Reduce Interpersonal Stress*
Posted: December 4, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, Exercise/movement, healing, health, meditation, mindfulness, Pain/discomfort, stress management | Tags: health, mental-health, nutrition, wellness 2 CommentsAdapted from: Peper, E. & Harvey, R. Adjunctive techniques to reduce interpersonal stress at home. Biofeedback. 53(3), 54-57. https://rdcu.be/eMJqt

Stress often triggers defensive reactions—manifesting as anger, frustration, or anxiety that may mirror fight-or-flight responses. These reactions can reduce rational thinking, increase long-term health risks, and contribute to psychological and physiological disorders. and complicate the management of specific symptoms. Outlined are some pragmatic techniques that can be implemented during the day to interrupt and reduce stress.
After we had been living in our house for a few years, a new neighbor moved in next door. Within months, she accused us of moving things in her yard, blamed us when there was a leak in her house, claimed we were blowing leaves from her property onto other neighbors’ properties, and even screamed at her tenants to the extent that the police were called numerous times. Just looking at her house through the window was enough to make my shoulders tighten and leave me feeling upset.
When I drove home and saw her standing in front of her house, I would drive around the block one more time to avoid her while . . . feeling my body contract. Often, when I woke up in the morning, I would already anticipate conflict with my neighbor. I would share stories of my disturbing neighbor and her antics with my friends. They were very supportive and agreed with me that she was crazy. However, the acknowledgment and validation from my friends did not resolve my anger or indignation or the anxiety that was triggered whenever I saw my neighbor or thought of her. I spent far too much time anticipating and thinking about her, which resulted in tension in my own body—my heart rate would increase, and my neck and shoulders would tighten.
I decided to change. I knew I could not change her; however, I could change my reactivity and perspective. Thus, I practiced a “pause and recenter” technique. At the first moment of awareness that I was thinking about her or her actions, I would change my posture by sitting up straight, begin looking upward, breathe lower and slower, and then, in my mind’s eye, send a thought of goodwill streaming to her like an ocean wave flowing through and around her in the distance. I chose to do this series of steps because I believe that within every person, no matter how crazy or cruel, there is a part that is good, and it is that part I want to support.
I repeated this pause and recenter technique many times, especially whenever I looked in the direction of her house or saw her in her yard. I also reframed and reappraised her aggressive, negative behavior as her way of coping with her own demons. Three months later, I no longer reacted defensively. When I see her, I can say hello and discuss the weather without triggering my defensive reaction. I feel so much more at peace living where I am.
When stressed, angry, rejected, frustrated, or hurt, we so often blame the other person (Leary, 2015). The moment we think about that person or event, our anger, indignation, resentment, and frustration are triggered. We keep rehashing what happened. As we relive the experiences in our mind, we are unaware that we are also reliving bodily reactions to past events.
We are often unaware of the harm we are doing to ourselves until we experience physical symptoms such as high blood pressure, gastrointestinal distress, and muscle tightness along with behavioral and psychological symptoms such as insomnia, anxiety, or depression (Carney et al., 2006; Gerin et al., 2012). As we think of past events or interact again with a person involved in those past events, our body automatically responds with a defense reaction as if we were being threatened again in the present moment.
This defense reaction to memory of past threats from a “crazy” neighbor activates our fight-or-flight responses and increases sympathetic activation so that we can run faster and fight more ferociously to survive; however, this reaction also reduces blood flow through the frontal cortex—a process that reduces our ability to think rationally (van Dinther et al., 2024; Willeumier, et al., 2011). When we become so upset and stressed that our mind is captured by the other person, this reaction contributes to symptoms of chronic stress such as an increase in hypertension, myofascial pain, depression, insomnia, cardiovascular disease, and other chronic disorders (Duan et al., 2022; Russell et al., 2015; Suls, 2013).
Sharing our frustrations with friends and others is normal. It feels good to blame people for their personal limitations or mental illness; however, over time, blaming others avoids building adaptive capacity in strengthening skills that reduce chronic stress reactions (Fast & Tiedens, 2010; Lou et al., 2023). The time spent rehashing and justifying our feelings diminishes the time we spend in the present moment and our focus on upcoming opportunities.
In the moment of an encounter with a difficult neighbor, we may not realize that we have a choice. Some people keep living and reacting to past hurts or losses perpetually. Some people can learn to let go and/or forgive and make space in favor of considering new opportunities for learning and growth. Although the choice is ours, it is often very challenging to implement—even with the best intentions—because we react automatically when reminded of past hurts (seeing that person, anticipating meeting or actually meeting that person who caused the hurt, or being triggered by other events that evoke memories of the pain).
What Can You Do
Choose to change your response. Choose to reduce reactivity. Choosing adaptive reactions does not mean you condone what happened or agree that the other person was right. You are just choosing to live your life and not continue to be captured by nor react to the previous triggers. Many people report that after implementing some of the practices described below along with many other stress management techniques, their automatic reactivity was noticeably decreased. They report that their chronic stress symptoms were reduced and they have the freedom to live in present instead of being captured by the painful past.
Pause and Recenter by Sending Goodwill
Our automatic reaction to the trigger elicits a defense reaction that reduces our ability to think rationally. Therefore, the moment you anticipate or begin to react, take three very slow diaphragmatic breaths, inhaling for approximately 4–5 seconds and exhaling for about 5–6 seconds, where one in-and-out breath takes about 10 seconds to complete. As you inhale, allow your abdomen to expand; then as you exhale, slowly make yourself tall and look up. Looking up allows easier access to empowering and positive memories (Peper et al., 2017).
Continue looking up, inhaling slowly to allow the abdomen to expand. Repeat this slow breath again. On the third long, slow breath, while looking up, evoke a memory of someone in whose presence you felt at peace and who loves you, such as your grandmother, aunt, uncle, or even a pet. Reawaken positive feelings associated with memories of being loved. Allow a smile inwardly or outwardly and soften your eyes as you experience the loving memory.
Next, put your hands on your chest, take another long slow breath as your abdomen expands, and as you exhale bring your hands away from your chest and stretch them out in front of you. At the same time in your mind’s eye, imagine sending goodwill to that person involved in the interpersonal conflict that previously evoked your stress response. As if you are sending an ocean wave that is streaming outward to the person.
As you do the pause and recenter technique, remember you are not condoning what happened; instead, you are sending goodwill to that person’s positive aspect. From this perspective, everyone has an intrinsic component—however small—that some label as the individual’s human potential, Christ nature or Buddha nature.
Why would this be effective? This practice short-circuits the automatic stress response and provides time to recenter, interrupting ongoing rumination by shifting the mind away from thoughts about the person or event that induced stress toward a positive memory. By evoking a loving memory from the past, we facilitate a reduction in arousal, evoke a positive mood, and decrease sympathetic nervous system activation (Speer & Delgado, 2017). Slower diaphragmatic breathing also reduces sympathetic activation (Birdee et al., 2023; Siedlecki et al., 2022). By combining body-centered and mind-centered techniques, we can pause and create the opportunity to respond positively rather than reacting with anger and hurt.
Practice Sending Goodwill the Moment You Wake Up
So often when we wake up, we anticipate the challenges, and even the prospect of interacting with a person or event heightens our defense reaction. Therefore, as soon as you wake up, sit at the edge of the bed, repeat the previous practice, pause, and center. Then, as you sit at the edge of the bed, slightly smile with soft eyes, look up, and inhale as your abdomen expands. Then, stamp a foot into the floor while saying, “Today is a new day.” Next, inhale, allowing your abdomen to expand; as you look up, stamp the opposite foot on the floor while saying, “Today is a new day.” Finally, send goodwill to the person who previously triggered your defensive reaction.
Why would this be effective? Looking up makes it easier to access positive memories and thoughts. Stamping your foot on the ground is a nonverbal expression of determination and anchors the thought of a new day, thereby focusing on new opportunities (Feldman, 2022).
Interrupt the Stress Response with the ABCs
The moment you notice discomfort, pain, stress, or negative thoughts, interrupt the cycle with a simple ABC strategy (Peper, 2025):
- Adjust posture and look up
- Breathe by allowing your abdomen to relax and expand while inhaling
- Change your internal dialogue, smile and focus on what you want to do
Why would this be effective? By shifting your posture and gently looking upward, you make it easier to access positive and empowering memories and thoughts (Peper et al., 2019). This simple change in body position can interrupt habitual stress responses and open the doorway to more constructive states.
Slow, diaphragmatic breathing further supports this process by reducing sympathetic arousal and restoring a sense of calm. As your breathing deepens, clarity of mind increases, allowing you to respond rather than react (Peper et al, 2024b; Matto et al, 2025).
Equally important is transforming critical, judgmental, or negative self-talk into affirmative, supportive statements. Describe what you want to do—rather than what you want to avoid. This reframing creates a clear internal guide and significantly increases the likelihood that you will achieve your desired goals.
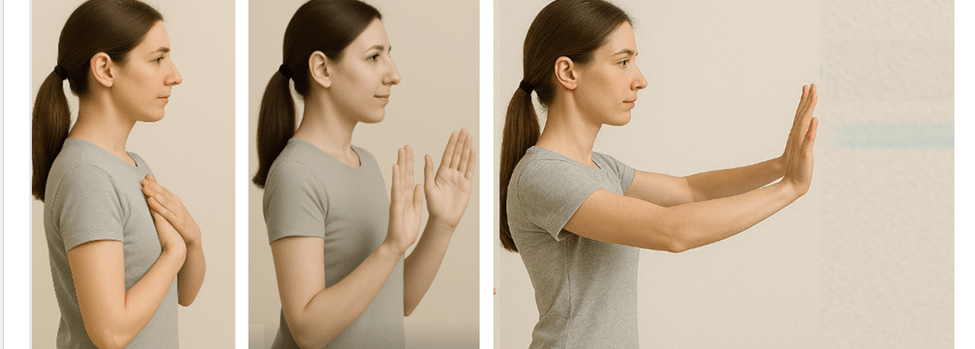
Complete the Alarm Reaction a Burst of Physical Activity
When you feel overwhelmed and fully captured by a stress reaction, one of the most effective strategies is to complete the fight-flight response with a brief burst of intense physical activity. This momentary action such as running in place, vigorously shaking your arms, or doing a few rapid push-offs from a wall (Peper et al., 2024a). After completing the physical activity implement your stress management strategies such as breathing, cognitive reframing, meditation, etc.
Why would this be effective? The intense physical activity discharges the excessive physiological arousal and interrupts the cycle of rumination. For practical examples and step-by-step guidance, see the article Quick Rescue Techniques When Stressed (Peper et al., 2024a) or the accompanying blog post: https://peperperspective.com/2024/02/04/quick-rescue-techniques-when-stressed/
Discuss Your Issue from the Third-Person Perspective
When thinking, ruminating, talking, texting, or writing about the event, discuss it from the third-person perspective. Replace the first-person pronoun “I” with “she” or “he.” For example, instead of saying “I was really pissed off when my boss criticized my work without giving any positive suggestions for improvement,” say “He was really pissed off when his boss criticized his work without offering any positive suggestions for improvement.”
Why would this be effective? The act of substituting the third-person pronoun for the first-person pronoun interrupts our automatic reactivity because it requires us to observe and change our language, which activates parts of the frontal cortex. This third-person/first-person process creates a psychological distance from our feelings, allowing for a more objective and calmer perspective on the situation, effectively reducing stress by stepping back from the immediate emotional response (Moser et al., 2017). This process can be interpreted as meaning that you are no longer fully captured by the emotions, as you are simultaneously the observer of your own inner language and speech.
Compare Yourself with Others Who are less Fortunate
When you feel sorry for yourself or hurt, take a breath, look upward, and compare yourself with others who are suffering much more. In that moment, consider yourself incredibly lucky compared with people enduring extreme poverty, bombings, or severe disfigurement. Be grateful for what you have.
Why would this be effective? Research shows that when we compare ourselves with people who are more successful, we tend to feel worse—especially when we have low self-esteem. However, when we compare ourselves with others who are suffering more, we tend to feel better (Aspinwall, & Taylor, 1993). This comparison relativizes our perspective on suffering, making our own hardships and suffering seem less significant compared with the severe suffering of others.
Conclusion
It is much easier to write and talk about these practices than to implement them. Reminding yourself to implement them can be very challenging. It requires significant effort and commitment. In some cases, the benefits are not experienced immediately; however, when practiced many times during the day for six to eight weeks, many people report feeling less resentment and experience a reduction in symptoms and improvements in health and relationships.
*This blog was inspired by the podcast “No Hard Feelings,” an episode on Hidden Brain produced by Shankar Vedantam (2025) that featured psychologist Fred Luskin, and the wisdom taught by Dora Kunz (Kunz & Peper, 1983, 1984a, 1984b, 1987).
See the following posts for more relevant information
References
Aspinwall, L. G., & Taylor, S. E. (1993). Effects of social comparison direction, threat, and self-esteem on affect, self-evaluation, and expected success. Journal of Personality and Social Psychology, 64(5), 708–722. https://doi.org/10.1037/0022-3514.64.5.708
Birdee, G., Nelson, K.,Wallston, K., Nian, H., Diedrich, A., Paranjape, S., Abraham, R., & Gamboa, A. (2023). Slow breathing for reducing stress: The effect of extending exhale. Complementary Therapies in Medicine, 73. https://doi.org/10.1016/j.ctim.2023.102937
Carney, C. E., Edinger, J. D., Meyer, B., Lindman, L., & Istre, T. (2006). Symptom-focused rumination and sleep disturbance. Behavioral Sleep Medicine, 4(4), 228–241. https://doi.org/10.1207/s15402010bsm0404_3
Defayette, A. B., Esposito-Smythers, C., Cero, I., Harris, K. M.,Whitmyre, E. D., & López, R. (2023). Interpersonal stress and proinflammatory activity in emerging adults with a history of suicide risk: A pilot study. Journal of Mood and Anxiety Disorders, 2. https://doi.org/10.1016/j.xjmad.2023.100016
Dienstbier, R. A. (1989). Arousal and physiological toughness: Implications for mental and physical health. Psychological Review, 96(1), 84. https://doi.org/10.1037/0033-95x.96.1.84
Duan, S., Lawrence, A., Valmaggia, L., Moll, J., & Zahn, R. (2022). Maladaptive blame-related action tendencies are associated with vulnerability to major depressive disorder. Journal of Psychiatric Research, 145, 70–76. https://doi.org/10.1016/j.jpsychires.2021.11.043
Fast, N. J., & Tiedens, L. Z. (2010). Blame contagion: The automatic transmission of self-serving attributions. Journal of Experimental Social Psychology, 46(1), 97–106. https://doi.org/10.1016/j.jesp.2009.10.007
Feldman, Y. (2022). The dialogical dance–A relational embodied approach to supervision. In C. Butte & T. Colbert (Eds.), Embodied approaches to supervision: The listening body (chap. 2). Routledge. https://www.amazon.com/Embodied-Approaches-Supervision-C%C3%A9line-Butt%C3%A9/dp/0367473348
Gerin,W., Zawadzki,M. J., Brosschot, J. F., Thayer, J. F., Christenfeld, N. J., Campbell, T. S., & Smyth, J. M. (2012). Rumination as a mediator of chronic stress effects on hypertension: A causal model. International Journal of Hypertension, 2012, 453465. https://doi.org/10.1155/2012/453465
Hase, A., O’Brien, J., Moore, L. J., & Freeman, P. (2019). The relationship between challenge and threat states and performance: A systematic review. Sport, Exercise, and Performance Psychology, 8(2), 123. https://doi.org/10.1037/spy0000132
Hassamal, S. (2023). Chronic stress, neuroinflammation, and depression: An overview of pathophysiological mechanisms and emerging anti-inflammatories. Frontiers in Psychiatry,
14, 1130989. https://doi.org/10.3389/fpsyt.2023.1130989
Kunz, D., & Peper, E. (1983). Fields and their clinical implications—Part III: Anger and how it affects human interactions. The American Theosophist, 71(6), 199–203. https://www.researchgate.net/publication/280777019_Fields_and_their_clinical_implications-Part_III_Anger_and_how_it_affects_human_interactions
Kunz, D., & Peper, E. (1984a). Fields and their clinical implications IV: Depression from the energetic perspective: Etiological underpinnings. The American Theosophist, 72(8), 268–275. https://www.researchgate.net/publication/280884054_Fields_and_their_clinical_implications_Part_IV_Depression_from_the_energetic_perspective-Etiological_underpinnings
Kunz, D., & Peper, E. (1984b). Fields and their clinical implications V: Depression from the energetic perspective: Treatment strategies. The American Theosophist, 72(9), 299–306. https://www.researchgate.net/publication/280884158_Fields_and_their_clinical_implications_Part_V_Depression_from_the_energetic_perspective-Treatment_strategies
Kunz, D., & Peper, E. (1987). Resentment: A poisonous undercurrent. The Theosophical Research Journal, IV(3), 54–59. Also in: Cooperative Connection, IX(1), 1–5. https://www.researchgate.net/publication/387030905_Resentment_Continued_from_page_4
Leary, M. R. (2015). Emotional responses to interpersonal rejection. Dialogues in Clinical Neuroscience, 17(4), 435–441. https://doi.org/10.31887/DCNS.2015.17.4/mleary
Lou, Y., Wang, T., Li, H., Hu, T. Y., & Xie, X. (2023). Blame others but hurt yourself: Blaming or sympathetic attitudes toward victims of COVID-19 and how it alters one’s health status. Psychology & Health, 39(13), 1877–1898. https://doi.org/10.1080/08870446.2023.2269400
Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
Moser, J. S., Dougherty, A., Mattson, W. I., Katz, B., Moran, T. P.,Guevarra, D., Shablack, H.,Ayduk,O., Jonides, J., Berman, M. G., & Kross, E. (2017). Third-person self-talk facilitates emotion regulation without engaging cognitive control: Converging evidence from ERP and fMRI. Scientific Reports, 7(1), 4519. https://doi.org/10.1038/s41598-017-04047-3
Peper, E. (2025). Breathe Away Menstrual Pain- A Simple Practice That Brings Relief. the peper perspective-ideas on illness, health and well-being from Erik Peper. https://peperperspective.com/2025/11/22/6825/
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3), 153-169. https://doi.org/10.15540/nr.6.3.1533-1
Peper, E., Lin, I.-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024b). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Russell, M. A., Smith, T. W., & Smyth, J. M. (2015). Anger expression, momentary anger, and symptom severity in patients with chronic disease. Annals of Behavioral Medicine, 50(2), 259–271. https://doi.org/10.1007/s12160-015-9747-7
Siedlecki, P., Ivanova, T. D., Shoemaker, J. K., & Garland, S. J. (2022). The effects of slow breathing on postural muscles during standing perturbations in young adults. Experimental Brain Research, 240, 2623–2631. https://doi.org/10.1007/s00221-022-06437-0
Speer, M. E., & Delgado, M. R. (2017). Reminiscing about positive memories buffers acute stress responses. Nature Human Behaviour, 1, 0093. https://doi.org/10.1038/s41562-017-0093
Suls, J. (2013). Anger and the heart: Perspectives on cardiac risk, mechanisms and interventions. Progress in Cardiovascular Diseases, 55(6), 538–547. https://doi.org/10.1016/j.pcad.2013.03.002
van Dinther, M., Hooghiemstra, A. M., Bron, E. E., Versteeg, A., et al. (2024). Lower cerebral blood flow predicts cognitive decline in patients with vascular cognitive impairment. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 20(1), 136–144. https://doi.org/10.1002/alz.13408
Vedantam, S. (2025). No hard feelings. Hidden brain. Accessed February 5, 2025. https://hiddenbrain.org/podcast/no-hard-feelings/
Willeumier, K., Taylor, D. V., & Amen, D. G. (2011). Decreased cerebral blood flow in the limbic and prefrontal cortex using SPECT imaging in a cohort of completed suicides. Translational Psychiatry, 1(8), e28. https://doi.org/10.1038/tp.2011.28
Zannas, A. S., & West, A. E. (2014). Epigenetics and the regulation of stress vulnerability and resilience. Neuroscience, 264, 157–170. https://doi.org/10.1016/j.neuroscience.2013.12.003
Exploring the pain-brain-breathing connection
Posted: August 30, 2025 Filed under: attention, behavior, Breathing/respiration, cognitive behavior therapy, education, emotions, healing, meditation, Pain/discomfort, placebo, self-healing, Uncategorized | Tags: deliberate harm Leave a commentIf you’re curious about how the mind and body interplay in shaping pain—or looking for real, actionable techniques grounded in research listen to this episode of the Heart Rate Variability Podcast, Matt Bennett interviews Dr. Erik Peper about his article and blogpost Pain – There Is Hope. The conversation takes listeners beyond the common perception of pain as merely a physical response. It is a balanced mix of scientific depth and real-life applications, especially valuable for anyone interested in self-healing, holistic health, or understanding mind-body medicine. Moreover, it explains how pain is shaped by posture, breathing, mindset, and emotional context. Finally, it provides practical strategies to shift the pain experience, offering an uplifting and science-backed blend of understanding and hope.
If you find this helpful, let me know! And feel free to share it with friends and post it on your social channels so more people can benefit.
Blogs that complement this interview
If you want to explore further, check out the companion blog posts I hve created to expand on the themes from this discussion. These blogs highlight practical strategies, scientific insights, and everyday applications.
Use the power of your mind to transform health and aging
Posted: February 18, 2025 Filed under: attention, behavior, cancer, CBT, cognitive behavior therapy, COVID, education, health, meditation, mindfulness, Pain/discomfort, placebo, stress management, Uncategorized | Tags: health, imimune function, longevity, mental-health, mind-body, nutrition, Reframing, wellness Leave a commentMost of the time when I drive or commute by BART, I listen to podcasts (e.g., Freakonomics, Hidden Brain, this podcast will kill you, Science VS, Huberman Lab). although many of the podcasts are highly informative; , rarely do I think that everyone could benefit from it. The recent podcast, Using your mind to control your health and longevity, is an exception. In this podcast, neuroscientist Andrew Huberman interviews Professor Ellen Langer. Although it is three hours and twenty-two minute long, every minute is worth it (just skip the advertisements by Huberman which interrupts the flow). Dr. Langer delves into how our thoughts, perceptions, and mindfulness practices can profoundly influence our physical well-being.
She presents compelling evidence that our mental states are intricately linked to our physical health. She discusses how our perceptions of time and control can significantly impact healing rates, hormonal balance, immune function, and overall longevity. By reframing our understanding of mindfulness—not merely as a meditative practice but as an active, moment-to-moment engagement with our environment—we can harness our mental faculties to foster better health outcomes. The episode also highlights practical applications of Dr. Langer’s research, offering insights into how adopting a mindful approach to daily life can lead to remarkable health benefits. By noticing new things and embracing uncertainty, individuals can break free from mindless routines, reduce stress, and enhance their overall quality of life. This podcast is a must-listen for anyone interested in the profound connection between mind and body. It provides valuable tools and perspectives for those seeking to take an active role in their health and well-being through the power of mindful thinking. It will change your perspective and improve your health. Listen to or watch the interview:
Youtube: https://www.youtube.com/watch?v=QYAgf_lfio4

Useful blogs to reduce stress
Compassionate Presence: Covert Training Invites Subtle Energies Insights
Posted: January 20, 2025 Filed under: attention, healing, meditation, mindfulness, relaxation, Uncategorized | Tags: being safe, compassion, energy, Energy healing, healing, reiki, spirituality, therapeutic touch Leave a commentAdapted from: Peper, E. (2015). Compassionate Presence: Covert Training Invites Subtle Energies Insights. Subtle Energies Magazine, 26(2), 22-25. https://www.researchgate.net/publication/283123475_Compassionate_Presence_Covert_Training_Invites_Subtle_Energies_Insights
“Healing is best accomplished when art and science are conjoined, when body and spirit are probed together. Only when doctors can brood for the fate of a fellow human afflicted with fear and pain do they engage the unique individuality of a particular human being…a doctor thereby gains courage to deal with the pervasive uncertainties for which technical skill alone is inadequate. Patient and doctor then enter into a partnership as equals.
I return to my central thesis. Our health care system is breaking down because the medical profession has been shifting its focus away from healing, which begins with listening to the patient. The reasons for this shift include a romance with mindless technology.” Bernard Lown, MD, The Lost art of healing: Practicing Compassion in Medicine (1999)

Therapeutic Touch healing by Dora Kunz.
I wanted to study with the healer and she instructed me to sit and observe, nothing more. She did not explain what she was doing, and provided no further instructions. Just observe. I did not understand. Yet, I continued to observe because she knew something, she did something that seemed to be associated with improvement and healing of many patients. A few showed remarkable improvement – at times it seemed miraculous. I felt drawn to understand. It was an unique opportunity and I was prepared to follow her guidance.
The healer was remarkable. When she put her hands on the patient, I could see the patient’s defenses melt. At that moment, the patient seemed to feel safe, cared for, and totally nurtured. The patient felt accepted for just who she was and all the shame about the disease and past actions appeared to melt away. The healer continued to move her hands here and there and, every so often, she spoke to the client. Tears and slight sobbing erupted from the client. Then, the client became very peaceful and quiet. Eventually, the session was finished and the client expressed gratitude to the healer and reported that her lower back pain and the constriction around her heart had been released, as if a weight had been taken from her body.
How was this possible? I had so many questions to ask the healer: “What were you doing? What did you feel in your hands? What did you think? What did you say so softly to the client?”
Yet she did not help me understand how I could do this. The main instruction the healer kept giving me was to observe. Yes, she did teach me to be aware of the energy fields around the person and taught me how I could practice therapeutic touch (Kreiger, 1979; Peper, 1986; Kunz & Peper,1995; Kunz & Krieger, 2004; Denison, 2004; van Gelder & Chesley, F, 2015). But she was doing much more and I longed to understand more about the process.
Sitting at the foot of the healer, observing for months, I often felt frustrated as she continued to insist that I just observe. How could I ever learn from this healer if she did not explain what I should do! Does the learning occur by activating my mirror neurons (Acharya & Shukla, 2012).? Similar instructions are common in spiritual healing and martial arts traditions – the guru or mentor usually tells an apprentice to observe and be there. But how can one gain healing skills or spiritual healing abilities if you are only allowed to observe the process? Shouldn’t the healer be demonstrating actual practices and teaching skills?
After many sessions, I finally realized that the healer’s instruction to to learn was to observe and observe. I began to learn how to be present without judging, to be present with compassion, to be present with total awareness in all senses, and to be present without frustration. The many hours at the foot of this master were not just wasted time. It eventually became clear that those hours of observation were important training and screening strategies used to insure that only those students who were motivated enough to master the discipline of non-judgmental observation, the discipline to be present and open to any experience, would continue to participate in the training process. I finally understood. I was being taught a subtle energies skill of compassionate, and mindful awareness. Once I, the apprentice, achieved this state, I was ready to begin work with clients and master technical aspects of the healing practice – but not before.
A major component of the healing skill that relies on subtle energies is the ability to be totally present with the client without judgment (Peper, Gibney & Wilson, 2005). To be peaceful, caring, and present seems to create an energetic ambiance that sets stage, creates the space, for more subtle aspects of the healing interaction. This energetic ambiance is similar to feeling the love of a grandparent: feeling total acceptance from someone who just knows you are a remarkable human being. In the presence of a healer with such a compassionate presence, you feel safe, accepted, and engaged in a timeless state of mind, a state that promotes healing and regeneration as it dissolves long held defensiveness and fear-based habits of holding others at bay. This state of mind provides an opportunity for worries and unsettled emotions to dissipate. Feeling safe, accepted, and experiencing compassionate love supports the bological processes that nurture regeneration and growth.
How different this is from the more common experience with health care/medical practitioners who have little time to listen and to be with a patient. We might experience a medical provider as someone who sees us only as an illness (the cancer patient, the asthma patient) instead of recognizing us as a human spirit who happens to have an illness ( a person with cancer or asthma). At times we can feel as though we are seen only as a series of numbers in a medical chart – yet we know we are more than that. People long to be seen. Often the medical provider interrupts with unrelated questions instead of listening. It becomes clear that the computerized medical record is more important than the human being seated there. We can feel more fragmented, less safe, when we are not heard, not understood.
As one 23 year old student reported after being diagnosed with a serious medical condition,”/ cried immediately upon leaving the physician’s office. Even though he is an expert on the subject, I felt like I had no psychological support. I was on Gabapentin, and it made me very depressed. I thought to myself: Is my life, as I know it, over?” (Peper, Martinez Aranda, P., & Moss, 2015).
The healing connection is often blocked, the absence of a human connection is so obvious. The medical provider may be unaware of the effect of their rushed behavior and lack of presence. They can issue a diagnosis based on the scientific data without recognizing the emotional impact on the person receiving it.
What is missing is compassion and caring for the patient. Sitting at the foot of the master healer is not wasted time when the apprentice learns how to genuinely attend to another with non-judgmental, compassionate presence. However, this requires substantial personal work. Possibly all healthcare providers should be required, or at least invited, to learn how to attain the state of mind that can enhance healing. Perhaps the practice of medicine could change if, as Bernard Lown wrote, the focus were once again on healing, “…which begins with listening to the patient.”
References
Acharya, S., & Shukla, S. (2012). Mirror neurons: Enigma of the metaphysical modular brain. Journal of natural science, biology, and medicine, 3(2), 118–124. https://doi.org/10.4103/0976-9668.101878
Denison, B. (2004). Touch the pain away: New research on therapeutic touch and persons with fibromyalgia syndrome. Holistic nursing practice, 18(3), 142-151. https://doi.org/10.1097/00004650-200405000-00006
Krieger, D. (1979). The therapeutic touch: How to use your hands to help or to heal. Vol. 15. Englewood Cliffs, NJ: Prentice-Hall. https://www.amazon.com/Therapeutic-Touch-Your-Hands-Help/dp/067176537X
Kunz, D. & Krieger, D. (2004). The spiritual dimension of therapeutic touch. Rochester, VT: Inner Traditions/Bear & Co. https://www.amazon.com/Spiritual-Dimension-Therapeutic-Touch/dp/1591430259/
Kunz, D., & Peper, E. (1995). Fields and their clinical implications. In Kunz, D. Spiritual Aspects of the Healing Arts. Wheaton, ILL: Theosophical Pub House, 213-222. https://www.amazon.com/Spiritual-Aspects-Healing-Arts-Quest/dp/0835606015
Lown, B. (1999). The lost art of healing: Practicing compassion in medicine. New York, NY: Ballantine Books. https://www.amazon.com/Lost-Art-Healing-Practicing-Compassion/dp/0345425979
Peper, E. (1986). You are whole through touch: An energetic approach to give support to a breast cancer patient. Cooperative Connection. VII (3), 1-6. Also in: (1986/87). You are whole through touch: Dora Kunz and Therapeutic Touch. Somatics. VI (1), 14-19. https://www.researchgate.net/publication/280884245_You_are_whole_through_touch_Dora_Kunz_and_therapeutic_touch
Peper, E. (2024). Reflections on Dora and the Healing Process, webinar presented to the Therapeutic Touch International Association, Saturday, December 14, 2024. https://youtu.be/skq9Chn-eME?si=HJNAhiUsgXSkqd_5
Peper, E., Gibney, K. H. & Wilson, V. E. (2005). Enhancing Therapeutic Success–Some Observations from Mr. Kawakami: Yogi, Teacher, Mentor and Healer. Somatics. XIV (4), 18-21. https://biofeedbackhealth.org/wp-content/uploads/2011/01/edited-enhancing-therapeutic-success-8-23-05.pdf
Peper, E., Martinez Aranda, P., & Moss, E. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback, 43(2), 103-109. https://doi.org/10.5298/1081-5937-43.2.04
Van Gelder, K & Chesley, F. (2015). A Most Unusual Life. Wheaton Ill: Theosophical Publishing House. https://www.amazon.com/Most-Unusual-Life-Clairvoyant-Theosophist/dp/0835609367
[1] I thank Peter Parks for his superb editorial support.
Pragmatic techniques for monitoring and coaching breathing
Posted: December 14, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, emotions, meditation, mindfulness, neurofeedback, Pain/discomfort, posture, relaxation, self-healing, Uncategorized | Tags: art, books, Breathing rate, coaching, FlowMD app, nasal breathing, personal-development, self-monitoring, writing 4 CommentsDaniella Matto, MA, BCIA BCB-HRV , Erik Peper, PhD, BCB, and Richard Harvey, PhD
Adapted from: Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
This blog aims to describe several practical strategies to observe and monitor breathing patterns to promote effortless diaphragmatic breathing. The goal of these strategies is to foster effortless, whole-body diaphragmatic breathing that promote health.
Breathing is usually covert and people are not usually aware of their breathing rate (breaths per minute) or pattern (abdominal or thoracic, breath holding or shallow breathing) unless they have an illness such as asthma, emphysema or are performing physical activity (Boulding et al, 2015)). Observing breathing is challenging; awareness of respiration often leads to unaware changes in the breath pattern or to an attempt to breathe perfectly (van Dixhoorn, 2021). Ideally breathing patterns should be observed/monitored when the person is unaware of their breathing pattern and the whole body participates (van Dixhoorn, 2008). A useful strategy is to have the person perform a task and then ask, “What happened to your breathing?”. For example, ask a person to simulate putting a thread through the eye of a needle or quickly look to the extreme right and left while keeping their head still. In almost all cases, the person holds their breath (Peper et al., 2002).
Teaching effortless slow diaphragmatic breathing is a precursor of Heart rate variability (HRV) biofeedback and is based on slow paced breathing (Lehrer & Gevirtz, 2014; Steffen et al., 2017; Shaffer and Meehan, 2020). Mastering effortless diaphragmatic breathing is a powerful tool in the treatment of a variety of physical, behavioural, and cognitive conditions; however, to integrate this method into clinical or educational practice is easier said than done. Clients with dysfunctional breathing patterns often have difficulty following a breath pacer or mastering effortless breathing at a slower pace.
The purpose of this paper is to describe a few simple strategies that can be used to observe and monitor breathing patterns, provide economic strategies for observation and training, and suggestions to facilitate effortless diaphragmatic breathing.
Strategies to observe and monitor breathing pattern
Observation of the breathing patterns
- Is the breathing through the nose or mouth? Nose is usually better (Watso et al., 2023; Nestor, 2020).
- Does the abdomen expand during inhalation and constricts during exhalation or does the chest expand and rise during inhalation and fall during exhalation? Abdominal movement is usually better.
- Is exhalation flow softly or explosively like a sigh? Slow flow exhalation is preferred.
- Is the breath held or continues during activities? In most cases continued breathing is usually better.
- Does the person gasp before speaking or allows to speak while normally exhaling?
- What is the breathing rate (breaths per minute)? When sitting peacefully less than 14 breaths/minute is usually better and about 6 breaths per minute to optimize HRV
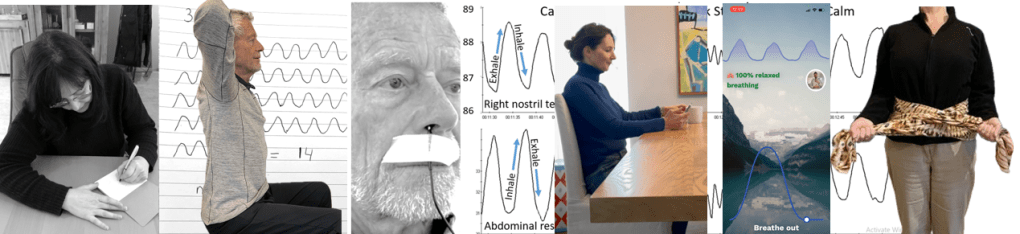
Physiological monitoring.
- Monitoring breathing with strain gauges around the abdomen and chest, and heart rate is the most common approach to identify the location of breath, the breathing pattern and heart rate variability. The strain gauges are placed around the chest and abdomen and heart rate is monitored with a blood volume pulse amplitude sensor from the finger. representative recording shows the effect of thoughts on breathing, heartrate and pulse amplitude of which the participant is totally unaware as shown in Figure 1.
Figure 1. Physiological recording of breathing patterns with strain gauges.
- Monitoring breathing with a thermistor placed at the entrance of the nostril that has the most airflow (nasal patency) (Jovanov et al., 2001; Lerman et al., 2016). When the person exhales through the nose, the thermistor temperature increases and decreases when they inhale. A representative recording of a person being calm, thinking a stressful thought. and being calm. Although there were significant changes as indicated by the change in breathing patterns, the person was unaware of the changes as shown in Figure 2.
Figure 2. Use of a thermistor to monitor breathing from the dominant nostril compared to the abdominal expansion as monitored by a strain gauge around the abdomen.
- Additional physiological monitoring approaches. There are many other physiological measures can be monitored to such as end-tidal carbon dioxide (EtCO2), a non-invasive measurement of the amount of carbon dioxide (CO2) in exhaled breath (Meuret et al., 2008; Meckley, 2013); scalene/trapezius EMG to identify thoracic breathing (Peper & Tibbett, 1992; Peper & Tibbets, 1994); low abdominal EMG to identify transfers and oblique tightening during exhalation and relaxation during inhalation (Peper et al., 2016; and heart rate to monitor cardiorespiratory synchrony (Shaffer & Meehan, 2020). Physiological monitoring is useful; since, the clinician and the participant can observe the actual breathing pattern in real time, how the pattern changes in response the cognitive and physical tasks, and used for feedback training. The recorded data can document breathing problems and evidence of mastery.
The challenges of using physiological monitoring arethat the equipment may be expensive, takes skill to operate and interpret the data, and is usually located in the office and not at home.
Economic strategies for observation and training breathing
To complement the physiological monitoring and allow observations outside the office and at home, some of the following strategies may be used to observe breathing pattern (rate and expansion of the breath in the body), and suggestion to facilitate effortless diaphragmatic breathing. These exercises make excellent homework for the client. Practicing awareness and internal self-regulation by the client outside the clinic contributes enormously to the effect of biofeedback training (Wilson et al., 2023),
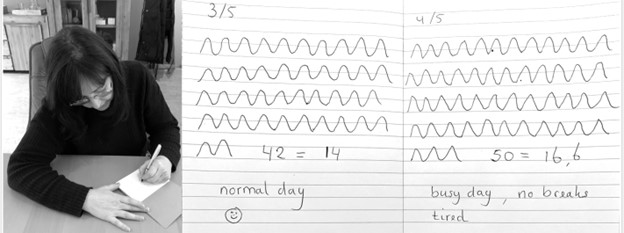
Observe breathing rate: Draw the breathing pattern
Take a piece of paper, a pen and a timer, set to 3 minutes. Start the timer. Upon inhalation draw the line up and upon exhalation draw the line down, creating a wave. When the timer stops, after 3 minutes, calculate the breathing rate per minute by dividing the number of waves by 3 as shown in Figure 3.
Figure 3. Drawing the breathing pattern for three minutes during two different days.
From these drawings, the breathing rate become evident. Many individuals are often surprised to discover that their breathing rate increased during periods of stress, such as a busy day with no breaks, compared to their normal days.
Monitoring and training diaphragmatic breathing
The scarf technique for abdominal feedback
Many participants are unaware that they are predominantly breathing in their chest and their abdomen expansion is very limited during inhalation. Before beginning, have participant loosen their belt and or stand upright since sitting collapsed/slouched or having the waist constriction such as a belt of tight constrictive clothing that inhibits abdominal expansion during inhalation.
Place the middle part of a long scarf or shawl on your lower back, take the ends in both hands and cross the ends: your left hand is holding the right part of the scarf, and the right hand is holding the left end of the scarf. Give a bit of a pull, so you can feel any movement of the scarf. When breathing more abdominally you will feel a pull at the ends of the scarf as you lower back, and flanks will expand as shown in Figure 4.

Figure 4. Using a scarf as feedback.
FlowMD app
A recent cellphone app, FlowMD, is unique because it uses the cellphone camera to detect the subtle movements of the chest and abdomen (FlowMD, 2024). It provides real time feedback of the persons breathing pattern. Using this app, the person sits in front of their cellphone camera and after calibration, the breathing pattern is displayed as shown in Figure 5.

Figure 5. Training breathing with FlowMD,.
Suggestions to optimize abdominal breathing that may lead to a slower breath rate when the client practices the technique
Beach pose
By locking the upper chest and sitting up straight it is often easier to breathe so that the abdomen can expand and constrict. Place your hands behind your head and Interlock your finger of both hands, pull your elbows back and up. The person can practice this either laying down on their back or sitting straight up at the edge of the chair as shown in Figure 6.

Figure 6. Sitting erect with the shoulders pulled back and up to allow abdominal expansion and constriction as the breathing pattern.
Observe the effect of posture on breathing
Have the person sit slouched/collapsed like a letter C and take a few slow breath, then have them sit up in a tall and erect position and take a few slow breaths. Usually they will observe that it is easier to breathe slower and lower and tall and erect.
Using your hands for feedback to guide natural breathing
Holding your hands with index fingers and thumbs touching the lower abdomen. When inhaling the fingers and thumbs separate and when exhaling they touch again (ensuring a full exhale and avoiding over breathing). The slight increase in lower abdominal muscle tension during the exhalation and relaxation during inhalation and the abdominal wall expands can also be felt with fingertips as shown in Figure 7.
Figure 7. Using your hands and finger for feedback to guide the natural breathing of expansion and constriction of the abdomen. Reproduced by permission from Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Coaching suggestions
There are many strategies to observe, teach and implement effortless breathing (Peper et al., 2024).. Even though breathing is natural and babies and young children breathe diaphragmatically as their large belly expands and constricts. Yet, in many cases the natural breathing shifts to dysfunctional breathing for multiple reasons such as chronic triggering defense reactions to avoiding pain following abdominal surgery (Peper et al, 2015). When participants initially attempt to relearn this natural pattern, it can be challenging especially, if the person habitually breathes shallowly, rapidly and predominantly in their chest.
When initially teaching effortless breathing, have the person exhale more air than normal without the upper chest compressing down and instead allow the abdomen comes in and up thereby exhaling all the air. If the person is upright then allow inhalation to occur without effort by letting the abdominal wall relaxes and expands. Initially inhale more than normal by expanding the abdomen without lifting the chest. Then exhale very slowly and continue to breathe so that the abdomen expands in 360 degrees during inhalation and constricts during exhalation. Let the breathing go slower with less and less effort. Usually, the person can feel the anus dropping and relaxing during inhalation.
Another technique is to ask the person to breathe in more air than normal and then breathe in a little extra air to completely fill the lungs, before exhaling fully. Clients often report that it teaches them to use the full capacity of the lungs.
The goal is to breath without effort. Indirectly this can be monitored by finger temperature. If the finger temperature decreases, the participant most likely is over-breathing or breathing with too much effort, creating sympathetic activity; if the finger temperature increases, breathing occurs slower and usually with less effort indicating that the person’s sympathetic activation is reduced.
Conclusion
There are many strategies to monitor and coach breathing. Relearning diaphragmatic breathing can be difficult due to habitual shallow chest breathing or post-surgical adaptations. Initial coaching may involve extended exhalations, conscious abdominal expansion, and gentle inhalation without chest movement. Progress can be monitored through indirect physiological markers like finger temperature, which reflects changes in sympathetic activity. The integration of these techniques into clinical or educational practice enhances self-regulation, contributing significantly to therapeutic outcomes. In this article we provided a few strategies which may be useful for some clients.
Additional blogs on breathing
https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
REFERENCES
Boulding, R., Stacey, R., & Niven, N. (2016). Dysfunctional breathing: a review of the literature and proposal for classification. European Respiratory Review, 25(141),: 287-294. https://doi.org/10.1183/16000617.0088-2015
FlowMD. (2024). FlowMD app. Accessed December 13, 2024. https://desktop.flowmd.co/
Jovanov, E., Raskovic, D., & Hormigo, R. (2001). Thermistor-based breathing sensor for circadian rhythm evaluation. Biomedical sciences instrumentation, 37, 493–497. https://pubmed.ncbi.nlm.nih.gov/11347441/
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Lerman, J., Feldman, D., Feldman, R. et al. Linshom respiratory monitoring device: a novel temperature-based respiratory monitor. (2016). Can J Anesth/J Can Anesth, 63, 1154–1160. https://doi.org/10.1007/s12630-016-0694-y
Meckley, A. (2013). Balancing Unbalanced Breathing: The Clinical Use of Capnographic Biofeedback. Biofeedback, 41(4), 183–187. https://doi.org/10.5298/1081-5937-41.4.02
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (2008). Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of psychiatric research, 42(7), 560–568. https://doi.org/10.1016/j.jpsychires.2007.06.005
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath-New-Science-Lost-Art/dp/0735213615/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make Health Happen. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Peper, E., & Tibbetts, V. (1992). Fifteen-month follow-up with asthmatics utilizing EMG/incentive inspirometer feedback. Biofeedback and self-regulation, 17(2), 143–151. https://doi.org/10.1007/BF01000104
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. https://biofeedbackhealth.org/wp-content/uploads/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Shaffer, F. and Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., and Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
van Dixhoorn, J.V. (2008). Whole-body breathing. Biofeedback, 36,54–58. https://www.euronet.nl/users/dixhoorn/L.513.pdf
van Dixhoorn, J.V. (2021). Functioneel ademen-Adem-en ontspannings oefeningen voor gevorderden. Amersfoort: Uiteveriy Van Dixhoorn. https://www.bol.com/nl/nl/p/functioneel-ademen/9300000132165255/
Watso, J. C., Cuba, J.N., Boutwell, S.L, Moss, J…(2023). Acute nasal breathing lowers diastolic blood pressure and increases parasympathetic contributions to heart rate variability in young adults. American Journal of Physiology Regulatory, Integrative and Comparative Physiology.
325I(6), R797-R80. https://doi.org/10.1152/ajpregu.00148.2023
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Health Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 415 338 7683 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com
360-Degree Belly Breathing with Jamie McHugh
Posted: April 26, 2024 Filed under: attention, Breathing/respiration, emotions, healing, health, meditation, mindfulness, Pain/discomfort, relaxation, self-healing | Tags: abdominal braething, belly breathing, daiphragm, effortless breathing, passive attention, self-acceptance, somatic awreness 4 Comments
Breathing is a whole mind-body experience and reflects our physical, cognitive and emotional well-being. By allowing the breath to occur effortlessly, we provide ourselves the opportunity to regenerate. Although there are many directed breathing practices that specifically directs us to inhale or exhale at specific rhythms or depth to achieve certain goals, healthy breathing is whole body experience. Many focus on being paced at a specific rhythm such as 5.5 breath per minute; however, effortless breathing is dynamic and constantly changing. It is contstantly adapting to the body’s needs: sometimes the breath is slightly slower, sometimes slightly faster, sometimes slightly deeper, sometimes slightly more shallower. The breathing process is effortless. This process can be described by the Autogenic training phrase, “It breathes me” (Luthe, 1969; Luthe, 1979; Luthe & de Rivera, 2015). Read the essay by Jamie McHugh, Registered Master Somatic Movement Therapist and then let yourself be guided in this non-striving somatic approach to allow effortless 360 degree belly breathing for regeneration.
The 360 degree belly breathing by Jamie McHugh, MSMT, is a somatic exploration to experience that breathing is not just abdominal breathing by letting the belly expand forward, but a rhythmic 360 degree increase and decrease in abdominal volume without effort. This effortless breathing pattern can often be observed in toddlers when they sit peacefully erect on the floor. This pattern of breathing not only enhances gas exchange, more importantly, it enhances abdominal blood and lymph circulation.
“The usual psychodynamic foundation for the self-experience is that of hunger, not breath. The body is experienced as an alien entity that has to be kept satisfied; the way an anxious mother might experience a new baby. When awareness is shifted from appetite to breath, the anxieties about not being enough are automatically attenuated. It requires a settling down or relaxing into one’s own body. When this fluidity moves to the forefront of awareness…there is a relaxation of the tensed self…and the emergence of a simpler, breath-based self that is capable of surrender to the moment.” – Mark Epstein (2013).
The intention behind 360 Degree Belly Breathing is to access and express the movement of the breath in all three dimensions. This is the basis for all subsequent somatic explorations within the Embodied Mindfulness protocol, a body-based approach to traditional meditation practices I have developed over the past 20 years (McHugh, 2016). Embodied Mindfulness explores the inner landscape of the body with the essential somatic technologies of breath, vocalization, self-contact, stillness and subtle movement. We focus and sustain mental attention while pleasurably cultivating bodily calm and clarity as a daily practice for survival in these turbulent times. Coupled with individual variations and experimentation, this practice becomes a reliable sanctuary from overwhelm, scattered attention, and emotional turmoil.
The Central Diaphragm

The central diaphragm, a dome-shaped muscular sheath that divides the thorax (chest) and the abdomen (belly), is the primary mechanism for breathing. It is the floor for your heart and lungs and the ceiling for your belly. The central diaphragm is a mostly impenetrable divide, with a few openings through it for the aorta, vena cava and the esophagus. Each time you inhale, the diaphragm contracts and flattens out a bit as it presses down towards your pelvis. Each time you exhale, the diaphragm relaxes and floats back up towards your heart. The motion of the diaphragm impacts the barometric pressure in your chest: the downward movement of the diaphragm on the inhale pulls oxygen into your lungs, and the subsequent exhale expels carbon dioxide into the world as the diaphragm releases upwards.
The movement of the diaphragm is twofold: involuntary and voluntary. Involuntary, ordinary breathing is a homebase and a point of return. Breathing just automatically happens – you don’t have to think about it. Breathing is also voluntary; you can choose to change the tempo (quick or slow), the duration (short or long) and quality (smooth or sharp) of this movement to “charge up and chill out” at will. Knowing how to collaborate with your diaphragm, discovering your own rhythm of diaphragmatic action, and undulating between the automatic and the chosen is a foundation for physiological equilibrium and emotional “self-soothing”.
Watch these two brief videos to get a visual image of your diaphragm in motion:
Beginning Sitting Practice
“When your back becomes straight, your mind will become quiet.” – Shunryu Suzuki
What does it mean to have a “straight back”? What are the inner coordinates and outer parameters of this position in space? And what kind of environment is needed to support this uprightness? This simple orientation to sitting can create more comfort, ease and support in your structure, which will stimulate more fluidity in your breathing and your thinking.
As you sit on a chair, consider two points of focus: body and environment. Can I sit upright with ease and comfort on this chair? If not, what changes can I make with my body and how can I adapt the environment of this chair to meet my needs? Since we are all various heights, it is not surprising a one-size-fits-all chair would need adaptation. Don’t be content with your first solution – experiment until you find just the right configuration. Valuing and seeking bodily comfort and ease are simple yet profound acts of self-kindness.
Do you need to move your pelvis forward on the chair or back? If you move your pelvis back, do you get the necessary support from the back of the chair for your pelvic bowl? If the back of the chair is too far away and/or makes you lean back into space, place a small cushion or two between the back of the chair and the base of your spine. With your back supported, are your feet on the floor? If not, place a folded blanket or a cushion under them.
With pelvis and feet in place, take a few full breaths to stabilize your pelvis and let your weight drop down through your sitz bones into the chair. The upper body receives more support from the core muscles of the lower body when your center of gravity drops – you don’t have to work so hard to maintain uprightness. Finally, rock on your sitz bones forward, backward, and side-to-side. Movement awakens bodily feedback so you can feel where center is in this moment. That sense of center will continue to change throughout the duration of the practice period so feel free to periodically adjust your position.
After this initial structural orientation, the next step is attending to the combination of breath and self-contact to fill out our self-perception. Self-contact is like using a magnifying glass – focusing the mind by feeling the substance of the belly’s movement in our hands. Since the diaphragm is a 360-degree phenomenon that generates movement in our sides and our back as well as our front, spreading awareness out not only creates different patterns of muscular activation – it also changes the brain’s map of the body and how we perceive ourselves. This change of orientation over time recalibrates our alignment and how we settle in ourselves, with awareness of our back in equal proportion to our front and sides.
360-Degree Belly Breath
“To stop your mind does not mean to stop the activities of the mind. It means your mind pervades your whole body.” – Shunryu Suzuki
Read text below or be guided by the audio file or YouTube video. http://somaticexpression.com/classes/360DegreeBreathingwithJamieMcHugh.mp3
Sit comfortably and place your hands on the front of your belly. With each inhale, become aware of the forward movement of your belly swelling. Then, with each exhale, notice the release of your belly and the settling back to center. Give this action and each subsequent action at least 5-7 breath cycles. Intersperse this way of breathing with ordinary, effortless breathing by letting the body breathe automatically. Return time and again to ordinary breathing, letting go of the focus and the effort to rest in the aftermath.
Now, slide your hands to the sides of your belly. Notice with each breath cycle how your belly moves laterally out to the sides on the inhale and then settles back to center again on the exhale.
Now, slide your hands to the back of your belly. You may wish to make contact with the back of your hands instead of your palms if it is more comfortable. With each inhale, focus on the movement into the backspace – this will be much smaller than the movement to the front; and with each exhale, the movement settling back to center.
Finally, connect all three directions: your belly radiates out 360 degrees on the horizon with each inhale, simultaneously moving forward, backward, and out to both sides, and then settles inward with each exhale.
Finish with open awareness – scanning your whole inner landscape from feet to head, back to front, and center to extremities, and letting your body breathe itself, as you notice what is alive in you now.
Inhale – Belly Radiates Outwards; Exhale – Belly Settles Inwards
“The belly is an extraordinary diagnostic instrument. It displays the armoring of the heart as a tension in the belly. Trying tightens the belly. Trying stimulates judgment. Hard belly is often judging belly. Observing the relative openness or closedness of the belly gives insight into when and how we are holding (on) to our pain. The deeper our relationship to the belly, the sooner we discover if we are holding in the mind or opening into the heart.” – Steven Levine (1991)
The contact of your hands on your belly helps the mind pay attention to the subtle movement created by the inhale-exhale cycle of the diaphragm. The combination of tactility and interoceptive awareness focusing on the belly shifts attention into our “second brain” (the enteric nervous system) and signals the mind it can rest and soften. More pleasurable sensation is often accompanied by an emergent feeling of safety as you settle into sensing the rhythm of a slower, more even breath, creating a feedback loop between bodily/somatic ease and mental calm. Giving yourself some daily “breathing room” in this way can help you build the calm muscle!
Naturally, there can be hiccups along the way so it is not all unicorns and rainbows! By giving the mind bodily tasks to accomplish, particularly in relationship to deepening and expanding the movement of the breath, we ease the self into a slower, more receptive state of being. Yet, in this receptive state of ease, whatever is in the background of awareness can arise and slip through the “border control”, sometimes taking us by surprise and causing distress. Depending upon the nature of the information, there are layers of action strategies that can be progressively taken to modulate and buffer what arises:
Tether your awareness to the breath rhythm with hands on your belly to stay present as a witness. Next step up: open your eyes softly and look around to orient in your present environment. Further step up: breath flow, hands-on belly, eyes open a wee bit looking around, and adding simple movement, like rocking a bit in all directions or expressing an exhale as a sigh, a yawn or a hum.
Note: If you find your personal resources are insufficient, find a guide to work with one-on-one to discover your own individual path for increasing the “window of capacity”. Above all, be gentle with yourself – take your time – cultivate your garden – and enjoy your breath!
References
Epstein, M. (2013) Thoughts without a Thinker: Psychotherapy from a Buddhist Perspective. New York: Basic Books. https://www.amazon.com/Thoughts-Without-Thinker-Psychotherapy-Perspective/dp/0465050948
Levine, S. (1991). Guided Meditations, Explorations and Healings. New York: Anchor. https://www.amazon.com/Guided-Meditations-Explorations-Healings-Stephen/dp/0385417373
Luthe, W. (1969). Autogenic Therapy Volume 1 Autogenic Methods. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-1-Methods/dp/B0013457B4/
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & de Rivera, L. (2015). Wolfgang Luthe Introductory workshop: Introduction to the Methods of Autogenic Training, Therapy and Psychotherapy (Autogenic Training & Psychotherapy). CreateSpace Independent Publishing Platform. https://www.amazon.com/WOLFGANG-LUTHE-INTRODUCTORY-WORKSHOP-Psychotherapy/dp/1506008038/
Is mindfulness training old wine in new bottles?
Posted: January 11, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, healing, health, meditation, self-healing, stress management | Tags: anxiety, autogenic training, biofeedback, health, meditation, mental-health, mindfulness, pain, passive attention, progressive muscle relaxation, wellness, yoga 2 CommentsAdapted from: Peper, E., Harvey, R., & Lin, I-M. (2019). Mindfulness training has themes common to other technique. Biofeedback. 47(3), 50-57. https://doi.org/10.5298/1081-5937-47.3.02

This extensive blog discusses the benefits of mindfulness-based meditation (MM) techniques and explores how similar beneficial outcomes occur with other mind-centered practices such as transcendental meditation, and body-centered practices such as progressive muscle relaxation (PMR), autogenic training (AT), and yoga. For example, many standardized mind-body techniques such as mindfulness-based stress reduction and mindfulness-based cognitive therapy (a) are associated with a reduction in symptoms of symptoms such as anxiety, pain and depression. This article explores the efficacy of mindfulness based techniques to that of other self-regulation techniques and identifies components shared between mindfulness based techniques and several previous self-regulation techniques, including PMR, AT, and transcendental meditation. The authors conclude that most of the commonly used self-regulation strategies have comparable efficacy and share many elements.
Mindfulness-based strategies are based in ancient Buddhist practices and have found acceptance as one of the major contemporary behavioral medicine techniques (Hilton et al, 2016; Khazan, 2013). Throughout this blog the term mindfulness will refer broadly to a mental state of paying total attention to the present moment, with a non-judgmental awareness of the inner and/ or outer experiences (Baer et al., 2004; Kabat-Zinn, 1994).
In 1979, Jon Kabat-Zinn introduced a manual for a standardized Mindfulness-Based Stress Reduction (MBSR) program at the University of Massachusetts Medical Center (Kabat-Zinn, 1994, 2003). The eight-week program combined mindfulness as a form of insight meditation with specific types of yoga breathing and movements exercises designed to focus on awareness of the mind and body, as well as thoughts, feelings, and behaviors.
There is a substantial body of evidence that mindfulness-based cognitive therapy (MBCT); Teasdale et al., 1995) and mindfulness-based stress reduction (MBSR) (Kabat-Zinn, 1994, 2003) have combined with skills of cognitive therapy for ameliorating stress symptoms such as negative thinking, anxiety and depression. For example, MBSR and MBCT has been confirmed to be clinical beneficial in alleviating a variety of mental and physical conditions, for people dealing with anxiety, depression, cancer-related pain and anxiety, pain disorder, or high blood pressure (The following are only a few of the hundred studies published: Andersen et al., 2013; Carlson et al., 2003; Fjorback et al., 2011; Greeson, & Eisenlohr-Moul, 2014; Hoffman et al., 2012; Marchand, 2012; Baer, 2015; Demarzo et al., 2015; Khoury et al, 2013; Khoury et al, 2015; Chapin et al., 2014; Witek Janusek et al., 2019). Currently, MBSR and MBCT techniques that are more standardized are widely applied in schools, hospitals, companies, prisons, and other environments.
The Relationship Between Mindfulness and Other Self-Regulation Techniques
This section addresses two questions: First, how do mindfulness-based interventions compare in efficacy to older self-regulation techniques? Second, and perhaps more basically, how new and different are mindfulness-based therapies from other self-regulation-oriented practices and therapies?
Is mindfulness more effective than other mind/body body/mind approaches?
Although mindfulness-based meditation (MM) techniques are effective, it does not mean that is is more effective than other traditional meditation or self-regulation approaches. To be able to conclude that MM is superior, it needs to be compared to equivalent well-coached control groups where the participants were taught other approaches such as progressive relaxation, autogenic training, transcendental meditation, or biofeedback training. In these control groups, the participants would be taught by practitioners who were self-experienced and had mastered the skills and not merely received training from a short audio or video clip (Cherkin et al, 2016). The most recent assessment by the National Centere for Complementary and Integrative Health, National Institutes of Health (NCCIH-NIH, 2024) concluded that generally “the effects of mindfulness meditation approaches were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise especially when they include how to generalize the skills during the day” (NCCIH, 2024). Generalizing the learned skills into daily life contributes to the successful outcome of Autogenic Training, Progressive Relaxation, integrated biofeedback stress management training, or the Quieting Response (Luthe, 1979; Davis et al., 2019; Wilson et al., 2023; Stroebel, 1982).
Unfortunately, there are few studies that compare the effective of mindfulness meditation to other sitting mental techniques such as Autogenic Training, Transcendental Meditation or similar meditative practices that are used therapeutically. When the few randomized control studies of MBSR versus autogenic training (AT) was done, no conclusions could be drawn as to the superior stress reduction technique among German medical students (Kuhlmann et al., 2016).
Interestingly, Tanner, et al (2009) in a waitlist study of students in Washington, D.C. area universities practicing TM used the concept of mindfulness, as measured by the Kentucky Inventory of Mindfulness Skills (KIM) (Baer et al, 2004) as a dependent variable, where TM practice resulted in greater degrees of ‘mindfulness.’ More direct comparisons of MM with body-focused techniques, such as progressive relaxation, or Autogenic training mindfulness-based approaches, have not found superior benefit. For example, Agee et al (2009) compared the stress management effects of a five-week Mindfulness Meditation (MM) to a five-week Progressive Muscle Relaxation (PMR) course and found no meaningful reports of superiority of one over the other program; both MM and PMR were effective in reducing symptoms of stress.
In a persuasive meta-analysis comparing MBSR with other similar stress management techniques used among military service members, Crawford, et al (2013) described various multimodal programs for addressing post-traumatic stress disorder (PTSD) and other military or combat-related stress reactions. Of note, Crawford, et al (2013) suggest that all of the multi-modal approaches that include Autogenic Training, Progressive Muscle Relaxation, movement practices including Yoga and Tai Chi, as well as Mindfulness Meditation, and various types of imagery, visualization and prayer-based contemplative practices ALL provide some benefit to service members experiencing PTSD.
An important observation by Crawford et al (2013) pointed out that when military service members had more physical symptoms of stress, the meditative techniques appeared to work best, and when the chief complaints were about cognitive ruminations, the body techniques such as Yoga or Tai Chi worked best to reduce symptoms. Whereas it may not be possible to say that mindfulness meditation practices are clearly superior to other mind-body techniques, it may be possible to raise questions about mechanisms that unite the mind-body approaches used in therapeutic settings.
Could there be negative side effects?
Another point to consider is the limited discussion of the possible absence of benefit or even harms that may be associated with mind-body therapies. For example, for some people, meditation does not promote prosocial behavior (Kreplin et al, 2018). For other people, meditation can evoke negative physical and/or psychological outcomes (Lindahl et al, 2017; Britton et al., 2021). There are other struggles with mind-body techniques when people only find benefit in the presence of a skilled clinician, practitioner, or guru, suggesting a type of psychological dependency or transference, rather than the ability to generalize the benefits outside of a set of conditions (e.g. four to eight weeks of one to four hour trainings) or a particular setting (e.g. in a natural and/or quiet space).
Whereas the detailed instructions for many mindfulness meditation trainings, along with many other types of mind-body practices (e.g. Transcendental Meditation, Autogenic Training, Progressive Muscle Relaxation, Yoga, Tai Chi…) create conditions that are laudable because they are standardized, a question is raised as to ‘critical ingredients’, using the metaphor of baking. The difference between a chocolate and a vanilla cake is not ingredients such as flour, or sugar, etc., which are common to all cakes, but rather the essential or critical ingredient of the chocolate or vanilla flavoring. So what are the essential or critical ingredients in mind-body techniques? Extending the metaphor, Crawford, et al (2013, p. 20) might say the critical ingredient common to the mind-body techniques they studied was that people “can change the way their body and mind react to stress by changing their thoughts, emotions, and behaviors…” with techniques that, relatively speaking, “involve minimal cost and training time.”
The skeptical view suggested here is that MM techniques share similar strategies with other mind-body approaches that encouraging learners to ‘pay attention and shift intention.’ This strategy is part of the instructions when learning Progressive Relaxation, Autogenic Training, Transcendental Meditation, movement meditation of Yoga and Tai Chi and, with instrumented self-regulation techniques such as bio/neurofeedback. In this sense, MM training repackages techniques that have been available for millennia and thus becomes ‘old wine sold in new bottles.’
We wonder if a control group for compassionate mindfulness training would report more benefits if they were asked not only to meditate on compassionate acts, but actually performed compassionate tasks such as taking care of person in pain, helping a homeless person, or actually writing and delivering a letter of gratitude to a person who has helped them in the past? The suggestion is to titrate the effects of MM techniques, moving from a more basic level of benefit to a more fully actualized level of benefit, generalizing their skill beyond a training setting, as measured by the Baer et al (2004) Kentucky Inventory of Mindfulness Skills.
Each generation of clinicians and educators rediscover principles without always recognizing that the similar principles were part of the previous clinical interventions. The analogies and language has changed; however, the underlying concepts may be the same. Mindfulness interventions are now the new, current and popular approach. Some of the underlying ‘mindfulness’ concepts that are shared in common with successfully other mind-body and self-regulation approaches include:
The practitioner must be self-experienced in mindfulness practice. This means that the practitioners do not merely believe the practice is effective; they know it is effective from self-experience. Inner confidence conveyed to clients and patients enhances the healing/placebo effect. It is similar to having sympathy or empathy for clients and patients that occurs from have similar life experiences, such as when a clinician speaks to a patient. For example, a male physician speaking to a female patient who has had a mastectomy may be compassionate; however, empathy occurs more easily when another mastectomy patient (who may also be a physician) shares how she struggled overcame her doubts and can still be loved by her partner.
There may also be a continuum of strengthening beliefs about the benefits of mindfulness techniques that leads to increase benefits for the approach. Knowing there are some kinds of benefits from initiating a practice of mindfulness increases empathy/compassion for others as they learn. Proving that mindfulness techniques are causing benefits after systematically comparing their effectiveness with other approaches strengthens the belief in the mindfulness approaches. Note that a similar process of strengthening one’s belief in an approach occurs gradually, over time as clients and patients progress through beginner, intermediate and advanced levels of mind-body practices.
Observing thoughts without being captured. Being a witness to the thoughts, emotions, and external events results in a type of covert global desensitization and skill mastery of NOT being captured by those thoughts and emotions. This same process of non-attachment and being a witness is one of the underpinnings of techniques that tacitly and sometime covertly support learning ways of controlling attention, such as with Autogenic Training; namely how to passively attend to a specific body part without judgment and, report on the subjective experience without comparison or judgment.
Ongoing daily practice. Participants take an active role in their own healing process as they learn to control and focus their attention. Participants are often asked to practice up to one hour a day and apply the practices during the day as mini-practices or awareness cues to interrupt the dysfunctional behavior. For example in Autogenic training, trainees are taught to practice partial formula (such my “neck and shoulders are heavy”) during the day to bring the body/mind back to balance. While with Progressive Relaxation, the trainee learns to identify when they tighten inappropriate muscles (dysponesis) and then inhibit this observed tension.
Peer support by being in a group. Peer support is a major factor for success as people can share their challenges and successes. Peer support tends to promote acceptance of self-and others and provides role modeling how to cope with stressors. It is possible that some peer support groups may counter the benefits of a mind-body technique, especially when the peers do not provide support or may in fact impede progress when they complain of the obstacles or difficulties in their process.
These concepts are not unique to Mindfulness Meditation (MM) training. Similar instructions have been part of the successful/educational intervention of Progressive Relaxation, Autogenic Training, Yogic practices, and Transcendental Meditation. These approaches have been most successful when the originators, and their initial students, taught their new and evolving techniques to clients and patients; however, they became less successful as later followers and practitioners used these approaches without learning an in-depth skill mastery. For example, Progressive relaxation as taught by Edmund Jacobson consisted of advanced skill mastery by developing subtle awareness of different muscle tension that was taught over 100 sessions (Mackereth & Tomlinson, 2010). It was not simply listening once to a 20-minute audio recording about tightening and relaxing muscles. Similarly, Autogenic training is very specific and teaches passive attention over a three to six-month time-period while the participant practices multiple times daily. Stating the obvious, learning Autogenic Training, Mindfulness, Progressive Relaxation, Bio/Neurofeedback or any other mind-body technique is much more than listening to a 20-minute audio recording.
The same instructions are also part of many movement practices. For many participants focusing on the movement automatically evoked a shift in attention. Their attention is with the task and they are instructed to be present in the movement.
Areas to explore.
Although Mindfulness training with clients and patients has resulted in remarkable beneficial outcomes for the participants, it is not clear whether mindfulness training is better than well taught PR, AT, TM or other mind/body or body/mind approaches. There are also numerous question to explore such as: 1) Who drops out, 2) Is physical exercise to counter sitting disease and complete the alarm reaction more beneficial, and 3) Strategies to cope with wandering attention.
- Who drops out?
We wonder if mindfulness is appropriate for all participants as sometimes participants drop out or experience negative abreactions. It not clear who those participants are. Interestingly, hints for whom the techniques may be challenging can be found in the observations of Autogenic Training that lists specific guidelines for contra-, relative- and non-indications (Luthe, 1970).
- Physical movement to counter sitting disease and complete the alarm reaction.
Although many mindfulness meditation practices may include yoga practices, most participants practice it in a sitting position. It may be possible that for some people somatic movement practices such as a slow Zen walk may quiet the inner dialogue more quickly. In our experience, when participants are upset and highly stressed, it is much easier to let go of agitation by first completing the triggered fight/flight response with vigorous physical activity such as rapidly walking up and downs stairs while focusing on the burning sensations of the thigh muscles. Once the physical stress reaction has been completed and the person feels physically calmer then the mind is quieter. Then have the person begin their meditative practice.
- Strategies to cope with wandering attention.
Some participants have difficulty staying on task, become sleepy, worry, and/or are preoccupied. We observed that first beginning with physical movement practices or Progressive Relaxation appears to be a helpful strategy to reduce wandering thoughts. If one has many active thoughts, progressive relaxation continuously pulls your attention to your body as you are directed to tighten and let go of muscle groups. Being guided supports developing the passive focus of attention to bring awareness back to the task at hand. Once internally quieter, it is easier hold their attention while doing Autogenic Training, breathing or Mindfullness Meditation.
By integrating somatic components with the mindfulness such as done in Progressive Relaxation or yoga practices facilitates the person staying present. Similarly, when teaching slower breathing, if a person has a weight on their abdomen while practicing breathing, it is easier to keep attending to the task: allow the weight to upward when inhaling and feeling the exhalation flowing out through the arms and legs.
Therapeutic and education strategies that implicitly incorporate mindfulness
Progressive relaxation
In the United States during the 1920 progressive relaxation (PR) was developed and taught by Edmund Jacobson (1938). This approach was clinically very successful for numerous illnesses ranging from hypertension, back pain, gastrointestinal discomfort, and anxiety; it included 50 year follow-ups. Patients were active participants and practiced the skills at home and at work and interrupt their dysfunctional patterns during the day such as becoming aware of unnecessary muscle tension (dyponetic activity) and then release the unnecessary muscle tension (Whatmore & Kohli, 1968). This structured approach is totally different than providing an audio recording that guides clients and patients through a series of tightening and relaxing of their muscles. The clinical outcome of PR when taught using the original specific procedures described by Jacobson (1938) was remarkable. The incorporation of Progressive Relaxation as the homework practice was an important cofactor in the successful outcome in the treatment of muscle tension headache using electromyography (EMG) biofeedback by Budzynski, Stoyva and Adler (1970).
Autogenic Training
In 1932 Johannes Schultz in Germany published a book about Autogenic Training describing the basic training procedure. The basic autogenic procedure, the standard exercises, were taught over a minimum period of three month in which the person practiced daily. In this practice they directed theri passive attention to the following cascading sequence: heaviness of their arms, warmth of their arms, heart beat calm and regular, breathing calm and regular or it breathes me, solar plexus is warm, forehead is cool, and I am at peace (Luthe, 1979). Three main principles of autonomic training mentioned by Luthe (1979) are: (1) mental repetition of topographically oriented verbal formulae for brief periods; (2) passive concentration; and (3) reduction of exteroceptive and proprioceptive afferent stimulation. The underlying concepts of Autogenic Therapy include as described by Peper and Williams (1980):
The body has an innate capacity for self-healing and it is this capacity that is allowed to become operative in the autogenic state. Neither the trainer nor trainee has the wisdom necessary to direct the course of the self-balancing process; hence, the capacity is allowed to occur and not be directed.
- Homeostatic self-regulation is encouraged.
- Much of the learning is done by the trainee at home; hence, the responsibility for the training lies primarily with the trainee.
- The trainer/teacher must be self-experience in the practice.
- The attitude necessary for successful practice is one of passive attention; active striving and concern with results impedes the learning process. An attitude of acceptance is cultivated, letting be whatever comes up. This quality of attention is known as “mindfulness’ in meditative traditions.
The clinical outcome for autogenic therapy is very promising. The detailed guided self-awareness training and uncontrolled studies showed benefits across a wide variety of psychosomatic illness such as asthma, cancer, hypertension, anxiety, pain irritable bowel disease, depression (Luthe & Schultz, 1970a; Luthe & Schultz, 1970b). Autogenic training components have also been integrated in biofeedback training. Elmer and Alice Green included the incorporation of autogenic training phrases with temperature biofeedback for the very successful treatment of migraines (Green & Green, 1989). Autonomic training combine with biofeedback in clinical practices produced better results than control group for headache population (Luthe, 1979). Empirical research found that autonomic training was applied efficiently in emotional and behavioral problems, and physical disorder (Klott, 2013), such as skin disorder (Klein & Peper, 2013), insomnia (Bowden et al., 2012), Meniere’s disease (Goto, Nakai, & Ogawa, 2011) and the multitude of stress related symptoms (Wilson et al., 2023).
Bio/neurofeedback training
Starting in the late 1960s, biofeedback procedures have been developed as a successful treatment approach for numerous illnesses ranging from headaches, hypertension, to ADHD (Peper et al., 1979; Peper & Shaffer, 2010; Khazan, 2013). In most cases, the similar instructions that are part of mindfulness meditation are also embedded in the bio/neurofeedback instructions. The participants are instructed to learn control over some physiological parameter and then practice the same skill during daily life. This means that during the learning process, the person learn passive attention and is not be captured by marauding thoughts and feeling. and during the day develop awareness Whenever they become aware of dysfunctional patterns, thoughts, emotions, they initiated their newly learned skill. The ongoing biological feedback signals continuously reminds them to focus.
Transcendental meditation
The next fad to hit the American shore was Transcendental Meditation (TM)– a meditation practice from the ancient Vedic tradition in India. The participant were given a mantra that they mentally repeated and if their attention wanders, they go back to repeating the mantra internally. The first study that captured the media’s attention was by Wallace (1970) published in the Journal Science which reported that “During meditation, oxygen consumption and heart rate decreased, skin resistance increased, and the electroencephalogram showed specific changes in certain frequencies. These results seem to distinguish the state produced by Transcendental Meditation from commonly encountered states of consciousness and suggest that it may have practical applications.” (Wallace, 1970).
The participants were to practice the mantra meditation twice a day for about 20 minutes. Meta-analysis studies have reported that those who practiced TM as compared to the control group experienced significant improved of numerous disorders such as CVD risk factors, anxiety, metabolic syndrome, drug abuse and hypertension (Paul-Labrador et al, 2006; Rainforth et al., 2007; Hawkins, 2003).
To make it more acceptable for the western audience, Herbert Benson, MD, adapted and simplified techniques from TM training and then labelled a core element, the ‘relaxation response’ (Benson et al., 1974) Instead of giving people a secret mantra and part of a spiritual tradition, he recommend using the word “one” as the mantra. Numerous studies have demonstrated that when patients practice the relaxation response, many clinical symptoms were reduced. The empirical research found that practiced transcendental meditation caused increasing prefrontal low alpha power (8-10Hz) and theta power of EEG; as well as higher prefrontal alpha coherence than other locations at both hemispheres. Moreover, some individuals also showed lower sympathetic activation and higher parasympathetic activation, increased respiratory sinus arrhythmic and frontal blood flow, and decreased breathing rate (Travis, 2001, 2014). Although TM and Benson’s relaxation response continues to be practiced, mindfulness has taking it place.
Conclusion
Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) are very beneficial and yet may be considered ‘old wine in new bottles’ where the metaphor refers to millennia old meditation techniques as ‘old wine’ and the acronyms such as MBSR or MBCT as ‘new bottles’. Like many other ‘new’ therapeutic approaches or for that matter, many other ‘new’ medications, use it now before it becomes stale and loses part of its placebo power. As long as the application of a new technique is taught with the intensity and dedication of the promotors of the approach, and as long as the participants are required to practice while receiving support, the outcomes will be very beneficial, and most likely similar in effect to other mind-body approaches.
The challenge facing mindfulness practices just as those from Autogenic Training, Progressive Relaxation and Transcendental Meditation, is that familiarity breeds contempt and that clients and therapists are continuously looking for a new technique that promises better outcome. Thus as Mindfulness training is taught to more and more people, it may become less promising. In addition, as mindfulness training is taught in less time, (e.g. fewer minutes and/or fewer sessions), and with less well-trained instructors, who may offer less support and supervision for people experiencing possible negative effects, the overall benefits may decrease. Thus, mindfulness practice, Autogenic training, progressive relaxation, Transcendental Meditation, movement practices, meditation, breathing practices as well as the many spiritual practices all appear to share common fate of fading over time. Whereas the core principles of mind-body techniques are ageless, the execution is not always assured.
References
Agee, J. D., Danoff-Burg, S., & Grant, C. A. (2009). Comparing brief stress management courses in a community sample: Mindfulness skills and progressive muscle relaxation. Explore: The Journal of Science and Healing, 5(2), 104-109. https://doi.org/10.1016/j.explore.2008.12.004
Andersen, S. R., Würtzen, H., Steding-Jessen, M., Christensen, J., Andersen, K. K., Flyger, H., … & Dalton, S. O. (2013). Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients. Acta Oncologica, 52(2), 336-344. https://doi.org/10.3109/0284186X.2012.745948
Alvarez-Jimenez, M., Gleeson, J. F., Bendall, S., Penn, D. L., Yung, A. R., Ryan, R. M., … Nelson, B. (2018). Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy. Schizophrenia Research, 202, 369-377 https://doi.org/10.1016/j.schres.2018.07.022
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. https://doi.org/10.1093/clipsy/bpg015
Baer, R. A.. (2015). Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. New York: Elsevier. https://www.elsevier.com/books/mindfulness-based-treatment-approaches/baer/978-0-12-416031-6
Baer, R., Smith, G., & Allen, K. (2004). Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment, 11, 191–206. https://doi.org/10.1177/1073191104268029
Benson, H., Beary, J. F., & Carol, M. P. (1974).The Relaxation Response. Psychiatry, 37(1), 37-46. https://www.tandfonline.com/loi/upsy20
Bowden, A., Lorenc, A., & Robinson, N. (2012). Autogenic Training as a behavioural approach to insomnia: A prospective cohort study. Primary Health Care Research & Development, 13, 175-185. https://doi.org/10.1017/S1463423611000181
Britton, W.B., Lindahl, J.R., Coope, D.J., Canby, N.K., & Palitsky, R. (2021). Defining and Measuring Meditation-Related Adverse Effects in Mindfulness-Based Programs. Clinical Psychological Science, 9(6), 1185-1204. https://doi.org/10.1177/2167702621996340
Budzynski, T., Stoyva, J., & Adler, C. (1970). Feedback-induced muscle relaxation: Application to tension headache. Journal of Behavior Therapy and Experimental Psychiatry, 1(3), 205-211. https://doi.org/10.1016/0005-7916(70)90004-2
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2003). Mindfulness‐based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine, 65(4), 571-581. https://doi.org/10.1097/01.psy.0000074003.35911.41
Chapin, H. L., Darnall, B. D., Seppala, E. M., Doty, J. R., Hah, J. M., & Mackey, S. C. (2014). Pilot study of a compassion meditation intervention in chronic pain. J Compassionate Health Care, 1(4), 1-12. https://doi.org/10.1186/s40639-014-0004-x
Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., … & Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA, 315(12), 1240-1249. https://doi.org/10.1001/jama.2016.2323
Crawford, C., Wallerstedt, D. B., Khorsan, R., Clausen, S. S., Jonas, W. B., & Walter, J. A. (2013). A systematic review of biopsychosocial training programs for the self-management of emotional stress: Potential applications for the military. Evidence-Based Complementary and Alternative Medicine, 747694: 1-23. https://doi.org/10.1155/2013/747694
Davis, M., Eshelman, E.R., & McKay, M. (2019). The Relaxation and Stress Reduction Workbook. Oakland, CA: New Harbinger Publications. https://www.amazon.com/Relaxation-Reduction-Workbook-Harbinger-Self-Help/dp/1684033349
Demarzo, M. M., Montero-Marin, J., Cuijpers, P., Zabaleta-del-Olmo, E., Mahtani, K. R., Vellinga, A., Vincens, C., Lopez del Hoyo, Y., & García-Campayo, J. (2015). The efficacy of mindfulness-based interventions in primary care: A meta-analytic review. The Annals of Family Medicine, 13(6), 573-582. https://doi.org/10.1370/afm.1863
Fjorback, L. O., Arendt, M., Ørnbøl, E., Fink, P., & Walach, H. (2011). Mindfulness‐Based Stress Reduction and Mindfulness‐Based Cognitive Therapy–A systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica, 124(2), 102-119. https://doi.org/10.1111/j.1600-0447.2011.01704.x
Goto, F., Nakai, K., & Ogawa, K. (2011). Application of autogenic training in patients with Meniere disease. European Archives of Oto-Rhino-Laryngology, 268(10), 1431-1435. https://doi.org/10.1007/s00405-011-1530-1
Greeson, J., & Eisenlohr-Moul, T. (2014). Mindfulness-based stress reduction for chronic pain. In R. A. Baer (Ed.), Mindfulness-Based Treatment Approaches: Clinician’s Guide to Evidence Base and Applications, 269-292. San Diego, CA: Academic Press. https://psycnet.apa.org/record/2014-40932-000
Green, E. and Green, A. (1989). Beyond Biofeedback. New York: Knoll. https://www.amazon.com/Beyond-Biofeedback-Elmer-Green/dp/0940267144
Hawkins, M. A. (2003). Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery. Journal of Offender Rehabilitation, 36(1-4), 47- 65. https://doi.org/10.1300/J076v36n01_03
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., …Maglione, M. A. (2016). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199-213. https://doi.org/10.1007/s12160-016-9844-2
Hoffman, C. J., Ersser, S. J., Hopkinson, J. B., Nicholls, P. G., Harrington, J. E., & Thomas, P. W. (2012). Effectiveness of mindfulness-based stress reduction in mood, breast-and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology, 30(12), 1335-1342. https://doi.org/10.1200/JCO.2010.34.0331
Jacobson, E. (1938). Progressive relaxation. Chicago, IL: University of Chicago Press. https://www.amazon.com/Progressive-Relaxation-Physiological-Investigation-Significance/dp/0226390594
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion. https://www.amazon.com/Wherever-You-There-Are-Mindfulness/dp/0306832011
Kabat-Zinn, J. (2003). Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences, 8, 73–107. https://psycnet.apa.org/record/2004-19791-008
Khazan, I. Z. (2013). The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. New York: John Wiley & Sons. https://www.amazon.com/Clinical-Handbook-Biofeedback-Step-Step/dp/1119993717
Klein, A., & Peper, E. (2013). There Is hope: Autogenic biofeedback training for the treatment of psoriasis. Biofeedback, 41 (4), 194-201. https://doi.org/10.5298/1081-5937-41.4.01
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763-771. https://doi.org/10.1016/j.cpr.2013.05.005
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519-528.
Klott, O. (2013). Autogenic Training–a self-help technique for children with emotional and behavioural problems. Therapeutic Communities: The International Journal of Therapeutic Communities, 34(4), 152-158. https://doi.org/10.1108/TC-09-2013-0027
Kreplin, U., Farias, M., & Brazil, I. A. (2018). The limited prosocial effects of meditation: A systematic review and meta-analysis. Sci Rep, 8, 2403. https://doi.org/10.1038/s41598-018-20299-z
Kuhlmann, S. M., Huss, M., Bürger, A., & Hammerle, F. (2016). Coping with stress in medical students: results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Medical Education, 16(1), 316. https://doi.org/10.1186/s12909-016-0833-8
Lindahl, J. R., Fisher, N. E., Cooper, D. J., Rosen, R. K, & Britton, W. B. (2017). The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoSONE, 12(5): e0176239. https://doi.org/10.1371/journal.pone.0176239
Luthe, W. (1970). Autogenic therapy: Research and theory. New York: Grune and Stratton. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/abs/autogenic-therapy-edited-by-wolfgang-luthe-volume-4-research-and-theory-by-wolfgang-luthe-grune-and-stratton-new-york-1970-pp-276-price-1475/6C8521C36C37254A08AAD1F2FE08211C
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970a). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
Luthe, W. & Schultz, J. H. (1970b). Autogenic therapy: Applications in psychotherapy. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-Applications-Psychotherapy-v/dp/0808902725
Mackereth, P.A. & Tomlinson, L. (2010). Progressive muscle relaxation. In Cawthorn, A. & Mackereth, P.A. eds. Integrative Hypnotherapy. London: Churchill Livingstone. https://www.amazon.com/Integrative-Hypnotherapy-Complementary-approaches-clinical/dp/0702030821
Marchand, W. R. (2012). Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice, 18(4), 233-252. https://doi.org/10.1097/01.pra.0000416014.53215.86
NCCIH (2024). Meditation and Mindfulness: What You Need To Know. National Center for Complementary and Integrative Health, National Institutes of Health. Accessed January 31, 2024. https://www.nccih.nih.gov/health/meditation-and-mindfulness-what-you-need-to-know?
Paul-Labrador, M., Polk, D., Dwyer, J.H. et al. (2006). Effects of a randomized controlled trial of Transcendental Meditation on components of the metabolic syndrome in subjects with coronary heart disease. Archive of Internal Medicine, 166(11), 1218-1224. https://doi.org/10.1001/archinte.166.11.1218
Peper, E., Ancoli, S. & Quinn, M. (Eds). (1979). Mind/Body Integration: Essential Readings in Biofeedback. New York: Plenum. https://www.amazon.com/Mind-Body-Integration-Essential-Biofeedback/dp/0306401029
Peper, E. & Shaffer, F. (2010). Biofeedback History: An Alternative View. Biofeedback, 38 (4): 142–147. https://doi.org/10.5298/1081-5937-38.4.03
Peper, E., & Williams, E.A. (1980). Autogenic therapy. In A. C. Hastings, J. Fadiman, & J. S. Gordon (Eds.), Health for the whole person (pp137-141).. Boulder: Westview Press. https://biofeedbackhealth.files.wordpress.com/2016/02/autogenic-therapy-peper-and-williams.pdf
Rainforth, M.V., Schneider, R.H., Nidich, S.I., Gaylord-King, C., Salerno, J.W., & Anderson, J.W. (2007). Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Current Hypertension Reports, 9(6), 520–528. https://doi.org/10.1007/s11906-007-0094-3
Stroebel, C. (1982). QR: The Quieting Reflex. New York: Putnam Pub Group. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570
Tanner, M. A., Travis, F., Gaylord‐King, C., Haaga, D. A. F., Grosswald, S., & Schneider, R. H. (2009). The effects of the transcendental meditation program on mindfulness. Journal of Clinical Psychology 65(6), 574-589. https://doi.org/10.1002/jclp.20544
Teasdale, J. D., Segal, Z., & Williams, J. M. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy, 33, 25–39. https://doi.org/10.1016/0005-7967(94)e0011-7
Travis, F. (2001). Autonomic and EEG patterns distinguish transcending from other experiences during transcendental meditation practice. International Journal of Psychophysiology, 42, 1–9. https://doi.org/10.1016/s0167-8760(01)00143-x
Travis, F. (2014). Transcendental experiences during meditation practice. Annals of the New York Academy of Sciences, 1307, 1–8. https://doi.og10.1111/nyas.12316
Wallace, K.W. (1970). Physiological Effects of Transcendental Meditation. Science, 167 (3926), 1751-1754. https://doi.org/10.1126/science.167.3926.1751
Whatmore, G. B., & Kohli, D. R. (1968). Dysponesis: A neurophysiologic factor in functional disorders. Behavioral Science, 13(2), 102–124. https://doi.org/10.1002/bs.3830130203
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
Witek Janusek, L., Tel,l D., & Mathews, H.L. (2019). Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: A randomized trial with active control. Brain Behav Immun, 80:358-373. https://doi.org/10.1016/j.bbi.2019.04.012
Hope for menstrual cramps (dysmenorrhea) with breathing
Posted: April 22, 2023 Filed under: behavior, biofeedback, Breathing/respiration, healing, health, meditation, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: dysmenorrhea, Imagery, menstrual cramps, stroking, visualization 6 CommentsAdapted from: Peper, E., Chen, S., Heinz, N., & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04; Republished in Townsend E-Letter – 18 November, 2023 https://www.townsendletter.com/e-letter-22-breath-affects-stress-and-menstrual-cramps/ Google NotebookLM generated podcast:

“I have always had extremely painful periods. They would get so painful that I would have to call in sick and take some time off from school. I have been to many doctors and medical professionals, and they told me there is nothing I could do. I am currently on birth control, and I still get some relief from the menstrual pain, but it would mess up my moods. I tried to do the diaphragmatic breathing so that I would be able to continue my life as a normal woman. And to my surprise it worked. I was simply blown away with how well it works. I have almost no menstrual pain, and I wouldn’t bloat so much after the diaphragmatic breathing.” -22 year old student
Each semester numerous students report that their cramps and dysmenorrhea symptoms decrease or disappear during the semester when they implement the relaxation and breathing practices that are taught in the semester long Holistic Health class. Given that so many young women suffer from dysmenorrhea, many young women could benefit by using this integrated approach as the first self-care intervention before relying on pain reducing medications or hormones to reduce pain or inhibit menstruation. Another 28-year-old student reported:
“Historically, my menstrual cramps have always required ibuprofen to avoid becoming distracting. After this class, I started using diaphragmatic breath after pain started for some relief. True benefit came when I started breathing at the first sign of discomfort. I have not had to use any pain medication since incorporating diaphragmatic breath work.”
This report describes students practicing self-regulation and effortless breathing to reduce stress symptoms, explores possible mechanisms of action, and suggests a protocol for reducing symptoms of menstrual cramps. Watch the short video how diaphragmatic breathing eliminated recurrent severe dysmenorrhea (pain and discomfort associated with menstruation).
Background: What is dysmenorrhea?
Dysmenorrhea is one of the most common conditions experienced by women during menstruation and affects more than half of all women who menstruate (Armour et al., 2019). Most commonly dysmenorrhea is defined by painful cramps in the lower abdomen often accompanied by pelvic pain that starts either a couple days before or at the start of menses. Symptoms also increase with stress (Wang et al., 2003) with pain symptoms usually decreasing in severity as women get older and, after pregnancy.
Economic cost of dysmenorrhea
Dysmenorrhea can significantly interfere with a women’s ability to be productive in their occupation and/or their education. It is “one of the leading causes of absenteeism from school or work, translating to a loss of 600 million hours per year, with an annual loss of $2 billion in the United States” (Itani et al, 2022). For students, dysmenorrhea has a substantial detrimental influence on academic achievement in high school and college (Thakur & Pathania, 2022). Despite the frequent occurrence and negative impact in women’s lives, many young women struggle without seeking or having access to medical advice or, without exploring non-pharmacological self-care approaches (Itani et al, 2022).
Treatment
The most common pharmacological treatments for dysmenorrhea are nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Aspirin, and Naproxen Sodium) along with hormonal contraceptives. NSAIDs act by preventing the action of cyclooxygenase which prevents the production of prostaglandins. Itani et al (2022) suggested that prostaglandin production mechanisms may be responsible for the disorder. Hormonal contraceptives also prevent the production of prostaglandins by suppressing ovulation and endometrial proliferation.
The pharmacological approach is predominantly based upon the model that increased discomfort appears to be due to an increase in intrauterine secretion of prostaglandins F2α and E2 that may be responsible for the pain that defines this condition (Itani et al, 2022). Pharmaceuticals which influence the presence of prostaglandins do not cure the cause but mainly treat the symptoms.
Treatment with medications has drawbacks. For example, NSAIDs are associated with adverse gastrointestinal and neurological effects and also are not effective in preventing pain in everyone (Vonkeman & van de Laar, 2010). Hormonal contraceptives also have the possibility of adverse side effects (ASPH, 2023). Acetaminophen is another commonly used treatment; however, it is less effective than other NSAID treatments.
Self-regulation strategies to reduce stress and influence dysmenorrhea
Common non-pharmacological treatments include topical heat application and exercise. Both non-medication approaches can be effective in reducing the severity of pain. According to Itani et al. (2022), the success of integrative holistic health treatments can be attributed to “several mechanisms, including increasing pelvic blood supply, inhibiting uterine contractions, stimulating the release of endorphins and serotonin, and altering the ability to receive and perceive pain signals.”
Although less commonly used, self-regulation strategies can significantly reduce stress levels associated menstrual discomfort as well as reduce symptoms. More importantly, they do not have adverse side effects, but the effectiveness of the intervention varies depending on the individual.
- Autogenic Training (AT), is a hundred year old treatment approach developed by the German psychiatrist Johannes Heinrich Schultz that involves three 15 minute daily practice of sessions, resulted in a 40 to 70 percent decrease of symptoms in patient suffering from primary and secondary dysmenorrhea (Luthe & Schultz, 1969). In a well- controlled PhD dissertation, Heczey (1978) compared autogenic training taught individually, autogenic training taught in a group, autogenic training plus vaginal temperature training and a no treatment control in a randomized controlled study. All treatment groups except the control group reported a decrease in symptoms and the most success was with the combined autogenic training and vaginal temperature training in which the subjects’ vaginal temperature increased by .27 F degrees.
- Progressive muscle relaxation developed by Edmund Jacobson in the 1920s and imagery are effective treatments for dysmenorrhea (Aldinda et al., 2022; Chesney & Tasto, 1975; Çelik, 2021; Jacobson, 1938; Proctor et al., 2007).
- Rhythmic abdominal massage as compared to non-treatment reduces dysmenorrhea symptoms (Suryantini, 2022; Vagedes et al., 2019):
- Biofeedback strategies such as frontalis electromyography feedback (EMG) and peripheral temperature training (Hart, Mathisen, & Prater, 1981); trapezius EMG training (Balick et al, 1982); lower abdominal EMG feedback training and relaxation (Bennink, Hulst, & Benthem, 1982); and integrated temperature feedback and autogenic training (Dietvorts & Osborne, 1978) all successfully reduced the symptoms of dysmenorrhea.
- Breathing relaxation for 5 to 30 minutes resulted in a decrease in pain or the pain totally disappeared in adolescents (Hidayatunnafiah et al., 2022). While slow deep breathing in combination with abdominal massage is more effective than applying hot compresses (Ariani et al., 2020). Slow pranayama (Nadi Shodhan) breathing the quality of life and pain scores improved as compared to fast pranayama (Kapalbhati) breathing and improved quality of life and reduces absenteeism and stress levels (Ganesh et al. 2015). When students are taught slow diaphragmatic breathing, many report a reduction in symptoms compared to the controls (Bier et al., 2005).
Observations from Integrated stress management program
This study reports on changes in dysmenorrhea symptoms by students enrolled in a University Holistic Health class that included homework assignment for practicing stress awareness, dynamic relaxation, and breathing with imagery.
Respondents: 32 college women, average age 24.0 years (S.D. 4.5 years)
Procedure: Students were enrolled in a three-unit class in which they were assigned daily home practices which changed each week as described in the book, Make Health Happen (Peper, Gibney & Holt, 2002). The first five weeks consisted of the following sequence: Week 1 focused on monitoring one’s reactions to stressor; week 2 consisted of daily practice for 30 minutes of a modified progressive relaxation and becoming aware of bracing and reducing the bracing during the day; Week 3 consisted of practicing slow diaphragmatic breathing for 30 minutes a day and during the day becoming aware of either breath holding or shallow chest breath and then use that awareness as cue to shift to lower slower diaphragmatic breathing; week 4 focused on evoking a memory of wholeness and relaxing; and week 5 focused on learning peripheral hand warming.
During the class, students observed lectures about stress and holistic health and met in small groups to discuss their self-regulation experiences. During the class discussion, some women discussed postures and practices that were beneficial when experiencing menstrual discomfort, such as breathing slowly while lying on their back, focusing on slow abdominal awareness in which their abdomen expanded during inhalation and contracted during exhalation. While exhaling they focused on imagining a flow of air initially going through their arms and then through their abdomen, down their legs and out their feet. This kinesthetic feeling was enhanced by first massaging down the arm while exhaling and then massaging down their abdomen and down their thighs when exhaling. In most cases, the women also experienced that their hands and feet warmed. In addition, they were asked to shift to slower diaphragmatic breathing whenever they observed themselves gasping, shallow breathing or holding their breath. After five weeks, the students filled out a short assessment questionnaire in which they rated the change in dysmenorrhea symptoms since the beginning of the class.
Results.
About two-thirds of all respondents reported a decrease in overall discomfort symptoms. In addition to any ‘treatment as usual’ (TAU) strategies already being used (e.g. medications or other treatments such as NSAIDs or birth control pills), 91% (20 out 22 women) who reported experiencing dysmenorrhea reported a decrease in symptoms when they practiced the self-regulation and diaphragmatic breathing techniques as shown in Figure 1.

Figure 1. Self-report in dysmenorrhea symptoms after 5 weeks.
Discussion
Many students reported that their symptoms were significantly reduced and they could be more productive. Generally, the more they practiced the relaxation and breathing self-regulation skills, the more they experienced a decrease in symptoms. The limitation of this report is that it is an observational study; however, the findings are similar to those reported by earlier self-care and biofeedback approaches. This suggests that women should be taught the following simple self-regulation strategies as the first intervention to prevent and when they experience dysmenorrhea symptoms.
Why would breathing reduce dysmenorrhea?
Many women respond by ‘curling up’ a natural protective defense response when they experience symptoms. This protective posture increases abdominal and pelvic muscle tension, inhibits lymph and blood flow circulation, increases shallow breathing rate, and decreases heart rate variability. Intentionally relaxing the abdomen with slow lower breathing when lying down with the legs extended is often the first step in reducing discomfort.
By focusing on diaphragmatic breathing with relaxing imagery, it is possible to restore abdominal expansion during inhalation and slight constriction during exhalation. This dynamic breathing while lying supine would enhance abdominal blood and lymph circulation as well as muscle relaxation (Peper et al., 2016). While practicing, participants were asked to wear looser clothing that did not constrict the waist to allow their abdomen to expand during inhalation; since, waist constriction by clothing (designer jean syndrome) interferes with abdominal expansion. Allowing the abdomen to fully extend also increased acceptance of self, that it was okay to let the abdomen expand instead of holding it in protectively. The symptoms were reduced most likley by a combination of the following factors.
- Abdominal movement is facilitated during the breathing cycle. This means reducing the factors that prevent the abdomen expanding during inhalation or constricting during exhalation (Peper et al., 2016).
- Eliminate‘Designer jean syndrome’ (the modern girdle). Increase the expansion of your abdomen by loosening the waist belt, tight pants or slimming underwear (MacHose & Peper, 1991).
- Accept yourself as you are. Allow your stomach to expand without pulling it in.
- Free up learned disuse: Allow the abdomen to expand and constrict instead of inhibiting movement to avoid pain that occurred following a prior abdominal injury/surgery (e.g., hernia surgery, appendectomy, or cesarean operation), abdominal pain (e.g., irritable bowel syndrome, recurrent abdominal pain, ulcers, or acid reflux), pelvic floor pain (e.g., pelvic floor pain, pelvic girdle pain, vulvodynia, or sexual abuse).
- The ‘defense response’ is reduced. Many students described that they often would curl up in a protective defense posture when experiencing menstrual cramps. This protective defense posture would maintain pelvic floor muscle contractions and inhibit blood and lymph flow in the abdomen, increase shallow rapid thoracic breathing and decrease pCO2 which would increase vasoconstriction and muscle constriction (Peper et al., 2015; Peper et al., 2016). By having the participant lie relaxed in a supine position with their legs extended while practicing slow abdominal breathing, the pelvic floor and abdominal wall muscles can relax and thereby increase abdominal blood and lymph circulation and parasympathetic activity. The posture of lying down implies feeling safe which is a state that facilitates healing.
- The pain/fear cycle is interrupted. The dysmenorrhea symptoms may trigger more symptoms because the person anticipates and reacts to the discomfort. The breathing and especially the kinesthetic imagery where the attention goes from the abdomen and area of discomfort to down the legs and out the feet acts as a distraction technique (not focusing on the discomfort).
- Support sympathetic-parasympathetic balance. The slow breathing and kinesthetic imagery usually increases heart rate variability and hand and feet temperature and supports sympathetic parasympathetic balance.
- Interrupt the classical conditioned response of the defense reaction. For some young girls, the first menstruation occurred unexpectedly. All of a sudden, they bled from down below without any understanding of what is going on which could be traumatic. For some this could be a defense reaction and a single trial condition response (somatic cues of the beginning of menstruation triggers the defense reaction). Thus, when the girl later experiences the initial sensations of menstruation, the automatic conditioned response causes her to tense and curl up which would amplify the discomfort. Informal interviews with women suggests that those who experienced their first menstruation experience as shameful, unexpected, or traumatic (“I thought I was dying”) thereafter framed their menstruation negatively. They also tended to report significantly more symptoms than those women who reported experiencing their first menstruation positively as a conformation that they have now entered womanhood.
How to integrate self-care to reduce dysmenorrhea
Be sure to consult your healthcare provider to rule out treatable underlying conditions before implementing learning effortless diaphragmatic breathing.
- Allow the abdomen to expand during inhalation and become smaller during exhalation. This often means, loosen belt and waist constriction, acceptance of allowing the stomach to be larger and reversing learned disuse and protective response caused by stress.
- Master diaphragmatic breathing (see: Peper & Tibbetts, 1994 and the blogs listed at the end of the article).
- Practice slow effortless diaphragmatic breathing lying down with warm water bottle on stomach in a place that feels safe.
- Include kinesthetic imagery as you breathe at about 6 breaths per minute (e.g. slowly inhale for 4 or 5 seconds and then exhale for 5 or 6 seconds, exhaling slightly longer than inhaling). Imaging that when you exhale you can sense healing energy flow through your abdomen, down the legs and out the feet.
- If possible, integrate actual touch with the exhalation can provide added benefit. Have a partner first stroke or massage down the arms from the shoulder to your fingertips as you exhale and, then on during next exhalation stroke gently from your abdomen down your legs and feet. Stroke in rhythm the exhalation.
- Exhale slowly and shift to slow and soft diaphragmatic breathing each time you become aware of neck and shoulder tension, breath holding, shallow breathing, or anticipating stressful situations. At the same time imagine /sense when exhaling a streaming going through the abdomen and out the feet when exhaling. Do this many times during the day.
- Practice and apply general stress reduction skills into daily life since stress can increase symptoms. Anticipate when stressful event could occur and implement stress reducing strategies.
- Be respectful of the biological changes that are part of the menstrual cycle. In some cases adjust your pace and slow down a bit during the week of the menstrual cycle; since, the body needs time to rest and regenerate. Be sure to get adequate amount of rest, hydration, and nutrition to optimize health.
- Use self-healing imagery and language to transform negative association with menstruation to positive associations (e.g., “curse” to confirmation “I am healthy”).
Conclusion
There are many ways to alleviate dysmenorrhea. Women can find ways to anticipate and empower themselves by practicing stress reduction, wearing more comfortable clothing, using heat compression, practicing daily diaphragmatic breathing techniques, visualizing relaxed muscles, and positive perception towards menstrual cycles to reduce the symptoms of dysmenorrhea. These self-regulation methods should be taught as a first level intervention to all young women starting in middle and junior high school so that they are better prepared for the changes that occur as they age.
“I have been practicing the breathing techniques for two weeks prior and I also noticed my muscles, in general, are more relaxed. Of course, I also avoided the skinny jeans that I like to wear and it definitely helped.
I have experienced a 90% improvement from my normal discomfort. I was still tired – and needed more rest and sleep but haven’t experienced any “terrible” physical discomfort. Still occasionally had some sharp pains or bloating but minor discomfort, unlike some days when I am bedridden and unable to move for half a day. – and this was a very positive experience for me “ — Singing Chen (Chen, 2023)
Useful blogs to learn diaphragmatic breathing
References
Aldinda, T. W., Sumarni, S., Mulyantoro, D. K., & Azam, M. (2022). Progressive muscle relaxation application (PURE App) for dysmenorrhea. Medisains Jurnal IlmiahLlmiah LLmu-LLmu Keshatan, 20(2), 52-57. https://doi.org/10.30595/medisains.v20i2.14351
Ariani, D., Hartiningsih, S.S., Sabarudin, U. Dane, S. (2020). The effectiveness of combination effleurage massage and slow deep breathing technique to decrease menstrual pain in university students. Journal of Research in Medical and Dental Science, 8(3), 79-84. https://www.jrmds.in/articles/the-effectiveness-of-combination-effleurage-massage-and-slow-deep-breathing-technique-to-decrease-menstrual-pain-in-university-stu-53607.html
Armour, M., Parry, K., Manohar, N., Holmes, K., Ferfolja, T., Curry, C., MacMillan, F., & Smith, C. A. (2019). The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. Journal of women’s health, 28(8), 1161-1171.https://doi.org/10.1089/jwh.2018.7615
ASPH. (2023). Estrogen and Progestin (Oral Contraceptives). MedlinePlus. Assessed March 3, 2023. https://medlineplus.gov/druginfo/meds/a601050.html
Balick, L., Elfner, L., May. J., Moore, J.D. (1982). Biofeedback treatment of dysmenorrhea. Biofeedback Self Regul, 7(4), 499-520. https://doi.org/10.1007/BF00998890
Bennink, C.D., Hulst, L.L. & Benthem, J.A. (1982). The effects of EMG biofeedback and relaxation training on primary dysmenorrhea. J Behav Med, 5(3), 329-341.https://doi.org/10.1007/BF00846160
Bier, M., Kazarian, D. & Peper, E. (2005). Reducing PMS through biofeedback and breathing. Poster presentation at the 36th Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract published in: Applied Psychophysiology and Biofeedback. 30 (4), 411-412.
Çelik, A.S. & Apay, S.E. (2021). Effect of progressive relaxation exercises on primary dysmenorrhea in Turkish students: A randomized prospective controlled trial. Complement Ther Clin Pract, Feb 42,101280. https://doi.org/10.1016/j.ctcp.2020.101280
Chen, S. (2023). Diaphragmatic breathing reduces dysmenorrhea symptoms-a testimonial. YouTube. Accessed March 3, 2023. https://youtu.be/E45iGymVe3U
De Sanctis, V., Soliman, A., Bernasconi, S., Bianchin, L., Bona, G., Bozzola, M., Buzi, F., De Sanctis, C., Tonini, G., Rigon, F., & Perissinotto, E. (2015). Primary Dysmenorrhea in Adolescents: Prevalence, Impact and Recent Knowledge. Pediatr Endocrinol Rev. 13(2), 512-20. PMID: 26841639. https://pubmed.ncbi.nlm.nih.gov/26841639/
De Sanctis, V., Soliman, A. T., Daar, S., Di Maio, S., Elalaily, R., Fiscina, B., & Kattamis, C. (2020). Prevalence, attitude and practice of self-medication among adolescents and the paradigm of dysmenorrhea self-care management in different countries. Acta Bio Medica: Atenei Parmensis, 91(1), 182. https://doi.org/10.23750/abm.v91i1.9242
Dietvorst, T.F. & Osborne, D. (1978). Biofeedback-Assisted Relaxation Training
for Primary Dysmenorrhea: A Case Study. Biofeedback and Self-Regulation, 3(3), 301-305. https://doi.org/10.1007/BF00999298
Chesney, M. A., & Tasto, D. L. (1975).The effectiveness of behavior modification with spasmodic and congestive dysmenorrhea. Behaviour Research and Therapy, 13, 245-253. https://doi.org/10.1016/0005-7967(75)90029-7
Ganesh, B.R., Donde, M.P., & Hegde, A.R. (2015). Comparative study on effect of slow and fast phased pranayama on quality of life and pain in physiotherapy girls with primary dysmenorrhea: Randomize clinical trial. International Journal of Physiotherapy and Research, 3(2), 960-965. https://doi.org/10.16965/ijpr.2015.115
Hart, A.D., Mathisen, K.S. & Prater, J.S. A comparison of skin temperature and EMG training for primary dysmenorrhea. Biofeedback and Self-Regulation 6, 367–373 (1981). https://doi.org/10.1007/BF01000661
Heczey, M. D. (1978). Effects of biofeedback and autogenic training on menstrual experiences: relationship among anxiety, locus of control and dysmenorrhea. City University of New York ProQuest Dissertations Publishing, 7805763. https://www.proquest.com/openview/088e0d68511b5b59de1fa92dec832cc8/1?pq-origsite=gscholar&cbl=18750&diss=y
Hidayatunnafiah, F., Mualifah, L., Moebari, M., & Iswantiningsih, E. (2022). The Effect of Relaxation Techniques in Reducing Dysmenorrhea in Adolescents. The International Virtual Conference on Nursing. in The International Virtual Conference on Nursing, KnE Life Sciences, 473–480. https://doi.org/10.18502/kls.v7i2.10344
Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H.M.J. (2022). Primary Dysmenorrhea: Pathophysiology, Diagnosis, and Treatment Updates. Korean J Fam Med, 43(2), 101-108. https://doi.org/10.4082/kjfm.21.0103
Jacobson, E. (1938). Progressive Relaxation: A Physiological and Clinical Investigation of Muscular States and Their Significance in Psychology and Medical Practice. Chicago: University of Chicago Press
Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiol Rev, 36, 104-13. https://doi.org/10.1093/epirev/mxt009
Karout, S., Soubra, L., Rahme, D. et al. Prevalence, risk factors, and management practices of primary dysmenorrhea among young females. BMC Women’s Health 21, 392 (2021). https://doi.org/10.1186/s12905-021-01532-w
Iacovides, S., Avidon,I, & Baker, F.C. (2015).What we know about primary dysmenorrhea today: a critical review, Human Reproduction Update, 21(6), 762–778. https://doi.org/10.1093/humupd/dmv039
Luthe, W. & Schultz, J.H. (1969). Autogenic Therapy, Volume II Medical Applications. New York: Grune & Stratton, pp144-148.
MacHose, M. & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. ISBN: 978-0787293314 https://he.kendallhunt.com/make-health-happen
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. Also in: Electromyography: Applications in Physical Therapy. Montreal: Thought Technology Ltd. https://biofeedbackhealth.files.wordpress.com/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Proctor, M. & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ. 13, 332(7550), 1134-8. https://doi.org/10.1136/bmj.332.7550
Proctor, M.L, Murphy, P.A., Pattison, H.M., Suckling, J., & Farquhar, C.M. (2007). Behavioural interventions for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev, (3):CD002248. https://doi.org/10.1002/14651858.CD002248.pub3
Suryantini, N. P. (2022). Effleurage Massage: Alternative Non-Pharmacological Therapy in Decreasing Dysmenorrhea Pain. Women, Midwives and Midwifery, 2(3), 41-50. https://wmmjournal.org/index.php/wmm/article/view/71/45
Thakur, P. & Pathania, A.R. (2022). Relief of dysmenorrhea – A review of different types of pharmacological and non-pharmacological treatments. MaterialsToday: Proceedings.18, Part 5, 1157-1162. https://doi.org/10.1016/j.matpr.2021.08.207
Vagedes, J., Fazeli, A., Boening, A., Helmert, E., Berger, B. & Martin, D. (2019). Efficacy of rhythmical massage in comparison to heart rate variability biofeedback in patients with dysmenorrhea—A randomized, controlled trial. Complementary Therapies in Medicine, 42, 438-444. https://doi.org/10.1016/j.ctim.2018.11.009
Vonkeman, H.E. & van de Laar, M,A. (2010). Nonsteroidal anti-inflammatory drugs: adverse effects and their prevention, Semin Arthritis Rheum, 39(4), 294-312. https://doi.org/10.1016/j.semarthrit.2008.08.001
Wang, L., Wand, X., Wang, W., Chen, C. Ronnennberg, A.G., Guang, W. Huang, A. Fang, Z. Zang, T., Wang, L. & Xu, X. (2003).Stress and dysmenorrhoea: a population based prospective study. Occupation and Environmental Medicine, 61(12). http://dx.doi.org/10.1136/oem.2003.012302
Bring joy through kindness
Posted: December 31, 2022 Filed under: behavior, healing, meditation, mindfulness | Tags: generousity, kindness Leave a commentAs the New Year begins, bring support through simple acts of kindness. As we share generously, our own well-being improves. I wish you health, happiness and peace for the New Year. Enjoy the two videos on simple acts of kindness.
Healing chronic back pain
Posted: July 31, 2022 Filed under: behavior, Breathing/respiration, CBT, cognitive behavior therapy, education, healing, health, meditation, relaxation, self-healing, stress management, surgery | Tags: back pain, Imagery, self-care, visualization 4 CommentsErik Peper, PhD, BCB, Jillian Cosby, and Monica Almendras
Adapted from Peper, E. Cosby, J. & Amendras, M. (2022).Healing chronic back pain. NeuroRegulation, 9(3), 165-172. https://doi.org/10.15540/nr.9.3.164

In at the beginning of 2021, I broke my L3 vertebra during a motor cycle accident and underwent two surgeries in which surgeons replaced my shattered L3 with a metal “cage” (looks like a spring) and fused this cage to the L4 and L2 vertebrae with bars. I also broke both sides of my jaw and fractured my left shoulder. I felt so overwhelmed and totally discouraged by the ongoing pain. A year later, after doing the self-healing project as part of the university class assignment, I feel so much better all the time, stopped taking all prescription pain medications and eliminated the sharp pains in my back. This project has taught me that I have the skill set needed to be whole and healthy. –J.C., 28-year-old college student
Chronic pain is defined as a pain that persist or recurs for more than 3 months (Treede et al., 2019). It is exhausting and often associated with reduced quality of life and increased medical costs (Yong, Mullins, & Bhattacharyya, 2022). Pain and depression co-exacerbate physical and psychological symptoms and can lead to hopelessness (IsHak, 2018; Von Korff & Simon, 1996). To go to bed with pain and anticipate that pain is waiting for you as you wake up is often debilitating. One in five American adults experience chronic pain most frequently in back, hip, knee or foot (Yong, Mullins, & Bhattacharyya, 2022). Patients are often prescribed analgesic medications (“pain killers”) to reduce pain. Although, the analgesic medications can be effective in the short term to reduce pain, the efficacy is marginal for relieving chronic pain (Eriksen et al., 2006; Tan, & Jensen, 2007). Recent research by Parisien and colleagues (2022) reported that anti-inflammatory drugs were associated with increased risk of persistent pain. This suggest that anti-inflammatory treatments might have negative effects on pain duration. In addition, the long-term medication use is a major contributor to opioid epidemic and increased pain sensitivity (NIH– NIDA, 2022; Higgins, Smith, & Matthews, 2019; Koop, 2020). Pain can often be successfully treated with a multidisciplinary approach that incorporates non-pharmacologic approaches. These include exercise, acceptance and commitment therapy, as well as hypnosis (Warraich, 2022). This paper reports how self-healing strategies as taught as part of an undergraduate university class can be an effective approach to reduce the experience of chronic pain and improve health.
Each semester, about 100 to 150 junior and senior college students at San Francisco State University enroll in a holistic health class that focused on ‘whole-person’ Holistic Health curriculum. The class includes an assessment of complementary medicine and holistic health. It is based upon the premise that mind/emotions affect body and body affect mind/emotions that Green, Green & Walters (1970) called the psychophysiological principle.
“Every change in the physiological state is accompanied by an appropriate change in the mental emotional state, conscious or unconscious, and conversely, every change in the mental emotional state, conscious or unconscious, is accompanied by an appropriate change in the physiological state.”
The didactic components of the class includes the psychobiology of stress, the role of posture, psychophysiology of respiration, lifestyle and other health factors, reframing internal language, guided and self-healing imagery. Students in the class are assigned self-healing projects using techniques that focus on awareness of stress, dynamic regeneration, stress reduction imagery for healing, and other behavioral change techniques adapted from the book, Make Health Happen (Peper, Gibney, & Holt, 2002).
The self-practices during the last six weeks of the class focus on identifying, developing and implementing a self-healing project to optimize their personal health. The self-healing project can range from simple life style changes to reducing chronic pain. Each student identifies their project such as increasing physical activity, eating a healthy diet and reducing sugar and junk food, stopping vaping/smoking, reducing anxiety or depression, stopping hair pulling, reducing headaches, decreasing ezema, or back pain, etc. At the end of the semester, 80% or more of the students report significant reduction in symptoms (Peper, Sato-Perry, & Gibney, 2003; Peper, Lin, Harvey, Gilbert, Gubbala, Ratkovich, & Fletcher, 2014; Peper, Miceli, & Harvey, 2016; Peper, Harvey, Cuellar, & Membrila, 2022). During the last five semesters, 13 percent of the students focused reducing pain (e.g., migraines, neck and shoulder pain, upper or lower back pain, knee pain, wrist pain, and abdominal pain). The students successfully improved their symptoms an average of 8.8 on a scale from 0 (No benefit) to 10 (total benefit/improvement). The success for improving their symptoms correlates 0.63 with their commitment and persistence to the project (Peper, Amendras, Heinz, & Harvey, in prep).
The purposes of this paper is to describe a case example how a student with severe back pain reduced her symptoms and eliminated medication by implementing an integrated self-healing process as part of a class assignment and offer recommendations how this could be useful for others.
Participant: A 28-year-old female student (J.C.) who on January 28, 2021 broke her L3 vertebra in a motor cycle accident. She underwent two surgeries in which surgeons replaced her shattered L3 with a metal “cage” (which she describes as looking like a spring) and fused this cage to the L2 and L4 vertebrae with bars. She also broke both sides of her jaw and fractured her left shoulder. More than a year later, at the beginning of the self-healing project, she continue to take 5-10 mgs of Baclofen and 300 mgs of Gabapentin three times a day to reduce pain.
Goal of the self-healing project: To decrease the sharp pain/discomfort in her lower back that resulted from the motor cycle accident and, although not explicitly listed, to decrease the pain medications.
Self-healing process
During the last six weeks of the 2022 Spring semester, the student implemented her self-healing practices for her personal project which consisted of the following steps.
1. Create a self-healing plan that included exploring the advantage and disadvantage of her illness.
2. Develop a step-by-step plan with specific goals to relief her tension and pain in her lower back. This practice allowed her to quantify her problem and the solutions. Like so many people with chronic pain, she focused on the problem and feelings (physical and emotional) associated with the pain. As a result, she often feel hopeless and worried that it would not change.
3. Observe and evaluate when pain sensations changed. She recognized that she automatically anticipated and focused on the pain and anxiety whenever she needed to bend down into a squat. She realized that she had been anticipating pain even before she began to squat. This showed that she needed to focus on healing the movement of this area of her body.
Through her detailed observations, she realized that her previous general rating of back pain could be separated into muscle tightness/stiffness and pain. With this realization, she changed the way she was recording her pain level. She changed it from “pain level” into into two categories: tightness and sharp pains.
4. Ask questions of her unconscious through a guided practice of accessing an inner guide through imagery (For detailed instructions, see Peper, Gibney, & Holt, 2002, pages 197-206). In this self-guided imagery the person relaxes and imagines being in a special healing place where you felt calm, safe and secure. Then as you relaxed, you become aware of another being (wise one or guide) approaching you (the being can be a person, animal, light, spirit, etc.). The being is wise and knows you well. In your mind, you ask this being or guide questions such as, “What do I need to do to assist in my own healing?” Then you wait and listen for an answer. The answer may take many forms such as in words, a pictures, a sense of knowing, or it may come later in dreams or in other forms. When students are assigned this practice for a week, almost all report experiencing some form of guide and many find the answers meaningful for their self-healing project.
Through this imagery of the inner guide script, she connected with her higher self and the wise one told her to “Wait.” This connecting with the wise one was key in accepting that the project was not as daunting as she initially thought. She realized that pain was not going to be forever in her future. She also interpreted that as reminder to have patience with herself. Change takes practice, time and practice such as she previously experienced while correcting her posture to manage her emotions and edit her negative thoughts into positive ones (Peper, Harvey, Cuellar, & Membrila, 2022). Whenever she would have pain or feel discouraged because of external circumstances, she would remind herself of three things:
A. I need to have patience with myself.
B. I have all the healing tools inside me and I am learning to use them.
C. If I do not make time for my wellness, I’ll be forced to make time for my illness.
5. Practice self-healing imagery as described by Peper, Gibney, & Holt (2002) and adapted from the work by Dr. Martin Rossman (Rossman, 2000). Imagery can be the communication channel between the conscious/voluntary and the unconscious/autonomic/involuntary nervous system (Bressler, 2005; Hadjibalassi et al, 2018; Rossman, 2019). It appears to act as the template and post-hypnotic suggestion to implement behavior change and may offer insight and ways to mobilize the self-healing potential (Battino, 2020). Imagery is dynamic and changeable.
The process of self-healing imagery consists of three parts.
- Inspection the problem and drawing a graphic illustration of the problem as it is experienced at that moment of time.
- Drawing of how that area/problem would look when being completely well/whole or disappeared.
- Creation of a self-healing process by which the problem would become transformed into health (Peper, Gibney & Holt, 2002, pp. 217-236). The process focused on what the person could do for themselves; namely, each time they became aware of, anticipated, or felt the problem, they would focus on the self-healing process. It provideshope; since, the person now focuses on the healing of the problem and becoming well.
The drawings of inspection of the pain and problem she experienced at that moment of time are shown in Figure 1.

Figure 1. Illustration of the problem of the pain. Thorns dug deep, muscles tight, and frozen vertebrates grinding.
The resolution of the problem and being well/whole are illustrated in Figure 2.

Figure 2. Resolution of the problem in which her muscles are warm, full of blood, free of thorns, relaxed and flexible and being whole happy and healthy in which her spine is warm, her muscles are warm, her back is flexible and full of movement.
Although she utilized the first image of the muscles warm, full of blood, free of thorns and the muscles relaxed and flexible, her second image of her fully being healed was inspired through a religious statue of Yemaya that she had in her room (Yemaya is a major water spirit from the Yoruba religion Santeria and Orisha of the seas and protector of women). Each time she saw the statue, she thought of the image of herself fully healed and embodying the spirit Orisha. Therefore, this image remained important to her all the time.
Her healing imagery process by which she transforms the image of inspecting of the problem to being totally well are illustrated in Figure 3.

Figure 3. The healing process: The sun’s warm fingers thaw my muscles, lubricate my vertebra, thorns fall out, and blood returns.
For five weeks as she implemented her self-healing project by creating a self-healing plan, asking questions of her unconscious, drawing her self-healing imagery. She also incorporated previously learned skills from the first part of the semester such diaphragmatic breathing, hand warming, shifting slouching to upright posture, and changing language. Initially she paired hand warming with the self-healing imagery and she could feel an increase in body warmth each time she practiced the imagery. She practiced the self-healing imagery as an in-depth daily practice and throughout the day when she became aware of her back as described in one of her log entries.
I repeated the same steps as the day prior today. I did my practice in the early morning but focused on the details of the slowed down movements of the sun’s hands. I saw them as they stretched out to my back, passed through my skin, wrapped around my muscles, and began to warm them. I focused on this image and tried to see, in realistic detail, my muscles with a little ice still on them, feeling hard through and through, the sun’s glowing yellow-orange fingers wrapped around my muscles. I imaged the thorns still in my muscles, though far fewer than when I started, and then I imaged the yellow-orange glow start to seep out from the sun’s palms and fingers and spread over my muscles. I imaged the tendons developing as the muscle tissue thawed and relaxed, the red of the muscle brightened, the ice on and within my muscles started to melt, and the condensation formed as it ran down into collected droplets at the bottom of my muscles. I imaged the thorns lose their grip and fall out, one at a time, in tandem with the droplets falling. I continued this process and imaged my muscles expanding with warmth and relaxation as they stayed engulfed in the warmth of the sun.
At the end of my practice, I did a small stretch session. I felt extremely refreshed and ready for yet another extremely busy day between internship, graduation, and school. I would say I felt warm and relaxed all the way into the afternoon, about 6 hours after my practice. This was by far the most detailed and impactful imagery practice I have had.
The self-healing imagery practice provided me with the ability to conceptualize more than my problem as it showed me the tools to (and the importance of) conceptualizing my solution, both the tool and end result.
Results
Pain and tightness decreased and she stopped her medication by the third week as shown in Figure 4.

Figure 4. Self-rating of sharp pains and tightness during the self-healing project.
At the 14-week follow-up, she has continued to improve, experiences minimal discomfort, and no longer takes medication. As she stated, I was so incredibly shocked how early on [in the project] I was able to stop taking pain medications that I had already taken every day for over a year.
Discussion
This individual case example provides hope that health can be improved when shifting the focus from pain and discomfort to focusing on actively participating in the self-healing process. As she wrote, The lesson was self- empowerment in regard to my health. I brought comfort to my back. There is metal in my back for the rest of my life and this is something I have accepted. I used to look at that as a horrible thing to have to handle forever. I now look at it as a beautiful contraption that has allowed me to walk across a graduation stage despite having literally shattered a vertebra. I am reintegrating these traumatized parts of my body back into a whole health state of mind and body. Doctors did not do this, surgeries did not, PT didn’t and neither did pain medications. MY body and MY mind did it. I did this.
Besides the self-healing imagery and acting upon the information she received from the asking questions from the unconscious there were many other factors contributed to her healing. These included the semester long self-practices and mastery of different stress management techniques, learning how stress impacts health and what can the person can do to self-regulate, as well as being introduced to the many case examples and research studies that suggested healing could be possible even in cases where it seemed impossible.
The other foundational components that was part of the class teachings included attending the weekly classes session and completing the assign homework practices. These covered discussion about placebo/nocebo, possibilities and examples of self-healing with visualization, the role of nutrition, psychophysiology of stress and factors are associated with healthy aging across cultures. The asynchronous assignments investigated factors that promoted or inhibited health and the role of hope. The discussions pointed out that not everyone may return to health; however, they can always be whole. For example, if a person loses a limb, the limb will not regrow. The healing process includes acceptance and creating new goals to achieve and live a meaningful life.
The possibility that students could benefit by implementing the different skills and concepts taught in the class were illustrated by sharing previous students’ successes in reversing disorders such as hair pulling, anxiety, psoriasis, and pain. In addition, students were assigned to watch and comment on videos of people who had overcome serious illness. These included Janine Shepherd’s 2012 TED talk, A broken body isn’t a broken person, and Dr. Terry Wahl’s 2011 TEDxIowaCity talk, Minding your mitochondria. Janine Shepard shared how she recovered from a very serious accident in which she became paralyzed to becoming an aecrobatic pilot instructor while Dr. Terry Wahl shares how she he used diet to cure her MS and get out of her wheelchair (Shepherd, 2012; Wahl, 2011). Other assignments included watching Madhu Anziani’s presentation, Healing from paralysis-Music (toning) to activate health, in which he discussed his recovery from being a quadriplegic to becoming an inspirational musician (Anziani, & Peper, 2021). The students as read and commented on student case examples of reversing acid reflux, irritable bowel and chronic headaches (Peper, Mason, & Huey, 2017a; Peper, Mason, & Huey, 2017b; Peper, 2018; Peper et al., 2020; Peper, Covell, & Matzembacker, 2021; Peper, 2022).
Although self-healing imagery appears to be the major component that facilitated the healing, it cannot be separated from the many other concepts and practices that may have contributed. For example, the previous practices of learning slow diaphragmatic breathing and hand warming may have allowed the imagery to become a real kinesthetic experience. In addition, by seeing how other students overcame chronic disorders, the class provided a framework to mobilize one’s health.
Lessons extracted from this case example that others may be able use to mobilize health.
- Take action to shifts from being hopeless and powerless to becoming empowered and active agent in the healing process.
- Change personal beliefs through experiential practices and storytelling that provides a framework that healing and improvement are possible.
- Teach the person self-regulation skills such as slower breathing, muscle relaxation, cognitive internal language changes, hand warming by which the person experiences changes.
- Provide believable role models who shared their struggle in overcoming traumatic injury, watch inspirational talks, and share previous clients or students’ self-reports who had previously improved.
- Transform the problem from global description into behavioral specific parts. For example, being depressed is a global statement and too big to work on. Breaking the global concept into specific behaviors such as, my energy is too low to do exercise or I have negative thoughts, would provide specific interventions to work on such as, increasing exercise or changing thoughts. In JC’s case, she changed the general rating of pain into ratings of muscle tightness and sharp pains. This provided the bases for strategies to relax and warm her muscles.
- Focus on what you can do at that moment versus focusing on the past, what happened, who caused it, or blaming yourself and others. Explore and ask what you now can do now to support your healing process and reframe the problem as a new opportunity for growth and development.
- Practice, practice, and practice with a childlike exploratory attitude. Focus on the small positive benefits that occur as a result of the practices. It is not mindless practice; it is practice while being present and being gentle with yourself. Do not discard very small changes. The benefits accrue as you practice more and more, just many people have experienced when learning to play a musical instrument or mastering a sport. Even though many participants think that practicing 15 minutes a day is enough, it usually takes much more time. Reflect on how a baby learns to walk or climb. The toddler practices day-long and takes naps to regenerate and grow. When the toddler is not yet successful in walking or climbing, it does not give up or interpret it as failure or blaming himself that he cannot do it, it just means more practice.
- Have external reminders to evoke the self-healing practices. In JC’s case, the small statue of Yemaya in her room was the reminder. It reminded her to thinks of the image of herself fully healed each time she saw it.
- Guide yourself through the wise one imagery, ask yourself a question and listen and act on the intuitional answers.
- Develop a self-healing imagery process that transforms the dysfunction to health or wholeness. Often the person only perceives the limitations and focusses on describing the problem. Instead, acknowledge, accept what was and is, and focus on developing a process to promote healing. What many people do not realize that if they think/imagine how their injury/illness was caused, it may reactivate and recreate the initial trauma. This can be illustrated through imagery. When we think or imagine something, it changes our physiology. For example, when one imagines eating a lemon, many people will salivate. The image affects physiology. Thus, focus on processes that support healing.
- While practicing the imagery, experience it as if it is real and feel it happening inside yourself. Many people initially find this challenging as they see it outside themselves. One way to increase the “felt sense” is to incorporate more body involvement such as acting out the imagery with hand and body movements.
- When having a relapse, remind yourself to keep going. Every morning is the beginning of a new day, do each practices anew. In addition, reflect of something that was challenging in the past but that you successfully overcame. Focus on that success. As JC wrote, I was also successful in that I gave myself slack and reminded myself that relapses will happen and what matters more is the steps I take to move forward.
- Make your healing a priority that means doing it often during the day. Allow the self-healing imagery and process to run in the back of the head all the time just as a worry can be present in the background. So often people practice for a few minutes (which is great and better than not practicing at all); however, at other times during the day they are captured by their worry, negative thoughts or focus on the limitations of the disorder. When a person focuses on the limitations, it may interrupt the self-healing process. The analogy we often use is that the healing process is similar to healing from a small cut in the skin. Initially a scab forms and eventually the scab falls off and the skin is healed. On the other hand, if you keep moving the skin or pick on the scab, healing is much slower. By focusing on the limitations and past visualization of the injury, self-healing is reduced. This is similar to removing the scab before the skin has healed. As JC stated, “If you don’t make time for your wellness, you’ll be forced to make time for your illness” was 100% a motivating factor in my success.
- Explore resources for providers and people living with pain. See Dr. Rachel Zoffness website which provides a trove of high quality articles, books, videos, apps, and podcasts. https://www.zoffness.com/resources
In summary, we do not know the limits of self-healing; however, this case example illustrates that by implementing self-healing strategies health and recovery occurred. As JC wrote:
To have broken a vertebra in my back and experience all the injuries that came with the accident when I already did not have the strongest mind-body connection was incredibly intense and really heartbreaking and discouraging in my life. And, that made things difficult because I was not able to 100% focus on my healing because I felt so overwhelmed by the feeling of discouragement that I felt. Experiencing this self-healing project, seeing the imagery that helped me not just feel so much better all the time but be able to stop taking all prescription pain medications and eliminate the sharp pains in my back has taught me that I have the skill set needed to be whole and healthy.
Watch the interview will Jillian Cosby inwhich she describes her self-healing process.
References
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. The peperperspective. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Battino, R. (2020). Using Guided Imagery and Hypnosis in Brief Therapy and Palliative Care. New York: Routledge.
Bresler, D. (2005).Physiological Consequences of Guided Imagery. Pract Pain Manag, 5(6). https://www.practicalpainmanagement.com/treatments/complementary/biobehavioral/physiological-consequences-guided-imagery
Eriksen, J., Sjøgren, P., Bruera, E., et al. (2006). Critical issues on opioids in chronic non-cancer pain: An epidemiologic study. Pain, 125,172–179. https://doi.org/10.1016/j.pain.2006.06.009
Green, E. E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological. The Journal of Transpersonal Psychology, 2(1), 1. https://atpweb.org/jtparchive/trps-02-70-01-001.pdf
Hadjibalassi, M., Lambrinou, E.., Papastavrou,E., & Papathanassoglou, E. (2018). The effect of guided imagery on physiological and psychological outcomes of adult ICU patients: A systematic literature review and methodological implications, Australian Critical Care, 31(2), 73-86. https://doi.org/10.1016/j.aucc.2017.03.001
Higgins, C, Smith, B.H., & Matthews, K. (2019). Evidence of opioid-induced hyperalgesia in clinical populations after chronic opioid exposure: a systematic review and meta-analysis, British Journal of Anaesthesia, 122(6), e114-e126. https://doi.org/10.1016/j.bja.2018.09.019
IsHak, W.W., Wen, R.Y., Naghdechi, L., Vanle, B., Dang, J., Knosp, M., Dascal, J., Lobsang, Gohar, Y.,; Eskander, L., Yadegar, J., Hanna, S., Sadek, A., Aguilar-Hernandez, L., Danovitch, I., Louy, C. (2018). Pain and Depression: A Systematic Review, Harvard Review of Psychiatry, 11/12, 26(6), 352-363. https://doi.org/10.1097/HRP.0000000000000198
Koob, G.F. (2020). Neurobiology of Opioid Addiction: Opponent Process, Hyperkatifeia, and Negative Reinforcement, Biological Psychiatry, 87(1), 44-53. https://doi.org/10.1016/j.biopsych.2019.05.023
Mullins, P.M., & Bhattacharyya, N. (2022). Prevalence of chronic pain among adults in the United States, Pain, 163(2), e328-e332. https://doi.org/10.1097/j.pain.0000000000002291NIH–
NIDA (2022). Opioid Overdose Crisis. Downloaded June 30, 2022. https://nida.nih.gov/research-topics/opioids/opioid-overdose-crisis
Parisien, M., Lima, L.V., Dagostino, C., El-Hachem, N., Drury, G.L., Grant, A.V., Huising, J., Verma, V…. .(2022). Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Science Translational Medicine, 14(644). https://doi.org/10.1126/scitranslmed.abj99
Peper, E. (2018). Breathing reduces acid reflux and dysmenorrhea discomfort. the peperperspective. https://peperperspective.com/2018/10/04/breathing-reduces-acid-reflux-and-dysmenorrhea-discomfort/
Peper, E. (2022). Resolving a chronic headache with posture feedback and breathing. the peperperspective. https://peperperspective.com/2022/01/04/resolving-a-chronic-headache-with-posture-feedback-and-breathing/
Peper, E., Almedras, M., Heinz, N. & Harvey, R. (in prep). How attending a Holistic Health class reduced symptoms.
Peper, E. Cosby, J. & Amendras, M. Healing chronic back pain. NeuroRegulation, 9I(3), 165-172. https://doi.org/10.15540/nr.9.3.164
Peper, E., Covell, A., & Matzembacker, N. (2021). How a chronic headache condition became resolved with one session of breathing and posture coaching. NeuroRegulation, 8(4), 194–197. https://doi.org/10.15540/nr.8.4.194
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt.ISBN: 978-0787293314 https://he.kendallhunt.com/make-health-happen
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91 https://www.neuroregulation.org/article/view/22815/14575
Peper, E., Lin, I-M., Harvey, r., Gilbert, M. Gubbala, P, Ratkovich, A., & Fletcher, L. (2014). Transforming Chained Behaviors: Case Studies of Overcoming Smoking, Eczema, and Hair Pulling (Trichotillomania), Biofeedback, 42 (4), 154–160. https://doi.org/10.5298/1081-5937-42.4.06
Peper, E., Mason, L, & Huey, C. (2017a). Healing irritable bowel syndrome with diaphragmatic breathing. the peperperspective. https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/
Peper, E., Mason, L., Huey, C. (2017b). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. (45-4). https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Miceli, B., & Harvey, R. (2016). Educational Model for Self-healing: Eliminating a Chronic Migraine with Electromyography, Autogenic Training, Posture, and Mindfulness. Biofeedback, 44(3), 130–137. https://doi.org/10.5298/1081-5937-44.3.03
Peper, E., Sato-Perry, K & Gibney, K. H. (2003). Achieving Health: A 14-Session Structured Stress Management Program—Eczema as a Case Illustration. 34rd Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract in: Applied Psychophysiology and Biofeedback, 28(4), 308. https://biofeedbackhealth.files.wordpress.com/2013/12/2003-aapb-poster-peper-keiko-long1.pdf
Peper, E., Lin, I-M, Harvey, R., Gilbert, M., Gubbala, P., Ratkovich, A., & Fletcher, F. (2014). Transforming chained behaviors: Case studies of overcoming smoking, eczema and hair pulling (trichotillomania). Biofeedback, 42(4), 154-160. https://doi.org/10.5298/1081-5937-42.4.06
Rossman, M. L.(2000). Guided imagery for self-healing. New York: New World Library. https://www.amazon.com/Guided-Imagery-Self-Healing-Martin-Rossman/dp/091581188X/ref=sr_1_3?crid=3M8I1Y1NV3A5N&keywords=martin+rossman&qid=1657649675&s=books&sprefix=rossman%2C+M%2Cstripbooks%2C131&sr=1-3
Rossman, M. L. (2019). Imagine health! Imagery in medical self-care. InSheikh, A.A. (ed). Imagination and healing (pp. 231-258). Routledge. https://www.amazon.com/Imagination-Healing-Imagery-Human-Development-ebook/dp/B07QB4RGSW/ref=sr_1_9?crid=3C7V3E5ZN92R&keywords=Imagination+and+healing&qid=1657818303&s=books&sprefix=imagination+and+healing+%2Cstripbooks%2C105&sr=1-9
Sheng, J., Liu, S., Wang, Y., Cui, R., & Zhang, X. (2017). The link between depression and chronic pain: Neural mechanisms in the brain. Neural Plasticity, 2017, Article 9724371. https://doi.org/10.1155/2017/9724371
Shepherd, Janine. (2012). A broken body isn’t a broken person. TEDxKC. https://www.ted.com/talks/janine_shepherd_a_broken_body_isn_t_a_broken_person
Tan, G., & Jensen, M. P. (2007). Integrating complementary and alternative medicine into multidisciplinary chronic pain treatment. In Chronic Pain Management (pp. 75-99). CRC Press. https://www.taylorfrancis.com/chapters/edit/10.3109/9781420045130-6/integrating-complementary-alternative-medicine-multidisciplinary-chronic-pain-treatment-gabriel-tan-mark-jensen
Treede, R-D., Rief, W., Barke, A., Aziz, Q., Bennett, M.I., Benoliel, R., Cohen, M., Evers, S., Finnerup, N.B., First, M.B., Giamberardino, M.A., Kaasa, S., Korwisi, B., Kosek, E., Lavand’homme, P., ; Nicholas, M., Perrot, S., Scholz, J., Schug, S., Smith, B.H., ; Svensson, P., Vlaeyen, J.S., & Wang, S-J. (2019). Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11), Pain, 160(1), 19-27. https://do.org/10.1097/j.pain.0000000000001384
Von Korff, M. & Simon, G. (1996). The relationship between pain and depression. British Journal of Psychiatry, 168(S30), 101-108. https://doi.org/10.1192/S0007125000298474
Wahl, T. (2011). Minding your mitochondria. TEDzIowaCity. https://www.youtube.com/watch?v=KLjgBLwH3Wc
Warraich, H. (2022). Medicine has failed chronic pain patients. Here’s what they need. Pscyhe, Aeon, https://psyche.co/ideas/medicine-has-failed-chronic-pain-patients-heres-what-they-need
Yong, R. J., Mullins, P. M., & Bhattacharyya, N. (2022). Prevalence of chronic pain among adults in the United States. Pain, 163(2), e328-e332. https://doi.org/10.1097/j.pain.0000000000002291