Use the power of your mind to transform health and aging
Posted: February 18, 2025 Filed under: attention, behavior, cancer, CBT, cognitive behavior therapy, COVID, education, health, meditation, mindfulness, Pain/discomfort, placebo, stress management, Uncategorized | Tags: health, imimune function, longevity, mental-health, mind-body, nutrition, Reframing, wellness Leave a commentMost of the time when I drive or commute by BART, I listen to podcasts (e.g., Freakonomics, Hidden Brain, this podcast will kill you, Science VS, Huberman Lab). although many of the podcasts are highly informative; , rarely do I think that everyone could benefit from it. The recent podcast, Using your mind to control your health and longevity, is an exception. In this podcast, neuroscientist Andrew Huberman interviews Professor Ellen Langer. Although it is three hours and twenty-two minute long, every minute is worth it (just skip the advertisements by Huberman which interrupts the flow). Dr. Langer delves into how our thoughts, perceptions, and mindfulness practices can profoundly influence our physical well-being.
She presents compelling evidence that our mental states are intricately linked to our physical health. She discusses how our perceptions of time and control can significantly impact healing rates, hormonal balance, immune function, and overall longevity. By reframing our understanding of mindfulness—not merely as a meditative practice but as an active, moment-to-moment engagement with our environment—we can harness our mental faculties to foster better health outcomes. The episode also highlights practical applications of Dr. Langer’s research, offering insights into how adopting a mindful approach to daily life can lead to remarkable health benefits. By noticing new things and embracing uncertainty, individuals can break free from mindless routines, reduce stress, and enhance their overall quality of life. This podcast is a must-listen for anyone interested in the profound connection between mind and body. It provides valuable tools and perspectives for those seeking to take an active role in their health and well-being through the power of mindful thinking. It will change your perspective and improve your health. Listen to or watch the interview:
Youtube: https://www.youtube.com/watch?v=QYAgf_lfio4

Useful blogs to reduce stress
From Conflict to Calm: Reframing Stress and Finding Peace with Difficult People
Posted: February 6, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, healing, health, Neck and shoulder discomfort, Pain/discomfort, stress management | Tags: anger, anger management, conflict resolution, Reframing, resentment 8 Comments
Adapted from: Peper, E. (2025, Feb 15). From Conflict to Calm: Reframing Stress and Finding Peace with Difficult People. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/from-conflict-to-calm-reframing-stress-and-finding-peace-with-difficult-people/
After living in our house for a few years, a new neighbor moved in next door. Within months, she accused us of moving things in her yard, blamed us when there was a leak in her house, dumped her leaves from her property onto other neighbors’ properties, and even screamed at her tenants to the extent that the police were called numerous times.
Just looking at her house through the window was enough to make my shoulders tighten and leave me feeling upset. When I drove home and saw her standing in front of her house, I would drive around the block one more time to avoid her while feeling my body contract. Often, when I woke up in the morning, I would already anticipate conflict with my neighbor. I would share stories of my disturbing neighbor and her antics with my friends. They were very supportive and agreed with me that she was crazy.
However, this did not resolve my anger, indignation, or the anxiety that was triggered whenever I saw her or thought of her. I spent far too much time anticipating and thinking about her, which resulted in tension in my own body—my heart rate would increase, and my neck and shoulders would tighten. I decided to change. I knew I could not change her; however, I could change my reactivity and perspective.
Thus, I practiced the “Pause and Recenter” technique described in the blog. At the first moment of awareness that I was thinking about her or her actions, I would change my posture by sitting up straight and looking upward, breathe lower and slower, and then, in my mind’s eye, send a thought of goodwill streaming to her like an ocean wave flowing through and around her in the distance. I choose to do this because I believe that within every person, no matter how crazy or cruel, there is a part that is good, and it is that part I want to support.
I repeated this many times—whenever I looked in the direction of her house or saw her in her yard. I also reframed her aggressive, negative behavior as her way of coping with her own demons. Three months later, I no longer react defensively. When I see her, I can say hello and discuss the weather without triggering my defensive reaction. I feel so much more at peace living where I am.
When stressed, angry, rejected, frustrated, or hurt, we so often blame the other person. The moment we think about that person or event, our anger, indignation, resentment, and frustration are triggered. We keep rehashing what happened. As we do this, we are unaware that we are reliving the past event and are often unaware of the harm we are doing to ourselves until we experience symptoms such as high blood pressure, gastrointestinal distress, insomnia, anxiety, or muscle tightness. As we think of the event or interact again with that person, our body automatically responds with a defense reaction as if we are actually being threatened. This response activates the defense to protect ourselves from harm— the person is not a threat like the saber-toothed tiger ready to attack. Yet we respond as if the person is the tiger.
This defense reaction activates our “fight or flight” responses and increases sympathetic activation so that we can run faster and fight more ferociously to survive; however, it reduces blood flow through the frontal cortex—a process that reduces our ability to think rationally (Willeumier, et al., 2011; van Dinther et al., 2024). When we become so upset and stressed that our mind is captured by the other person, it contributes to an increase in hypertension, myofascial pain, depression, insomnia, cardiovascular disease, and other chronic disorders (Russel et al., 2015; Suls, 2013; Duan et al., 2022).
Our initial response of sharing our frustrations with others is normal. It feels good to blame the other; however, over time, the only person who gets hurt is yourself (Fast & Tiedens, 2010; Lou et al., 2023). The time spent rehashing and justifying our feelings diminishes our time we are in the present moment or focus on upcoming opportunities.
We may not realize that we have a choice. We can keep living and reacting to past hurt or losses, or we can let go and/or forgive and make space for new opportunities. Although the choice is ours, it is often very challenging to implement—even with the best intentions—as we react automatically when reminded of the past hurt (seeing that person, anticipating meeting or actually meeting that person who caused the hurt, or being triggered by other events that evoke memories of the pain).
What can you do
If choose to change your response and reactivity, it does not mean you condone what happened or agree that the other person was right. You are just choosing to live your life and not continue to be captured and react to the previous triggers. Many people report that after implementing some of the practices described below or others stress management techniques frequently their automatic reactivity was significantly reduced. They report that their symptoms are reduced and have the freedom to live in present instead of being captured by the painful past.
Pause and recenter
Our automatic reaction to the trigger elicits a defense reaction that reduces our ability to think rationally. Therefore, the moment you anticipate or begin to react, take three very slow diaphragmatic breaths. As you inhale, allow your abdomen to expand; then, as you exhale slowlymake your yourself tall and look up. Looking up allows easier access to empowering and positive memories (Peper et al., 2017). Continue looking up and inhale slowly allow the abdomen to expand. Repeat this slow breath again.
On the third breath, while looking up, evoke a memory of someone in whose presence you felt at peace and who loves –you such as your grandmother, aunt or uncle or your dog. Reawaken that feeling associated with that memory. Allow a smile with soft eyes to come to your face as you experience the loving memory. Then, put your hands on your chest, take a breath as your abdomen to expands, and as you exhale, bring your hands away from your chest and stretch them out in front of you. At the same time, in your mind’s eye imagine sending good will to that person or conflict that previously evoked your stress response.
As you do this, you are not condoning what happened; instead, you are sending goodwill to that person’s positive aspect. From this perspective, everyone has an intrinsic component—however small—that some label as Christ nature or Buddha nature.
Why could this be effective? This practice short-circuits the automatic stress response and provides time to recenter. It interrupts ongoing rumination by shifting the mind away from thoughts about the person or event that induces stress and toward a positive memory. Evoking a loving memory from the past facilitates a reduction in arousal, evokes a positive mood, and decreases sympathetic nervous system activation (Speer & Delgado, 2017). Additionally, slower diaphragmatic breathing reduces sympathetic activation (Birdee et al., 2023; Siedlecki et al., 2022). By combining body and mind, we can pause and create the opportunity to respond positively rather than reacting with anger and hurt.
Practice sending goodwill the moment you wake up
So often when we wake up, we already anticipate the challenges and even the prospect of interacting with person or event heightens our defense reaction. Therefore, as soon as you wake up, sit at the edge of the bed, repeat the previous practice, Pause and Center. Then, as you sit at the edge of the bed, slightly smile with soft eyes, look up, inhale as your abdomen expand. Then, stamp your right foot into the floor while saying, “Today is a new day.” Next, inhale allowing your abdomen expand; as you look up, stamp your left foot on the floor while saying, “Today is a new day.” Finally, send goodwill to the person who previously triggered your defensive reaction.
Why could this be effective?
Looking up makes it easier to access positive memories and thoughts. Stamping your foot on the ground is a non-verbal expression of determination and anchors the thought of a new day, thereby focuses on new opportunities (Feldman, 2022).
Discuss your issue from the third-person perspective instead of the first-person perspective
When thinking, ruminating, talking, texting, or writing about the event, discuss it from the third-person perspective. Replace the first-person pronoun “I” with “she” or “he.” For example, instead of saying:
I was really pissed off when my boss criticized my work without giving any positive suggestions for improvement,
Say:
He was really pissed off when his boss criticized his work without offering any positive suggestions for improvement.
Why could this be effective? The act of substituting the third person pronoun for the first-person pronoun interrupts our automatic reactivity because it requires us to observe and change our language, which activating the frontal cortex. This process creates a psychological distance from our feelings, allowing for a more objective and calmer perspective on the situation. It effectively reducing stress by stepping back from the immediate emotional response (Moser et al., 2017). It means that you are no longer fully captured by the emotions, as you are simultaneously the observer of your own inner language and speech.
Compare yourself to others who are suffering more
When you feel sorry for yourself or hurt, take a breath, look upward, and compare yourself to others who are suffering much more. In that moment, consider yourself incredibly lucky compared to people enduring extreme poverty, bombings, or severe disfigurement. Be grateful for what you have.
Why could this be effective? The research data shows that if we have low self-esteem when we compare ourselves to people who are more successful (healthier, richer, or successful), we feel worse in comparison and if we compare ourselves to other who are suffering more we feel better (Aspinwall, & Taylor, 1993). The comparision relativize our suffering. Thus our own suffering become less significant compared to the other people’s severe suffering.
Research shows that when we compare ourselves to people who are more successful (healthier, richer, or more accomplished), we tend to feel worse—especially if we have low self-esteem. However, when we compare ourselves to others who are suffering more, we tend to feel better (Aspinwall, & Taylor, 1993). This comparison relativizes our suffering, making our own hardships and suffering seem less significant compared to the severe suffering of others.
Interrupt the stress response
When overwhelmed by a stress reaction, implement the recue techniques described in the article, Quick rescue techniques when stress (Peper, Oded and Harvey, 2024) and the blog to help reduce stress. https://peperperspective.com/2024/02/04/quick-rescue-techniques-when-stressed/
Conclusion
It is much easier to write and talk about these practices than to actually do them. Remembering and reminding yourself to implement them can be very challenging. It requires significant effort and commitment. In most cases, the benefits are not experienced immediately. However, when practiced many times over weeks and months, many people report feeling less resentment, experience a reduction in symptoms, and improvements in health and relationships.
*This blog was inspired by the podcast, No hard feelings, that featured psychologist Fred Luskin. It is an episode on Hidden Brain, produced by Shankar Vedantam (2025) and the wisdom taught by Dora Kunz (Kunz & Peper, 1983; Kunz and Peper, 1984a; Kunz and Peper, 1984b; Kunz and Peper, 1987).
Useful blog that complement the concepts in this blog
References
Aspinwall, L. G., & Taylor, S. E. (1993). Effects of social comparison direction, threat, and self-esteem on affect, self-evaluation, and expected success. Journal of Personality and Social Psychology, 64(5), 708–722. https://doi.org/10.1037/0022-3514.64.5.708
Birdee, G., Nelson, K., Wallston, K., Nian, H., Diedrich, A., Paranjape, S., Abraham, R., & Gamboa, A. (2023). Slow breathing for reducing stress: The effect of extending exhale. Complementary Therapies in Medicine, 73. https://doi.org/10.1016/j.ctim.2023.102937
Duan, S., Lawrence, A., Valmaggia, L., Moll, J. & Zahn, R. (2022). Maladaptive blame-related action tendencies are associated with vulnerability to major depressive disorder. Journal of Psychiatric Research, 145, 70-76. https://doi.org/10.1016/j.jpsychires.2021.11.043
Fast, N.J. & Tiedens, L.Z. (2010). Blame contagion: The automatic transmission of self-serving attributions. Journal of Experimental Social Psychology, 46(1), 97-106. https://doi.org/10.1016/j.jesp.2009.10.007
Feldman, Y. (2022). The Dialogical Dance-A Relational Embodied Approach to Supervision. In Butte, C. & Colbert, T. (Eds). Embodied Approaches to Supervision-The Listening Body. London: Routledge. https://www.amazon.com/Embodied-Approaches-Supervision-C%C3%A9line-Butt%C3%A9/dp/0367473348
Kunz, D. & Peper, E. (1983). Fields and Their Clinical Implications-Part III: Anger and How It Affects Human Interactions. The American Theosophist, 71(6), 199-203. https://www.researchgate.net/publication/280777019_Fields_and_their_clinical_implications-Part_III_Anger_and_how_it_affects_human_interactions
Kunz, D. & Peper, E. (1984a). Fields and Their Clinical Implications IV: Depression from the Energetic Perspective: Etiological Underpinnings. The American Theosophist, 72(8), 268-275. https://biofeedbackhealth.org/wp-content/uploads/2011/01/fields-and-their-clinical-implications-iv-depression-from-the-energetic-perspectivive.pdf
Kunz, D. & Peper, E. (1984b). Fields and Their Clinical Implications V: Depression from the Energetic Perspective: Treatment Strategies. The American Theosophist, 72(9), 299-306. https://biofeedbackhealth.org/wp-content/uploads/2011/01/fields-and-their-clinical-implications-part-v-depression-treatment-strategies.pdf
Kunz, D. & Peper, E. (1987). Resentment: A poisonous undercurrent. The Theosophical Research Journal. IV (3), 54-59. Also in: Cooperative Connection. IX (1), 1-5. https://www.researchgate.net/publication/387030905_Resentment_Continued_from_page_4
Lou, Y., Wang, T., Li, H., Hu, T. Y., & Xie, X. (2023). Blame others but hurt yourself: blaming or sympathetic attitudes toward victims of COVID-19 and how it alters one’s health status. Psychology & Health, 39(13), 1877–1898. https://doi.org/10.1080/08870446.2023.2269400
Moser, J. S., Dougherty, A., Mattson, W. I., Katz, B., Moran, T. P., Guevarra, D., Shablack, H., Ayduk, O., Jonides, J., Berman, M. G., & Kross, E. (2017). Third-person self-talk facilitates emotion regulation without engaging cognitive control: Converging evidence from ERP and fMRI. Scientific reports, 7(1), 4519. https://doi.org/10.1038/s41598-017-04047-3
Oneda, B., Ortega, K., Gusmão, J. et al. (2010). Sympathetic nerve activity is decreased during device-guided slow breathing. Hypertens Res, 33, 708–712. https://doi.org/10.1038/hr.2010.74
Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41. https://doi.org/10.5298/1081-5937-45.2.01
Russell, M. A., Smith, T. W., & Smyth, J. M. (2016). Anger Expression, Momentary Anger, and Symptom Severity in Patients with Chronic Disease. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 50(2), 259–271. https://doi.org/10.1007/s12160-015-9747-7
Siedlecki, P., Ivanova, T.D., Shoemaker, J.K. et al. (2022). The effects of slow breathing on postural muscles during standing perturbations in young adults. Exp Brain Res, 240, 2623–2631. https://doi.org/10.1007/s00221-022-06437-0
Speer, M. & Delgado, M. (2017).Reminiscing about positive memories buffers acute stress responses. Nat Hum Behav 1, 0093 (2017). https://doi.org/10.1038/s41562-017-0093
Suls J. (2013). Anger and the heart: perspectives on cardiac risk, mechanisms and interventions. Progress in cardiovascular diseases, 55(6), 538–547. https://doi.org/10.1016/j.pcad.2013.03.002
van Dinther, M., Hooghiemstra, A. M., Bron, E. E., Versteeg, A., Leeuwis, A. E., Kalay, T., Moonen, J. E., Kuipers, S., Backes, W. H., Jansen, J. F. A., van Osch, M. J. P., Biessels, G. J., Staals, J., van Oostenbrugge, R. J., & Heart-Brain Connection consortium (2024). Lower cerebral blood flow predicts cognitive decline in patients with vascular cognitive impairment. Alzheimer’s & dementia : the journal of the Alzheimer’s Association, 20(1), 136–144. https://doi.org/10.1002/alz.13408
Vedantma, S. (2025). Hidden Brain episode, No hard feelings. Accessed February 5, 2025. https://hiddenbrain.org/podcast/no-hard-feelings/
Willeumier, K., Taylor, D. V., & Amen, D. G. (2011). Decreased cerebral blood flow in the limbic and prefrontal cortex using SPECT imaging in a cohort of completed suicides. Translational psychiatry, 1(8), e28. https://doi.org/10.1038/tp.2011.28
Act now before history repeats itself
Posted: January 23, 2025 Filed under: education | Tags: Brexit, Gladwell, history, Musk, Nazi, Politics, Trump 20 CommentsOn November 8–9, 1923, Adolf Hitler and the Nazi Party launched a bold attempt to overthrow Germany’s federal government in Munich, aiming to establish a nationalist regime. Known as the Beer Hall Putsch, this failed coup grabbed global headlines, shocking the world. Hitler and his associates were quickly arrested, and after a dramatic 24-day trial, they were convicted of treason. Despite being sentenced to prison, Hitler served less than a year before his release—time he used to lay the groundwork for his infamous future.
Fast forward to January 6, 2021: history echoed in eerie ways. Fueled by false claims of a stolen election, groups like the Oath Keepers and Proud Boys, with the backing of then-President Donald Trump, stormed the U.S. Capitol in a desperate bid to block Joe Biden’s certification as the newly elected President. The attack left the nation reeling, its democratic institutions shaken.
By August 2024, over 1,400 individuals had been charged with federal crimes related to the insurrection, and more than 900 had been convicted. Yet, in a shocking twist, Trump—returning to the presidency—undermined the justice system on his first day back in office. He issued sweeping pardons for approximately 1,500 individuals and commuted the sentences of 14 key allies connected to the Capitol attack.
Are we seeing echoes of 1930s Germany in today’s America? In 1935, the Nuremberg Laws stripped citizenship from anyone not deemed “Aryan,” cementing a dangerous precedent of exclusion and authoritarianism. Now on the first day in office, President Trump President Donald Trump’s executive order that purports to limit birthright citizenship-
Fast forward to now: former President Donald Trump’s blanket clemency and pardons for Proud Boys and other January 6 participants seem to signal unconditional support for his loyal MAGA followers. The message is clear—carry out Trump’s agenda without fear of legal consequences because he’ll have your back. Could the Proud Boys become a modern-day equivalent of Hitler’s Brownshirts (Sturmabteilung, or SA)—used to protect Trump’s movement, suppress dissent, and disrupt political opposition? This question grows even more pressing in an age where social media wields enormous influence. With Elon Musk controlling X (formerly Twitter), critics worry about the platform’s role in shaping discourse. Musk’s actions and statements have led some to compare his influence to that of Joseph Goebbels, the Nazi Minister of Propaganda. My fears are heightened after Musk made gestures similarly to that associated with Nazi symbolism during Trump’s inauguration.

Read about the possible impact of the Trump policies in the New York Times, “Donald Trump Is Running Riot” by David French, the outstanding New York Times’ opinion writer.
How Did We Get Here? A Warning from History
How could this happen? It might seem that the majority of Americans support Trump’s actions, but the numbers tell a different story. In reality, only about 33% of eligible voters cast their ballots for Trump. Over one-third of eligible voters stayed home, choosing not to vote at all. To put it in perspective, Trump’s 2024 total of 77,284,118 votes fell short of Biden’s 81,284,666 votes in 2020. The difference wasn’t that Trump gained overwhelming support—it was that fewer people showed up for Harris, and 36% did not vote.
This scenario isn’t unique to America. Take Brexit, for example: In January 2020, the United Kingdom voted to leave the European Union, a decision driven by a passionate and sometimes misinformed minority. Now, just a few years later, many in England regret that choice, realizing the long-term consequences of their decision to leave the EU.
The truth is, in almost every major upheaval, it only takes about 30% of highly dedicated and committed individuals—some might even call them zealots—to shift the course of history. It was true for Brexit, it was true for Hitler, and is now true for Trump.
If you want to understand how this dynamic works, Malcolm Gladwell’s The Revenge of the Tipping Point offers invaluable insights into how a small but determined group can take control of the narrative and change the agenda for everyone.

Now is the time to act. It’s not too late to support democratic institutions and ensure the U.S. doesn’t slide into the abyss. Staying silent or staying home isn’t an option—democracy needs defenders–silence in the face of oppression is siding with the oppressor.
Compassionate Presence: Covert Training Invites Subtle Energies Insights
Posted: January 20, 2025 Filed under: attention, healing, meditation, mindfulness, relaxation, Uncategorized | Tags: being safe, compassion, energy, Energy healing, healing, reiki, spirituality, therapeutic touch Leave a commentAdapted from: Peper, E. (2015). Compassionate Presence: Covert Training Invites Subtle Energies Insights. Subtle Energies Magazine, 26(2), 22-25. https://www.researchgate.net/publication/283123475_Compassionate_Presence_Covert_Training_Invites_Subtle_Energies_Insights
“Healing is best accomplished when art and science are conjoined, when body and spirit are probed together. Only when doctors can brood for the fate of a fellow human afflicted with fear and pain do they engage the unique individuality of a particular human being…a doctor thereby gains courage to deal with the pervasive uncertainties for which technical skill alone is inadequate. Patient and doctor then enter into a partnership as equals.
I return to my central thesis. Our health care system is breaking down because the medical profession has been shifting its focus away from healing, which begins with listening to the patient. The reasons for this shift include a romance with mindless technology.” Bernard Lown, MD, The Lost art of healing: Practicing Compassion in Medicine (1999)

Therapeutic Touch healing by Dora Kunz.
I wanted to study with the healer and she instructed me to sit and observe, nothing more. She did not explain what she was doing, and provided no further instructions. Just observe. I did not understand. Yet, I continued to observe because she knew something, she did something that seemed to be associated with improvement and healing of many patients. A few showed remarkable improvement – at times it seemed miraculous. I felt drawn to understand. It was an unique opportunity and I was prepared to follow her guidance.
The healer was remarkable. When she put her hands on the patient, I could see the patient’s defenses melt. At that moment, the patient seemed to feel safe, cared for, and totally nurtured. The patient felt accepted for just who she was and all the shame about the disease and past actions appeared to melt away. The healer continued to move her hands here and there and, every so often, she spoke to the client. Tears and slight sobbing erupted from the client. Then, the client became very peaceful and quiet. Eventually, the session was finished and the client expressed gratitude to the healer and reported that her lower back pain and the constriction around her heart had been released, as if a weight had been taken from her body.
How was this possible? I had so many questions to ask the healer: “What were you doing? What did you feel in your hands? What did you think? What did you say so softly to the client?”
Yet she did not help me understand how I could do this. The main instruction the healer kept giving me was to observe. Yes, she did teach me to be aware of the energy fields around the person and taught me how I could practice therapeutic touch (Kreiger, 1979; Peper, 1986; Kunz & Peper,1995; Kunz & Krieger, 2004; Denison, 2004; van Gelder & Chesley, F, 2015). But she was doing much more and I longed to understand more about the process.
Sitting at the foot of the healer, observing for months, I often felt frustrated as she continued to insist that I just observe. How could I ever learn from this healer if she did not explain what I should do! Does the learning occur by activating my mirror neurons (Acharya & Shukla, 2012).? Similar instructions are common in spiritual healing and martial arts traditions – the guru or mentor usually tells an apprentice to observe and be there. But how can one gain healing skills or spiritual healing abilities if you are only allowed to observe the process? Shouldn’t the healer be demonstrating actual practices and teaching skills?
After many sessions, I finally realized that the healer’s instruction to to learn was to observe and observe. I began to learn how to be present without judging, to be present with compassion, to be present with total awareness in all senses, and to be present without frustration. The many hours at the foot of this master were not just wasted time. It eventually became clear that those hours of observation were important training and screening strategies used to insure that only those students who were motivated enough to master the discipline of non-judgmental observation, the discipline to be present and open to any experience, would continue to participate in the training process. I finally understood. I was being taught a subtle energies skill of compassionate, and mindful awareness. Once I, the apprentice, achieved this state, I was ready to begin work with clients and master technical aspects of the healing practice – but not before.
A major component of the healing skill that relies on subtle energies is the ability to be totally present with the client without judgment (Peper, Gibney & Wilson, 2005). To be peaceful, caring, and present seems to create an energetic ambiance that sets stage, creates the space, for more subtle aspects of the healing interaction. This energetic ambiance is similar to feeling the love of a grandparent: feeling total acceptance from someone who just knows you are a remarkable human being. In the presence of a healer with such a compassionate presence, you feel safe, accepted, and engaged in a timeless state of mind, a state that promotes healing and regeneration as it dissolves long held defensiveness and fear-based habits of holding others at bay. This state of mind provides an opportunity for worries and unsettled emotions to dissipate. Feeling safe, accepted, and experiencing compassionate love supports the bological processes that nurture regeneration and growth.
How different this is from the more common experience with health care/medical practitioners who have little time to listen and to be with a patient. We might experience a medical provider as someone who sees us only as an illness (the cancer patient, the asthma patient) instead of recognizing us as a human spirit who happens to have an illness ( a person with cancer or asthma). At times we can feel as though we are seen only as a series of numbers in a medical chart – yet we know we are more than that. People long to be seen. Often the medical provider interrupts with unrelated questions instead of listening. It becomes clear that the computerized medical record is more important than the human being seated there. We can feel more fragmented, less safe, when we are not heard, not understood.
As one 23 year old student reported after being diagnosed with a serious medical condition,”/ cried immediately upon leaving the physician’s office. Even though he is an expert on the subject, I felt like I had no psychological support. I was on Gabapentin, and it made me very depressed. I thought to myself: Is my life, as I know it, over?” (Peper, Martinez Aranda, P., & Moss, 2015).
The healing connection is often blocked, the absence of a human connection is so obvious. The medical provider may be unaware of the effect of their rushed behavior and lack of presence. They can issue a diagnosis based on the scientific data without recognizing the emotional impact on the person receiving it.
What is missing is compassion and caring for the patient. Sitting at the foot of the master healer is not wasted time when the apprentice learns how to genuinely attend to another with non-judgmental, compassionate presence. However, this requires substantial personal work. Possibly all healthcare providers should be required, or at least invited, to learn how to attain the state of mind that can enhance healing. Perhaps the practice of medicine could change if, as Bernard Lown wrote, the focus were once again on healing, “…which begins with listening to the patient.”
References
Acharya, S., & Shukla, S. (2012). Mirror neurons: Enigma of the metaphysical modular brain. Journal of natural science, biology, and medicine, 3(2), 118–124. https://doi.org/10.4103/0976-9668.101878
Denison, B. (2004). Touch the pain away: New research on therapeutic touch and persons with fibromyalgia syndrome. Holistic nursing practice, 18(3), 142-151. https://doi.org/10.1097/00004650-200405000-00006
Krieger, D. (1979). The therapeutic touch: How to use your hands to help or to heal. Vol. 15. Englewood Cliffs, NJ: Prentice-Hall. https://www.amazon.com/Therapeutic-Touch-Your-Hands-Help/dp/067176537X
Kunz, D. & Krieger, D. (2004). The spiritual dimension of therapeutic touch. Rochester, VT: Inner Traditions/Bear & Co. https://www.amazon.com/Spiritual-Dimension-Therapeutic-Touch/dp/1591430259/
Kunz, D., & Peper, E. (1995). Fields and their clinical implications. In Kunz, D. Spiritual Aspects of the Healing Arts. Wheaton, ILL: Theosophical Pub House, 213-222. https://www.amazon.com/Spiritual-Aspects-Healing-Arts-Quest/dp/0835606015
Lown, B. (1999). The lost art of healing: Practicing compassion in medicine. New York, NY: Ballantine Books. https://www.amazon.com/Lost-Art-Healing-Practicing-Compassion/dp/0345425979
Peper, E. (1986). You are whole through touch: An energetic approach to give support to a breast cancer patient. Cooperative Connection. VII (3), 1-6. Also in: (1986/87). You are whole through touch: Dora Kunz and Therapeutic Touch. Somatics. VI (1), 14-19. https://www.researchgate.net/publication/280884245_You_are_whole_through_touch_Dora_Kunz_and_therapeutic_touch
Peper, E. (2024). Reflections on Dora and the Healing Process, webinar presented to the Therapeutic Touch International Association, Saturday, December 14, 2024. https://youtu.be/skq9Chn-eME?si=HJNAhiUsgXSkqd_5
Peper, E., Gibney, K. H. & Wilson, V. E. (2005). Enhancing Therapeutic Success–Some Observations from Mr. Kawakami: Yogi, Teacher, Mentor and Healer. Somatics. XIV (4), 18-21. https://biofeedbackhealth.org/wp-content/uploads/2011/01/edited-enhancing-therapeutic-success-8-23-05.pdf
Peper, E., Martinez Aranda, P., & Moss, E. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback, 43(2), 103-109. https://doi.org/10.5298/1081-5937-43.2.04
Van Gelder, K & Chesley, F. (2015). A Most Unusual Life. Wheaton Ill: Theosophical Publishing House. https://www.amazon.com/Most-Unusual-Life-Clairvoyant-Theosophist/dp/0835609367
[1] I thank Peter Parks for his superb editorial support.
Implement your New Year’s resolution successfully[1]
Posted: December 29, 2024 Filed under: attention, behavior, CBT, cognitive behavior therapy, education, emotions, Exercise/movement, healing, health, self-healing | Tags: goal setting, health, lifestyle, motivation, performance, personal-development Leave a comment
Adapted from: Peper, E. Pragmatic suggestions to implement behavior change. Biofeedback.53(2), 41-45. https://doi.org/10.5298/1081-5937-53.02.05
Ready to crush your New Year’s resolutions and actually stick to them this time? Whether you’re determined to quit vaping or smoking, cut back on sugar and processed foods, reduce screen time, get moving, volunteer more, or land that dream job, sticking to your goals is the real challenge. We’ve all been there: kicking off the year with ambitious plans like, “I’ll work out every day,” or “I’m done with junk food for good.” But a few weeks in? The gym is a distant memory, the junk food stash is back, and those cigarettes are harder to let go of than expected.
So, how can you make this year different? Here are some tried-and-true tips to help you turn those resolutions into lasting habits:
Be clear of your goal and state exactly what you want to do (Pilcher et al., 2022; Latham & Locke, 2006).
Did you know your brain is super literal and doesn’t process “not” the way you think it does? For example, if you say, “I will not smoke,” your brain has to first imagine you smoking, then mentally cross it out. Guess what? By rehearsing the act of smoking in your mind, you’re actually increasing the chances that you’ll light up again.
Think of it like this: hand a four-year-old a cup of hot chocolate and ask them to walk it over to someone across the room. Halfway there, you call out, “Be careful, don’t spill it!” What usually happens? Yep, the hot chocolate spills. That’s because the brain focuses on “spill,” not the “don’t.” Now, imagine instead you say, “You’re doing great! Keep walking steadily.” Positive framing reinforces the action you want to see. The lesson is to reframe your goals in a way that focuses on what you want to achieve, not what you’re trying to avoid. Let’s look at some examples to get you started:
| Negative framing | Positive framing |
| I plan to stop smoking | I choose to become a nonsmoker |
| I will eat less sugar and ultra-processed foods | I will shop at the farmer’s market, buy more fresh vegetable and prepare my own food. |
| I will reduce my negative thinking (e.g., the glass is half empty). | I will describe events and thoughts positively (e.g., the class is half full). |
Describe what you want to do positively.
Be precise and concrete.
The more specific you can describe what you plan to do, the more likely will it occur as illustrated in the following examples.
| Imprecise | Concrete and specific |
| I will begin exercising. | I will buy the gym membership next week Monday and will go to the gym on Monday, Wednesday and Friday right after work at 5:30pm for 45 minutes. |
| I will reduce my angry outbursts, | Before I respond, I will take a slow breath, look up, relax my shoulders and remind myself that the other person is doing their best. |
| I want to limit watching streaming videos | At home, I will move the couch so that it does not face the large TV screen, and I have enrolled in a class to learn another language and I will spent 30 minutes in the evening practicing the new language. |
| I will stop smoking | When I feel the initial urge to smoke, I stand up, do a few stretches, and practice box breathing and remind myself that I am a nonsmoker. |
Describe in detail what you will do.
Identify the benefits of the old behavior that you want to change and how you can achieve the same benefits with your new behavior. (Peper et al, 2002)
When setting a New Year’s resolution, it’s easy to focus on the perks of the new behavior and the harms of the old behavior while overlooking the benefits your old habit provided. However, if you don’t plan ways to achieve the same benefits, the old behavior provided, it’s much harder to stick to your goal.
Before diving into your new resolution, take a moment to reflect. What did your old behavior do for you? What needs did it meet? Once you identify those, you can develop strategies to achieve the same benefits in healthier, more constructive ways.
For example, let’s say your goal is to stop smoking. Smoking might have helped you relax during stressful moments or provided a social activity with friends. To make the switch, you’ll need to find alternatives that deliver similar results, like practicing deep-breathing exercises to manage stress or inviting friends for a walk instead of a smoke break. By creating a plan to meet those needs, you’ll set yourself up for lasting success.
| Benefits of smoking | How to achieve the same benefits when being a none smoker |
| Stress reduction | I will learn relaxation and diaphragmatic breathing. The moment, I feel the urge to smoke, I sit up, look up, raise my shoulder and dropped them, and breathe slowly |
| Breaks during work | I will install a reminder on my cellphone to ping and each time it pings, I stop, stand up, walk around and stretch. |
| Meeting with friends | I will tell my friends, not to offer me a cigarette and I will spent time with friends who are non-smokers. |
| Rebelling against my parents who were opposed to smoking | I will explore how to be independent without smoking |
Describe your benefits and how you will achieve them.
Reduce the cues that evoke the old behavior and create new cues that will trigger the new behavior (Peper & Wilson, 2021).
A lot of our behavior is automatic—shaped by classical conditioning, just like Pavlov’s dog. Remember the famous experiment? Pavlov paired the sound of a bell with food, and after a while, the bell alone made the dog salivate (McLeod, 2024). We’re not so different.
Think about it: if you’ve gotten into the habit of smoking in your car, simply sitting in the driver’s seat can trigger the automatic urge to grab a cigarette. Or, if you tend to feel depressed when you’re home but better when you’re out with friends, your home environment might be acting as a cue for those feelings.
Interestingly, many people find it easier to change habits in a new environment. Why? Because there are no built-in triggers to reinforce the behavior they’re trying to change. This highlights how much of what we often call “addiction” might actually be conditioned behavior, reinforced by familiar cues in our surroundings. By recognizing the power of these triggers can help you disrupt old patterns. By creating a fresh environment or consciously changing your responses to cues, you can take control and start forming new, healthier habits.
This concept has been understood for centuries by some hunting and gathering societies. When something tragic happened—like the death of a family member in a hut—the community would often burn the hut to “eliminate the evil spirit.” Beyond the spiritual aspect, this practice served a practical purpose: it removed all the physical cues that reminded people of their loss, making it easier to focus on the present and move forward.
Of course, I’m not suggesting you destroy your home. But the underlying principle still holds true in modern times. In fact, many Northern European cultures incorporate a version of this idea through the ritual of Spring Cleaning. By decluttering, rearranging furniture, and refreshing the home, the old cues are removed and create a sense of renewal.
So often we forget that cues in our environment play a powerful role in triggering our behavior. By identifying the triggers that evoke old habits and finding ways to remove or change them, you can create a fresh environment that supports your goals. For example, if you’re trying to stop snacking on junk food late at night, consider rearranging your pantry so the tempting items are out of sight—or better yet, replace them with healthier options. Small changes like this can have a big impact on your ability to stay on track.
| Cues that triggered the behavior | How cues were changed |
| In the evening going to the kitchen and getting the chocolate from the cupboard. | Buying fruits and have them on the table and not buying chocolate. If I do buy chocolate store it on the top shelf away so that I do not see it or store it in the freezer. |
| Getting home and being depressed. | Clean the house, change the furniture around and put positive picture high up on the wall. |
| Smoking in the car. | Replace the car with another car that no one had smoked in and spray the care with pine scent. |
Identify the cues that trigger your behavior and how you changed them.
Identify the first sensation that triggered the behavior you would like to change.
Whether it’s smoking, drinking, scratching your skin, spiraling into negative thoughts, or eating too many pastries, once a behavior starts, it can feel nearly impossible to stop. That’s why the key is to catch yourself before the habit takes over., t’s much easier to interrupt a pattern at the very first sign—the initial trigger—rather than after you’ve fully dived into the behavior. Yet how often do we find ourselves saying, “Next time, I’ll do it differently”?
Here’s the strategy: identify the first trigger. This could be a physical sensation, an emotion, a thought, or an external cue. Once you’re aware of that first flicker of a trigger, redirect your thoughts and actions toward what you actually want, rather than letting the automatic behavior take control. For example:
I just came home at 10:15 PM and felt lonely and slightly depressed. I walked into the kitchen, opened the fridge, grabbed a beer, and drank it. Then, I reached for another bottle.
Observing this behavior, the first trigger was the loneliness and slight depression upon arriving home. Recognizing that feeling in the moment offers an opportunity to pause and make a conscious choice. Instead of heading to the fridge, you could redirect your actions—call a friend, go for a quick walk, or write down your thoughts in a journal. By catching that initial trigger, you can focus yourself toward healthier behaviors and break the cycle.
| First sensation | Changed response to the sensation |
| I observed that the first sensation was feeling tired and lonely. | When I entered the house, instead of going to the kitchen, I stretched, looked up and took a deep breath and then called a close friend of mine. We talked for ten minutes and then I went to bed. |
Identify your first sensation and how you changed your behavior.
Incorporate social support and social accountability (Drageset, 2021).
Doing something on your own often requires a lot of willpower, and sticking to it every time can feel like an uphill battle. Take this example:
My goal is to exercise every other morning. But last night, I stayed up late and felt tired in the morning, so I skipped my workout.
Sound familiar? Now imagine if I’d planned to meet a workout buddy. Knowing someone was counting on me would’ve gotten me out of bed, even if I was tired, because I wouldn’t want to let them down.
Accountability can make all the difference. Another powerful strategy is sharing your goals publicly. When you announce your plans on social media or to friends and family, you create a sense of commitment—not just to yourself but to others. It’s like having a built-in support system cheering you on and holding you accountable. Whether it’s finding a partner, joining a group, or sharing your progress online, involving others can help turn your resolutions into habits you’re more likely to stick with.
Describe a strategy to increase social support and accountability.
Be honest in identifying what motivates you.
Exercising, eating healthy foods, thinking positively, or being on time are laudable goals; however, it often feels like work doing the “right” thing. To increase success, analyze what really helped you be successful. For example:
Many years ago, I decided that I should exercise more. Thus, I drove from house to the track and ran eight laps. I did this for the next three weeks and then stopped exercising. Eventually, I pushed myself again to exercise and after a while stopped again. The same pattern kept repeating. I would exercise and fall off the wagon and stop. Later that fall, I met a woman who was a jogger and we became friends and for the next year we jogged together and even did races. During this time, I did not experience any effort to go jogging. After a year, she broke up with me and once again, I had to use willpower to go jogging and my old pattern emerged and after a few days I stopped jogging even though I felt much better after having jogged.
I finally, asked what is going on? I realized that the joy of the jogging was running with a friend. Once, I recognized this, instead using will power to go running, I spent my willpower finding people with whom I could exercise. With these new friends, running did not depend upon my willpower– It only depended on making running dates with my new friends.
Explore factors that will allow you to do your activity without having to use willpower.
Conclusion
These seven strategies are just a starting point—there are countless other techniques that can help you stick to your New Year’s resolutions. For example, keeping a log, setting reminders, or rewarding yourself for progress are all powerful ways to stay on track. The real magic happens when your new behavior becomes part of your routine—embedded in your habitual patterns. The more automatic it feels, the greater your chances of long-term success.
So, take joy in identifying, implementing, and maintaining your resolutions. Let them enhance your well-being and become second nature. Share your successful strategies with me and others—it could be just the inspiration someone else needs to achieve their goals, too.
References
Drageset, J. (2021). Social Support. In: Haugan G, Eriksson M, editors. Health Promotion in Health Care – Vital Theories and Research [Internet]. Cham (CH): Springer, Chapter 11. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585650/ https://doi.org/10.1007/978-3-030-63135-2_11
Latham, G. P., & Locke, E. A. (2006). Enhancing the Benefits and Overcoming the Pitfalls of Goal Setting. Organizational Dynamics, 35(4), 332–340. https://doi.org/10.1016/j.orgdyn.2006.08.008
McLeod, S. (2024). Classical Conditioning: How It Works With Examples.Simple Psychology. Accessed December 29, 2024. https://www.simplypsychology.org/classical-conditioning.html
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. (Pp 185-192). https://he.kendallhunt.com/make-health-happen
Peper, E. & Wilson, V. (2021). Optimize the learning state: techniques and habits. Biofeedback, 9(2), 46-49. https://doi.org/10.5298/1081-5937-49-2-04
Pilcher, S., Schweickle, M. J., Lawrence, A., Goddard, S. G., Williamson, O., Vella, S. A., & Swann, C. (2022). The effects of open, do-your-best, and specific goals on commitment and cognitive performance. Sport, Exercise, and Performance Psychology, 11(3), 382–395. https://doi.org/10.1037/spy0000301
For detailed suggestions, see the following blogs:
[1] Edited with the help of ChatGPT.
Pragmatic techniques for monitoring and coaching breathing
Posted: December 14, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, emotions, meditation, mindfulness, neurofeedback, Pain/discomfort, posture, relaxation, self-healing, Uncategorized | Tags: art, books, Breathing rate, coaching, FlowMD app, nasal breathing, personal-development, self-monitoring, writing 4 CommentsDaniella Matto, MA, BCIA BCB-HRV , Erik Peper, PhD, BCB, and Richard Harvey, PhD
Adapted from: Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
This blog aims to describe several practical strategies to observe and monitor breathing patterns to promote effortless diaphragmatic breathing. The goal of these strategies is to foster effortless, whole-body diaphragmatic breathing that promote health.
Breathing is usually covert and people are not usually aware of their breathing rate (breaths per minute) or pattern (abdominal or thoracic, breath holding or shallow breathing) unless they have an illness such as asthma, emphysema or are performing physical activity (Boulding et al, 2015)). Observing breathing is challenging; awareness of respiration often leads to unaware changes in the breath pattern or to an attempt to breathe perfectly (van Dixhoorn, 2021). Ideally breathing patterns should be observed/monitored when the person is unaware of their breathing pattern and the whole body participates (van Dixhoorn, 2008). A useful strategy is to have the person perform a task and then ask, “What happened to your breathing?”. For example, ask a person to simulate putting a thread through the eye of a needle or quickly look to the extreme right and left while keeping their head still. In almost all cases, the person holds their breath (Peper et al., 2002).
Teaching effortless slow diaphragmatic breathing is a precursor of Heart rate variability (HRV) biofeedback and is based on slow paced breathing (Lehrer & Gevirtz, 2014; Steffen et al., 2017; Shaffer and Meehan, 2020). Mastering effortless diaphragmatic breathing is a powerful tool in the treatment of a variety of physical, behavioural, and cognitive conditions; however, to integrate this method into clinical or educational practice is easier said than done. Clients with dysfunctional breathing patterns often have difficulty following a breath pacer or mastering effortless breathing at a slower pace.
The purpose of this paper is to describe a few simple strategies that can be used to observe and monitor breathing patterns, provide economic strategies for observation and training, and suggestions to facilitate effortless diaphragmatic breathing.
Strategies to observe and monitor breathing pattern
Observation of the breathing patterns
- Is the breathing through the nose or mouth? Nose is usually better (Watso et al., 2023; Nestor, 2020).
- Does the abdomen expand during inhalation and constricts during exhalation or does the chest expand and rise during inhalation and fall during exhalation? Abdominal movement is usually better.
- Is exhalation flow softly or explosively like a sigh? Slow flow exhalation is preferred.
- Is the breath held or continues during activities? In most cases continued breathing is usually better.
- Does the person gasp before speaking or allows to speak while normally exhaling?
- What is the breathing rate (breaths per minute)? When sitting peacefully less than 14 breaths/minute is usually better and about 6 breaths per minute to optimize HRV
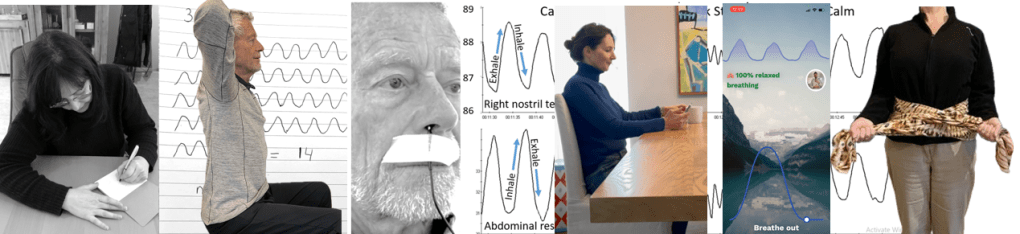
Physiological monitoring.
- Monitoring breathing with strain gauges around the abdomen and chest, and heart rate is the most common approach to identify the location of breath, the breathing pattern and heart rate variability. The strain gauges are placed around the chest and abdomen and heart rate is monitored with a blood volume pulse amplitude sensor from the finger. representative recording shows the effect of thoughts on breathing, heartrate and pulse amplitude of which the participant is totally unaware as shown in Figure 1.
Figure 1. Physiological recording of breathing patterns with strain gauges.
- Monitoring breathing with a thermistor placed at the entrance of the nostril that has the most airflow (nasal patency) (Jovanov et al., 2001; Lerman et al., 2016). When the person exhales through the nose, the thermistor temperature increases and decreases when they inhale. A representative recording of a person being calm, thinking a stressful thought. and being calm. Although there were significant changes as indicated by the change in breathing patterns, the person was unaware of the changes as shown in Figure 2.
Figure 2. Use of a thermistor to monitor breathing from the dominant nostril compared to the abdominal expansion as monitored by a strain gauge around the abdomen.
- Additional physiological monitoring approaches. There are many other physiological measures can be monitored to such as end-tidal carbon dioxide (EtCO2), a non-invasive measurement of the amount of carbon dioxide (CO2) in exhaled breath (Meuret et al., 2008; Meckley, 2013); scalene/trapezius EMG to identify thoracic breathing (Peper & Tibbett, 1992; Peper & Tibbets, 1994); low abdominal EMG to identify transfers and oblique tightening during exhalation and relaxation during inhalation (Peper et al., 2016; and heart rate to monitor cardiorespiratory synchrony (Shaffer & Meehan, 2020). Physiological monitoring is useful; since, the clinician and the participant can observe the actual breathing pattern in real time, how the pattern changes in response the cognitive and physical tasks, and used for feedback training. The recorded data can document breathing problems and evidence of mastery.
The challenges of using physiological monitoring arethat the equipment may be expensive, takes skill to operate and interpret the data, and is usually located in the office and not at home.
Economic strategies for observation and training breathing
To complement the physiological monitoring and allow observations outside the office and at home, some of the following strategies may be used to observe breathing pattern (rate and expansion of the breath in the body), and suggestion to facilitate effortless diaphragmatic breathing. These exercises make excellent homework for the client. Practicing awareness and internal self-regulation by the client outside the clinic contributes enormously to the effect of biofeedback training (Wilson et al., 2023),
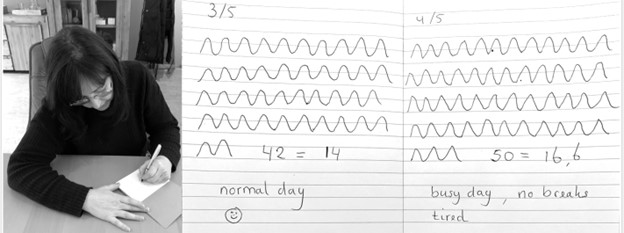
Observe breathing rate: Draw the breathing pattern
Take a piece of paper, a pen and a timer, set to 3 minutes. Start the timer. Upon inhalation draw the line up and upon exhalation draw the line down, creating a wave. When the timer stops, after 3 minutes, calculate the breathing rate per minute by dividing the number of waves by 3 as shown in Figure 3.
Figure 3. Drawing the breathing pattern for three minutes during two different days.
From these drawings, the breathing rate become evident. Many individuals are often surprised to discover that their breathing rate increased during periods of stress, such as a busy day with no breaks, compared to their normal days.
Monitoring and training diaphragmatic breathing
The scarf technique for abdominal feedback
Many participants are unaware that they are predominantly breathing in their chest and their abdomen expansion is very limited during inhalation. Before beginning, have participant loosen their belt and or stand upright since sitting collapsed/slouched or having the waist constriction such as a belt of tight constrictive clothing that inhibits abdominal expansion during inhalation.
Place the middle part of a long scarf or shawl on your lower back, take the ends in both hands and cross the ends: your left hand is holding the right part of the scarf, and the right hand is holding the left end of the scarf. Give a bit of a pull, so you can feel any movement of the scarf. When breathing more abdominally you will feel a pull at the ends of the scarf as you lower back, and flanks will expand as shown in Figure 4.

Figure 4. Using a scarf as feedback.
FlowMD app
A recent cellphone app, FlowMD, is unique because it uses the cellphone camera to detect the subtle movements of the chest and abdomen (FlowMD, 2024). It provides real time feedback of the persons breathing pattern. Using this app, the person sits in front of their cellphone camera and after calibration, the breathing pattern is displayed as shown in Figure 5.

Figure 5. Training breathing with FlowMD,.
Suggestions to optimize abdominal breathing that may lead to a slower breath rate when the client practices the technique
Beach pose
By locking the upper chest and sitting up straight it is often easier to breathe so that the abdomen can expand and constrict. Place your hands behind your head and Interlock your finger of both hands, pull your elbows back and up. The person can practice this either laying down on their back or sitting straight up at the edge of the chair as shown in Figure 6.

Figure 6. Sitting erect with the shoulders pulled back and up to allow abdominal expansion and constriction as the breathing pattern.
Observe the effect of posture on breathing
Have the person sit slouched/collapsed like a letter C and take a few slow breath, then have them sit up in a tall and erect position and take a few slow breaths. Usually they will observe that it is easier to breathe slower and lower and tall and erect.
Using your hands for feedback to guide natural breathing
Holding your hands with index fingers and thumbs touching the lower abdomen. When inhaling the fingers and thumbs separate and when exhaling they touch again (ensuring a full exhale and avoiding over breathing). The slight increase in lower abdominal muscle tension during the exhalation and relaxation during inhalation and the abdominal wall expands can also be felt with fingertips as shown in Figure 7.
Figure 7. Using your hands and finger for feedback to guide the natural breathing of expansion and constriction of the abdomen. Reproduced by permission from Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Coaching suggestions
There are many strategies to observe, teach and implement effortless breathing (Peper et al., 2024).. Even though breathing is natural and babies and young children breathe diaphragmatically as their large belly expands and constricts. Yet, in many cases the natural breathing shifts to dysfunctional breathing for multiple reasons such as chronic triggering defense reactions to avoiding pain following abdominal surgery (Peper et al, 2015). When participants initially attempt to relearn this natural pattern, it can be challenging especially, if the person habitually breathes shallowly, rapidly and predominantly in their chest.
When initially teaching effortless breathing, have the person exhale more air than normal without the upper chest compressing down and instead allow the abdomen comes in and up thereby exhaling all the air. If the person is upright then allow inhalation to occur without effort by letting the abdominal wall relaxes and expands. Initially inhale more than normal by expanding the abdomen without lifting the chest. Then exhale very slowly and continue to breathe so that the abdomen expands in 360 degrees during inhalation and constricts during exhalation. Let the breathing go slower with less and less effort. Usually, the person can feel the anus dropping and relaxing during inhalation.
Another technique is to ask the person to breathe in more air than normal and then breathe in a little extra air to completely fill the lungs, before exhaling fully. Clients often report that it teaches them to use the full capacity of the lungs.
The goal is to breath without effort. Indirectly this can be monitored by finger temperature. If the finger temperature decreases, the participant most likely is over-breathing or breathing with too much effort, creating sympathetic activity; if the finger temperature increases, breathing occurs slower and usually with less effort indicating that the person’s sympathetic activation is reduced.
Conclusion
There are many strategies to monitor and coach breathing. Relearning diaphragmatic breathing can be difficult due to habitual shallow chest breathing or post-surgical adaptations. Initial coaching may involve extended exhalations, conscious abdominal expansion, and gentle inhalation without chest movement. Progress can be monitored through indirect physiological markers like finger temperature, which reflects changes in sympathetic activity. The integration of these techniques into clinical or educational practice enhances self-regulation, contributing significantly to therapeutic outcomes. In this article we provided a few strategies which may be useful for some clients.
Additional blogs on breathing
https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
REFERENCES
Boulding, R., Stacey, R., & Niven, N. (2016). Dysfunctional breathing: a review of the literature and proposal for classification. European Respiratory Review, 25(141),: 287-294. https://doi.org/10.1183/16000617.0088-2015
FlowMD. (2024). FlowMD app. Accessed December 13, 2024. https://desktop.flowmd.co/
Jovanov, E., Raskovic, D., & Hormigo, R. (2001). Thermistor-based breathing sensor for circadian rhythm evaluation. Biomedical sciences instrumentation, 37, 493–497. https://pubmed.ncbi.nlm.nih.gov/11347441/
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Lerman, J., Feldman, D., Feldman, R. et al. Linshom respiratory monitoring device: a novel temperature-based respiratory monitor. (2016). Can J Anesth/J Can Anesth, 63, 1154–1160. https://doi.org/10.1007/s12630-016-0694-y
Meckley, A. (2013). Balancing Unbalanced Breathing: The Clinical Use of Capnographic Biofeedback. Biofeedback, 41(4), 183–187. https://doi.org/10.5298/1081-5937-41.4.02
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (2008). Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of psychiatric research, 42(7), 560–568. https://doi.org/10.1016/j.jpsychires.2007.06.005
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath-New-Science-Lost-Art/dp/0735213615/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make Health Happen. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Peper, E., & Tibbetts, V. (1992). Fifteen-month follow-up with asthmatics utilizing EMG/incentive inspirometer feedback. Biofeedback and self-regulation, 17(2), 143–151. https://doi.org/10.1007/BF01000104
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. https://biofeedbackhealth.org/wp-content/uploads/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Shaffer, F. and Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., and Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
van Dixhoorn, J.V. (2008). Whole-body breathing. Biofeedback, 36,54–58. https://www.euronet.nl/users/dixhoorn/L.513.pdf
van Dixhoorn, J.V. (2021). Functioneel ademen-Adem-en ontspannings oefeningen voor gevorderden. Amersfoort: Uiteveriy Van Dixhoorn. https://www.bol.com/nl/nl/p/functioneel-ademen/9300000132165255/
Watso, J. C., Cuba, J.N., Boutwell, S.L, Moss, J…(2023). Acute nasal breathing lowers diastolic blood pressure and increases parasympathetic contributions to heart rate variability in young adults. American Journal of Physiology Regulatory, Integrative and Comparative Physiology.
325I(6), R797-R80. https://doi.org/10.1152/ajpregu.00148.2023
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Health Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 415 338 7683 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com
Suggestions for mastering and generalizing breathing skills
Posted: October 30, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cellphone, cognitive behavior therapy, emotions, ergonomics, healing, health, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: abdominal beathing, anxiety, diaphragmatic braething, health, hyperventilation, meditation, mental-health, mindfulness, mouth breathing, Toning 3 CommentsAdapted from: Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/

Breathing techniques are commonly employed with complimentary treatments, biofeedback, neurofeedback or adjunctive therapeutic strategies to reduce stress and symptoms associated with excessive sympathetic arousal such as anxiety, high blood pressure, insomnia, or gastrointestinal discomfort. Even though it seems so simple, some participants experience difficulty in mastering effortless breathing and/or transferring slow breathing skills into daily life. The purpose of this article is to describe: 1) factors that may interfere with learning slow diaphragmatic breathing (also called cadence or paced breathing, HRV or resonant frequency breathing along with other names), 2) challenges that may occur when learning diaphragmatic breathing, and 3) strategies to generalize the effortless breathing into daily life.
Background
A simple two-item to-do list could be: ‘Breathe in, breathe out.’ Simple things are not always easy to master. Mastering and implementing effortless ‘diaphragmatic’ or ‘abdominal belly’ breathing may be simple, yet not easy. Breathing is a dynamic process that involves the diaphragm, abdominal, pelvic floor and intercostal muscles that can include synchronizing the functions of the heart and lungs and may result in cardio-respiratory synchrony or coupling, as well as ‘heart-rate variability breathing training (Codrons et al., 2014; Dick et al., 2014; Elstad et al., 2018; Maric et al., 2020; Matic et al., 2020). Improving heart-rate variability is a useful approach to reduce symptoms of stress and promotes health and reduce anxiety, asthma, blood pressure, insomnia, gastrointestinal discomfort and many other symptoms associated with excessive sympathetic activity (Lehrer & Gevirtz, 2014; Xiao et al., 2017; Jerath et al., 2019; Chung et al., 2021; Magnon et al., 2021; Peper et al., 2022).
Breathing can be effortful and In some cases people have dysfunctional breathing patterns such as breath holding, rapid breathing (hyperventilation), shallow breathing and lack of abdominal movement. This usually occurs without awareness and may contribute to illness onset and maintenance. When participants learn and implement effortless breathing, symptoms often are reduced. For example, when college students are asked to practice effortless diaphragmatic breathing twenty-minutes a day for one week, as well as transform during the day dysfunction breathing patterns into diaphragmatic breathing, they report a reduction in shallow breathing, breath holding,, and a decrease of symptoms as shown in Fig 1 (Peper et al, 2022).

Figure 1. Percent of people who reported that their initial symptoms improved after practicing slow diaphragmatic breathing for twenty minutes per day over the course of a week (reproduced from: Peper et al, 2022).
Most students became aware of their dysfunctional breathing and substituted slow, diaphragmatic breathing whenever they realized they were under stress; however, some students had difficulty mastering ‘effortless’ (e.g., automated, non-volitional) slow, diaphragmatic breathing that allowed abdominal expansion during inhalation.
Among those had more difficulty, they tended to have almost no abdominal movement (expansion during inhalation and abdominal constriction during exhalation). They tended to breathe shallowly as well as quickly in their chest using the accessory muscles of breathing (sternocleidomastoid, pectoralis major and minor, serratus anterior, latissimus dorsi, and serratus posterior superior).
The lack of abdominal movement during breathing reduced the movement of lymph as well as venous blood return in the abdomen; since; the movement of the diaphragm (the expansion and constriction of the abdomen) acts a pump. Breathing predominantly in the chest may increase the risk of anxiety, neck, back and shoulder pain as well as increase abdominal discomfort, acid reflux, irritable bowel, dysmenorrhea and pelvic floor pain (Banushi et al., 2023; Salah et al., 2023; Peper & Cohen, 2017; Peper et al., 2017; Peper et al., 2020, Peper et al., 2023). Learning slow, diaphragmatic or effortless breathing at about six breaths per minute (resonant frequency ) is also an ‘active ingredient’ in heartrate variability (HRV) training (Steffen et al., 2017; Shaffer & Meehan, 2020).
1. Factors that interfere with slow, diaphragmatic breathing
Difficulty allowing the skeletal and visceral muscles in the abdomen to expand or constrict in ‘three-dimensions’ (e.g., all around you in 360 degrees) during inhalation or exhalation. Whereas internal factors under volitional control and will mediate breathing practices, external factors can restrict and moderate the movement of the muscles. For example:
Clothing restrictions (designer jeans syndrome). The clothing is too tight around the abdomen; thereby, the abdomen cannot expand (MacHose & Peper, 1991; Peper et al., 2016). An extreme example were the corsets worn in the late 19th century that was correlated with numerous illnesses.
Suggested solutions and recommendations: Explain the physiology of breathing and how breathing occurs by the diaphragmatic movement. Discuss how babies and dogs breathe when they are relaxed; namely, the predominant movement is in the abdomen while the chest is relaxed. This would also be true when a person is sitting or standing tall. Discuss what happens when the person is eating and feels full and how they feel better when they loosen their waist constriction. When their belt is loosened or the waist button of their pants is undone, they usually feel better.
Experiential practice. If the person is wearing a belt, have the person purposely tighten their belt so that the circumference of the stomach is made much smaller. If the person is not wearing a belt, have them circle their waist with their hands and compress it so that the abdomen can not expand. Have them compare breathing with the constricted waist versus when the belt is loosened and then describe what they experienced.
Most participants will feel it is easier to breathe and much more comfortable when the abdomen is not constricted.
Previous abdominal injury. When a person has had abdominal surgery (e.g., Cesarean section, appendectomy, hernia repair, or episiotomy), they unknowingly may have learned to avoid pain by not moving (relaxing or tensing) the abdomen muscles (Peper et al., 2015; Peper et al., 2016). Each time the abdomen expands or constricts, it would have pulled on the injured area or stitches that would have cause pain. The body immediately learns to limit movement in the affected area to avoid pain. The reduction in abdominal movement becomes the new normal ‘feeling’ of abdominal muscle inactivity and is integrated in all daily activities. This is a process known as ‘learned disuse’ (Taub et al., 2006). In some cases, learned disuse may be combined with fear that abdominal movement may cause harm or injury such as after having a kidney transplant. The reduction in abdominal movement induces shallow thoracic breathing which could increase the risk of anxiety and would reduce abdominal venous and lymph circulation that my interfere with the healing.
Suggested solutions and recommendations. Discuss the concept of learned disuse and have participant practice abdominal movement and lower and slower breathing.
Experiential practices: Practicing abdominal movements
Sit straight up and purposely exhale while pulling the abdomen in and upward and inhale while expanding the abdomen. Even with these instructions, some people may continue to breathe in their chest. To limit chest movement, have the person interlock their hands and bring them up to the ceiling while going back as far as possible. This would lock the shoulders and allows the abdomen to elongate and thereby increase the diaphragmatic movement by allowing the abdomen to expand. If people initially have held their abdomen chronically tight then the initial expansion of abdomen by relaxing those muscle occurs with staccato movement. When the person becomes more skilled relaxing the abdominal muscles during inhalation the movement becomes smoother.
Make a “psssssst” sound while exhaling. Sit tall and erect and slightly pull in and up the abdominal wall and feel the anus tightening (pulling the pelvic floor up) while making the sound. Then allow inhalation to occur by relaxing the stomach and feeling the anus go down.
Use your hands as feedback. Sit up straight, placing one hand on the chest and another on the abdomen. While breathing feel the expansion of the abdomen and the contraction of the abdomen during exhalation. Use a mirror to monitor the chest-muscle movement to ensure there is limited rising and falling in this area.
Observe the effect of collapsed sitting. When sitting with the lower back curled, there is limited movement in the lower abdomen (between the pubic region and the umbilicus/belly button) and the breathing movement is shallower without any lower pelvic involvement (Kang et al., 2016). This is a common position of people who are working at their computer or looking at their cellphone.
Experiential practice: looking at your cellphone
Sit in a collapsed position and look down at your cellphone. Look at the screen and text as quickly as possible.
Compare this to sitting up and then lift the cell phone at eye level while looking straight ahead at the cellphone. Look at the screen and text as quickly as possible.
Observe how the position effected your breathing and peripheral awareness. Most likely, your experience is similar those reported by students. Close to 85%% of students who complete this activity reported that their breathing was shallower sitting slouched versus erect and about 85% of the students reported that their peripheral awareness and vision improved when sitting erect (Peper et al., 2024).
Suggested solutions and recommendations. Be aware how posture affect breathing. While sitting, place a rolled-up towel against the lower back so that the person sits more erect which would allow the abdomen to expand when inhaling.
Self-image, self-esteem, and confidence. Participants may hold their abdomen in because they want to look slim (sometimes labeled as the “hourglass syndrome” associate expanding the abdomen as unattractive (PTI, 2023). A flat abdomen is culturally reinforced by social media and fashion models and encouraged in some activities such as ballet. On the other hand, some people purposely puff up their chest to increase size and dominance (Cohen & Leung, 2009).
Suggested solutions and recommendations. Discuss the benefits of diaphragmatic breathing including its ability to reduce anxiety in social settings that may enhance confidence. Similar to an earlier suggestion, have the person explore clothing with a looser waist that still supports feelings of attractiveness and power.
Feeling anxious, fearful or threatened. The normal physiological stress reaction is a slight gasp with the tightening of the abdomen muscles for protection when a stressor occurs (Gilbert, 1998; Ekerholt & Bergland., 2008). The stressor can be an actual physical event, social situation or thoughts and emotions. Shallow breathing is a natural self-protective response. This pattern is often maintained until one feels ‘safe’ enough to relax, which for many can have a duration of the entire day or until finding the relative safety of sleep.
Suggested solutions and recommendations. Discuss how the physiological stress reaction is a normal response pattern that the person most likely learned in early childhood for self-protection. This pattern is often observed in clients who are emotionally sensitive and/or react excessively to a variety of stimuli. Note that some people have learned not to show their reactivity on their face or in the overt behaviors, yet they continue to breathe shallowly as a telltale sign of ‘distress.’ People who breath shallowly may experience this response as burdensome. Discuss with them how to reframe their sensitivity as a gift; namely, they are more aware of other people’s reactions and emotions. They just need to learn how not to respond automatically. Encourage awareness of their breath-holding and shallow breathing. Follow this by teaching them to replace the dysfunctional breathing with slow, diaphragmatic breathing at 6-breaths-per-minute. A possible training sequence is the following:
- Teach slow, diaphragmatic breathing
- Practice evoking a stressor and the moment the client senses the stress response, shallow breaths or holds their breath have them shift to slow, diaphragmatic breathing.
- If the person slouches in response to stress, the moment they become aware of slouching, have then sit erect, look up and then breathe diaphragmatically. (Peper et al., 2019)
Experiential practice: Transform stressful thoughts by looking up, breathing, and changing thoughts.
Evoke a stressor and then attempt to reframe the experience (cognitive behavior therapy or CBT approach).
Compare this to evoking a stressor, then shift to an upright position while looking up, take a few slow, diaphragmatic breaths, and reframe the experience.
In almost all cases, when the client shifts position, looks up and then reframes, the stress reaction is significantly reduced and it is much easier to reframe the experiences positively compared to when only attempting to reframe the experience (Peper et al., 2019).
Diaphragmatic breathing feels abnormal. How you breathe habitually is what feels normal unless there is overt illness such as asthma or emphysema. Any new pattern usually feels abnormal. When the person shifts their breathing pattern, such as in a transition from habitual shallow chest breathing to slower diaphragmatic abdominal breathing, it feels strange and wrong.
Suggested solutions and recommendations. Discuss the concept that habitual patterns are normal (e.g., a person who typically slouches when standing straight may experience that they are going to fall backwards). Emphasize the importance of making a shift in posture and leaning into the discomfort of the new experience. Often after practicing slow diaphragmatic breathing, the person may report feeling much more relaxed (e.g., sensing heaviness and warmth) with their fingers increasing in temperature.
2. Challenges that may occur when learning diaphragmatic breathing
Ideally, breathing is an effortless diaphragmatic process as described by the phrase, “it breathes me” (Luthe & Schultz, 1970; Luthe, 1979); however, some participants struggle to achieve this type of breathing. The following are common challenges and possible solutions:
Distraction and internal dialogue. Many people struggle with thoughts jumping from one area to another. Some people refer to this mental state as “monkey mind.”
Suggested solutions and recommendations. Validate that distraction and internal dialogue are normal and require continual managing and practice to overcome. Experimental Practice: Have the person train focus during diaphragmatic breathing techniques by focusing on 1 item in the room. Remind them that when thoughts arise, note them briefly instead of engaging with them and then refocus on the item. Start with increments of time and increase with practice.
Effect of gravity on breathing. In the vertical position, exhalation occurs when the abdomen constricts (slight tightening of the transverse and oblique abdominal muscles and the pelvic floor) pushes the diaphragm up, allowing the air to go out. It needs to push against gravity.
In the vertical position, inhalation occurs when the abdominal muscles and pelvic floor muscles relax and the abdomen widens in all directions (360 degrees) which causes the diaphragm to descend as it is being pulled down by gravity. This process allows effortless inhalation. The experience is the opposite when lying supine on one’s back. While lying down, gravity pulls on the abdomen that cause the diaphragm to go upward allowing the air to flow out during exhalation. Inhalation takes work because as the diaphragm descends it has to push the abdominal content upward against gravity.
Experiential practice: Erect versus supine
- Vertical position. Begin by exhaling completely by pulling the abdomen in and up while staying erect and not pressing/contracting the chest downward. At the end of exhalation, allow the abdomen to relax (pop out) and feel how the air is sucked in without trying to inhale
- Horizontal position. Begin by lying down, with the face pointing up. Inhale by expanding your abdomen and pushing your abdomen upward against gravity. Then let exhalation occur while totally relaxing as gravity pushes the abdomen downward, which pushes the diaphragm upward into the chest allowing the air to flow out. Optionally, place a small bag of rice/beans (e.g., approximately one to five pound or. One-half to two kilograms) on your lower abdomen while lying down. When you inhale, push the weight upward and away from you by allowing the stomach, but not the chest, to expand. Allow exhalation to occur as the weight pushes your abdomen down and upward into your chest. The weight is useful as it allows the mind to focus more easily on the task of feeling the movement of the abdomen.
Over breathing/hyperventilation. Even breathing at about six breaths per minute can cause hyperventilation can occur. Hyperventilation occurs when a person is breathing in excess of the metabolic needs of the body and thereby eliminating more carbon dioxide. The result is respiratory alkalosis and an elevated blood pH as the dissolved carbon dioxide (pCO2) in the blood is reduced (Folgering, 1999).
The most common symptoms of over breathing are colder sweaty hands and light-headedness. If this starts to occur, focus on decreasing the airflow during exhalation by exhaling through pursed lips making the sound, “Pssssssst.” While making this sound, make the sound softer with less airflow. Alternatively, have them imagine a holding a dandelion flower a few inches from their lips and blow so softly the seeds do not blow away. The blowing away of the seed is the feedback that you are blowing to hard as shown in Figure 2.

Figure 2. Dandelion seeds as feedback when the person is blowing with too much effort. Alternatively, we recommend that the client imagine smelling the scent/fragrance of a flower that usually causes nose inhalation and then exhale gently through pursed lips ast if the air flows over a candle and, the flame does not move back and forth.
Mouth breathing. Mouth breathing contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded miss-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. Nose breathing reduces airway irritation since the nose filters, humidifies, warms/cools the inhaled air as well as reduces the air turbulence in the upper airways. The epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation (McKeown, 2019; Allen, 2024). Note that alternate nostril breathing, such as breathing in one nostril for 5-seconds and out of the other for 5-seconds is another technique which some people find beneficial.
Slower breathing approaches also facilitates sympathetic parasympathetic balance and reduces airway irritation. If the person breathes habitually through their mouth, refer them to health care provider to explore factors that may contribute to mouth breathing such as enlarged tonsils and adenoids or deviated septum. In addition, explore environmental factors that could contribute nasal inflammation such as allergies or foods such as dairy (Al-Raby, 2016).
Performance anxiety. Many participants are concerned about their performance. The direct instructions such as “follow the graphic” causes the person to try hard to breathe with too much effort. Explore some of the following indirect strategies to interrupt ongoing cognitive judgements and self-talk.
- Toning or humming (Peper et al., 2019a). While exhaling, have the person hum a sound with their mouth closed. Let the sound go for about 6 seconds, relax, inhale and hum again. Toning is very similar except you verbalize a tone such as “Oammm.” (For detailed instructions on toning, see: Anziani & Peper (2021)).
- Stroking down arms and legs during exhalation. Have a partner gently stroke down your arms from your shoulder past your fingertips as you are exhaling. The downward stroking is in rhythm with the exhalation. As the arm is being stroked, attend to the sensations going down the arms. Be sure that the toucher exhales at the same time and the stroking down the arm takes about six seconds. After being stroked for a few times, have the person imagine that each time they exhale they feel a flow down through their arms and out their fingers.
- Repeat the same process while stroking down the legs from the side of their hips to their toes.
- Finally, have the person imagine/feel the sensation streaming down their legs with each exhalation.
- Many participants will report that they sense a steaming going down their arms, that they hands warm up, and their thought have stopped.
- Integrated body movement with breathing especially flexion and contraction (Meehan & Shaffer, 2023). Integrate the normal response of flexion that induces exhalation and extension evokes inhalation. Be careful that the flexion movement does not encourage participants to compress their chest during exhalation, which tends to encourage chest breathing. Have the person focus on their head staying tall and erect. Have the person sit straight up with their feet slight apart and their hands palm down on their lap. Allow inhaling to initiate as the person simultaneously arches their lower back expanding the stomach, separating the knees and turning the hands palm up. Initiate exhalation while simultaneously bringing the knees together, turning the palms face down on the thighs and rolling the pelvic back slightly rounding the lower back. Do the movements smoothly while keeping the legs and shoulders relaxed.
Flooded by emotions. Although very rare, at times when the person allows the abdomen to relax, they may experience by the emotions from a past trauma as the habitual bracing patterns are relaxed.
Suggested solutions and recommendations. Validate these emotions for the person. Explain that this is a normal process that may occur if past trauma has occurred. Clients who have had past trauma often experience hypervigilance, which may interfere with the relaxation response that occurs during more optimal states of breathing. Transitioning to a more optimal rest state may be uncomfortable for a person who has experienced trauma because it reduces hypervigilance. This can feel uncomfortable as hypervigilance in these cases serves a protective role, even if it is an illusory feeling of protection from future harm. Since persistent hypervigilance can interfere with the relaxation response, the benefits of allowing a relaxation response to occur through slower breathing should be highlighted. Grounding techniques as described by Peper et al (2024a) can be useful to become centered.
3. Strategies to generalize the effortless breathing into daily life.
Generalizing the skill occurs after having mastered diaphragmatic breathing in different positions (sitting, standing, lying down, and while performing tasks). It is important to remember that our breathing patterns are conditioned with our behavior. Become aware how breathing affects cognitions and emotions and how emotions and cognitions affects breathing. The following are some strategies that may facilitate learning and generalizing the slower breathing skills.
Observing how our behavior affects our breathing: Anything that may evoke the alarm or defense reaction tends to cause the person gasp and/or hold their breath. For example, when a person is sitting peacefully, make an unexpected noise behind their back or movement in their periphery of vision. In most cases they will gasp or hold their breath. Usually, they are unaware of this process unless they are asked what happened to their breathing. The major reason for the breath holding is that the stimuli triggers an alarm/defense reaction and when we hold our breath our hearing is more acute (we can hear approaching danger earlier). The problem is that we give this response when there is no actual, immediate or present threat.
Experiential practice. Sit comfortably. Now as quickly as possible without rotating the head, look with your eyes to the extreme right and then left and back and forth as if trying to identify danger at the periphery. Do this for a few eye movements. Almost everyone holds their breath when doing this exercise. For generalizing the skill, ask the person to observe during the day situations in which they hold their breath, ask them if it was necessary and encourage them to start diaphragmatic breathing.
Observing how breathing affects our thoughts and emotions. Breathing patterns are intrinsically linked to our emotions and thoughts as illustrated in the many language phrases such as sigh of relief, full of hot air, waiting with bated breath. At the same time, our breathing patterns also affect our thoughts. For instance, when we breathe shallowly and more rapidly, we can induce feelings of fear or anxiety. If we gasp, we can experience thought stopping.
Experiential practices: Incomplete exhalation: Observe what happens when you exhale less than you inhale. Begin by exhaling only 70% of the air you inhaled, then inhale and exhale again only 70% of the air you just inhaled continue this for 30 seconds. Many people will experience the onset of anxiety symptoms, lightheadedness, dizziness, neck and shoulder tension, etc. (Peper & MacHose, 1993). If you experience symptoms during this exercise and you have experienced these symptoms in the past, it is likely that unknowingly breathing in a dysfunctional pattern could have evoked them. Therefore, practicing effortless breathing may interrupt and reduce the symptoms. Do this practice while observing the person carefully and immediately interrupt and distract the person if they start feeling dizzy, too anxious, or trigger the beginning of a panic attack or PTSD symptoms.
Experiential practice: Gasp or sniff-hold sniff. Observe what happens when you are performing a cognitive task and you rapidly gasp or do sniff-hold-sniff again before exhaling. Begin by sequentially subtracting mentally, the number 7 from 146 (e.g., 146, 139, 132….). Do this as rapidly as possible and do not make a mistake. While doing the subtracting, take a rapid gasp (such as one is triggered by surprise or fear), alternatively, take a quick sniff through your nose, hold your breath and take another sniff on top of the first one, then exhale. Whereas subtrating numbers is a skill most adults can perform, the ‘time pressure’ along with the direction to avoid mistakes may be the ‘immediate’ source of strain. Whether it was the time pressure, the direction to avoid mistakes or the direction to gasp, observe what happened to your thinking process. In almost all cases, your higher-order thoughts (doing the sequential subtraction under time pressure while gasping) have disappeared, replaced by the immediate thoughts of ‘performance anxiety.’
If you blank out on exams or experience anxiety, gasping and breath holding may be one of the factors that increases symptoms and affects your performance. If you are aware that you are holding your breath or gasped, use that as the cue to shift to slow diaphragmatic breathing and you may find that your performance improves. Therefore, observe when and where you were blanking out, gasping and/or holding your breathing then substitute slow, effortless diaphragmatic breathing.
How to develop awareness and interrupting of dysfunctional breathing response. Most participants are unaware of their somatic responses until symptoms occur. Being aware of the initiation of a somatic response may assist you in identifying triggers and interrupting the developing process. A significant component of the training is symptom prescription rehearsal.
Symptom prescription is a practice in which the participant simulates/acts out the psychophysiological pattern associated with their symptoms. They amplify the body pattern until they feel the onset of the actual symptoms. The moment the person feels the beginning of the symptom, they stop the practice and initiate slow breathing and relaxation. After practicing the symptom rehearsal, they are instructed to become aware of the onset of the symptom and then use that signal to trigger the effortless breathing while looking up and shifting the body into an upright sitting position (Peper et al., 2019). Gasping and breath holding are normal responses to unexpected stimuli; however, they may trigger sympathetic activation even when there is no actual danger.
Experiential practice: Developing awareness on neck and shoulder tension:
Sit comfortably and practice effortless breathing for a minute. Take a fearful gasp and observe what happens in your body (e.g., slight neck and upper chest tension, light headedness, slight radiating pain into the eye, etc.). Shift back to effortless breathing until all symptoms /sensations have disappeared.
- Now gasp with less effort and observe the first sensations, use the awareness of first sensations to trigger the effortless breathing and continue to breathe until symptoms have disappeared
- Continue this practice. Reduce the gasping effort each time.
- After having developed the initial somatic sensation then during the day observe what triggers this response and immediately shift to slower diaphragmatic breathing. After you have shifted to effortless breathing, reflect on the trigger. Was it necessary to react? If yes, explore strategies to resolve the issue.
The same process can be done to assist with desensitization to painful memories or stressful events. Each time the person becomes aware of their somatic reaction to an evoked memory or stressful event, they shift to effortless diaphragmatic breathing. If they find that it is difficult to interrupt the emotional memories and it triggers more and more negative thoughts and associations, use the sniff-hold-sniff technique and follow that with box-breathing or any of the other quick somatic rescue techniques (Peper et al., 2024a). Box-breathing in this context could include a brief breath-holding. A typical box-breathing technique is to breath in for a count of four, hold for a count of four, breath out for a count of four, then breath in again for a count of four, continuing the figurative 4-4-4-4 count of breathing.
Practice slower diaphragmatic breathing during the day. Implement effortless diaphragmatic breathing through regeneration and interrupting the stress response.
- Support regeneration. Each day set aside 10 to 20 minutes to practice slow effortless diaphragmatic breathing at about 6-breaths-per-minute. In the beginning 10 to 20 minutes may be too long, thus in some cases have the person practice a few times a day for two minutes and slowly build up to 10 or more minutes. The practice is not just a mechanical process of breathing it includes mindfulness training. Namely, as you are breathing each time you exhale imagine a flow doing down your arms and legs and as you inhale an energy coming into you. Whenever your attention drifts bring it back to the breathing.
- Integrate breathing with daily activities. Practice slower breather before eating, after putting the seat belt on in the car, or whenever a notification pops up on the cell phone.
- Set reminders and alarms on your phone to check how you are feeling and breathing. Leave notes on nearby furniture such as a nightstand, on the shower door, and/or on the kitchen table as reminders to be mindful of your breath. If stressed or breathing shallowly, take a moment to breathe slowly.
- Interrupt the stress response. During the day when you are aware that you shallow breathe, are holding your breath, feel anxious, experience neck and shoulder tightness, or worry and use that as a cue to shift position by sitting or standing more erect, looking upward and take a few slow diaphragmatic breaths.
- Use cue condition to facilitate this process. Each time you begin the practice smell a specific aroma or do some behavioral movement and then do the breathing. After a while the aroma or behavioral movement will become the classically conditioned cue to trigger the effortless breathing.
- Use role rehearsal and conditioning to generalize the skill. Generalizing the skills often takes more time than what may be expected. In a culture where instant relief is expected— implied message associated with medication— self-mastery techniques are different and challenging as they take time to master the skill and implement them during daily life. The process of mastery is similar to learning to play a musical instrument or sports. Learning to play the violin requires practice as well as practice with failures along the way until one is ready for more challenging musical pieces, recitals, or performances.
A useful strategy to implement the learning is role rehearsal in the office, at home at work, and in real life. It is usually much easier to practice these skills in a safe space such as your own room or, with a therapist compared to with other people or, at work. To generalize the skill most efficiently, it can be helpful to practice in a safe environment while imagining being in the actual stressful location This process is illustrated by the strategy to reduce social anxiety and menstrual cramps.
Social anxiety when seeing my supervisor. Master effortless breathing in a safe environment. Role rehearsal in imagery. If you observed that you held your breath when your supervisor is around, begin with imagery when your supervisor is not present. Sit, comfortably. Let go of muscle tension and breathe effortlessly, evoking a scenario where your supervisor is walking by and continue to breathe slowly as you imagine the scene. Role rehearsal in action. Ask another person to role-play your supervisor. Sit, comfortably. Let go of muscle tension and breathe effortlessly. Have this person walk into the room in a similar way that your supervisor would. Imagine that person is your supervisor while practicing your effortless breathing. Repeat until the effortless breathing is more automatic. Practice many times in real life. Whenever the rehearsed situation occurs, implement slower paced breathing.
Menstrual cramps that causes most women to curl up and breathe shallowly when experiencing menstrual cramps (Peper et al., 2023). Master effortless breathing in a safe environment. Practice breathing lying down. While lying down, breathe diaphragmatically by having a three-to-five-pound weight such as a bag of rice or hot water pad on your abdomen. If you have a partner, have the person stroke your legs from the abdomen to your toes while you exhale. Role rehearse experiencing pain and then practice lower diaphragmatic breathing. Namely, tighten your abdomen as if you have discomfort, then focus on relaxing the buttocks and sensing the air flowing down your legs and out your feet as you exhale. Practice in real life. A few days before you expected menstruation, practice slow diaphragmatic breathing several times for at least 5-10 minutes during the day. When your menstruation starts practice the slower and lower breathing while imagining the air flowing down the abdomen, through the legs and out the feet.
Summary/Conclusion
Breathing is the mind-body bridge. It usually occurs without awareness and breathing changes affect our thought, emotions and body. Mastering and implementing slower breathing during the day takes time and practice. By observing when breathing patterns change, participants may identify internal and external factors that affect breathing which provides an opportunity to implement effortless diaphragmatic breathing to optimize health as well as resolve some of the triggers. As one 20-year-old, female student reported,
The biggest benefit from learning diaphragmatic breathing was that it gave me the feeling of safety in many moments. My anxiety tended to make me feel unsafe in many situations but homing in and mastering diaphragmatic breathing helped tremendously. I shifted from constant chest breathing to acknowledging it and in turn, reminding myself to breathe with my diaphragm.
References
Allen, R. (2024). The health benefits of nose breathing. Nursing in General Practice. http://hdl.handle.net/10147/559021
Al-Rabia, M.W. (2016). Food-induced immunoglobulin E-mediated allergic rhinitis. J Microsc Ultrastruct, 4(2), 69-75. https://doi.org/doi.org/10.1016/j.jmau.2015.11.004
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. Peperperspective –ideas on illness, health and well-being from Erik Peper. Accessed April 16, 2024. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Banushi, B., Brendle, M., Ragnhildstveit, A., Murphy, T., Moore, C., Egberts, J., & Robison, R. (2023). Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sci. 13(2), 256. https://doi.org/10.3390/brainsci13020256
Chung, A.H., Gevirtz, R.N., Gharbo, R.S. et al. (2021).Pilot Study on Reducing Symptoms of Anxiety with a Heart Rate Variability Biofeedback Wearable and Remote Stress Management Coach. Appl Psychophysiol Biofeedback 46, 347–358. https://doi.org/10.1007/s10484-021-09519-x
Cohen, D. & Leung, A.K.Y. (2009). The hard embodiment of culture. European Journal of Social Psychology, 9, 1278–1289 https://doi.org/10.1002/ejsp.671
Codrons, E., Bernardi, N. F., Vandoni, M., & Bernardi, L. (2014). Spontaneous group synchronization of movements and respiratory rhythms. PloS one, 9(9), e107538. https://doi.org/10.1371/journal.pone.0107538
Dick, T. E., Mims, J. R., Hsieh, Y. H., Morris, K. F., & Wehrwein, E. A. (2014). Increased cardio-respiratory coupling evoked by slow deep breathing can persist in normal humans. Respiratory physiology & neurobiology, 204, 99-111. https://doil.org/10.1016/j.resp.2014.09.013
Ekerholt, K. & Bergland, A. (2008). Breathing: A sign of life and a unique area for reflection and action. Physical therapy, 88(7), 832-840. https://doi.org/10.2522/ptj.20070316
Elstad, M., O’Callaghan, E. L., Smith, A. J., Ben-Tal, A., & Ramchandra, R. (2018). Cardiorespiratory interactions in humans and animals: rhythms for life. American Journal of Physiology-Heart and Circulatory Physiology, 315(1), H6-H17. https://doi.org/10.1152/ajpheart.00701.2017
Folgering, H. (1999). The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis, 54(4), 365-72. https://pubmed.ncbi.nlm.nih.gov/10546483/
Gilbert, C. (1998). Emotional sources of dysfunctional breathing. Journal of bodywork and movement therapies, 2(4), 224-23. https://doi.org/10.1016/S1360-8592(98)80019-3
Jerath, R., Beveridge, C., & Barnes, V.A. (2019). Self-Regulation of Breathing as an Adjunctive Treatment of Insomnia. Front Psychiatry, 9(780). https://doi.org/10.3389/fpsyt.2018.00780
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Kang, K.W., Jung, S.I., Lee, do Y., Kim, K., & Lee, N.K. (2016) Effect of sitting posture on respiratory function while using a smartphone. J Phys Ther Sci, 28(5), 1496-8. https://doi.org/10.1589/jpts.28.1496
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol. 5, 756. https://doi.org/10.3389/fpsyg.2014.00756
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
MacHose, M., & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Magnon. V., Dutheil, F., & Vallet, G.T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 11(1),19267. https://doi.org/10.1038/s41598-021-98736-9
Maric, V., Ramanathan, D., & Mishra, J. (2020). Respiratory regulation & interactions with neuro-cognitive circuitry. Neuroscience & Biobehavioral Reviews, 112, 95-106. https://doi.org/10.1016/j.neubiorev.2020.02.001
Matić, Z., Platiša, M. M., Kalauzi, A., & Bojić, T. (2020). Slow 0.1 Hz breathing and body posture induced perturbations of RRI and respiratory signal complexity and cardiorespiratory coupling. Frontiers in physiology, 11, 24. https://doi.org/10.3389/fphys.2020.00024
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Meehan, Z.M. & Shaffer, F. (2023). Adding Core Muscle Contraction to Wrist-Ankle Rhythmical Skeletal Muscle Tension Increases Respiratory Sinus Arrhythmia and Low-Frequency Power. Appl Psychophysiol Biofeedback. 48(1), 127-134. https://doi.org/10.1007/s10484-022-09568-w
McKeown, P. (2021). The breathing cure: Develop new habits for a healthier, happier, and longer life. Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E. & Cohen, T. (2017). Inhale to Breathe Away Pelvic Floor Pain and Enjoy Intercourse. Biofeedback, 45 (1), 21–24. https://doi.org/10.5298/1081-5937-45.1.04
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. https://doi.org/10.15540/nr.6.3.153
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07 or https://www.researchgate.net/publication/383151816_WHAT_ABOUT_THIS_Increase_Attention_Concentration_and_School_Performance_with_Posture_Feedback
Peper, E. & MacHose, M. (1993). Symptom prescription: Inducing anxiety by 70% exhalation. Applied Psychophysiology and Biofeedback, 18(3), 133-138. https://doi.org/10.1007/BF00999790
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. 45(4), 83–87. https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019a). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128-133. https://doi.org/10.15540/nr.6.3.12
Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512
PTI. (2023 August 3). Often suck your stomach in to look slimmer in pictures? It can lead to ‘hourglass syndrome.’ The Economic Times Panache. Accessed March 26, 2024. https://economictimes.indiatimes.com/magazines/panache/often-suck-your-stomach-in-to-look-slimmer-in-pictures-it-can-lead-to-hourglass-syndrome/articleshow/102392681.cms?from=mdr
Salah, H.M., Goldberg, L.R., Molinger, J., Felker, G.M., Applefeld, W., Rassaf, T., Tedford, R.J., Mirro, M., Cleland, J.GF., & Fudim, M. (2022). Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week, Journal of the American College of Cardiology, 80(17), 1647-1659. https://doi.org/10.1016/j.jacc.2022.08.760
Shaffer, F. & Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience,14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
Taub, E., Uswatte, G., Mark, V. W., Morris, D. M. (2006). The learned nonuse phenomenon: Implications for rehabilitation. Europa Medicophysica, 42(3), 241-256. https://pubmed.ncbi.nlm.nih.gov/17039223/
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Xiao, M., Zi-Qi, Y., Gong, Z.Q., Zhang, H., Duan, N.Y., Shi, Y.T,, Wei, G.X., Li, Y.F. (2017).The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front Psychol. 8(874). https://doi.org/10.3389/fpsyg.2017.00874
Cellphones affects social communication, vision, breathing, and health: What to do!
Posted: September 4, 2024 Filed under: ADHD, attention, behavior, Breathing/respiration, cellphone, computer, digital devices, educationj, ergonomics, health, laptops, Neck and shoulder discomfort, posture, screen fatigue, self-healing, stress management, techstress, Uncategorized, vision, zoom fatigue | Tags: communication, myopia, pedestrian deaths, peripheral vision, text neck 7 CommentsAdapted from: Peper, E. & Harvey, R. (2024). Cell phones affects social communication, vision, breathing, and mental and physical health: What to do! TownsendLetter-The Examiner of Alternative Medicine,September 15, 2024. https://townsendletter.com/smartphone-affects-social-communication-vision-breathing-and-mental-and-physical-health-what-to-do/

Abstract
Smartphones are an indispensable part of our lives. Unfortunately too much of a ‘good thing’ regarding technology can work against us, leading to overuse, which in turn influences physical, mental and emotional development among current ‘Generation Z’ and ‘Millennial’ users (e.g., born 1997-2012, and 1981-1996, respectively). Compared to older technology users, Generation Z report more mental and physical health problems. Categories of mental health include attentional deficits, feelings of depression, anxiety social isolation and even suicidal thoughts, as along with physical health complaints such as sore neck and shoulders, eyestrain and increase in myopia. Long duration of looking downward at a smartphone affects not only eyestrain and posture but it also affects breathing which burden overall health. The article provides evidence and practices so show how technology over use and slouching posture may cause a decrease in social interactions and increases in emotional/mental and physical health symptoms such as eyestrain, myopia, and body aches and pains. Suggestions and strategies are provided for reversing the deleterious effects of slouched posture and shallow breathing to promote health.
We are part of an uncontrolled social experiment
We, as technology users, are all part of a social experiment in which companies examine which technologies and content increase profits for their investors (Mason, Zamparo, Marini, & Ameen, 2022). Unlike University research investigations which have a duty to warn of risks associated with their projects, we as participants in ‘profit-focused’ experiments are seldom fully and transparently informed of the physical, behavioral and psychological risks (Abbasi, Jagaveeran, Goh, & Tariq, 2021; Bhargava, & Velasquez, 2021). During university research participants must be told in plain language about the risks associated with the project (Huh-Yoo & Rader, 2020; Resnik, 2021). In contrast for-profit technology companies make it possible to hurriedly ‘click through’ terms-of-service and end-user-license-agreements, ‘giving away’ our rights to privacy, then selling our information to the highest bidder (Crain, 2021; Fainmesser, Galeotti, & Momot, 2023; Quach et al., 2022; Yang, 2022).
Although some people remain ignorant and or indifferent (e.g., “I don’t know and I don’t care”) about the use of our ‘data,’ an unintended consequence of becoming ‘dependent’ on technology overuse includes the strain on our mental and physical health (Abusamak, Jaber & Alrawashdeh, 2022; Padney et al., 2020). We have adapted new technologies and patterns of information input without asking the extent to which there were negative side effects (Akulwar-Tajane, Parmar, Naik & Shah, 2020; Elsayed, 2021). As modern employment shifted from predominantly blue-collar physical labor to white collar information processing jobs, people began sitting more throughout the day. Workers tended to look down to read and type. ‘Immobilized’ sitting for hours of time has increased as people spend time working on a computer/laptop and looking down at smartphones (Park, Kim & Lee, 2020). The average person now sits in a mostly immobilized posture 10.4 hours/day and modern adolescents spent more than two thirds of their waking time sitting and often looking down at their smartphones (Blodgett, et al., 2024; Arundell et al., 2019).
Smartphones are an indispensable part of our lives and is changing the physical and mental emotional development especially of Generation Z who were born between 1997-2012 (Haidt, 2024). They are the social media and smartphone natives (Childers & Boatwright, 2021). The smartphone is their personal computer and the gateway to communication including texting, searching, video chats, social media (Hernandez-de-Menendez, Escobar Díaz, & Morales-Menendez, 2020; Nichols, 2020; Schenarts, 2020; Szymkowiak et al., 2021). It has 100,000 times the processing power of the computer used to land the first astronauts on the moon on July 20, 1969 according to University of Nottingham’s computer scientist Graham Kendal (Dockrill, 2020). More than one half of US teens spend on the average more than 7 hours on daily screen time that includes watching streaming videos, gaming, social media and texting and their attention span has decreased from 150 seconds in 2004 to an average of 44 seconds in 2021 (Duarte, F., 2023; Mark, 2022, p. 96).
For Generation Z, social media use is done predominantly with smartphones while looking down. It has increased mental health problems such as attentional deficits, depression, anxiety suicidal thoughts, social isolation as well as decreased physical health (Haidt, 2024; Braghieri et al., 2023; Orsolini, Longo & Volpe, 2023; Satılmış, Cengız, & Güngörmüş, 2023; Muchacka-Cymerman, 2022; Fiebert, Kistner, Gissendanner & DaSilva, 2021; Mohan et al., 2021; Goodwin et al., 2020).
The shift in communication from synchronous (face-to-face) to asynchronous (texting) has transformed communications and mental health as it allows communication while being insulated from the other’s reactions (Lewis, 2024). The digital connection instead of face-to-face connection by looking down at the smart phone also has decreased the opportunity connect with other people and create new social connections, with three typical hypotheses examining the extent to which digital technologies (a) displace/ replace; (b) compete/ interfere with; and/or, (c) complement/ enhance in-person activities and relationships (Kushlev & Leitao, 2020).
As described in detail by Jonathan Haidt (2024), in his book, The Anxious Generation, the smartphone and the addictive nature of social media combined with the reduction in exercise, unsupervised play and childhood independence was been identified as the major factors in the decrease in mental health in your people (Gupta, 2023). This article focuses less on distraction such as attentional deficits, or dependency leading to tolerance, withdrawal and cravings (e.g., addiction-like symptoms) and focuses more on ‘dysregulation’ of body awareness (posture and breathing changes) and social communication while people are engaged with technology (Nawaz,Bhowmik, Linden & Mitchell, 2024).
The excessive use of the smartphones is associated with a significant reduction of physical activity and movement leading to a so-called sedentarism or increases of sitting disease (Chandrasekaran & Ganesan, 2021; Nakshine, Thute, Khatib, & Sarkar, 2022). Unbeknown to the smartphone users their posture changes, as they looks down at their screen, may also affect their mental and physical health (Aliberti, Invernizzi, Scurati & D’lsanto, 2020).
(1) Explore how looking at your smartphone affects you (adapted from: Peper, Harvey, & Rosegard, 2024)
For a minute, sit in your normal slouched position and look at your smartphone while intensely reading the text or searching social media. For the next minute sit tall and bring the cell phone in front of you so you can look straight ahead at it. Again, look at your smartphone while intensely reading the text or searching social media.
Compare how the posture affects you. Most likely, your experience is similar to the findings from students in a classroom observational study. Almost all experienced a reduction in peripheral awareness and breathed more shallowly when they slouched while looking at their cellphone.
Decreased peripheral awareness and increased shallow breathing that affects physical and mental health and performance. The students reported looking down position reduces the opportunity of creating new social connections. Looking down my also increases the risk for depression along with reduced cognitive performance during class (Peper et al., 2017; Peper et al., 2018).
(2) Explore how posture affects eye contact (adapted from the exercise shared by Ronald Swatzyna, 2023)[2]
Walk around your neighborhood or through campus either looking downwards or straight ahead for 30 minutes while counting the number of eye contacts you make.
Most likely, when looking straight ahead and around versus slouched and looking down you had the same experience as Ronald Swatzyna (2023), Licensed Clinical Social Worker. He observed that when he walked a three-mile loop around the park in a poor posture with shoulders forward in a head down position, and then reversed direction and walked in good posture with the shoulders back and the head level, he would make about five times as many eye contacts with a good posture compared to the poor posture.
Anecdotal observations, often repeated by many educators, suggest before the omnipresent smartphone, students would look around and talk to each other before a university class began. Now, when Generation Z students enter an in-person class, they sit down, look down at their phone and tend not to interact with other students.
(3) Experience the effect of face-to-face in-person communication
During the first class meeting, ask students to put their cellphones away, meet with three or four other students for a few minutes, and share a positive experience that happened to them last week as well as what they would like to learn in the class. After a few minutes, ask them to report how their energy and mood changed.
In our observational class study with 24 junior and senior college students in the in-person class and 54 students in the online zoom class, almost all report that that their energy and positive mood increased after they interacted with each other. The effects were more beneficial for the in-person small group sharing than the online breakout groups sharing on Zoom as shown in Figure 1.

Figure 1. Change in subjective energy and mood after sharing experiences synchronously in small groups either in-person or online.
Without direction of a guided exercise to increase social connections, students tend to stay within their ‘smartphone bubble’ while looking down (Bochicchio et al., 2022). As a result, they appear to be more challenged to meet and interact with other people face-to-face or by phone as is reflected in the survey data that Generation Z is dating much less and more lonely than the previous generations (Cox et al., 2023).
What to do:
- Put the smartphone away so that you do not see it in social settings such as during meals or classes. This means that other people can be present with you and the activity of eating or learning.
- Do not permit smartphones in the classroom including universities unless it is required for a class assignment.
- In classrooms and in the corporate world, create activities that demands face-to-face synchronous communication.
- Unplug from the audio programs when walking and explore with your eyes what is going on around you.
(4) Looking down increases risk of injury and death
Looking down at a close screen reduces peripheral awareness and there by increases the risk of accidents and pedestrian deaths. Pedestrian deaths are up 69% since 2011 (Cova, 2024) and have consistently increased since the introduction of the iPhone in 2007 as shown in Figure 3.

Figure 3. Increase in pedestrian death since the introduction of the iphone (data plotted from https://www.iihs.org/topics/fatality-statistics/detail/pedestrians)
In addition, the increase use of mobile phones is also associated with hand and wrist pain from overuse and with serious injuries such as falls and texting while driving due to lack of peripheral awareness. McLaughlin et al (2023) reports an increase in hand and wrist injuries as well serious injuries related to distracted behaviors, such as falls and texting while driving. The highest phone related injuries (lacerations) as reported from the 2011 to 2020 emergency room visits were people in the age range from 11–20 years followed by 21–30 years.
What to do:
- Do not walk while looking at your smartphone. Attend to the environment around you.
- Unplug from the audio podcasts when walking and explore with your eyes what is going on around you.
- Sit or stop walking when answering the smartphone to reduce the probability of an accident.
- For more pragmatic suggestions, see the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics, by Peper, Harvey and Faass (2020).
(5) Looking at screens increases the risk of myopia
Looking at a near screen for long periods of time increases the risk of myopia (near sightedness) which means that distant vision is more blurry. Myopia has increased as children predominantly use computers or, smartphones with smaller screen at shorter distances. By predominantly focusing on nearby screens without allowing the eye to relax remodels the eyes structure. Consequently, myopia has increase in the U.S. from 25 percent in the early 1970s to nearly 42 percent three decades later (OHSU, 2022).
Looking only at nearby screens, our eyes converge and the ciliary muscles around the lens contract and remain contracted until the person looks at the far distance. The less opportunity there is to allow the eyes to look at distant vision, the more myopia occurs. in Singapore 80 per cent of young people aged 18 or below have nearsightedness and 20 % of the young people have high myopia as compared to 10 years ago (Singapore National Eye Centre, 2024). The increase in myopia is a significant concern since high myopia is associated with an increased risk of vision loss due to cataract, glaucoma, and myopic macular degeneration (MMD). MMD is rapidly increasing and one of the leading causes of blindness in East Asia that has one of the highest myopia rates in the world (Sankaridurg et al., 2021).
What to do:
- Every 20 minutes stop looking at the screen and look at the far distance to relax the eyes for 20 seconds.
- Do not allow young children access to cellphones or screens. Let them explore and play in nature where they naturally alternate looking at far and near objects.
- Implement the guided eye regenerating practices descrubed in the article, Resolve eyestrain and screen fatigue, by Peper (2021).
- Read Meir Schneider’s (2016) book, Vision for Life, for suggestions how to maintain and improve vision.
(6) Looking down increases tech neck discomfort
Looking down at the phone while standing or sitting strains the neck and shoulder muscles because of the prolonged forward head posture as illustrated in the YouTube video, Tech Stress Symptoms and Causes (DeWitt, 2018). Using a smartphone while standing or walking causes a significant increase in thoracic kyphosis and trunk (Betsch et al., 2021). When the head is erect, the muscle of the neck balance a weight of about 10 to 12 pounds or, approximately 5 kilograms; however, when the head is forward at 60 degrees looking at your cell phone the forces on the muscles are about 60 pound or more than 25 kilograms, as illustrated in Figure 4 (Hansraj, 2014).

Figure 4. The head forward position puts as much as sixty pounds of pressure on the neck muscles and spine (by permission from Dr. Kenneth Hansraj, 2014).
This process is graphically illustrated in the YouTube video, Text Neck Symptoms and Causes Video, produced by Veritas Health (2020).
What to do:
- Keep the phone in front of you so that you do not slouch down by having your elbow support on the table.
- Every ten minutes stretch, look up and roll your shoulders backwards.
- Wear a posture feedback device such as the UpRight Go 2 to remind you when you slouch to change posture and activity (Peper et al., 2019; Stuart, Godfrey & Mancini, 2022).
- Take Alexander Technique lessons to improve your posture (Cacciatore, Johnson, & Cohen, 2020; AmAT, 2024; STAT, 2024).
(7) Looking down increases negative memory recall and depression
In our previous research, Peper et al. (2017) have found that recalling hopeless, helpless, powerless, and defeated memories is easier when sitting in a slouched position than in an upright position. Recalling positive memories is much easier when sitting upright and looking slightly upward than sitting slouched position. If attempting to recall positive memories the brain has to work hard as indicated by an significantly higher amplitudes of beta2, beta3, and beta4 EEG (i.e., electroencephalograph) when sitting slouched then when sitting upright (Tsai et al., 2016).
Not only does the postural position affect memory recall, it also affects mental math under time-pressure performance. When students sit in a slouched position, they report that is much more difficult to do mental math (serial 7ths) than when in the upright position (Peper et al., 2018). The effect of posture is most powerful for the 70% of students who reported that they blanked out on exams, were anxious, or worried about class performance or math. For the 30% who reported no performance anxiety, posture had no significant effect. When students become aware of slouching thought posture feedback and then interrupt their slouching by sitting up, they report an increase in concentration, attention and school performance (Peper et al., 2024).
How we move and walk also affects our subjective energy. In most cases, when people sit for a long time, they report feeling more fatigue; however, if participants interrupt sitting with short movement practices they report becoming less fatigue and improved cognition (Wennberg et al., 2016). The change in subjective energy and mood depends upon the type of movement practice. Peper & Lin (2012) reported that when students were asked to walk in a slow slouching pattern looking down versus to walk quickly while skipping and looking up, they reported that skipping significantly increased their subjective energy and mood while the slouch walking decreased their energy. More importantly, student who had reported that they felt depressed during the last two years had their energy decrease significantly more when walking very slowly while slouched than those who did not report experiencing depression. Regardless of their self-reported history of depression, when students skipped, they all reported an increase in energy (Peper & Lin, 2012; Miragall et al., 2020).
What to do:
- Walk with a quick step while looking up and around.
- Wear a posture feedback device such as the UpRight Go 2 to remind you when you slouch to change posture and activity (Peper et al., 2019; Roggio et al., 2021).
- When sitting put a small pillow in the mid back so that you can sit more erect (for more suggestions, see the article by Peper et al., 2017a, Posture and mood: Implications and applications to therapy).
- Place photo and other objects that you like to look a slightly higher on your wall so that you automatically look up.
(8) Shallow breathing increases the risk for anxiety
When slouching we automatically tend to breathe slightly faster and more shallowly. This breathing pattern increases the risk for anxiety since it tends to decrease pCO2 (Feinstein et al., 2022; Meuret, Rosenfield, Millard & Ritz, 2023; Paulus, 2013; Smits et al., 2022; Van den Bergh et al., 2013). Sitting slouched also tends to inhibit abdominal expansion during the inhalation because the waist is constricted by clothing or a belt –sometimes labeled as ‘designer jean syndrome’ and may increase abdominal symptoms such as acid reflux and irritable bowel symptoms (Engeln & Zola, 2021; Peper et al., 2016; Peper et al., 2020). When students learn diaphragmatic breathing and practice diaphragmatic breathing whenever they shallow breathe or hold their breath, they report a significant decrease in anxiety, abdominal symptoms and even menstrual cramps (Haghighat et al., 2020; Peper et al., 2022; Peper et al., 2023).
What to do:
- Loosen your belt and waist constriction when sitting so that the abdomen can expand.
- Learn and practice effortless diaphragmatic breathing to reduce anxiety.
Conclusion
There are many topics related to postural health and technology overuse that were addressed in this article. Some topics are beyond the scope of the article, and therefore seen as limitations. These relate to diagnosis and treatment of attentional deficits, or dependency leading to tolerance, withdrawal and cravings (e.g., addiction-like symptoms), or of modeling relationships between factors that contribute to the increasing epidemic of mental and physical illness associated with smartphone use and social media, such as hypotheses examining the extent to which digital technologies (a) displace/ replace; (b) compete/ interfere with; and/or, (c) complement/ enhance in-person activities and relationships. Typical pharmaceutical ‘treat-the-symptom’ approaches for addressing ‘tech stress’ related to technology overuse includes prescribing ‘anxiolytics, pain-killers and muscle relaxants’ (Kazeminasab et al., 2022; Kim, Seo, Abdi, & Huh, 2020). Although not usually included in diagnosis and treatment strategies, suggesting improving posture and breathing practices can significantly affect mental and physical health. By changing posture and breathing patterns, individuals may have the option to optimize their health and well-being.
See the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics by Erik Peper, Richard Harvey and Nancy Faass. Available from: https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/

Explore the following blogs for more background and useful suggestions
References
Abbasi, G. A., Jagaveeran, M., Goh, Y. N., & Tariq, B. (2021). The impact of type of content use on smartphone addiction and academic performance: Physical activity as moderator. Technology in Society, 64, 101521. https://doi.org/10.1016/j.techsoc.2020.101521
Abusamak, M., Jaber, H. M., & Alrawashdeh, H. M. (2022). The effect of lockdown due to the COVID-19 pandemic on digital eye strain symptoms among the general population: a cross-sectional survey. Frontiers in Public Health, 10, 895517. https://doi.org/10.3389/fpubh.2022.895517
Akulwar-Tajane, I., Parmar, K. K., Naik, P. H., & Shah, A. V. (2020). Rethinking screen time during COVID-19: impact on psychological well-being in physiotherapy students. Int J Clin Exp Med Res, 4(4), 201-216. https://doi.org/10.26855/ijcemr.2020.10.014
Aliberti, S., Invernizzi, P. L., Scurati, R., & D’Isanto, T. (2020). Posture and skeletal muscle disorders of the neck due to the use of smartphones. Journal of Human Sport and Exercise , 15 (3proc), S586-S598. https://www.jhse.ua.es/article/view/2020-v15-n3-proc-posture-skeletal-muscle-disorders-neck-smartpho; https://air.unimi.it/retrieve/handle/2434/774436/1588570/HSE%20-%20Posture%20and%20skeletal%20muscle%20disorders.pdf
AmSAT. (2024). American Society for the Alexander Technique. Accessed July 27, 2024. https://alexandertechniqueusa.org/
Arundell, L., Salmon, J., Koorts, H. et al. (2019). Exploring when and how adolescents sit: cross-sectional analysis of activPAL-measured patterns of daily sitting time, bouts and breaks. BMC Public Health 19, 653. https://doi.org/10.1186/s12889-019-6960-5
Bhargava, V. R., & Velasquez, M. (2021). Ethics of the attention economy: The problem of social media addiction. Business Ethics Quarterly, 31(3), 321-359. https://doi.org/10.1017/beq.2020.32
Betsch, M., Kalbhen, K., Michalik, R., Schenker, H., Gatz, M., Quack, V., Siebers, H., Wild, M., & Migliorini, F. (2021). The influence of smartphone use on spinal posture – A laboratory study. Gait Posture, 85, 298-303. https://doi.org/10.1016/j.gaitpost.2021.02.018
Blodgett, J.M., Ahmadi, M.N., Atkin, A.J., Chastin, S., Chan, H-W., Suorsa, K., Bakker, E.A., Hettiarcachchi, P., Johansson, P.J., Sherar,L. B., Rangul, V., Pulsford, R.M…. (2024). ProPASS Collaboration , Device-measured physical activity and cardiometabolic health: the Prospective Physical Activity, Sitting, and Sleep (ProPASS) consortium, European Heart Journal, 45(6) 458–471, https://doi.org/10.1093/eurheartj/ehad717
Bochicchio, V., Keith, K., Montero, I., Scandurra, C., & Winsler, A. (2022). Digital media inhibit self-regulatory private speech use in preschool children: The “digital bubble effect”. Cognitive Development, 62, 101180. https://doi.org/10.1016/j.cogdev.2022.101180
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Cacciatore, T. W., Johnson, P. M., & Cohen, R. G. (2020). Potential mechanisms of the Alexander technique: Toward a comprehensive neurophysiological model. Kinesiology Review, 9(3), 199-213. https://doi.org/10.1123/kr.2020-0026
Chandrasekaran, B., & Ganesan, T. B. (2021). Sedentarism and chronic disease risk in COVID 19 lockdown–a scoping review. Scottish Medical Journal, 66(1), 3-10. https://doi.org/10.1177/0036933020946336
Childers, C., & Boatwright, B. (2021). Do digital natives recognize digital influence? Generational differences and understanding of social media influencers. Journal of Current Issues & Research in Advertising, 42(4), 425-442. https://doi.org/10.1080/10641734.2020.1830893
Cox, D.A., Hammond, K.E., & Gray, K. (2023). Generation Z and the Transformation of American Adolescence: How Gen Z’s Formative Experiences Shape Its Politics, Priorities, and Future. Survey Center of American Life, November 23, 2023. Accessed July 4, 2024. https://www.americansurveycenter.org/research/generation-z-and-the-transformation-of-american-adolescence-how-gen-zs-formative-experiences-shape-its-politics-priorities-and-future/
Crain, M. (2021). Profit over privacy: How surveillance advertising conquered the internet. U of Minnesota Press. https://www.amazon.com/Profit-over-Privacy-Surveillance-Advertising/dp/1517905044
Cova, E. (2024). Pedestrian fatalities at historic high. Smart Growth America (data from U.S. Department of Transportation (USDOT). Accessed July 2, 2024. https://smartgrowthamerica.org/pedestrian-fatalities-at-historic-high/
Duarte, F. (2023). Average Screen Time for Teens (2024). Exploding Topics. Accessed July 5, 2024. https://explodingtopics.com/blog/screen-time-for-teens#average
DeWitt, D. (2018). How Does Text Neck Cause Pain? Spine-Health October 26, 2018. Accessed July 5, 2024. https://www.spine-health.com/conditions/neck-pain/how-does-text-neck-cause-pain
Dockrill, P. (2020). Your laptop charger is more powerful than Apollo11’s computer, says apple developer. Science Alert, Janural 12, 2020. Accessed July 4, 2024. https://www.sciencealert.com/apollo-11-s-computer-was-less-powerful-than-a-usb-c-charger-programmer-discovers
Elsayed, W. (2021). Covid-19 pandemic and its impact on increasing the risks of children’s addiction to electronic games from a social work perspective. Heliyon, 7(12). https://doi.org/10.1016/j.heliyon.2021.e08503
Engeln, R., & Zola, A. (2021). These boots weren’t made for walking: gendered discrepancies in wearing painful, restricting, or distracting clothing. Sex roles, 85(7), 463-480. https://doi.org/10.1007/s11199-021-01230-9
Fainmesser, I. P., Galeotti, A., & Momot, R. (2023). Digital privacy. Management Science, 69(6), 3157-3173. https://doi.org/10.1287/mnsc.2022.4513
Feinstein, J. S., Gould, D., & Khalsa, S. S. (2022). Amygdala-driven apnea and the chemoreceptive origin of anxiety. Biological psychology, 170, 108305. https://10.1016/j.biopsycho.2022.108305
Fiebert, I., Kistner, F., Gissendanner, C., & DaSilva, C. (2021). Text neck: An adverse postural phenomenon. Work, 69(4), 1261-1270. https://doi.org/10.3233/WOR-213547
Goodwin, R. D., Weinberger, A. H., Kim, J. H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. Journal of Psychiatric Research. 130, 441–446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Gupta, N. (2023). Impact of smartphone overuse on health and well-being: review and recommendations for life-technology balance. Journal of Applied Sciences and Clinical Practice, 4(1), 4-12. https://doi.org/10.4103/jascp.jascp_40_22
Haghighat, F., Moradi, R., Rezaie, M., Yarahmadi, N., & Ghaffarnejad, F. (2020). Added Value of Diaphragm Myofascial Release on Forward Head Posture and Chest Expansion in Patients with Neck Pain: A Randomized Controlled Trial. Research Square. https://doi.org/10.21203/rs.3.rs-53279/v1
Haidt, J. (2024). The Anxious generation: How the great rewiring of childhood is causing an epidemic of mental illness. New York: Penguin Press. https://www.anxiousgeneration.com/book
Hansraj, K.K. (2014). Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 25, 277-279. https://pubmed.ncbi.nlm.nih.gov/25393825/
Hernandez-de-Menendez, M., Escobar Díaz, C. A., & Morales-Menendez, R. (2020). Educational experiences with Generation Z. International Journal on Interactive Design and Manufacturing (IJIDeM), 14(3), 847-859. https://doi.org/10.1007/s12008-020-00674-9
Huh-Yoo, J., & Rader, E. (2020). It’s the Wild, Wild West: Lessons learned from IRB members’ risk perceptions toward digital research data. Proceedings of the ACM on Human-Computer Interaction, 4(CSCW1), 1-22. https://doi.org/10.1145/3392868
IIHS (2024). Fatality Facts 2022Pedestrians. The Insurance Institute for Highway Safety (IIHS). Accessed July 2, 2024. https://www.iihs.org/topics/fatality-statistics/detail/pedestrians
Kazeminasab, S., Nejadghaderi, S. A., Amiri, P., Pourfathi, H., Araj-Khodaei, M., Sullman, M. J., … & Safiri, S. (2022). Neck pain: global epidemiology, trends and risk factors. BMC musculoskeletal disorders, 23, 1-13. https://doi.org/10.1186/s12891-021-04957-4
Kim, K. H., Seo, H. J., Abdi, S., & Huh, B. (2020). All about pain pharmacology: what pain physicians should know. The Korean journal of pain, 33(2), 108-120. https://doi.org/10.3344/kjp.2020.33.2.108
Kushlev, K., & Leitao, M. R. (2020). The effects of smartphones on well-being: Theoretical integration and research agenda. Current opinion in psychology, 36, 77-82. https://doi.org/10.1016/j.copsyc.2020.05.001
Lewis, H.R. (2024). Mechanical intelligence and counterfeit humanity. Harvard Magazine, 126(6), 38-40. https://www.harvardmagazine.com/2024/07/harry-lewis-computers-humanity#google_vignette
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press. https://www.amazon.com/Attention-Span-Finding-Fighting-Distraction-ebook/dp/B09XBJ29W9
Mason, M. C., Zamparo, G., Marini, A., & Ameen, N. (2022). Glued to your phone? Generation Z’s smartphone addiction and online compulsive buying. Computers in Human Behavior, 136, 107404. https://doi.org/10.1016/j.chb.2022.107404
McLaughlin, W.M., Cravez, E., Caruana, D.L., Wilhelm, C., Modrak, M., & Gardner, E.C. (2023). An Epidemiological Study of Cell Phone-Related Injuries of the Hand and Wrist Reported in United States Emergency Departments From 2011 to 2020. J Hand Surg Glob, 5(2),184-188. https://doi.org/10.1016/j.jhsg.2022.11.009
Meuret, A. E., Rosenfield, D., Millard, M. M., & Ritz, T. (2023). Biofeedback Training to Increase Pco2 in Asthma With Elevated Anxiety: A One-Stop Treatment of Both Conditions?. Psychosomatic medicine, 85(5), 440-448. https://doi.org/10.1097/PSY.0000000000001188
Miragall, M., Borrego, A., Cebolla, A., Etchemendy, E., Navarro-Siurana, J., Llorens, R., … & Baños, R. M. (2020). Effect of an upright (vs. stooped) posture on interpretation bias, imagery, and emotions. Journal of Behavior Therapy and Experimental Psychiatry, 68, 101560. https://doi.org/10.1016/j.jbtep.2020.101560
Mohan, A., Sen, P., Shah, C., Jain, E., & Jain, S. (2021). Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1). Indian journal of ophthalmology, 69(1), 140-144. https://doi.org/10.4103/ijo.IJO_2535_20
Muchacka-Cymerman, A. (2022). ‘I wonder why sometimes I feel so angry’ The associations between academic burnout, Facebook intrusion, phubbing, and aggressive behaviours during pandemic Covid 19. Polish Psychological Bulletin, 53(4). https://doi.org/10.24425/ppb.2022.143376
Nakshine, V. S., Thute, P., Khatib, M. N., & Sarkar, B. (2022). Increased screen time as a cause of declining physical, psychological health, and sleep patterns: a literary review. Cureus, 14(10). https://doi.org/10.7759/cureus.30051
Nawaz, S., Bhowmik, J., Linden, T., & Mitchell, M. (2024). Validation of a modified problematic use of mobile phones scale to examine problematic smartphone use and dependence. Heliyon, 10(2). https://doi.org/10.1016/j.heliyon.2024.e24832
Nicholas, A. J. (2020). Preferred learning methods of generation Z. Faculty and Staff – Articles & Papers. Digital Commons @ Salve Regina. Salve Regina University. https://digitalcommons.salve.edu/fac_staff_pub/74
OHSU. (2022). Myopia on the rise, especially among children. Casey Eye Institute. Oregan Health and Science University. Accessed July 7, 2024. https://www.ohsu.edu/casey-eye-institute/myopia-rise-especially-among-children
Orsolini, L., Longo, G., & Volpe, U. (2023). The mediatory role of the boredom and loneliness dimensions in the development of problematic internet use. International Journal of Environmental Research and Public Health, 20(5), 4446. https://doi.org/10.3390/ijerph20054446
Pandey, R., Gaur, S., Kumar, R., Kotwal, N., & Kumar, S. (2020). Curse of the technology-computer related musculoskeletal disorders and vision syndrome: a study. International Journal of Research in Medical Sciences, 8(2), 661. https://doi.org/10.18203/2320-6012.ijrms20200253
Park, J. C., Kim, S., & Lee, H. (2020). Effect of work-related smartphone use after work on job burnout: Moderating effect of social support and organizational politics. Computers in human behavior, 105, 106194. https://doi.org/10.1016/j.chb.2019.106194
Paulus, M.P. (2013). The breathing conundrum-interoceptive sensitivity and anxiety. Depress Anxiety.30(4), 315-20. https://doi.org/10.1002/da.22076
Peper, E. (2021). Resolve eyestrain and screen fatigue. Well Being Journal, 30(1), 24-28. https://wellbeingjournal.com/resolve-eyestrain-and-screen-fatigue/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Mason, L. (2019). “Don’t slouch!” Improve health with posture feedback. Townsend Letter-The Examiner of Alternative Medicine, 436, 58-61. https://www.researchgate.net/publication/337424599_Don%27t_slouch_Improve_health_with_posture_feedback
Peper, E., Harvey, R., Mason, L., & Lin, I.-M. (2018). Do better in math: How your body posture may change stereotype threat response. NeuroRegulation, 5(2), 67–74. http://dx.doi.org/10.15540/nr.5.2.67
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07
Peper, E. & Lin, I-M. (2012). Increase or decrease depression-How body postures influence your energy level. Biofeedback, 40 (3), 126-130. https://doi.org/10.5298/1081-5937-40.3.01
Peper, E., Lin, I-M, & Harvey, R. (2017a). Posture and mood: Implications and applications to therapy. Biofeedback, 35(2), 42-48. https://doi.org/10.5298/1081-5937-45.2.03
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Quach, S., Thaichon, P., Martin, K. D., Weaven, S., & Palmatier, R. W. (2022). Digital technologies: tensions in privacy and data. Journal of the Academy of Marketing Science, 50(6), 1299-1323. https://doi.org/10.1007/s11747-022-00845-y
Resnik, D. B. (2021). Standards of evidence for institutional review board decision-making. Accountability in research, 28(7), 428-455. https://doi.org/10.1080/08989621.2020.1855149
Roggio, F., Ravalli, S., Maugeri, G., Bianco, A., Palma, A., Di Rosa, M., & Musumeci, G. (2021). Technological advancements in the analysis of human motion and posture management through digital devices. World journal of orthopedics, 12(7), 467. https://doi.org/10.5312/wjo.v12.i7.467
Sankaridurg, P., Tahhan, N., Kandel, H., Naduvilath, T., Zou, H., Frick,K.D., Marmamula, S., Friedman, D.S., Lamoureux, e. Keeffe, J. Walline, J.J., Fricke, T.R., Kovai, V., & Resnikoff, S. (2021) IMI Impact of Myopia. Invest. Ophthalmol. Vis. Sci, 62(5), 2. https://doi.org/10.1167/iovs.62.5.2
Satılmış, S. E., Cengız, R., & Güngörmüş, H. A. (2023). The relationship between university students’ perception of boredom in leisure time and internet addiction during social isolation process. Bağımlılık Dergisi, 24(2), 164-173. https://doi.org/10.51982/bagimli.1137559
Schenarts, P. J. (2020). Now arriving: surgical trainees from generation Z. Journal of surgical education, 77(2), 246-253. https://doi.org/10.1016/j.jsurg.2019.09.004
Schneider, M. (2016). Vision for life. Ten Steps to Natural Eyesight Improvement. Berkeley: North Atlantic books. https://www.amazon.com/Vision-Life-Revised-Eyesight-Improvement/dp/1623170087
Singapore National Eye Centre. (2024). Severe myopia cases among children in Singapore almost doubled in past decade. CAN. Accessed July 4, 2024. https://www.channelnewsasia.com/singapore/myopia-children-cases-almost-double-glasses-eye-checks-4250266
Smits, J. A., Monfils, M. H., Otto, M. W., Telch, M. J., Shumake, J., Feinstein, J. S., … & Exposure Therapy Consortium. (2022). CO2 reactivity as a biomarker of exposure-based therapy non-response: study protocol. BMC psychiatry, 22(1), 831. https://doi.org/10.1186/s12888-022-04478-x
STAT (2024). The society of teachers of the Alexander Technique. Assessed July 27, 2024. https://alexandertechnique.co.uk/
Stuart, S., Godfrey, A., & Mancini, M. (2022). Staying UpRight in Parkinson’s disease: A pilot study of a novel wearable postural intervention. Gait & Posture, 91, 86-93. https://doi.org/10.1016/j.gaitpost.2021.09.202
Swatzyna, R. (2023). Personal communications.
Szymkowiak, A., Melović, B., Dabić, M., Jeganathan, K., & Kundi, G. S. (2021). Information technology and Gen Z: The role of teachers, the internet, and technology in the education of young people. Technology in Society, 65, 101565. https://doi.org/10.1016/j.techsoc.2021.101565
Tsai, H. Y., Peper, E., & Lin, I. M.*(2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23-27. https://doi.org/10.15540/nr.3.1.23
Van den Bergh, O., Zaman, J., Bresseleers, J., Verhamme, P., Van Diest, I. (2013). Anxiety, pCO2 and cerebral blood flow, International Journal of Psychophysiology, 89 (1), 72-77. https://doi.org/10.1016/j.ijpsycho.2013.05.011
Veritas Health. (2020). Text Neck Symptoms and Causes Video. YouTube video, accessed August 29, 2024. https://www.spine-health.com/conditions/neck-pain/how-does-text-neck-cause-pain?source=YT
Wennberg, P., Boraxbekk, C., Wheeler, M., et al. (2016). Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open, 6, e009630. https://doi.org/10.1136/bmjopen-2015-009630
Yang, K. H. (2022). Selling consumer data for profit: Optimal market-segmentation design and its consequences. American Economic Review, 112(4), 1364-1393. https://www.aeaweb.org/articles/pdf/doi/10.1257/aer.20210616
[1] Correspondence should be addressed to: Erik Peper, Ph.D., Institute for Holistic Health Studies, Department of Recreation, Parks, Tourism and Holistic Health, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Email: epeper@sfsu.edu; web: www.biofeedbackhealth.org; blog: www.peperperspective.com
[2] I thank Ronald Swatzyna (2023), Licensed Clinical Social Worker for sharing this exercise with me. He discovered that a difference in the number of eye contacts depending how he walked. When he walked a 3.1 mile loop around the park in a poor posture- shoulders forward, head down position- and then reversed direction and walked in good posture with the shoulders back and the head level, that that he make about 5 times as many eye contacts with good posture compared to the poor posture. He observed that he make about five times as many eye contacts with good posture as compared to the poor posture.
Increase attention, concentration and school performance
Posted: August 15, 2024 Filed under: ADHD, attention, behavior, Breathing/respiration, digital devices, education, ergonomics, posture, screen fatigue, stress management, vision, zoom fatigue | Tags: cellphone, concentration 5 CommentsReproduced from: Peper, E., Harvey, R., & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2), 48-52. https://doi.org/10.5298/1081-5937-52.02.07

When I sit with good posture on my computer, I am significantly more engaged in what I’m doing. When I slouch on my computer I tend to procrastinate, go on my phone, and get distracted so it ends up taking much longer to do my work when my posture is bad.…I have ADHD and I struggle a lot with my mind wandering when I should be paying attention. Having good posture really helps me to lock in and focus.—22 year old male student.
Over the past two decades, there has been a significant increase in the prevalence of attention-deficit/hyperactivity disorder (ADHD), anxiety, and depression. ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18–25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020). Students are more distracted, stressed and exhausted (Hanscom, 2022; Hoyt et al., 2021). The more students are distracted, the lower their academic achievement (Feng et al., 2019). In our recent class survey of more than 100 junior and senior college students on the first day of class, 54% reported that they were tired and dreading the day when they woke up. When you are tired and stressed it is difficult to focus attention and have clarity of thought. Their self-report is similar to the mental health trends in the United States by age group in 2008–2019. Mental health of young people has significantly deteriorated over the last 15 years (Braghieri et al., 2021/2023).
The increase in psychological distress is most prevalent in people ages 18–29 and who were brought up with the cellphone (the iPhone was introduced in 2007) and social media. Now when students enter a class, they tend to sit down, look down at their cellphone while slouching, and they do not make contact with most other students unless instructed or reminded by the instructor. When instructed to talk to another student for less than 5 minutes (e.g., share something positive that happened to you this week), 93% of the students reported an increase in subjective energy and alertness (Peper, 2024).
As a group, students are social media and cell phone natives and thus have many distractions and stimuli to which they continuously respond. It is not surprising that the average attention span has decreased from 150 seconds in 2004 to 44 seconds in 2021 (Mark, 2023). More importantly, they now tend to sit in a slouched collapsed position, which facilitates access to hopeless, helpless, powerless and defeated thoughts and memories (Tsai et al., 2016; Peper et al., 2017) and reduces cognitive performance when performing mental math (Peper et al., 2018). Sitting slouched and looking down also reduces peripheral awareness and increases shallow thoracic breathing—a breathing pattern that increases the risk of anxiety. Experience this yourself.
For a minute, look at your cellphone while intensely reading the text or searching social media in the following two positions: sitting straight up and looking straight ahead at your cell phone or slouching and looking down at your cell phone, as shown in Figure 1. Most likely, your experience is similar to the findings from the classroom observational study in which half the students looked down and the other half looked straight ahead and then reversed their positions (Peper, unpublished). They then compared the subjective experience associated with the position. In the slouched position, most experienced a reduction in peripheral awareness and breathed more shallowly (see Figure 1).

Figure 1. Effect of slouching or looking straight ahead on vision and breathing.
The slouched position reduces social awareness and decreases awareness of external stimuli as illustrated in Steve Cutts’ superb animation, Mobile world (https://www.youtube.com/watch?v=wUW1wjlKvmY).
Given the constant stimulation, distractions and shortened attention span, it is more challenging to be calm and have clarity of mind when having to study or take an exam at school. As educators, we constantly explore ways to engage students and support their learning and especially share quick skills they can use to optimize performance (Peper& Wilson, 2021). In previous research, Harvey et al., 2020 showed that students who used posture feedback improved their health scores compared to the control group. The purpose of this paper is to share a 4-week class assignment by which numerous students reported an increase in attention, concentration, confidence, school performance and a decrease in stress.
Participants: 18 undergraduate students (7 males and 11 females, average age 22 [STDEV 2.2]) enrolled in an upper division class. As a report about an effort to improve the quality of a classroom activity, this report of findings was exempted from Institutional Review Board oversight.
Equipment: Wearable posture feedback device, UpRight Go 2, which the person wears on their neck and which provides vibratory feedback whenever they slouch, as shown in Figure 2. It is used in conjunction with the cellphone app that allows them to calibrate the feedback device.

Figure 2. Attachment of posture feedback device on neck or spine and the app to calibrate the device.
Procedure: Students attended the 3-hour weekly class that explored autogenic training, somatic awareness, psychobiology of stress, the role of posture, and the psychophysiology of respiration. The lectures included short experiential practices demonstrating the body-mind connections such as imagining a lemon to increase salivation, the effect of slouched versus erect posture on evoking positive/empowering or hopeless/helpless/powerless/defeated thoughts, and the effect of sequential 70% exhalation for 30 seconds on increasing anxiety (Tsai et al., 2016; Peper et al., 2017).
Each week for 4 weeks the students were assigned a self-practice that they would implement daily at home and record their experiences. At the end of the week, they reviewed their own log and summarized their own observations (benefits, difficulties). During the next class session, they met in small groups of 5 to 6 students to discuss their experiences and extract common themes.
The 4-week curriculum was sequenced as follows:
Week 1
- Lecture on the benefits/harms of posture with experiential practices (effect of slouching vs erect on access to hopeless/helpless/powerless thoughts versus optimistic and empowering thoughts; posture and arm strength (Peper, 2022).
- Homework assignments:
- Watch the great Ted Talk and one of the most viewed by Amy Cuddy (2013), “Your body language shapes who you are.”
- Keep a detailed log to monitor situations where they slouched and identify situations that were associated with slouching.
Week 2
- Lecture on psychophysiology and class discussion in which students shared their experiences of slouching; namely, what were the triggers, how it affected them and what they could do to change.
- Demonstration, explanation, and how to use the posture feedback device, UpRight Go 2.
- Homework assignment: Wear UpRight Go 2 during the day, use it in different settings (studying, walking, work), and keep a log. When it vibrates (slouching) observe what was going on and change your behavior such as when tired>get rest or do exercise; when depressed>change internal language; ergonomic issues>change the environment, posture>give yourself lower back support.
Week 3
- Class discussion on what to do when slouching is triggered by tiredness, negative and hopeless thoughts, ergonomics such as laptop placement and chair. Students meet in groups to share their experiences and what they did in response to the vibratory feedback.
- Homework assignment: Continue to wear the UpRight Go 2 during the day and keep a log.
Week 4
- Class discussion in groups of five students about their experiences of slouching, what to do and how it affects them.
- Homework assignment: Wear UpRight Go 2 during the day and keep a log. Submit a paper that describes their experience with the posture feedback from the UpRight Go 2 and fill out a short anonymous survey in which they rated their change in experience since using the posture feedback device on a scale from 3 (worse) to 0 (no change) to 3 (better) .
Results
All students reported that wearing the feedback device increased attention and concentration as shown in Figure 3.

Figure 3.
Amount of time using the UpRight Go 2:On the average the students used the device 4.8 days a week (STDEV 2.0) and 2.2 hours per day (STDEV 1.3).
Location of use:Although most students practiced sitting in front of their computer, they also reported using it while at work, playing pool or doing yoga and even while seeing a therapist.
Discussion
All the students reported that the posture feedback helped them to become more aware of slouching and when they then interrupted their slouching, they experienced an increase in energy and a decrease in stress. As a 21-year-old male student said: “I felt more engaged with whatever I was doing. I tend to … daydream and get distracted, but I experience much less of that when I sit with good posture.”
Many reported that it helped identify their emotions when they were feeling overwhelmed. Then they could sit up, shift their perspective, and many reported a decrease in back and neck pain as well as a decrease in tiredness. When participants wear non-invasive wearables that provide accurate feedback, they are often surprised what triggers are associated with feedback or how their performance improves when they respond to the feedback signal by changing their thoughts and behavior. This posture self-awareness project should be embedded in strategies that optimize the learning state as described by Peper & Wilson (2021).
To the students’ surprise, they were often unaware that they started to slouch, nor were they aware of how much this slouching was connected to their emotions, mental state or external factors. For example, one student reported that he wore the device while being in a therapy session. All of a sudden, it vibrated. At that moment, he realized that he was becoming anxious, although he and therapist were unaware. He then shared what happened with the therapist, and that helped the therapeutic process.
The benefits may not only be due to posture change but that the students became aware and interrupted their habitual pattern. This process is similar to that described by Charles Stroebel (1985) when he taught patients the Quieting Reflect that reduced numerous somatic symptoms ranging from headaches to hypertension.
The posture feedback intervention is both simple and challenging since it requires the participants to wear the device, identify factors that trigger the slouching, and interrupt their automatic patterns by changing posture and behavior whenever they felt the vibratory feedback. The awareness gave them the opportunity to change posture and thoughts. By shifting to an upright posture, they experienced that they could concentrate more and have increased energy. As a 19-year-old female student wrote: “My breathing was better and sitting in an upright position gave me more energy when doing tasks.”
Conclusion
We recommend that a 4-week home practice module that incorporates wearable posture feedback is offered to all students to enhance their well-being. With the posture feedback, participants can increase their awareness of slouching, identify situations that trigger slouch, and learn strategies to shift their posture, thoughts, emotions and external environment to optimize maintaining an empowered position. As a 20-year old male student reported, “The app helped me when I was feeling overwhelmed and then I would sit up. When I had it on, I did a lot of work. I was more concentrated.”
Explore the following blogs for more background and useful suggestions
References
Braghieri, L., Levy, R., & Makarin, A. (2023). Media and mental health (July 28, 2022). SSRN. (Original work published 2021). https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Centers for Disease Control and Prevention. (n.d.). ADHD through the years. Attention-Deficit / Hyperactivity Disorder (ADHD). Retrieved March 27, 2023, from https://www.cdc.gov/ncbddd/adhd/timeline.html
Cuddy, A. (2012) Your body language may shape who you are. TED Talk. Retrieved March 16, 2024 from https://www.youtube.com/watch?v=Ks-_Mh1QhMc
Feng, S., Wong, Y. K., Wong, L. Y., & Hossain, L. (2019). The internet and Facebook usage on academic distraction of college students, Computers & Education, 134, 41-49. https://doi.org/10.1016/j
Goodwin, R. D., Weinberger, A. H., Kim, J. H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. Journal of Psychiatric Research. 130, 441–446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hanscom, N. (2022). Students, staff notice higher levels of student distraction this school year, reflect on potential causes. Retrieved September 28, 2023, from https://dgnomega.org/13162/feature/students-staff-notice-higher-levels-of-student-distraction-this-school-year-reflect-on-potential-causes/
Harvey, R., Peper, E., Mason, L., & Joy, M. (2020). Effect of posture feedback training on health. Applied Psychophysiology and Biofeedback, 45(1), 59–65. https://doi.org/10.1007/s10484-020-09457-0
Hoyt, L. T., Cohen, A. K., Dull, B., Castro, E. M., & Yazdani, N. (2021). “Constant stress has become the new normal”: Stress and anxiety inequalities among U.S. college students in the time of COVID-19. Journal of Adolescent Health. 68(2), 270–276. https://doi.org/10.1016/j.jadohealth.2020.10.030
Mark, G. (2023). Attention span: A groundbreaking way to restore balance, happiness and productivity. Hanover Square Press.
Peper, E. (2022, March 4). A breath of fresh air: Breathing and posture to optimize health. [Conference presentation at the 2nd Virtual Ergonomics Summit], Krista Burns, PhD. https://www.youtube.com/watch?v=PhV7Ulhs38s
Peper, E. (2024a). Change in energy and alertness after talking with each other versus looking at cellphone. Data collected from HH380 class fall 2023. Unpublished.
Peper, E. (2024b). Changes in vision and breathing when looking down or straight ahead at the cellphone. Data collected from HH380 class, Spring, 2024, San Francisco State University. Unpublished.
Peper, E., Harvey, R., Mason, L., & Lin, I.-M. (2018). Do better in math: How your body posture may change stereotype threat response. NeuroRegulation, 5(2), 67–74. http://dx.doi.org/10.15540/nr.5.2.67
Peper, E., Lin, I.-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 49(2), 46-49. https://doi.org/10.5298/1081-5937-49-2-04
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570
Tsai, H. Y., Peper, E., & Lin, I.-M.(2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23–27. https://doi.org/10.15540/nr.3.1.23
Grandmother Therapy: A Common-Sense Approach to Health and Wellness
Posted: July 24, 2024 Filed under: ADHD, attention, behavior, education, Evolutionary perspective, Exercise/movement, Nutrition/diet, Pain/discomfort, relaxation, self-healing | Tags: anxiety, depression, epilepsy, exhaustion, grandmother therapy, health, insomnia, life style change, mental-health, therapy 1 CommentErik Peper, PhD and Angelika Sadar, MA

In today’s fast-paced world, college students and young adults often struggle with various health issues. From anxiety and depression to ADHD and epilepsy, these challenges can significantly impact their daily lives. But what if the solution to many of these problems lies in something as simple as “Grandmother Therapy”?
What is Grandmother Therapy? Grandmother Therapy is all about going back to basics and establishing healthy lifestyle habits. It’s the common-sense approach that our grandmothers might have suggested: regular sleep patterns, balanced nutrition, increased social connections, and regular physical activity.
The Problem: Many college students:
- Skip breakfast before their first class
- Rely on fast food and sugary stimulants
- Have irregular sleep schedules
- Spend excessive time on gaming and social media
The Medical Approach: Often, the quick solution is medication:
- Depression? Take antidepressants.
- Insomnia? Use sleeping pills.
- Anxiety? Try anti-anxiety medication.
- ADHD? Prescribe Ritalin or similar drugs.
While these treatments may help manage symptoms, they often overlook the underlying lifestyle factors contributing to these issues.
The Grandmother Therapy Approach:
- Establish regular sleep patterns
- Adopt healthy eating habits
- Increase social connections
- Incorporate regular physical activity
- Reduce gaming and social media use
Case Study #1: The Power of Sleep
This illustrates the simple intervention of having a bedtime routine. A college student in a holistic health class complained that she was tired most of the time and had difficulty focusing her attention and continuously drifted off in class.
Here is her reported sleep schedule:
- last night I went to bed at 3am and woke up 7;
- the day before, I went to bed at 1pm and woke up at 6,
- two nights before, I went to bed at 4pm and woke up at 10 am.
Holistic treatment approach:
Set a sleep schedule: she was provided with information about the importance of having a regular pattern of sleep and waking. Namely, go to bed at the same time and get up 8 hours later. She agreed to do an experiment for a week to go to bed at 12 and wake up at 8m. To her surprise, she felt so much more energized and could pay attention in class during the week of the experiment.
Case Study #2: Beyond Seizures: A Holistic Approach to Treating Psychogenic Nonepileptic Seizures
This case study highlights the importance of a comprehensive, lifestyle-based approach to treating psychogenic nonepileptic seizures (PNES). It follows a 24-year-old male student initially diagnosed with intractable epilepsy, experiencing over 10 seizures per week that didn’t respond to medication.
Key points:
1. Initial misdiagnosis: Despite normal MRI and EEG results, the client was initially treated for epilepsy.
2. Limited assessment: Traditional medical evaluations focused solely on seizure descriptions and diagnostics, overlooking crucial lifestyle factors.
3. Comprehensive evaluation: A psychophysiological assessment revealed high sympathetic arousal, including rapid breathing, sweaty palms, and muscle tension.
4. Lifestyle factors: The client’s diet consisted of high-glycemic fast foods, excessive caffeine, alcohol, and daily marijuana use. He also had significant student debt and a history of abdominal surgery.
Holistic treatment approach:
– Dietary changes: Switching to unprocessed, low-glycemic foods and increasing vegetable and fruit intake
– Breathing techniques: Learning and practicing slow diaphragmatic breathing
– Stress management: Addressing underlying stressors and practicing relaxation techniques
– Supplements: Adding omega-3 and multivitamins to support brain health
Remarkable results: Within four months, the patient became seizure-free, reduced marijuana use significantly, and decreased medication dosage.
Summary
These cases underscore the potential of integrating lifestyle modifications and stress management techniques in treating attention, anxiety and even psychogenic nonepileptic seizures; offering hope for patients who don’t respond to traditional treatments alone. Before turning to medication or complex treatments, consider the power of Grandmother Therapy. By addressing fundamental lifestyle factors, we can often improve our health and well-being significantly. Remember, sometimes the most effective solutions are the simplest ones.
The Challenges of Simplicity: While Grandmother Therapy may seem straightforward, its simplicity can make it challenging to implement. It requires commitment and a willingness to change long-standing habits.
Implement many Life Style Changes at once: Recommending one change at the time is logical; however, participants will more likely experience rapid benefits and are more motivated to continue when they change multiple lifestyle factors at once.
Call to Action: Are you struggling with health issues? Try implementing some aspects of Grandmother Therapy in your life. Implement changes and see how they impact your overall well-being.
Please let us know your experience with implementing Grandmother Therapy.
See the following blogs for more background information