthesia complications, for example, are four times higher in the afternoon than in the morning (Wright et al, 2006). Our biological rhythms affect our ability to attend and focus. In the morning most people are able to concentrate better than in the afternoon (Pink, 2018).
- Avoid weekends. Procedures performed on weekends (as compared to those done in the middle of the week) increase the risk of complications or dying. For example, babies born on the weekend have a 9.2% higher infant mortality than those born during the week, while those born on Tuesdays have the lowest death rate (Palmer et al, 2015). It is possible that on Mondays medical staff are recovering from weekend binging, while on Fridays they are tired and looking forward to the weekend? If elective procedures are done on a Friday and complications arise, the emergency room is the only option, as the medical staff may not be available over the weekend. In my case the procedure was done on a Friday, and I left the surgical outpatient facility at 2 pm. When complications occurred, it was after 5:30 pm—phone support from the advice nurse and the surgeon on call were my only option until the following Monday. Thus, I had to go the emergency room late Friday evening and again the next evening because of urinary retention, with a long delay in a busy waiting room. Since, I wasn’t bleeding or having a heart attack, that meant I had to wait, wait and wait, which significantly aggravated my specific problem.
- Schedule medical procedures at least one or two weeks before any holiday. Do not schedule surgery just before or during holidays. Medical staff also take holidays and may not available. In my case, I scheduled the procedure the Friday before Thanksgiving because I thought I would have a week of recovery during my Thanksgiving break from teaching. This meant that medical staff were less available and more involved in their holiday planning.
- Schedule procedures so that you are released early in the day. This can allow you to return to the facility in case complications arise. I was released at 2 pm and the complications did not occur until early evening. The facility was closed, so the only option was the ER. When possible, schedule medical procedures or surgery in a facility that is able to provide post-operative care after 5 pm.
- Do not schedule elective procedures during the month of July in an academic teaching hospital. During this month mortality increases and efficiency of care decreases because of the end of the academic year and subsequent changeover to new personnel (Young et al, 2011). Medical school graduates with limited clinical experience begin their residencies and experienced house staff are replaced with new trainees. This is known as the July effect in the U.S. and Killing season in the United Kingdom. During the month of July in any given year, fatal medication errors, for example, increase by 10% at teaching hospitals, but not at neighboring hospitals which do not experience this turnover in medical personnel (Phillips & Barker, 2010).
- Have procedures performed at a medical facility in which the health care professional has no financial interest—take economics out of the equation. When health care practitioners have financial interest in a facility, they tend to order more tests and procedures than health care providers who have no financial interests (Bishop et al, 2010). In my case the surgeon had a financial interest in the outpatient surgical facility where I received surgery. Had I had the operation across the street in the hospital where the surgeon also operates, I probably would not have been released early, avoiding the problems in follow-up care.
STRATEGIES TO OPTIMIZE OUTCOMES AND HEALTH
Organize your support system. Assume that recovery could be more difficult then promised.
Before your procedure, ask family members, friends, and neighbors to be prepared to help. If you did not need them, thank them for their willingness to help. In my case I did not plan for complications, thus my wife was my entire support system, especially for the first three weeks when I was unable to do anything except rest and cope. I was very fortunate to have numerous family, friends, and colleagues who offered their expertise to help me understand what was going on and who assumed my responsibilities when needed.[1]
- Bring an advocate to your appointments. Have your advocate/friend keep notes and ask questions, especially if the health care provider is a respected authority and you are suffering, exhausted, and/or anxious. Record any detailed instructions you must follow at home as a video or audio file on your cell phone or write them down (be sure to ask the health provider for permission). Under stress one may not be able to fully process instructions from the health care provider.
- Make a list of questions and concerns before seeing your health care provider. Talk to your partner and close friends and ask them if there are questions or concerns that you should raise with your provider.
- Ask for more information when tests or procedures are proposed (Robin, 1984).
- Why do you recommend this particular test/procedure/intervention for me and what are the major benefits?
- What are the risks and how often do they occur, in your experience and in the research literature?
- What will you do if the treatment is not successful?
- Ask your provider if there is anything that you should or should not do to promote healing. As much as possible, ask for advice on specific efforts you can make. General statements without instructions such as, “Relax” or “Don’t worry,” are not helpful unless the practitioner teaches you specific skills to relax or to interrupt worrisome thoughts. Many health professionals do not have the time to teach you these types of skills. In many cases the provider may not be able to recommend documented peer-reviewed self-care strategies. Often they imply—and they can be correct—that the specific medical treatment is the only thing that will make you better. In my case I did not find any alternative procedures that would reverse a hernia, although there may be habitual postural and movement patterns that could possibly prevent the occurrence of a hernia (Bowman, 2016). Being totally dependent upon the medical procedure may leave you feeling powerless, helpless, and prone to worry. In most cases there are things you can do to optimize self- healing.
- Think outside the box. Explore other forms of self-care that could enhance your healing. Initiate self-care action instead of waiting passively. By taking the initiative, you gain a sense of control, which tends to enhance your immune system and healing potential. Do anything that may be helpful, as long as it is not harmful. In my case, future medical options to resolve urinary retention could include additional medications or even surgery. Researching the medical literature, there were a number of studies showing that certain herbs in traditional Chinese medicine and Ayurveda medicine could help to reduce prostate inflammation and possibly promote healing. Thus, I began taking three different herbal substances for which there was documented scientific literature. I also was prescribed herbal tea to sooth the bladder. Additionally, I reduced my sugar and caffeine intake to lower the risk of bladder irritation and infection.
- Collaborate with your health care provider. Let your provider know the other approaches you are using. Report any interventions such as vitamins, herbs, Chinese medicine. Ask if they know of any harm that could occur. In most cases there is no harm. The health care professional may just think it is a waste of time and money. However, if you find it helpful, if it gives you control, if it makes you less anxious, and if it is not harmful, it may be beneficial. What do you have to lose?
- Assume that all the health care professionals are committed to improving your health to the best of their ability. Yet at times professionals are now so specialized that they focus only on their own discipline and not the whole person. In their quest to treat the specific problem, they may lose sight of other important aspects of care. Thus, hope for the best, but plan for the worst.
PREPARING FOR SURGERY
Assume that the clinical staff will predict a more positive outcome than that reported in the medical literature. In most cases, especially in the United States, there is no systematic follow-up data since many post-surgical complications are resolved at another location. In addition, many studies are funded by medical companies which have a vested interest and report only the positive outcomes. The companies tend not to investigate for negative side-affects, especially if the iatrogenic effects occur weeks, months, or years after the procedure. This has also been observed in the pharmaceutical companies sponsoring studies for new medications.
Generally, when independent researchers investigated medical procedures they found the complication rate three-fold higher than the medical staff reported. For example, for endoscopic procedures such colonoscopies, doctors reported only 31 complications from 6,383 outpatient upper endoscopies and 11,632 outpatient colonoscopies. The actual rate was 134 trips to the emergency room and 76 hospitalizations. This discrepancy occurred because the only incidents reported involved patients who went back to their own doctors. It did not capture those patients who sought help at other locations or hospitals (Leffler et al, 2010).
The data are even worse for patients who are hospitalized; in the U.S. 20% of patients who leave the hospital return within a month while in England, 7% of those leaving the hospital return within a month (Krumholz, 2013).
- Ask about possible complications that could arise, the symptoms, and what the physician would do if they occurred. Do not assume the health professional will have the time to explain or know all the possible complications. In my case when the surgeon removed the catheter at 4 pm during my second emergency room visit, I had to ask, “What would happen if I still cannot urinate?” Again, the emergency room was the only answer. However, I know now that he could have taught me simple self-catherization which would have eliminated the long waiting in the emergency room, the excessive stretching of the bladder and the subsequent emergency room medical error on my third visit to the ER. It would also have reduced the medical costs by a thousand-fold.
- Get a second opinion. In my case, the surgeon came highly recommended, is very experienced, and has done many hernia repairs. I trusted his judgement that I needed a bilateral hernia repair although I only felt the bulging in the right inguinal area and did not feel bulging or sensations in the left inguinal area. Despite my feeling of trust, I should have asked for a second independent opinion just to be sure. In many moments of despair when suffering the significant complications, I even started to wonder if the bilateral laparoscopic surgical repair was really necessary or just done to increase the income of the surgeon and the outpatient surgical facility in which he had a financial interest. My surgery resulted in large hematomas, irritation of internal organs, and possible damage to the GI track. This type of complication did not occur for a close friend who had a single-sided hernia repair by the same surgeon in a hospital where the surgeon had no financial interests.
- Request medical personnel who are highly experienced in the intervention. Mortality and complications rates are significantly lower for practitioners who have done the procedure at least 250 times.
- Don’t assume the worst but be prepared for the worst. Ask your health care provider about the various side effects of surgery, including the worst things that could happen, and then develop a pre-emptive plan.
The most common problems associated with surgery and general anesthesia include:
- Urinary retention. Following general anesthesia, neural enervation to the bladder and gastrointestinal tract are often affected. The general risk for postoperative urinary retention (POUR) for all types of surgeries ranges from 7% to 52% (Tammela et al, 1986; Petros et al, 1990; Petros et al, 1991; Gonullu et al, 1993; Tammela, 1995). For patients who have surgery for hernia repair 24.4% will experience postoperative urinary retention (Keita et al, 2005)—one in four. The risk for older males is even higher (Blair et al, 2017). Do not leave the medical unit until you have urinated or have a Foley catheter inserted with a leg bag and appropriate follow-up managed by a urologist. In my case, neither the surgeon nor the outpatient hospital checked to determine whether I could urinate—they just discharged me the moment I was conscious. Discharging a patient who has had general anesthesia without checking to determine whether they can urinate goes against all medical guidelines and standard hospital policies and constitutes malpractice. As this was my first surgery, I had no idea that urinary retention could occur. Thus, I did not recognize the symptoms nor did the advice nurse or the surgeon when called for advice before I checked into the emergency room.
- Expect constipation and plan to eat a high roughage diet that supports bowel movements. In case bowel function is slow in resuming, you may want to have on hand simple over-the-counter supplements such as magnesium capsules, psyllium husks, and aloe vera juice or gel, all available at any health food store. Liquid magnesium citrate (GoLytely® solution available at drug stores), can be useful, but tends to be a little stressful to take. Check these over-the-counter supplements with your provider to avoid supplement-drug interaction.
- Infection. Many patients pickup hospital-induced infections (nosocomial infections). In my case, I after four weeks with a Foley catheter, I got a mild bladder infection and had to control it with antibiotics. While in the hospital, avoid direct physical contact with other patients and staff, wash and rewash your hands. Remember medical staff tend are less attentive and wash their hands 10% less in the afternoons than in morning. Ask the medical staff to thoroughly wash their hands before they examine you. If you do get an infection, contact your medical provider immediately.
ACTION STEPS
- Pace yourself. Assume that recovery could be slower than promised. Although your body may appear to be healed, in many cases your vitality could be significantly reduced for a number of months, and you will probably feel much more fatigued in the evening. The recovery from general anesthesia has been compared to recovery from a head-on car collision.
- Identify your support system in case you cannot take care of yourself initially. Organize family and friends to help you. In my case, for the first two weeks I did not have the energy to do anything for myself—the overwhelming abdominal spasms and the three episodes in the ER had drained my energy. I was very lucky that I had my family and friends to help me. For the first few weeks I was so distracted by the pain and discomfort that I did not drive or take care of myself.
- Have a plan in case you need to go to the Emergency Room in the evening. Know its location and have someone who can take you.
- Assume that you will probably have an extensive wait in the ER unless you are desperately ill. Do not try to “tough it out.” Be totally honest about your level of pain, so you can get the best possible care. In my case, I had horrible abdominal pain and spasms with urinary retention, but still acted as if I were okay. When the admitting nurse asked me how I felt, I rated my discomfort as a 5 on a scale from 0 to 10. In my mind I compared the pain with that I had experienced after a skiing accident, which was much worse. What I had forgotten was that the ER is triage system, so I had to wait and wait and wait, which was phenomenally uncomfortable.
- In the ER, ask which medical specialist can follow up with you if further issues develop. A general hospital usually has specialists on call. In my case, if I had requested care from a specialist, I would have been treated directly by a urologist. I would not have had to follow the advice of the surgeon who said, “When you go to Emergency Room, have them empty the bladder and then go home.” Almost all urologists would have recommended keeping the Foley catheter in for a few days to allow the side effects of the anesthesia and the trauma caused by the bladder expansion to ameliorate and then test whether urination was possible.
- Have a medical advocate with you at all times who can observe that the procedures are done correctly. There is a four-fold increase in errors during the evenings and nights as compared to the morning. The more medical staff is multi-tasking, the more likely they will make errors. Have the medical personnel explain any procedure before they perform it—why and how they will do the procedure and what you will experience. You also need to know if they are experienced in that particular procedure? If the answers do not make sense, stop them and ask for another staff member.
- In the ER, record the instructions on your phone. Have medical staff explain and demonstrate to you and your support person what you will need to do at home. Then repeat the instructions back to them to be certain you have it right.
- Remind yourself that errors can occur. In my case, during the third ER visit for urinary retention, the nurse delayed the anchoring of the catheter and it had slipped down into the urethra. As she began to pump, I could feel my urethra tearing and I alerted her to stop. This was immediately followed by another procedural error on her part, so I had to again alert her to stop, which she finally did. All this occurred at 1 am in the morning. As the patient, I had to take charge at a time when I was totally exhausted. As the nurse retreated, I was left sitting on the gurney waiting for someone to come and follow-up. I waited and waited and when I finally stood up, the catheter dropped out and I began bleeding.
Lesson learned: hope for the best but prepare for the worst. In my situation, after eight weeks and numerous visits to the urologist, he removed the catheter. He did this at 8:30 in the morning. This way I could go home and in case something happened, I could go back to his office for further care. Before leaving the office, I planned for the worst. I asked what would happen if I could not urinate later in the evening and requested that he give me a few catheters, so if problems developed, I could catheterize myself.
The urologist gave me the catheters and explained how to use them, although I did not actually practice on myself. Still, I felt better prepared. During the day, I become more and more optimistic because I had no problems; however, at 2 am I woke up unable to urinate. For the next hour, I felt very anxious about inserting the catheter, since I had never done it myself. Finally, my discomfort overcame my anxiety. To my surprise, it was easy. After waiting a few minutes, I removed the catheter and went to bed feeling much more comfortable. The next morning after breakfast and a cup of coffee, I found that my body was working fine without the catheter.
Had I not planned for the worst, I would have once again gone to the Emergency Room and probably waited for hours, risking a repeat of tremendous discomfort and irritation. This simple planning reduced my medical cost more than a thousand-fold from $1700 for the emergency room to $2 for some single-use catheters.
References
Angell, M. (2009). Drug companies & doctors: A story of corruption. The New York Review of Books, 56(1), 8-12. http://www.nybooks.com/articles/2009/01/15/drug-companies-doctorsa-story-of-corruption/
Bishop, T.F., Federman, A.D., & Ross, J.S. (2010). Laboratory test ordering at physician offices with and without on-site laboratories, Journal of Gen Intern Med, 25(10)m 1057-1063. doi: 10.1007/s11606-010-1409-7
Blair, A.B., Dwarakanath, A., Mehta, A., Liang, H., Hui, X., Wyman, C., Ouanes, J.P.P., & Nguyen, H.T. (2017). Postoperative urinary retention after inguinal hernia repair: a single institution experience. Hernia, 21(6), 895-900.
Bowman, K. (2016). Diastasis Recti: The whole-body solution to abdominal weakness and separation. Propriometrics Press: Carlsborg, WA 98324
Davis, C., Naci, N., Gurpinar, E., Poplavska, E., Pinto, A., Aggarwal, A. (2017). Availability of evidence of benefits on overall survival and quality of life of cancer drugs approved by European Medicines Agency: retrospective cohort study of drug approvals 2009-13. BMJ, 2017; j4530 DOI: 10.1136/bmj.j4530
Ferguson, T. B. (2012). The Institute of Medicine Committee report “best care at lower cost: the path to continuously learning health care”. Circulation: Cardiovascular Quality and Outcomes, 5(6), e93-e94. http://jama.jamanetwork.com/article.aspx?articleid=185157
Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., & Fawcett, J. (2010). Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA, 303(1), 47-53.
Gönüllü, N. N., Gönüllü, M., Utkan, N. Z., Dülger, M., Gökgöz, S., & Karsli, B. (1993). Postoperative retention of urine in general surgical patients. The European journal of surgery= Acta chirurgica, 159(3), 145-147.
Horton, R. (2015). Offline: What is medicine’s 5 sigma? The Lancet, 385(9976), 1380. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2815%2960696-1/fulltext?rss%3Dyes
Institute of Medicine’s Infographic, accompanying their 2012 report, Best Care at Lower Cost, at http://www.iom.edu/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America/Infographic.aspx
Keita, H., Diouf, E., Tubach, F., Brouwer, T., Dahmani, S., Mantz, J., & Desmonts, J. M. (2005). Predictive factors of early postoperative urinary retention in the postanesthesia care unit. Anesthesia & Analgesia, 101(2), 592-596.
Kim, C. & Prasad, V. (2015). Cancer drugs approved on the basis of a surrogate end point and subsequent overall survival-An analysis of 5 Years of US Food and Drug Administration approvals. JAMA Intern Med,175(12):1992-1994. doi:10.1001/jamainternmed.2015.5868
Kirsch, I. (2014). The emperor’s new drugs: medication and placebo in the treatment of depression. In Placebo (pp. 291-303). Springer Berlin Heidelberg.
Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (2000). To err is human: building a safer health system (Vol. 6). National Academies Press. http://www.ncbi.nlm.nih.gov/books/NBK221671/
Krumholz, H. M. (2013). Post-hospital syndrome—an acquired, transient condition of generalized risk. New England Journal of Medicine, 368(2), 100-102. http://www.nejm.org/doi/full/10.1056/NEJMp1212324
Leffler, D.A, Kheraj, R., Garud, S., Neeman, N., Nathanson, L.A., Kelly, C.P., Sawhney, M., Landon, B., Doyle, R., Rosenberg, S., & Aronson, M. (2010). The incidence and cost of unexpected hospital use after scheduled outpatient endoscopy. Arch Intern Medicine, 170(19), 1752-1757. http://archinte.jamanetwork.com/article.aspx?articleid=226125
Makary, M.A. & Daniel, M. (2016). Medical error–the third leading cause of death in the US. British Medical Journal, 353:i2139
Neumayer, L., Giobbie-Hurder, A., Jonasson, O., Fitzgibbons Jr, R., Dunlop, D., Gibbs, J., & Henderson, W. (2004). Open mesh versus laparoscopic mesh repair of inguinal hernia. New England Journal of Medicine, 350(18), 1819-1827. http://academicdepartments.musc.edu/surgery/education/resident_info/journal_club/09-10/April-inguinal.pdf
Palmer, W. L., Bottle, A., & Aylin, P. (2015). Association between day of delivery and obstetric outcomes: observational study. BMJ, 351, h5774. http://www.bmj.com/content/bmj/351/bmj.h5774.full.pdf
Peper, E. & Harvey, R. (2017). The fallacy of the placebo controlled clinical trials: Are positive outcomes the result indirect treatment side effects? NeuroRegulation. 4(3–4):102–113 2017 doi:10.15540/nr.4.3-4.102
Perugini, R. A., & Callery, M. P. (2001). Complications of laparoscopic surgery. http://www.ncbi.nlm.nih.gov/books/NBK6923/?report=reader
Petros, J. G., & Bradley, T. M. (1990). Factors influencing postoperative urinary retention in patients undergoing surgery for benign anorectal disease. The American Journal of Surgery, 159(4), 374-376.
Petros, J. G., Rimm, E. B., Robillard, R. J., & Argy, O. (1991). Factors influencing postoperative urinary retention in patients undergoing elective inguinal herniorrhaphy. The American Journal of Surgery, 161(4), 431-433.
Phillips, D. P., & Barker, G. E. (2010). A July spike in fatal medication errors: a possible effect of new medical residents. Journal of General Internal Medicine, 25(8), 774-779. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2896592/
Pink, D.H. (2018). When: The Scientific Secrets of Perfect Timing. New York: Riverhead Books, ISBN-13: 978-0735210622
Robins, E.D. (1984). Matter of Life & Death: Risks vs. Benefits of Medical Care. New York: W.H. Freeman and Company.
Sauerland, S., Walgenbach, M., Habermalz, B., Seiler, C. M., & Miserez, M. (2011). Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. The Cochrane Library.
Tammela, T. (1994). Postoperative urinary retention–why the patient cannot void. Scandinavian Journal of Urology and Nephrology. Supplementum, 175, 75-77.
Tammela, T., Kontturi, M., & Lukkarinen, O. (1986). Postoperative urinary retention: I. Incidence and predisposing factors. Scandinavian Journal of Urology and Nephrology. 20(3), 197-201.
Vigneswaran, Y., Gitelis, M., Lapin, B., Denham, W., Linn, J., Carbray, J., & Ujiki, M. (2015). Elderly and octogenarian cohort: Comparable outcomes with nonelderly cohort after open or laparoscopic inguinal hernia repairs. Surgery, 158(4), 1137-1144.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. BMJ: British Medical Journal, 320(7237), 774. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117772/
Wright, M.D., Philips-Bute, B., Mark, J.B., Stafford-Smith, M., Grichnik, K.P., Andregg, B.C., & Taekman, J.M. (2006). Time of day effects on the incidence of anesthetic adverse events. Quality and Safety in Health Care. 15(4): 258–263.doi: 10.1136/qshc.2005.017566
Young, J. Q., Ranji, S. R., Wachter, R. M., Lee, C. M., Niehaus, B., & Auerbach, A. D. (2011). “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. Annals of Internal Medicine, 155(5), 309-315. http://www.girardslaw.com/library/July_Effect_Annals_of_Internal_Medicine.pdf
[1] I think my family, friends and colleagues (Karen Peper, Norihiro Muramatsu, Richard Harvey, David Wise, Annette Booiman, Lance Nagel and many others) who generously supported me during this journey.