Do self-healing first
Posted: May 27, 2019 Filed under: behavior, Breathing/respiration, emotions, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, Nutrition/diet, Pain/discomfort, placebo, relaxation, self-healing, stress management, surgery, Uncategorized 2 Comments
“I am doing very well, and I am very healthy. The vulvodynia symptoms have never come back. Also,my stomach (gastrointestinal discomfort) has gotten much, much better. I don’t really have random pain anymore, now I just have to be watchful and careful of my diet and my exercise, which are all great things!” —A five-year follow-up report from a 28-year-old woman who had previously suffered from severe vulvodynia (pelvic floor pain).
Numerous clients and students have reported that implementing self-healing strategies–common sense suggestions often known as “grandmother’s therapy”—significantly improves their health and find that their symptoms decreased or disappeared (Peper et al, 2014). These educational self-healing approaches are based upon a holistic perspective aimed to reduce physical, emotional and lifestyle patterns that interfere with healing and to increase those life patterns that support healing. This may mean learning diaphragmatic breathing, doing work that give you meaning and energy, alternating between excitation and regeneration, and living a life congruent with our evolutionary past.
If you experience discomfort/symptoms and worry about your health/well-being, do the following:
- See your health professional for diagnosis and treatment suggestions.
- Ask what are the benefits and risks of treatment.
- Ask what would happen if you if you first implemented self-healing strategies before beginning the recommended and sometimes invasive treatment?
- Investigate how you could be affecting your self-healing potential such as:
- Lack of sleep
- Too much sugar, processed foods, coffee, alcohol, etc.
- Lack of exercise
- Limited social support
- Ongoing anger, resentment, frustration, and worry
- Lack of hope and purpose
- Implement self-healing strategies and lifestyle changes to support your healing response. In many cases, you may experience positive changes within three weeks. Obviously, if you feel worse, stop and reassess. Keep a log and monitor what you do so that you can record changes.
This self-healing process has often been labeled or dismissed as the “placebo effect;” however, the placebo effect is the body’s natural self-healing response (Peper & Harvey, 2017). It is impressive that many people report feeling better when they take charge and become active participants in their own healing process. A process that empowers and supports hope and healing. When participants change their life patterns, they often feel better. Their health worries and concerns become reminders/cues to initiate positive action such as:
- Practicing self-healing techniques throughout the day (e.g., diaphragmatic breathing, self-healing imagery, meditation, and relaxation)
- Eating organic foods and eliminating processed foods
- Incorporating daily exercise and movement activities
- Accepting what is and resolving resentment, anger and fear
- Taking time to regenerate
- Resolving stress
- Focusing on what you like to do
- Be loving to yourself and others
For suggestions of what to do, explore some of the following blogs that describe self-healing practices that participants implemented to improve or eliminate their symptoms.
Acid reflux (GERD) https://peperperspective.com/2018/10/04/breathing-reduces-acid-reflux-and-dysmenorrhea-discomfort/
Dyspareunia https://peperperspective.com/2017/03/19/enjoy-sex-breathe-away-the-pain/
Epilepsy https://peperperspective.com/2013/03/10/epilepsy-new-old-treatment-without-drugs/
Irritability/hangry https://peperperspective.com/2017/10/06/are-you-out-of-control-and-reacting-in-anger-the-role-of-food-and-exercise/
Hot flashes and premenstrual symptoms https://peperperspective.com/2015/02/18/reduce-hot-flashes-and-premenstrual-symptoms-with-breathing/
Internet addiction https://peperperspective.com/2018/02/10/digital-addiction/
Irritable bowel syndrome (IBS) https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/
Math and test anxiety https://peperperspective.com/2018/07/03/do-better-in-math-dont-slouch-be-tall/
Neck stiffness https://peperperspective.com/2017/04/06/freeing-the-neck-and-shoulders/
Neck tension https://peperperspective.com/2019/05/21/relieve-and-prevent-neck-stiffness-and-pain/
Posture and mood https://peperperspective.com/2017/11/28/posture-and-mood-implications-and-applications-to-health-and-therapy/
Psoriasis https://peperperspective.com/2013/12/28/there-is-hope-interrupt-chained-behavior/
Surgery https://peperperspective.com/2018/03/18/surgery-hope-for-the-best-but-plan-for-the-worst/
Trichotillomania (hair pulling) https://peperperspective.com/2015/03/07/interrupt-chained-behaviors-overcome-smoking-eczema-and-hair-pulling/
Vulvodynia https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
References
Relive memory to create healing imagery
Posted: February 15, 2019 Filed under: behavior, health, placebo, relaxation, self-healing, Uncategorized | Tags: conditioning, Imagery, Pavlov, visualization 4 Comments
This blog describes a structured imagery that evokes past memories of joy and health and integrates them into a relaxation practice to support healing. First, a look at the logic for the practice and then the process of creating your own personal imagery script. A sample audio file is included as a model for creating your MP3 file. The blog is adapted from Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt.
“I enjoyed regressing back into my childhood, remembered playing in the rain, making paper sailboats with my brother…. Placing my fingers in a bowl of water and stroking a paper sailboat enabled me to participate in the total experience… I felt tingling sensations all over my body, like tiny bundles of energy exploding inside of me. By the end of the week the simple word “rain” could induce these sensations inside my whole being.”–Student
Daydreaming! We all know how to do it. When we daydream, we feel, sense, hear, and taste our daydream—the image becomes tangible, as if we are living it. A well-developed relaxation image can also include colors, scents, sounds, flavors, temperature, and so forth. Evoking a past memory image of wholeness may contribute significant to healing, as illustrated in Pavlov’s experience with controlled conditioning and with self-healing.
THE POWER OF CONDITIONING
Pavlov’s experience
Most of us are probably familiar with the classical conditioning experiment of the famous Russian physiologist, Ivan Pavlov, who taught dogs to salivate on cue when they heard a bell ring—even when no food was provided. Pavlov accomplished this by giving the dogs food immediately after ringing a bell. Eventually, the dogs became conditioned to expect the food with the bell and simply hearing the bell ring would induce salivation (shown in Figure 1).

Figure 1. The process of classical conditioning. (Figure adapted from: https://opentextbc.ca/introductiontopsychology/chapter/7-1-learning-by-association-classical-conditioning/)
The conditioning effects of imagery can have an effect on health as well as physiology as reflected in an anecdote told by Theodore Melnechuk about Ivan Pavlov. As an old man, he became quite ill with heart disease and his doctors had no hope of curing him. They took his family aside and told them that the end was near. Pavlov himself, however, was not disheartened. He asked the nurse who was caring for him to bring him a bowl of warm water with a little dirt or mud in it. All day, as he lay in bed, he dabbled one hand in the water, with a dreamy, faraway look on his face. His family was quite sure that he had taken leave of his wits and would die soon. However, the next morning he announced that he felt fine, ate a large breakfast, and sat out in the sun awhile. By the end of the day, when the doctor came to check on him, there was no trace of the heart condition. When asked to explain what he had done, he said that he had reasoned that if he could recall a time when he was completely carefree and happy, it might have some healing benefit for him. As a young boy, he used to spend his summers playing with his friends in a shallow swimming hole in a nearby river. The memory of the warm, slightly muddy water was delightful to him. With his knowledge of the power of conditioned stimuli, he reasoned that having a physical reminder of that water might help him evoke that experience and those blissful feelings, and bring some of those memories into the present time. Using this strategy, he harnessed positive memory and the associated emotions that evoked the associated body changes to bring about his healing.
Conditioned Behaviors
We all performs many conditioned behaviors every day. Some of these behaviors can have implications for our health and wellness. There may be aspects of allergic reactions that are conditioned. For example, the literature reports that a woman who was allergic to roses developed a severe allergic reaction to a very realistic-looking paper rose, even though she was not allergic to paper. Her body reacted as if the paper rose was real. (McKenzie, 1886; Vits et al, 2011).
Conditioning can also affect our immune system. When rats were injected with a powerful immune-suppressing drug, while being fed saccharin-flavored water, their immune function showed an immediate drop. After the drug and saccharine water were paired a number of times, the rats were then given just the saccharin water and a harmless injection of salt water. Their immune cells responded exactly as if they had received the drug! The reverse ability, increasing immune cell function, has been shown to be influenced through conditioning (Ader, Cohen & Felten, 1995; Ader and Cohen, 1993).
Belief can also play a role in these scenarios. Bernie Siegel, MD,(2011) has recounted the story of a woman scheduled for chemotherapy who was first given a saline solution, and cautioned that it could cause hair loss. Although this is an unlikely result of a saline injection, given her belief, her hair fell out.
Actions, thoughts, and images affect our physiology.
We often anticipate, react, and form conclusions with incomplete information. Thoughts and images affect our physiology and even our immune system. Re-evoking a positive memory and living in that memory could potentially improve your health. In a remarkable study by a Harvard psychologist, Ellen Langer, eight men in their 70s lived together for one week, recreating aspects of the world that they had experienced more than 20 years earlier. They were instructed to act as they had in 1959, while the control group was instructed to focus entirely on the present time.
In the experimental group, all the physical cues were reminiscent of the culture twenty years earlier. Black and white television and magazines were from 1959. There were no mirrors to remind them of their current age—only photos on the wall of their younger selves. After a week in which the participants acted as if they were younger and the cues around them evoked their younger selves, 63% of the experimental group had improved their cognitive performance as compared with 44% of the control group. Among participants in the experimental group, even their physical health had improved. Independent raters who looked at the before and after pictures of these participants rated their appearance a little younger than the photos taken before the experiment (Langer, 2009; Grierson, 2014; Friedman, 2015). It is possible that by acting and thinking younger, we actually stay younger!
The limits of our belief are the limits of our experience. This concept underlies the remarkable power of placebo. If one believes a drug or a procedure is helpful, that can have a powerful healing effect (Peper & Harvey, 2017; also see the blog, How effective is treatment? The importance of active placebos).
CREATE YOUR OWN VISUALIZATION
Begin by remembering a time when you felt happy, healthy, and whole. Draw inspiration from Pavlov, who evoked happy memories from his childhood, apparently dramatically changing his health. To develop your personal visualization, set aside the time to recreate a healing memory. Remember a time in your life when you felt healthy and joyous (possibly from your childhood). For some, this might be time in nature or with your family or with friends.
Once you remember the event, re-experience it as if you were there right now. Evoke as many senses as possible. Think of the memory and any associations such as an old teddy bear, a shell from the beach, a favorite song, a certain perfume or some other tangible aspect of the experience. The goal is to recreate the experience as if it was current reality. Olfactory and gustatory cues can be especially powerful. If possible include the actual objects and cues associated with that memory—articles, pictures, music, songs, fragrances, or even food.
Sounds, scents, or touching and objects from that era of your life can deepen your ability to recreate and experience the quality of that memory—to actually be in the memory. These sensory reminders will help to evoke the memory and increase the felt experience. You might find it helpful to review Ellen Langer’s experiment, recreating an environment from twenty years earlier. The actual cues will deepen the experience, just as aromas often evoke specific memories and emotions.
The underlying principle is that memories are associated with conditioned stimuli that evoke the physiological state(s) in the body present when the memory was created.
Once you have created a vivid memory that engenders a sense of wholeness, develop a detailed description of your memory to help you evoke that experience. (For some, the memory calls up a timeless setting—relaxing on a warm beach, sitting in front of the fire on a winter evening, or sailing on a calm day. For others, the sense of trust may be associated with a specific person—someone you love—being with your grandmother, helping your mother bake a cake, or going fishing with your dad.). As you recreate the experience, engage all your senses (images, fragrance, tastes, textures, sounds, kinetics). Stay in your image: see it, smell it, taste it, touch it, hear it, be it and allow the experience to deepen.
Begin by writing up your imagery. Then record the introduction the structured relaxation and follow it with a description that evokes the memory as an MP3 audiofile. Use the following three-step process to create the script for your personal relaxation.
- Describe a time in your past when you felt joy, peace, love, or a sense of integration and wholeness.
_________________________________________________________________
_________________________________________________________________
- Identify the specific cues or stimuli associated with that memory.
_________________________________________________________________
_________________________________________________________________
- Write out a detailed description that will evoke your personal memory.
_________________________________________________________________
_________________________________________________________________
_________________________________________________________________
_________________________________________________________________
CREATING YOUR AUDIO FILE
In this approach, there are three components to your script: first, a relaxation practice to ease you into your visualization, then the visualization of your memory, closing with a brief script that brings you back into the present moment.
Begin the recording with progressive relaxation—use your favorite process for relaxing, or apply the script included here.
Generally tense the muscles for about 5 to 8 seconds and let go for 15 to 20 seconds as indicated by the …. inthe script. While tightening and relaxing the muscles, sense the muscle sensations with passive attention. Tense only the muscles that you are instructed to tighten and continue to breathe while tensing and relaxing the muscles. If your attention wanders, gently bring it back to feeling the sensations in the specific muscles that you are instructed to tighten or relax.
First, find a comfortable position for relaxation… To fully relax your face, squeeze your eyes shut tight, press your lips and teeth together, and wrinkle up your nose… feel the tightness in your whole face… Now let it go completely and relax… Allow your face to soften, feel the eyes sinking in their sockets, and your breath to flow effortlessly in and out…
Tense both arms by making fists, and extend them straight ahead, while continuing to breathe deeply… study the tension… Now relax and let your arms drop as if you were a rag doll… To relax your shoulders, hunch them toward your ears and tighten your neck, while keeping the rest of your body loose and relaxed… Continue to breathe easily… Allow your shoulders to drop… Feel the weight of your arms… Feel the relaxation flowing from your shoulders, down your arms into your hands and out your fingers…
Now your stomach. Then let go and relax… Arch your back and feel the tightness in the back. Let go and relax….Allow your body to sink comfortably into the surface on which you are resting… Finally, tighten your butt, thighs, calves, and feet by pressing your heels down into the surface where you are lying, curling your toes and squeezing your knees together… Feel the tension as you continue to breathe, keeping your upper body relaxed… Now let go and relax… Allow relaxation to flow through your legs… Be aware of the sensations of letting go…
Feel the deepening relaxation, the calmness and the serenity… Feel each exhalation flowing down and through your arms, chest, and legs… Let the feelings of relaxation and heaviness deepen as you relax more… Notice the developing sense of inner peace… a calm indifference to external events… Let the feelings of relaxation, calmness, and serenity deepen for a few minutes. After a few minutes, evoke your memory of wholeness.
Insert your imagery script here.
Finish with the brief closing script
Allow yourself to just stay in this special place all your own… and know that you can return to this peaceful sanctuary any time you choose to do so. When you are ready to release the imagery, take a deep breath, gently stretch your body, and open your eyes.
Record these this whole script on your cell phone as an MP3 file.
When you record, it often takes a few tries before the pacing is correct. You may find it helpful to listen to the following audio file as a model for to create your own.
LISTENING TO YOUR VISUALIZATION
Create a sanctuary for yourself by turning off your cellphone, adjusting the heat to a comfortable temperature, and ensuring that you will have uninterrupted quiet time for 20 to 30 minutes. Loosen any constricting clothing or jewelry, your glasses, and so on. Settle into a comfortable chair, bed, or setting where you can easily relax. Enjoy letting yourself drift into and relive the memory experience.
Many participants report that this practice is an exceptionally relaxing and nurturing experience, one that supports regeneration. You’ll probably find that the more you practice, the more the relaxation deepens. You may find it helpful to keep notes and observe how you feel after each practice. Although it may feel strange to listen to your own voice, most people find that after a while it becomes more comfortable. After listening to it for a few times, you may want to rerecord the script. Finally, generalize this practice by smiling and evoking the memory scene as much as you desire during the day.
Additional strategies to enhance the relaxation
- Have a massage or take a warm shower or soak and then do the practice. Compare your level of relaxation afterwards to the result of using the audio alone.
- Practice gentle stretches to loosen tight muscles or “shake out” your arms and legs just before doing your relaxation practice.
- Draw or paint the relaxing image or actually go to the location where your memory occurred (if possible) and do your practice. Or practice outdoors in the most relaxing place you can find. Nature can be a great healer.
- Create an atmosphere that helps to evoke and augment your relaxation image (e.g., play background music or use fragrances that you associated with the image).
Common challenges
- Inability to evoke a memory of wholeness. When this occurs, it is as if one draws a blank. This is common, especially if one has experienced abuse or feels depressed. In that case, use the image presented in the script or make one up and create a totally imaginary peaceful image.
- Positive memories of wholeness evoke a bitter/sweet feeling. This occurs when images of wholeness include a loved one who has passed on or who is no longer in your life. On the one hand, this may call up strongly positive feelings, but it may evoke a sense of loss and sadness. If this occurs, simply chose a different memory or create a different script. Let the memory of loss go. Accept your experience and your feelings as much as possible, and know that at least you have been loved. For your image, it may be easier to focus on a natural setting you love—one you associate with peace and tranquility.
- Lack of experience with places in nature. Some people have only urban experiences and find nature alien. See what comes up for you. Does your favorite memory as a city kid recall a day of freedom on your bike or skateboarding, or an afternoon with your playmates? Perhaps you have treasured memories as a teen or an adult of long walks in the city or time spent with close friends. You also have the option of creating new images such as sitting by a fireplace, in a walled garden, or some other scene of peace and safety.
- Difficulty using progressive relaxation. If you’re having trouble isolating a muscle: touch it, stroke it with your hands, and then tense it fully (without strain) and feel the tension in your hands; feel the difference with your hands as you let go of the tension. Or, you may tighten only as much as is needed to feel the tension.
- The desire to stay in the imagery and not wanting to return to reality. If the imagery is much more pleasant than the present, use this process as a stimulus to reorganize your life and set new goals and priorities.
References
Ader, R. & Cohen, N. (1993). Psychoneuroimmunology, Conditioning,_and_Stress. Annual Review of Psychology, 44(1), 53-85.
Ader, R., Cohen, N. and Felten, D. (1995) Psychoneuroimmunology: Interactions between the Nervous System and the Immune System. The Lancet, 345, 99-103.
https://doi.org/10.1016/S0140-6736(95)90066-7
Friedman, L. F. (2015). A radical experiment tried to make old people young again–and the results were astonishing . https://www.businessinsider.com/ellen-langers-reversing-aging-experiment-2015-4
Grierson, B. (2014). What if age is nothing more than a mind-set? New York Times Magazine. October 22.
Langer, E. (2009). Counterclockwise: Mindful Health and the Power of Possibility . New York: Ballantine Books.
McKenzie, J. (1886). The production of the so-called rose effect by means of an artificial rose, with remarks and historical notes. Am. J. Med. Sci. 91, 45–57
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness . Dubuque, IA: Kendall-Hunt. ISBN-13: 978-0787293314
Peper, E. & Harvey, R. (2017). The fallacy of placebo controlled clinical trials: Are positive outcomes the result of indirect treatment side effects? NeuroRegulation. 4(3–4), 102–113. doi:10.15540/nr.4.3-4.102
Siegel, B. (2011, May). Remarkable recoveries. Retrieved from: http://berniesiegelmd.com/resources/articles/remarkable-recoveries/
Vits, S., Cesko, E., Enck, P., Hillen, U., Schadendorf, D., & Schedlowski, M. (2011). Behavioural conditioning as the mediator of placebo responses in the immune system. Philosophical Transactions: Biological Sciences, 366(1572), 1799–1807. http://www.jstor.org/stable/23035535
Today is a new day-a new beginning
Posted: December 31, 2018 Filed under: behavior, health, Pain/discomfort, self-healing, Uncategorized | Tags: dance, hope, joy, pain, regenration, spinal injury 3 CommentsIn a world of turmoil, it is often challenging to think that tomorrow can be different and better. Yet, each day is an opportunity to accept whatever happened in the past and look forward to the unfolding present. So often, we anticipate that the future will be the same or worse especially if we feel depressed, suffer from ongoing pain, chronic illness, family or work stress, etc. At those moments, we forget that yesterday’s memories may contribute to how we experience and interpret the future. Most of us do not know what the future will bring, thus be open to new opportunities for growth and well-being. For the New Year, adapt a daily ritual that I learned from a remarkable healer Dora Kunz.
Each morning when you get out of bed, take a few slow deep breaths. Then think of someone who you feel loved by and makes you smile whether your grandmother, aunt or dog. Then when you get up and put your feet on the ground, say out loud, “Today is a new day- a new beginning.”
Watch the following two videos of people for whom the future appeared hopeless and yet had the courage to transcend their limitations and offer inspiration and joy.
Janine Shepherd: A broken body isn’t a broken person. Cross-country skier Janine Shepherd hoped for an Olympic medal — until she was hit by a truck during a training bike ride. She shares a powerful story about the human potential for recovery. Her message: you are not your body, and giving up old dreams can allow new ones to soar.
Ma Li and Zhai Xiaowei: Hand in Hand. This is a video of a broadcast that originally aired on China’s English-language CCTV channel 9 during a modern dance competition in Beijing, China in 2007. This very unique couple–she without an arm, he without a leg–was one of the finalists among 7000 competitors in the 4th CCTV national dance competition. It is the first time a handicapped couple had ever entered the competition. They won the silver medal and became an instant national hit. The young woman, in her 30’s, was a dancer who had trained since she was a little girl. Later in life, she lost her entire right arm in an automobile accident and fell into a state of depression for a few years. After rebounding, she decided to team with a young man who had lost his leg in a farming accident as a boy and who was completely untrained in dance. After a long and sometimes agonizing training regimen, this is the result. The dance is performed by Ma Li (馬麗) and Zhai Xiaowei (翟孝偉). The music “Holding Hands” is composed by San Bao and choreographed by Zhao Limin.
Cell phone radio frequency radiation increases cancer risk*
Posted: November 12, 2018 Filed under: cancer, digital devices, self-healing, Uncategorized | Tags: cellphones, digital devices, Radio frequency radiation, technology 3 CommentsBe safe rather than sorry. Cellphone radio frequency radiation is harmful!
The National Toxicology Program (NTP) released on October 31, 2018 their final report on rat and mouse studies of radio frequency radiation like that used with cellphones. The $30 million NTP studies took more than 10 years to complete and are the most comprehensive assessments to date of health effects in animals exposed to Radio Frequency Radiation (RFR) with modulations used in 2G and 3G cell phones. 2G and 3G networks were standard when the studies were designed and are still used for phone calls and texting.
The report concluded there is clear evidence that male rats exposed to high levels of radio frequency radiation (RFR) like that used in 2G and 3G cell phones developed cancerous heart tumors, according to final reports. There was also some evidence of tumors in the brain and adrenal gland of exposed male rats. For female rats, and male and female mice, the evidence was equivocal as to whether cancers observed were associated with exposure to RFR.
“The exposures used in the studies cannot be compared directly to the exposure that humans experience when using a cell phone,” said John Bucher, Ph.D., NTP senior scientist. “In our studies, rats and mice received radio frequency radiation across their whole bodies. By contrast, people are mostly exposed in specific local tissues close to where they hold the phone. In addition, the exposure levels and durations in our studies were greater than what people experience.”
In the NTP study, the lowest exposure level used in the studies was equal to the maximum local tissue exposure currently allowed for cell phone users. This power level rarely occurs with typical cell phone use. The highest exposure level in the studies was four times higher than the maximum power level permitted. Butcher state, “We believe that the link between radio frequency radiation and tumors in male rats is real, and the external experts agreed.”
I interpret that their results support the previous–often contested–observations that brain cancers were more prevalent in high cell phone users especially on the side of the head they held the cellphone.
More some women who have habitually stashed their cell phone in their bra have been diagnosed with a rare breast cancer located beneath the area of the breast where they stored their cell phone. Watch the heart breaking TV interview with Tiffany. She was 21 years old when she developed breast cancer which was located right beneath the breast were she had kept her cell phone against her bare skin for the last 6 years.
While these rare cases could have occurred by chance, they could also be an early indicator of risk. Previously, most research studies were based upon older adults who have tended to use their mobile phone much less than most young people today. The average age a person acquires a mobile phone is ten years old (this data was from 2016 and many children now have cellphones even earlier). Often infants and toddlers are entertained by smartphones and tablets–the new technological babysitter. The possible risk may be much greater for a young people since their bodies and brains are still growing rapidly. I wonder if the antenna radiation may be one of the many initiators or promoters of later onset cancers. We will not know the answer; since, most cancer take twenty or more years to develop.
What can you do to reduce risk?
Act now and reduce the exposure to the antenna radiation by implementing the following suggestions:
- Keep your phone, tablet or laptop in your purse, backpack or briefcase. Do not keep it on or close to your body.
- Use the speakerphone or earphones with microphone while talking. Do not hold it against the side of your head, close to your breast or on your lap.
- Text while the phone is on a book or on a table away from your body.
- Put the tablet and laptop on a table and away from the genitals.
- Set the phone to airplane mode.
- Be old fashioned and use a cable to connect to your home router instead of relying on the WiFi connection.
- Keep your calls short and enjoy the people in person.
- Support legislation to label wireless devices with a legible statement of possible risk and the specific absorption rate (SAR) value. Generally, higher the SAR value, the higher the exposure to antenna radiation.
- Support the work by the Environmental Health Trust.
For an radio interview on this topic, listen to my interview on Deborah Quilter’s radio show. http://www.blogtalkradio.com/rsihelp/2018/11/20/why-you-should-keep-your-cell-phone-away-from-your-body-with-dr-erik-peper
For more information on NTP study see:
*The blog is adapted in part from the November 1, 2018 news release from the National Toxicology Program (NTP)1, National Institute of Environmental Health Sciences2, National Institute of Health (NIH)3.
- About the National Toxicology Program (NTP):NTP is a federal, interagency program headquartered at NIEHS, whose goal is to safeguard the public by identifying substances in the environment that may affect human health. For more information about NTP and its programs, visit niehs.nih.gov.
- About the National Institute of Environmental Health Sciences (NIEHS): NIEHS supports research to understand the effects of the environment on human health and is part of NIH. For more information on environmental health topics, visit niehs.nih.gov. Subscribe to one or more of the NIEHS news lists (www.niehs.nih.gov/news/newsroom/newslist/index.cfm) to stay current on NIEHS news, press releases, grant opportunities, training, events, and publications.
- About the National Institutes of Health (NIH):NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit nih.gov.
Breathing reduces acid reflux and dysmenorrhea discomfort
Posted: October 4, 2018 Filed under: Breathing/respiration, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: acid reflux, dysmenorrhea, gastroesophageal reflux disease, GERD, menstrual cramps, PMS 14 CommentsPublished as: Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
“Although difficult and going against my natural reaction to curl up in the response to my cramps, I stretched out on my back and breathed slowly so that my stomach got bigger with each inhalation. My menstrual pain slowly decreased and disappeared.
“For as long as I remember, I had stomach problems and when I went to doctors, they said, I had acid reflux. I was prescribed medication and nothing worked. The problem of acid reflux got really bad when I went to college and often interfered with my social activities. After learning diaphragmatic breathing so that my stomach expanded instead of my chest, I am free of my symptoms and can even eat the foods that previously triggered the acid reflux.”
In the late 19th earlier part of the 20th century many women were diagnosed with Neurasthenia. The symptoms included fatigue, anxiety, headache, fainting, light headedness, heart palpitation, high blood pressure, neuralgia and depression. It was perceived as a weakness of the nerves. Even though the diagnosis is no longer used, similar symptoms still occur and are aggravated when the abdomen is constricted with a corset or by stylish clothing (see Fig 1).

Figure 1. Wearing a corset squeezes the abdomen.
The constricted waist compromises the functions of digestion and breathing. When the person inhales, the abdomen cannot expand as the diaphragm is flattening and pushing down. Thus, the person is forced to breathe more shallowly by lifting their ribs which increases neck and shoulder tension and the risk of anxiety, heart palpitation, and fatigue. It also can contribute to abdominal discomfort since abdomen is being squeezed by the corset and forcing the abdominal organs upward. It was the reason why the room on top of stairs in the old Victorian houses was call the fainting room (Melissa, 2015).
During inhalation the diaphragm flattens and attempts to descend which increases the pressure of the abdominal content. In some cases this causes the stomach content to be pushed upward into the esophagus which could result in heart burn and acid reflux. To avoid this, health care providers often advice patients with acid reflux to sleep on a slanted bed with the head higher than their feet so that the stomach content flows downward. However, they may not teach the person to wear looser clothing that does not constrict the waist and prevent designer jean syndrome. If the clothing around the waist is loosened, then the abdomen may expand in all directions in response to the downward movement of the diaphragm during inhalation and not squeeze the stomach and thereby pushing its content upward into the esophagus.
Most people have experienced the benefits of loosening the waist when eating a large meal. The moment the stomach is given the room to spread out, you feel more comfortable. If you experienced this, ask yourself, “Could there be a long term cost of keeping my waist constricted?” A constricted waist may be as harmful to our health as having the emergency brake on while driving for a car.
We are usually unaware that shallow rapid breathing in our chest can contribute to symptoms such as anxiety, neck and shoulder tension, heart palpitations, headaches, abdominal discomfort such as heart burn, acid reflux, irritable bowel syndrome, dysmenorrhea and even reduced fertility (Peper, Mason, & Huey, 2017; Domar, Seibel, & Benson, 1990).
Assess whether you are at risk for faulty breathing
Stand up and observe what happens when you take in a big breath and then exhale. Did you feel taller when you inhaled and shorter/smaller when you exhaled?
If the answer is YES, your breathing pattern may compromise your health. Most likely when you inhaled you lifted your chest, slightly arched your back, tightened and raised your shoulders, and lifted your head up while slightly pulling the stomach in. When you exhaled, your body relaxed and collapsed downward and even the stomach may have relaxed and expanded. This is a dysfunctional breathing pattern and the opposite of a breathing pattern that supports health and regeneration as shown in figure 2.
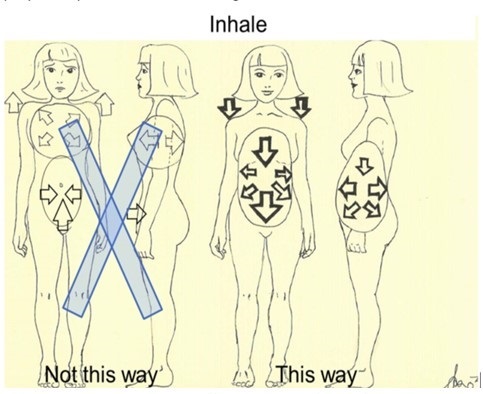
Figure 2. Incorrect and correct breathing. Source unknown.
Observe babies, young children, dogs, and cats when they are peaceful. The abdomen is what moves during breathing. While breathing in, the abdomen expands in all 360 degrees directions and when breathing out, the abdomen constricts and comes in. Similarly when dogs or cats are lying on their sides, their stomach goes up during inhalation and goes down during exhalation.
Many people tend to breathe shallowly in their chest and have forgotten—or cannot– allow their abdomen and lower ribs to widen during inhalation (Peper et al, 2016). These factors include:
- Constriction by the modern corset called “Spanx” to slim the figure or by wearing tight fitting pants. In either case the abdominal content is pushed upward and interferes with normal healthy breathing.
- Maintaining a slim figure by pulling the abdomen (I will look fat when my stomach expands; I will suck it in).
- Avoiding post-surgical abdominal pain by inhibiting abdominal movement. Numerous patients have unknowingly learned to shallowly breathe in their chest to avoid pain at the site of the incision of the abdominal surgery such as for hernia repair or a cesarean operation. This dysfunctional breathing became the new normal unless they actively practice diaphragmatic breathing.
- Slouching as we sit or watch digital screens or look down at our cell phone.
Observe how slouching affects the space in your abdomen.
When you shift from an upright erect position to a slouched or protective position the distance between your pubic bone and the bottom of the sternum (xiphoid process) is significantly reduced.
- Tighten our abdomen to protect ourselves from pain and danger as shown in Figure 3.

Figure 3. Erect versus collapsed posture. There is less space for the abdomen to expand in the protective collapsed position. Reproduced by permission from Clinical Somatics (http://www.clinicalsomatics.ie/).
Regardless why people breathe shallowly in their chest or avoid abdominal and lower rib movement during breathing, by re-establishing normal diaphragmatic breathing many symptoms may be reduced. Numerous students have reported that when they shift to diaphragmatic breathing which means the abdomen and lower ribs expand during inhalation and come in during exhalation as shown in Figure 4, their symptoms such as acid reflux and menstrual cramp significantly decrease.
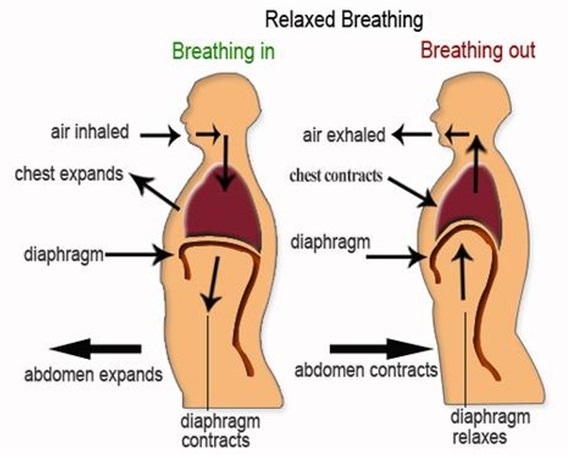
Figure 4. Diaphragmatic breathing. Reproduced from: www.devang.house/blogs/thejob/belly-breathing-follow-your-gut.
Reduce acid reflux
A 21-year old student, who has had acid reflux (GERD-gastroesophageal reflux diseases) since age 6, observed that she only breathed in her chest and that there were no abdominal movements. When she learned and practiced slower diaphragmatic breathing which allowed her abdomen to expand naturally during inhalation and reduce in size during exhalation her symptoms decreased. The image she used was that her lungs were like a balloon located in her abdomen. To create space for the diaphragm going down, she bought larger size pants so that her abdominal could spread out instead of squeezing her stomach (see Figure 5).
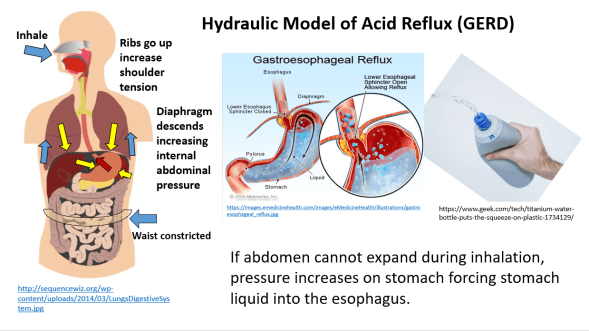
Figure 5. Hydraulic model who inhaling without the abdomen expanding increases pressure on the stomach and possibly cause stomach fluids to be pushed into the esophagus.
She practiced diaphragmatic breathing many times during the day. In addition, the moment she felt stressed and tightened her abdomen, she interrupted this tightening and re-established abdominal breathing. Practicing this was very challenging since she had to accept that she would still be attractive even if her stomach expanded during inhalation. She reported that within two weeks her symptom disappeared and upon a year follow-up she has had no more symptoms. In the video she describes her experiences of integrate breathing and awareness into daily life.
We have also use this similar approach to successfully overcome irritable bowel syndrome see: https://peperperspective.com/2017/06/23/healing-irritable-bowel-syndrome-with-diaphragmatic-breathing/
Take control of menstrual cramps
Numerous college students have reported that when they experience menstrual cramps, their natural impulse is to curl up in a protective cocoon. If instead they interrupted this natural protective pattern and lie relaxed on their back with their legs straight out and breathe diaphragmatically with their abdomen expanding and going upward during inhalation, they report a 50 percent decrease in discomfort (Gibney & Peper, 2003). For some the discomfort totally disappears when they place a warm pad on their lower abdomen and focused on breathing slowly about six breaths per minute so that the abdomen goes up when inhaling and goes down when exhaling. At the same time, they also imagine that the air would flow like a stream from their abdomen through their legs and out their feet while exhaling. They observed that as long as they held their abdomen tight the discomfort including the congestive PMS symptoms remained. Yet, the moment they practice abdominal breathing, the congestion and discomfort is decreased. Most likely the expanding and constricting of the abdomen during the diaphragmatic breathing acts as a pump in the abdomen to increase the lymph and venous blood return and improve circulation.
Conclusion
Breathing is the body-mind bridge and offers hope for numerous disorders. Slower diaphragmatic breathing with the corresponding abdomen movement at about six breaths per minute may reduce autonomic dysregulation. It has profound self-healing effects and may increase calmness and relaxation. At the same time, it may reduce heart palpitations, hypertension, asthma, anxiety, and many other symptoms.
References
DeVault, K.R. & Castell, D.O. (2005). Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The American Journal of Gastroenterology, 100, 190-200.
Domar, A.D., Seibel, M.M., & Benson, H. (1990). The Mind/Body Program for Infertility: a new behavioral treatment approach for women with infertility. Fertility and sterility, 53(2), 246-249.
Gibney, H.K. & Peper, E. (2003). Taking control: Strategies to reduce hot flashes and premenstrual mood swings. Biofeedback, 31(3), 20-24.
Johnson, L.F. & DeMeester, T.R. (1981). Evaluation of elevation of the head of the bed, bethanechol, and antacid foam tablets on gastroesophageal reflux. Digestive Diseases Sciences, 26, 673-680. https://www.ncbi.nlm.nih.gov/pubmed/7261830
Melissa. (2015). Why women fainted so much in the 19th century. May 20, 2015. Donloaded October 2, 1018. http://www.todayifoundout.com/index.php/2015/05/women-fainted-much-19th-century/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. (45-4)
Stanciu, C. & Bennett, J.R.. (1977). Effects of posture on gastro-oesophageal reflux. Digestion, 15, 104-109. https://www.karger.com/Article/Abstract/197991
Experience how thoughts affect body with lemon imagery*
Posted: July 25, 2018 Filed under: behavior, Breathing/respiration, emotions, relaxation, self-healing, Uncategorized | Tags: autonomic nervous system, Holistic health, Imagery, mind-body, salivation, visualization 2 CommentsMost of us are aware that thoughts affect our body; however, we often overlook the impact of this effect. To demonstrate the power of visualization, participants are guided through a lemon imagery. In a study with 131 college students, 94% report an increase in salivation which is a parasympathetic nervous system response. The participants now know–not believe–that visualization affects physiology. Once salivation has been experienced, participants may apply other visualization techniques to change their physiology and behavior. Through visualization we communicate with our autonomic nervous system which can provide a matrix for self-healing and enhanced performance. In addition, the guided practice shows that almost everyone holds their breath when asked to tighten their muscles and some people have difficulty relaxing after tightening. Once aware, the person can and continue to breathe and relax the muscles. Enjoy the guided exercise, Mindbody connection: Lemon Imagery.
*I thank Paul Godina, Jung Lee and Lena Stampfli for participating in the videos.
Adapted from Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt
Be careful what you think*
Posted: July 23, 2018 Filed under: behavior, Exercise/movement, self-healing, stress management, Uncategorized | Tags: CBT, cognitive therapy, Mind body connection, muscle testing, performance, psyching out, somatic practices Leave a comment“I couldn’t belief it. I thought that I was strong and yet, I could not resist the downward pressure when I recalled a hopeless and helpless memory. Yet a minute later, I could easily resist the downward pressure on my arm when I thought of a positive and empower memory. I now understand how thoughts affect me.”
Thoughts/emotions affect body and body affects thoughts and emotions is the basis of the psychophysiological principle formulated by the biofeedback pioneers Elmer and Alice Green. The language we use, the thoughts we contemplate, the worries and ruminations that preoccupy us may impact our health.
Changing thoughts is the basis of cognitive behavior therapy and practitioners often teach clients to become aware of their negative thoughts and transform the internal language from hopeless, helpless, or powerless to empowered and positive. Think and visualize what you want and not what you do not want. For example, state, “I have studied and I will perform as best as I can” or “I choose to be a non-smoker instead of stating, “I hope I do not fail the exam” or “I want to stop smoking.” The more you imagine what you what in graphic detail, the more likely will it occur.
Most people rationally accept that thoughts may affect their body; however, it is abstract and not a felt experience. Also, some people have less awareness of the mind-body connection unless it causes discomfort. Our attention tends to be captured by visual and auditory stimuli that constantly bombard us so that we are d less aware of the subtle somatic changes.
This guided practice explores what happens when you recall helpless, hopeless, powerless or defeated memories as compared to recalling empowering positive memories. It allows a person to experience–instead of believing—how thoughts impact the body. 98% of participants felt significantly weaker after recalling the helpless, hopeless, powerless or defeated memories. Once the participants have experienced the effect, they realize how thoughts effect their body.
The loss of strength is metaphor of what may happen to our immune system and health. Do you want to be stronger or weaker? The challenge in transforming thoughts is that they occur automatically and we often doubt that we can change them. The key is to become aware of the onset of the thought and transform the thought. Thoughts are habit patterns and the more you practice a habit, the more it becomes automatic. Enjoy the experiential exercise, Mind-body/Bodymind-connection: Muscle testing.
*I thank Paul Godina, Jung Lee and Lena Stampfli for participating in the videos.
The practice was adapted from, Gorter, R. & Peper, E. (2011). Fighting Cancer-A Non Toxic Approach to Treatment. Berkeley: North Atlantic.
Cancer: What you can do to prevent and support healing
Posted: April 22, 2018 Filed under: cancer, self-healing, Uncategorized | Tags: cancer, healing, Holistic health, prevention, self-care, stress Leave a commentAre you curious to know if there is anything you can do to help prevent cancer?
Are you searching for ways to support your healing process and your immune system?
If yes, watch the invited lecture presented October 14, 2017, at the Caribbean Active Aging Congress, Oranjestad, Aruba, http://www.caacaruba.com
Surgery: Hope for the best and plan for the worst!
Posted: March 18, 2018 Filed under: Pain/discomfort, placebo, self-healing, stress management, surgery, Uncategorized | Tags: anesthesia, hernia, iatrogenic illness, technology, urinary retention 20 CommentsAdapted from: Peper, E. Surviving and preventing medical errors. (2019). Townsend Letter-The Examiner of Alternative Medicine. 429, 63-69. https://townsendletter.com/surviving-and-preventing-medical-errors-peper/
The purpose of this blog is to share what I have learned from a cascade of medical errors that happen much more commonly than surgeons, hospitals, or health care providers acknowledge and is the third leading cause of death in the US (Makary, M.A. & Daniel, M., 2016). My goal here is to provide a few simple recommendations to reduce these errors.

It is now two years since my own surgery—double hernia repair by laparoscopy. The recovery predicted by my surgeon, “In a week you can go swimming again,” turned out to be totally incorrect.
Six weeks after the surgery, I was still lugging a Foley catheter with a leg collection bag that drained my bladder. I had swelling due to blood clots in the abdominal area around my belly button, severe abdominal cramping, and at times, overwhelming spasms. For six weeks my throat was hoarse following the intubation. Instead of swimming, hiking, walking, working, and making love with my wife, I was totally incapacitated, unable to work, travel, or exercise. I had to lie down every few hours to reduce the pain and the spasms.
Instead of going to Japan for a research project, I had to cancel my trip. Rather than teaching my class at the University, I had another faculty member teach for me. I am a fairly athletic guy—I swim several times a week, bike the Berkeley hills, and hiked. Yet after the surgery, I avoided even walking in order to minimize the pain. I moved about as if I were crippled. Now two years later, I finally feel healthy again.
How come my experiences were not what the surgeon promised?
All those who cared for me during this journey were compassionate individuals, committed to doing their best, including the emergency staff, the nurses, my two primary physicians, my surgeon, and my urologist. However, given the personal, professional, and economic cost to me and my family, I feel it is important to assess where things went wrong. The research literature makes it clear that my experience was by no means unique, so I have summarized some of the most important factors that contributed to these unexpected complications, following “simple arthroscopic surgery.”
- Underestimating the risk. Although the surgeon suggested that the operation would be very low risk with no complications, the published research data does not support his optimistic statement and misrepresented the actual risk. Complications for laparoscopic surgery range from 15% to as high as 38% or higher, depending on the age of the patient and how well they do with general anesthesia (Vigneswaran et al, 2015; Neumayer et al, 2004; Perugini & Callery, 2001). Experienced surgeons who have done more than 250 laparoscopic surgeries have a lower complication rate. However, a 2011 Cochran review points out that there is theoretically a higher risk that intra-abdominal organs will be injured during a laparoscopic procedure (Sauerland, 2011). In addition, bilateral laparoscopic hernia repair has significantly higher risk than single sided laparoscopic hernia repair for post-operative urinary retention (Blair et al, 2016). My experience is not an outlier–it is more common.
- Inappropriate post-operative procedures. In my case I was released directly after waking up from general anesthesia without checking to determine whether I could urinate or not. The medical staff and facility should never have released me, since older males have a 30% or higher probability that urinary retention will occur after general anesthesia. However, it was a Friday afternoon and the staff probably wanted to go home since the facility closes at 5:30 pm. This landed me in the Emergency Room.
- Medical negligence. In my case the surgeon recommended that I have my bladder in the emergency room emptied and then go home. That was not sufficient, and my body still was not working properly, requiring a second visit to the ER and the insertion of a Foley catheter. Following the second ER visit, the surgeon removed the catheter in his office in the late afternoon and did not check to determine whether I could urinate or not. This resulted in a third ER visit.
- Medical error. On my third visit to the emergency room, the nurse made the error of inflating the Foley catheter balloon when it was in the urethra (rather than the bladder) which caused tearing and bleeding of the urethra and possible irritation to the prostate.
- Drawbacks of the ER as the primary resource for post-surgical care. Care is not scheduled for the patient’s needs, but rather based on a triage system. In my case I had to wait sometimes two hours or more until a catheter could be inserted. The wait kept increasing the urine volume which expanded and irritated the bladder further.
- A medical system that does not track treatment outcomes. Without good follow-up and long-term data, no one is accountable or responsible.
- A reimbursement system that rewards lower up-front costs. The system favors quick outpatient surgeries without factoring in the long-term costs and harm of the type I experienced.
Assuming the best and not planning for the worst.
Can I trust the health care provider’s statement that the procedure is low risk and that the recovery will go smoothly?
The typical outcome of a medical procedure or surgery may be significantly worse than generally reported by hospitals or medical staff. In many cases there is no systematic follow-up nor data on outcomes and complications, thus no one knows the actual risks.
In the United States medical error results in at least 98,000 unnecessary deaths each year and 1,000,000 excess injuries (Weingart et al, 2000; Khon et al, 2000). The Institute of Medicine reported in 2012 that one-third of hospitalized patients are harmed during their stay (Ferguson, 2012; Institute of Medicine, 2012).
One should also be intelligently skeptical about positive claims for any specific study—it is important to know whether the study has been replicated with other populations and not just a particular group of patients.
To quote Dr. Marcia Angell (2009), the first woman editor of the highly respected New England Journal of Medicine, “It is simply no longer possible to believe much of the clinical research that is published, or to rely on the judgment of trusted physicians or authoritative medical guidelines. I take no pleasure in this conclusion, which I reached slowly and reluctantly over my two decades as an editor of The New England Journal of Medicine.”
The evidence for many procedures and medications is surprisingly limited
- Research studies frequently select specific subsets of patients. They may exclude many patients who have other co-morbidities.
- Clinical trials may demonstrate statistical significance without providing clinically meaningful results. For example, between 2009 and 2013 all most all cancer drugs that were approved for treatment in Europe showed upon follow-up no clear evidence that they improved survival or quality of life for patients (Davis et al, 2017; Kim & Prasad, 2015).
- Pharmaceuticals are tested only against a passive placebo. In some cases, the patient’s positive response may actually be the placebo effect, due to physical sensations induced by the medication or its side effects, thus inspiring hope that the drug is working (Peper and Harvey, 2017).
- Negative side effects are significantly underreported. The data depend on self-report by both the patient and the health care provider.
Many published studies on the positive clinical outcome of pharmaceuticals are suspect. As Dr. Richard Horton (2015), Editor-in-Chief of The Lancet, wrote in 2015, “A lot of what is published is incorrect … much of the scientific literature, perhaps half, may simply be untrue. Afflicted by studies with small sample sizes, tiny effects, invalid exploratory analyses, and flagrant conflicts of interest, together with an obsession for pursuing fashionable trends of dubious importance, science has taken a turn towards darkness.”
Most studies, including those on surgery, lack long-term follow-up.
The apparent short-term benefits may be not beneficial in the long term or may even be harmful. For example, doctors and patients are convinced that SSRIs (serotonin re-uptake inhibitors—antidepressants such as Paxil and Prozac) are beneficial, with resulting global sales in 2011 of $11.9 billion. However, when all the research data were pooled, metanalysis showed that these drugs are no more effective than placebo for the treatment of mild to moderate depression and increase suicides significantly among young adults (Fournier et all, 2010; Kirsch, 2014).
Consider long-term follow-up in my case: the surgeon will report a successful surgery, despite the fact that it took me almost two years to recover fully. (I did not die during surgery and left in seemingly good shape.). Although I called him numerous times for medical guidance during my complications, the outpatient surgical facility will report no complications since I was not transferred from that facility during the surgery to a hospital for continuing care. My insurance carrier that paid the majority of the medical bills recorded the invoices as separate unrelated events: one surgery/one bill, but three separate bills for the emergency room, an additional visit to my primary care physician to check my abdomen when my surgeon did not return my call, and the ongoing invoices from the urologist. They all reported success because the iatrogenic events were not linked to the initial procedure in the data base.
In my case, following surgery, I had to go to the emergency room on three separate occasions due to post-operative urinary retention, placing me at risk of permanent detrusor muscle damage. For more than 18 months, I was under the care of a urologist.
Over the past two years, my symptoms have included gastrointestinal inflammation, spasms, and abdominal bulging, which are only now disappearing. Even my posture has changed. I am now working to reverse the automatic flexing at the hips and leaning forward which I covertly learned to reduce the abdominal discomfort. This level of discomfort and dysfunction are new to me. Reading the research on laparoscopy, I realized that excessive internal bruising, large hematomas, and internal adhesions are fairly common with this type of surgery. However, soft tissue injuries are difficult to confirm with imaging techniques.
My complications were also a direct result of inappropriate post-surgical recommendations and treatment. The symptoms were further compounded by faulty patient discharge procedures performed by the outpatient surgical facility. Since this was my first general anesthesia, I had no idea that I would be one of the people whose outcome were not what the surgeon had predicted. Thus, hope for the best, but plan for the worst.
SCHEDULING MEDICAL PROCEDURES
The following are recommendations may help reduce post-surgical or medical procedure complications.
- Schedule elective medical procedures or surgery early the morning and in the middle of the week. Do not schedule procedures on Mondays, Fridays, or in the afternoon. Procedures performed in the afternoon have significant increase in complications and errors. Anesthesia complications, for example, are four times higher in the afternoon than in the morning (Wright et al, 2006). Our biological rhythms affect our ability to attend and focus. In the morning most people are able to concentrate better than in the afternoon (Pink, 2018).
- Avoid weekends. Procedures performed on weekends (as compared to those done in the middle of the week) increase the risk of complications or dying. For example, babies born on the weekend have a 9.2% higher infant mortality than those born during the week, while those born on Tuesdays have the lowest death rate (Palmer et al, 2015). It is possible that on Mondays medical staff are recovering from weekend binging, while on Fridays they are tired and looking forward to the weekend? If elective procedures are done on a Friday and complications arise, the emergency room is the only option, as the medical staff may not be available over the weekend. In my case the procedure was done on a Friday, and I left the surgical outpatient facility at 2 pm. When complications occurred, it was after 5:30 pm—phone support from the advice nurse and the surgeon on call were my only option until the following Monday. Thus, I had to go the emergency room late Friday evening and again the next evening because of urinary retention, with a long delay in a busy waiting room. Since, I wasn’t bleeding or having a heart attack, that meant I had to wait, wait and wait, which significantly aggravated my specific problem.
- Schedule medical procedures at least one or two weeks before any holiday. Do not schedule surgery just before or during holidays. Medical staff also take holidays and may not available. In my case, I scheduled the procedure the Friday before Thanksgiving because I thought I would have a week of recovery during my Thanksgiving break from teaching. This meant that medical staff were less available and more involved in their holiday planning.
- Schedule procedures so that you are released early in the day. This can allow you to return to the facility in case complications arise. I was released at 2 pm and the complications did not occur until early evening. The facility was closed, so the only option was the ER. When possible, schedule medical procedures or surgery in a facility that is able to provide post-operative care after 5 pm.
- Do not schedule elective procedures during the month of July in an academic teaching hospital. During this month mortality increases and efficiency of care decreases because of the end of the academic year and subsequent changeover to new personnel (Young et al, 2011). Medical school graduates with limited clinical experience begin their residencies and experienced house staff are replaced with new trainees. This is known as the July effect in the U.S. and Killing season in the United Kingdom. During the month of July in any given year, fatal medication errors, for example, increase by 10% at teaching hospitals, but not at neighboring hospitals which do not experience this turnover in medical personnel (Phillips & Barker, 2010).
- Have procedures performed at a medical facility in which the health care professional has no financial interest—take economics out of the equation. When health care practitioners have financial interest in a facility, they tend to order more tests and procedures than health care providers who have no financial interests (Bishop et al, 2010). In my case the surgeon had a financial interest in the outpatient surgical facility where I received surgery. Had I had the operation across the street in the hospital where the surgeon also operates, I probably would not have been released early, avoiding the problems in follow-up care.
STRATEGIES TO OPTIMIZE OUTCOMES AND HEALTH
Organize your support system. Assume that recovery could be more difficult then promised.
Before your procedure, ask family members, friends, and neighbors to be prepared to help. If you did not need them, thank them for their willingness to help. In my case I did not plan for complications, thus my wife was my entire support system, especially for the first three weeks when I was unable to do anything except rest and cope. I was very fortunate to have numerous family, friends, and colleagues who offered their expertise to help me understand what was going on and who assumed my responsibilities when needed.[1]
- Bring an advocate to your appointments. Have your advocate/friend keep notes and ask questions, especially if the health care provider is a respected authority and you are suffering, exhausted, and/or anxious. Record any detailed instructions you must follow at home as a video or audio file on your cell phone or write them down (be sure to ask the health provider for permission). Under stress one may not be able to fully process instructions from the health care provider.
- Make a list of questions and concerns before seeing your health care provider. Talk to your partner and close friends and ask them if there are questions or concerns that you should raise with your provider.
- Ask for more information when tests or procedures are proposed (Robin, 1984).
- Why do you recommend this particular test/procedure/intervention for me and what are the major benefits?
- What are the risks and how often do they occur, in your experience and in the research literature?
- What will you do if the treatment is not successful?
- Ask your provider if there is anything that you should or should not do to promote healing. As much as possible, ask for advice on specific efforts you can make. General statements without instructions such as, “Relax” or “Don’t worry,” are not helpful unless the practitioner teaches you specific skills to relax or to interrupt worrisome thoughts. Many health professionals do not have the time to teach you these types of skills. In many cases the provider may not be able to recommend documented peer-reviewed self-care strategies. Often they imply—and they can be correct—that the specific medical treatment is the only thing that will make you better. In my case I did not find any alternative procedures that would reverse a hernia, although there may be habitual postural and movement patterns that could possibly prevent the occurrence of a hernia (Bowman, 2016). Being totally dependent upon the medical procedure may leave you feeling powerless, helpless, and prone to worry. In most cases there are things you can do to optimize self- healing.
- Think outside the box. Explore other forms of self-care that could enhance your healing. Initiate self-care action instead of waiting passively. By taking the initiative, you gain a sense of control, which tends to enhance your immune system and healing potential. Do anything that may be helpful, as long as it is not harmful. In my case, future medical options to resolve urinary retention could include additional medications or even surgery. Researching the medical literature, there were a number of studies showing that certain herbs in traditional Chinese medicine and Ayurveda medicine could help to reduce prostate inflammation and possibly promote healing. Thus, I began taking three different herbal substances for which there was documented scientific literature. I also was prescribed herbal tea to sooth the bladder. Additionally, I reduced my sugar and caffeine intake to lower the risk of bladder irritation and infection.
- Collaborate with your health care provider. Let your provider know the other approaches you are using. Report any interventions such as vitamins, herbs, Chinese medicine. Ask if they know of any harm that could occur. In most cases there is no harm. The health care professional may just think it is a waste of time and money. However, if you find it helpful, if it gives you control, if it makes you less anxious, and if it is not harmful, it may be beneficial. What do you have to lose?
- Assume that all the health care professionals are committed to improving your health to the best of their ability. Yet at times professionals are now so specialized that they focus only on their own discipline and not the whole person. In their quest to treat the specific problem, they may lose sight of other important aspects of care. Thus, hope for the best, but plan for the worst.
PREPARING FOR SURGERY
Assume that the clinical staff will predict a more positive outcome than that reported in the medical literature. In most cases, especially in the United States, there is no systematic follow-up data since many post-surgical complications are resolved at another location. In addition, many studies are funded by medical companies which have a vested interest and report only the positive outcomes. The companies tend not to investigate for negative side-affects, especially if the iatrogenic effects occur weeks, months, or years after the procedure. This has also been observed in the pharmaceutical companies sponsoring studies for new medications.
Generally, when independent researchers investigated medical procedures they found the complication rate three-fold higher than the medical staff reported. For example, for endoscopic procedures such colonoscopies, doctors reported only 31 complications from 6,383 outpatient upper endoscopies and 11,632 outpatient colonoscopies. The actual rate was 134 trips to the emergency room and 76 hospitalizations. This discrepancy occurred because the only incidents reported involved patients who went back to their own doctors. It did not capture those patients who sought help at other locations or hospitals (Leffler et al, 2010).
The data are even worse for patients who are hospitalized; in the U.S. 20% of patients who leave the hospital return within a month while in England, 7% of those leaving the hospital return within a month (Krumholz, 2013).
- Ask about possible complications that could arise, the symptoms, and what the physician would do if they occurred. Do not assume the health professional will have the time to explain or know all the possible complications. In my case when the surgeon removed the catheter at 4 pm during my second emergency room visit, I had to ask, “What would happen if I still cannot urinate?” Again, the emergency room was the only answer. However, I know now that he could have taught me simple self-catherization which would have eliminated the long waiting in the emergency room, the excessive stretching of the bladder and the subsequent emergency room medical error on my third visit to the ER. It would also have reduced the medical costs by a thousand-fold.
- Get a second opinion. In my case, the surgeon came highly recommended, is very experienced, and has done many hernia repairs. I trusted his judgement that I needed a bilateral hernia repair although I only felt the bulging in the right inguinal area and did not feel bulging or sensations in the left inguinal area. Despite my feeling of trust, I should have asked for a second independent opinion just to be sure. In many moments of despair when suffering the significant complications, I even started to wonder if the bilateral laparoscopic surgical repair was really necessary or just done to increase the income of the surgeon and the outpatient surgical facility in which he had a financial interest. My surgery resulted in large hematomas, irritation of internal organs, and possible damage to the GI track. This type of complication did not occur for a close friend who had a single-sided hernia repair by the same surgeon in a hospital where the surgeon had no financial interests.
- Request medical personnel who are highly experienced in the intervention. Mortality and complications rates are significantly lower for practitioners who have done the procedure at least 250 times.
- Don’t assume the worst but be prepared for the worst. Ask your health care provider about the various side effects of surgery, including the worst things that could happen, and then develop a pre-emptive plan.
The most common problems associated with surgery and general anesthesia include:
- Urinary retention. Following general anesthesia, neural enervation to the bladder and gastrointestinal tract are often affected. The general risk for postoperative urinary retention (POUR) for all types of surgeries ranges from 7% to 52% (Tammela et al, 1986; Petros et al, 1990; Petros et al, 1991; Gonullu et al, 1993; Tammela, 1995). For patients who have surgery for hernia repair 24.4% will experience postoperative urinary retention (Keita et al, 2005)—one in four. The risk for older males is even higher (Blair et al, 2017). Do not leave the medical unit until you have urinated or have a Foley catheter inserted with a leg bag and appropriate follow-up managed by a urologist. In my case, neither the surgeon nor the outpatient hospital checked to determine whether I could urinate—they just discharged me the moment I was conscious. Discharging a patient who has had general anesthesia without checking to determine whether they can urinate goes against all medical guidelines and standard hospital policies and constitutes malpractice. As this was my first surgery, I had no idea that urinary retention could occur. Thus, I did not recognize the symptoms nor did the advice nurse or the surgeon when called for advice before I checked into the emergency room.
- Expect constipation and plan to eat a high roughage diet that supports bowel movements. In case bowel function is slow in resuming, you may want to have on hand simple over-the-counter supplements such as magnesium capsules, psyllium husks, and aloe vera juice or gel, all available at any health food store. Liquid magnesium citrate (GoLytely® solution available at drug stores), can be useful, but tends to be a little stressful to take. Check these over-the-counter supplements with your provider to avoid supplement-drug interaction.
- Infection. Many patients pickup hospital-induced infections (nosocomial infections). In my case, I after four weeks with a Foley catheter, I got a mild bladder infection and had to control it with antibiotics. While in the hospital, avoid direct physical contact with other patients and staff, wash and rewash your hands. Remember medical staff tend are less attentive and wash their hands 10% less in the afternoons than in morning. Ask the medical staff to thoroughly wash their hands before they examine you. If you do get an infection, contact your medical provider immediately.
ACTION STEPS
- Pace yourself. Assume that recovery could be slower than promised. Although your body may appear to be healed, in many cases your vitality could be significantly reduced for a number of months, and you will probably feel much more fatigued in the evening. The recovery from general anesthesia has been compared to recovery from a head-on car collision.
- Identify your support system in case you cannot take care of yourself initially. Organize family and friends to help you. In my case, for the first two weeks I did not have the energy to do anything for myself—the overwhelming abdominal spasms and the three episodes in the ER had drained my energy. I was very lucky that I had my family and friends to help me. For the first few weeks I was so distracted by the pain and discomfort that I did not drive or take care of myself.
- Have a plan in case you need to go to the Emergency Room in the evening. Know its location and have someone who can take you.
- Assume that you will probably have an extensive wait in the ER unless you are desperately ill. Do not try to “tough it out.” Be totally honest about your level of pain, so you can get the best possible care. In my case, I had horrible abdominal pain and spasms with urinary retention, but still acted as if I were okay. When the admitting nurse asked me how I felt, I rated my discomfort as a 5 on a scale from 0 to 10. In my mind I compared the pain with that I had experienced after a skiing accident, which was much worse. What I had forgotten was that the ER is triage system, so I had to wait and wait and wait, which was phenomenally uncomfortable.
- In the ER, ask which medical specialist can follow up with you if further issues develop. A general hospital usually has specialists on call. In my case, if I had requested care from a specialist, I would have been treated directly by a urologist. I would not have had to follow the advice of the surgeon who said, “When you go to Emergency Room, have them empty the bladder and then go home.” Almost all urologists would have recommended keeping the Foley catheter in for a few days to allow the side effects of the anesthesia and the trauma caused by the bladder expansion to ameliorate and then test whether urination was possible.
- Have a medical advocate with you at all times who can observe that the procedures are done correctly. There is a four-fold increase in errors during the evenings and nights as compared to the morning. The more medical staff is multi-tasking, the more likely they will make errors. Have the medical personnel explain any procedure before they perform it—why and how they will do the procedure and what you will experience. You also need to know if they are experienced in that particular procedure? If the answers do not make sense, stop them and ask for another staff member.
- In the ER, record the instructions on your phone. Have medical staff explain and demonstrate to you and your support person what you will need to do at home. Then repeat the instructions back to them to be certain you have it right.
- Remind yourself that errors can occur. In my case, during the third ER visit for urinary retention, the nurse delayed the anchoring of the catheter and it had slipped down into the urethra. As she began to pump, I could feel my urethra tearing and I alerted her to stop. This was immediately followed by another procedural error on her part, so I had to again alert her to stop, which she finally did. All this occurred at 1 am in the morning. As the patient, I had to take charge at a time when I was totally exhausted. As the nurse retreated, I was left sitting on the gurney waiting for someone to come and follow-up. I waited and waited and when I finally stood up, the catheter dropped out and I began bleeding.
Lesson learned: hope for the best but prepare for the worst. In my situation, after eight weeks and numerous visits to the urologist, he removed the catheter. He did this at 8:30 in the morning. This way I could go home and in case something happened, I could go back to his office for further care. Before leaving the office, I planned for the worst. I asked what would happen if I could not urinate later in the evening and requested that he give me a few catheters, so if problems developed, I could catheterize myself.
The urologist gave me the catheters and explained how to use them, although I did not actually practice on myself. Still, I felt better prepared. During the day, I become more and more optimistic because I had no problems; however, at 2 am I woke up unable to urinate. For the next hour, I felt very anxious about inserting the catheter, since I had never done it myself. Finally, my discomfort overcame my anxiety. To my surprise, it was easy. After waiting a few minutes, I removed the catheter and went to bed feeling much more comfortable. The next morning after breakfast and a cup of coffee, I found that my body was working fine without the catheter.
Had I not planned for the worst, I would have once again gone to the Emergency Room and probably waited for hours, risking a repeat of tremendous discomfort and irritation. This simple planning reduced my medical cost more than a thousand-fold from $1700 for the emergency room to $2 for some single-use catheters.
References
Angell, M. (2009). Drug companies & doctors: A story of corruption. The New York Review of Books, 56(1), 8-12. http://www.nybooks.com/articles/2009/01/15/drug-companies-doctorsa-story-of-corruption/
Bishop, T.F., Federman, A.D., & Ross, J.S. (2010). Laboratory test ordering at physician offices with and without on-site laboratories, Journal of Gen Intern Med, 25(10)m 1057-1063. doi: 10.1007/s11606-010-1409-7
Blair, A.B., Dwarakanath, A., Mehta, A., Liang, H., Hui, X., Wyman, C., Ouanes, J.P.P., & Nguyen, H.T. (2017). Postoperative urinary retention after inguinal hernia repair: a single institution experience. Hernia, 21(6), 895-900.
Bowman, K. (2016). Diastasis Recti: The whole-body solution to abdominal weakness and separation. Propriometrics Press: Carlsborg, WA 98324
Davis, C., Naci, N., Gurpinar, E., Poplavska, E., Pinto, A., Aggarwal, A. (2017). Availability of evidence of benefits on overall survival and quality of life of cancer drugs approved by European Medicines Agency: retrospective cohort study of drug approvals 2009-13. BMJ, 2017; j4530 DOI: 10.1136/bmj.j4530
Ferguson, T. B. (2012). The Institute of Medicine Committee report “best care at lower cost: the path to continuously learning health care”. Circulation: Cardiovascular Quality and Outcomes, 5(6), e93-e94. http://jama.jamanetwork.com/article.aspx?articleid=185157
Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., & Fawcett, J. (2010). Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA, 303(1), 47-53.
Gönüllü, N. N., Gönüllü, M., Utkan, N. Z., Dülger, M., Gökgöz, S., & Karsli, B. (1993). Postoperative retention of urine in general surgical patients. The European journal of surgery= Acta chirurgica, 159(3), 145-147.
Horton, R. (2015). Offline: What is medicine’s 5 sigma? The Lancet, 385(9976), 1380. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2815%2960696-1/fulltext?rss%3Dyes
Institute of Medicine’s Infographic, accompanying their 2012 report, Best Care at Lower Cost, at http://www.iom.edu/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America/Infographic.aspx
Keita, H., Diouf, E., Tubach, F., Brouwer, T., Dahmani, S., Mantz, J., & Desmonts, J. M. (2005). Predictive factors of early postoperative urinary retention in the postanesthesia care unit. Anesthesia & Analgesia, 101(2), 592-596.
Kim, C. & Prasad, V. (2015). Cancer drugs approved on the basis of a surrogate end point and subsequent overall survival-An analysis of 5 Years of US Food and Drug Administration approvals. JAMA Intern Med,175(12):1992-1994. doi:10.1001/jamainternmed.2015.5868
Kirsch, I. (2014). The emperor’s new drugs: medication and placebo in the treatment of depression. In Placebo (pp. 291-303). Springer Berlin Heidelberg.
Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (2000). To err is human: building a safer health system (Vol. 6). National Academies Press. http://www.ncbi.nlm.nih.gov/books/NBK221671/
Krumholz, H. M. (2013). Post-hospital syndrome—an acquired, transient condition of generalized risk. New England Journal of Medicine, 368(2), 100-102. http://www.nejm.org/doi/full/10.1056/NEJMp1212324
Leffler, D.A, Kheraj, R., Garud, S., Neeman, N., Nathanson, L.A., Kelly, C.P., Sawhney, M., Landon, B., Doyle, R., Rosenberg, S., & Aronson, M. (2010). The incidence and cost of unexpected hospital use after scheduled outpatient endoscopy. Arch Intern Medicine, 170(19), 1752-1757. http://archinte.jamanetwork.com/article.aspx?articleid=226125
Makary, M.A. & Daniel, M. (2016). Medical error–the third leading cause of death in the US. British Medical Journal, 353:i2139
Neumayer, L., Giobbie-Hurder, A., Jonasson, O., Fitzgibbons Jr, R., Dunlop, D., Gibbs, J., & Henderson, W. (2004). Open mesh versus laparoscopic mesh repair of inguinal hernia. New England Journal of Medicine, 350(18), 1819-1827. http://academicdepartments.musc.edu/surgery/education/resident_info/journal_club/09-10/April-inguinal.pdf
Palmer, W. L., Bottle, A., & Aylin, P. (2015). Association between day of delivery and obstetric outcomes: observational study. BMJ, 351, h5774. http://www.bmj.com/content/bmj/351/bmj.h5774.full.pdf
Peper, E. & Harvey, R. (2017). The fallacy of the placebo controlled clinical trials: Are positive outcomes the result indirect treatment side effects? NeuroRegulation. 4(3–4):102–113 2017 doi:10.15540/nr.4.3-4.102
Perugini, R. A., & Callery, M. P. (2001). Complications of laparoscopic surgery. http://www.ncbi.nlm.nih.gov/books/NBK6923/?report=reader
Petros, J. G., & Bradley, T. M. (1990). Factors influencing postoperative urinary retention in patients undergoing surgery for benign anorectal disease. The American Journal of Surgery, 159(4), 374-376.
Petros, J. G., Rimm, E. B., Robillard, R. J., & Argy, O. (1991). Factors influencing postoperative urinary retention in patients undergoing elective inguinal herniorrhaphy. The American Journal of Surgery, 161(4), 431-433.
Phillips, D. P., & Barker, G. E. (2010). A July spike in fatal medication errors: a possible effect of new medical residents. Journal of General Internal Medicine, 25(8), 774-779. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2896592/
Pink, D.H. (2018). When: The Scientific Secrets of Perfect Timing. New York: Riverhead Books, ISBN-13: 978-0735210622
Robins, E.D. (1984). Matter of Life & Death: Risks vs. Benefits of Medical Care. New York: W.H. Freeman and Company.
Sauerland, S., Walgenbach, M., Habermalz, B., Seiler, C. M., & Miserez, M. (2011). Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. The Cochrane Library.
Tammela, T. (1994). Postoperative urinary retention–why the patient cannot void. Scandinavian Journal of Urology and Nephrology. Supplementum, 175, 75-77.
Tammela, T., Kontturi, M., & Lukkarinen, O. (1986). Postoperative urinary retention: I. Incidence and predisposing factors. Scandinavian Journal of Urology and Nephrology. 20(3), 197-201.
Vigneswaran, Y., Gitelis, M., Lapin, B., Denham, W., Linn, J., Carbray, J., & Ujiki, M. (2015). Elderly and octogenarian cohort: Comparable outcomes with nonelderly cohort after open or laparoscopic inguinal hernia repairs. Surgery, 158(4), 1137-1144.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. BMJ: British Medical Journal, 320(7237), 774. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117772/
Wright, M.D., Philips-Bute, B., Mark, J.B., Stafford-Smith, M., Grichnik, K.P., Andregg, B.C., & Taekman, J.M. (2006). Time of day effects on the incidence of anesthetic adverse events. Quality and Safety in Health Care. 15(4): 258–263.doi: 10.1136/qshc.2005.017566
Young, J. Q., Ranji, S. R., Wachter, R. M., Lee, C. M., Niehaus, B., & Auerbach, A. D. (2011). “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. Annals of Internal Medicine, 155(5), 309-315. http://www.girardslaw.com/library/July_Effect_Annals_of_Internal_Medicine.pdf
[1] I think my family, friends and colleagues (Karen Peper, Norihiro Muramatsu, Richard Harvey, David Wise, Annette Booiman, Lance Nagel and many others) who generously supported me during this journey.


 Figure 1. Increase in U.S. obesity begins after the publication of the U.S. recommendations to eat a low-fat diet. Reproduced from National Center for Health Statistics (US).
Figure 1. Increase in U.S. obesity begins after the publication of the U.S. recommendations to eat a low-fat diet. Reproduced from National Center for Health Statistics (US).