Welcome the New Year with Inspiration
Posted: December 22, 2025 Filed under: attention, behavior, CBT, cognitive behavior therapy, emotions, healing, health, mindfulness, self-healing | Tags: hope, Inspreiation, meaning, post=traumatic growth, purpose, resilience 1 CommentAs the holiday season begins, I find myself looking back on all that has unfolded this year and looking forward with hope to the year ahead. My social media feed is full of touching, uplifting messages and videos—reminders of resilience, creativity, and the simple goodness in the world. Best wishes for the holidays and the New Year and I hope you will enjoy the two inspiring videos.
1. Nine life lessons from comedian Tim Minchin, presented at the University of Western Australia. His humor and wisdom offer a refreshing take on what truly matters.
2. A powerful story about transforming disaster into blessing.
If you ever feel stuck or unsure about the future, this video is a beautiful reminder that unexpected turns can lead to new possibilities.
Wishing you a healthy and inspiring New Year!
Erik
Breathe Away Menstrual Pain- A Simple Practice That Brings Relief *
Posted: November 22, 2025 Filed under: attention, behavior, biofeedback, Breathing/respiration, cognitive behavior therapy, education, emotions, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: dysmenorrhea, health, meditation, menstrual cramps, mental-health, mindfulness, wellness 2 CommentsAdapted from: Peper, E. Harvey, R., Chen, & Heinz, N. (2025). Practicing diaphragmatic breathing reduces menstrual symptoms both during in-person and synchronous online teaching. Applied Psychophysiology and Biofeedback, Published online: 25 October 2025. https://rdcu.be/eMJqt https://doi.org/10.1007/s10484-025-09745-7
“Once again, the pain starts—sharp, deep, and overwhelming—until all I can do is curl up and wait for it to pass. There’s no way I can function like this, so I call in sick. The meds take the edge off, but they don’t really fix anything—they just mask it for a little while. I usually don’t tell anyone it’s menstrual pain; I just say I’m not feeling well. For the next couple of days, I’m completely drained, struggling just to make it through.
Many women experience discomfort during menstruation, from mild cramps to intense, even disabling pain. When the pain becomes severe, the body instinctively responds by slowing down—encouraging rest, curling up to protect the abdomen, and often reaching for medication in hopes of relief. For most, the symptoms ease within a day or two, occasionally stretching into three, before the body gradually returns to balance.
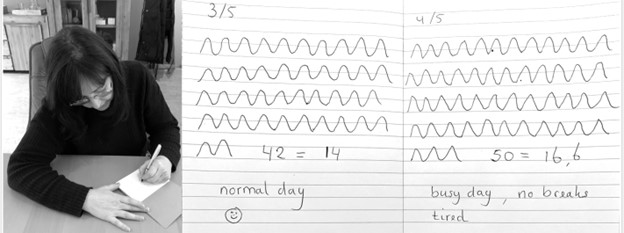
Another helpful approach is to practice slow abdominal breathing, guided by a breathing app FlowMD. In our study led by Mattia Nesse, PhD, in Italy, the response of one 22-year-old woman illustrated the power of this simple practice.
“Last night my period started, so I was a bit discouraged because I knew I’d get stomach pain, etc. On the other hand, I said, “Okay, let’s see if the breathing works,” and it was like magic — incredible. I’ll need to try it more times to understand whether it consistently has the same effect, but right now it truly felt magical. Just 3 minutes of deep breathing with the app were enough, and I’m not saying I don’t feel any pain anymore, but it has decreased a lot, so thank you! Thank you again for this tool… I’m really happy!”
The Silent Burden of Menstrual Pain
Menstrual pain, or dysmenorrhea, affects most women at some point in their lives — often silently. For many, the monthly cycle brings not only physical discomfort but also shame, fatigue, and interruptions to work or school. It is one of the leading causes of absenteeism and reduced productivity worldwide (Itani et al., 2022; Thakur & Pathania, 2022). In addition, the estimated health cost ranged from US $1367 to US$ 7043 per year (Huang et al., 2021). Yet, despite its prevalence, most women are never taught how to use their own physiology to ease these symptoms.
The Study (Peper et al, 2025)
Seventy-five university women participated across two upper-division Holistic Health courses. Forty-nine practiced 30 minutes per day of breathing and relaxation over five weeks as well as practicing the moment they anticipated or felt discomfort; twenty-six served as a comparison group without a specific daily self-care routine. Students rated change in menstrual symptoms on a scale from –5 (“much worse”) to +5 (“much better”). For the detailed steps in training, see the blog: https://peperperspective.com/2023/04/22/hope-for-menstrual-cramps-dysmenorrhea-with-breathing/ (Peper et al., 2023).
What changed
The results were striking. Women who practiced breathing and relaxation showed significant decrease in menstrual symptoms compared to the non-intervention group (p = 0.0008) as shown in Figure 1.

Figure 1. Decrease in menstrual symptoms as compared to the control group after implementing slow diaphragmatic breathing.
Why does breathing and posture change have a beneficial effect?
When you stay curled up, your abdomen becomes compressed, leaving little room for the lower belly to relax or for the diaphragm to move freely. The result? Tension builds, and pain often increases.
To reverse this, create space for relaxation. Gently loosen your waist and let your abdomen expand as you inhale. Uncurl your body—lengthen your spine and open your chest, as shown in Figure 2. With each easy breath, you invite calm and allow your body to shift from tension to ease.
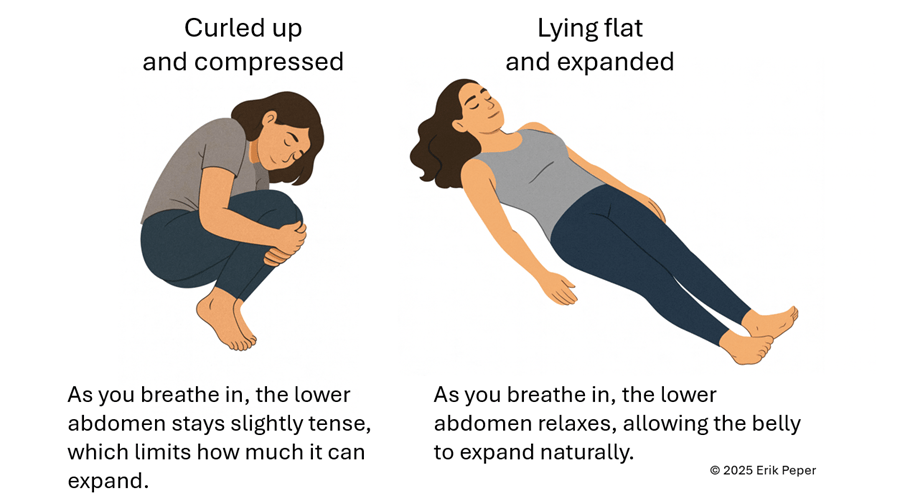
Figure 2. Curling up compresses the abdomen and prevents relaxation of the lower belly. In contrast, lying flat with the body gently expanded allows the abdomen to move freely with each breath, which can help reduce menstrual discomfort.
In contrast, slow abdominal or diaphragmatic breathing activates the body’s natural relaxation response. It quiets the stress-driven sympathetic nervous system, calms the mind, and improves circulation in the abdominal area. With each slow breath in, the abdomen gently expands while the pelvic floor and abdominal muscles relax. As you exhale, these muscles naturally tighten slightly, helping to massage and move blood and lymph through the abdominal region. This rhythmic movement supports healing and ease, as illustrated in Figure 3.
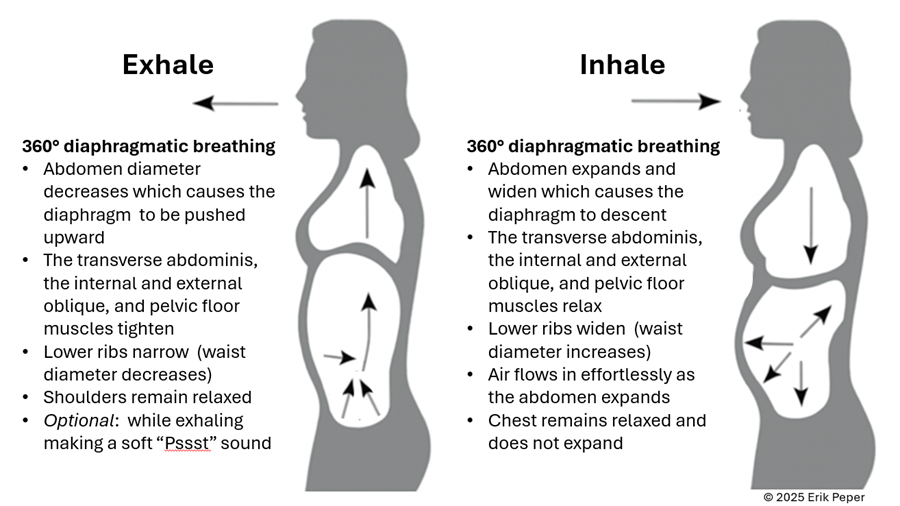
Figure 3. The dynamic process of diaphragmatic breathing.
The process of slower, lower diaphragmatic breathing
When lying down, rest comfortably on your back with your legs slightly apart. Allow your abdomen to rise naturally as you inhale and fall as you exhale. As you breathe out, imagine the air flowing through your abdomen, down your legs, and out through your feet. To deepen this sensation, you can ask a partner to gently stroke from your abdomen down your legs as you exhale—helping you sense the flow of release through your body.
Gently focus on slow, effortless diaphragmatic breathing. With each inhalation, your abdomen expands, and the lower belly softens. As you exhale, the abdomen gently goes down pushing the diaphragm upward and allowing the air to leave easily. Breathing slowly—about six breaths per minute—helps engage the body’s natural relaxation response.
If you notice that your breath is staying high in your chest instead of expanding through the abdomen, your symptoms may not improve and can even increase. One participant experienced this at first. After learning to let her abdomen expand with each inhalation while keeping her shoulders and chest relaxed, her next menstrual cycle was markedly easier and far less uncomfortable. The lesson is clear: technique matters.
“During times of pain, I practiced lying down and breathing through my stomach… and my cramps went away within ten minutes. It was awesome.” — 22-year-old college student
“Whenever I felt my cramps worsening, I practiced slow deep breathing for five to ten minutes. The pain became less debilitating, and I didn’t need as many painkillers.” — 18-year-old college student
These successes point out that it’s not just breathing — it’s how you breathe by providing space for the abdomen to expand during inhalation.
Practice: How to Do Diaphragmatic Breathing
- Find a quiet space. Lie on your back or sit comfortably erect with your shoulders relaxed.
- Place one hand on your chest and one on your abdomen.
- Inhale slowly through your nose for about 3–4 seconds. Let your abdomen expand as you breathe in — your chest should remain relaxed.
- Exhale gently through your mouth for 4—6 seconds, allowing the abdomen to fall or constrict naturally.
- As you exhale imagine the air moving down your arms, through your abdomen, down your legs, and out your feet
- Practice daily for 20 minutes and also for 5–10 minutes during the day when menstrual discomfort begins.
- Add warmth. Placing a warm towel or heating pad over your abdomen can enhance relaxation while lying on your back and breathing slowly.
With regular practice and implementing it during the day when stressed, this simple method can reduce cramps, promote calm, and reconnect you with your body’s natural rhythm.
Implement the ABCs during the day
The ABC sequence—adapted from the work of Dr. Charles Stroebel, who developed The Quieting Reflex (Stroebel, 1982)—teaches a simple way to interrupt stress reactions in real time. The moment you notice discomfort, pain, stress, or negative thoughts, interrupt the cycle with a simple ABC strategy:
A — Adjust your posture
Sit or stand tall, slightly arch your lower back and allowing the abdomen to expand while you inhale and look up. This immediately shifts your body out of the collapsed “defense posture’ and increases access to positive thoughts (Tsai et all, 2016; Peper et al., 2019)
B — Breathe
Allow your abdomen to expand as you inhale slowly and deeply. Let it get smaller as you exhale. Gently make a soft hissing sound as you exhale while helps the abdomen and pelvic floor to tighten. Then allow the abdomen to relax and widen which without effort draws the air in during inhalation. As you exhale, stay tall and imagine the air flowing through you and down your legs and out your feet.
C — Concentrate
Refocus your attention on what you want to do and add a gentle smile. This engages positive emotions, the smile helps downshift tension.
The video clip guides you through the ABCs process.
Integrate the breathing during the day by implementing your ABCs
When students practice relaxation technique and this method, they reported greater reductions in symptoms compared with a control group. By learning to notice tension and apply the ABC steps as soon as stress arises, they could shift their bodies and minds toward calm more quickly, as shown in Figure 4.
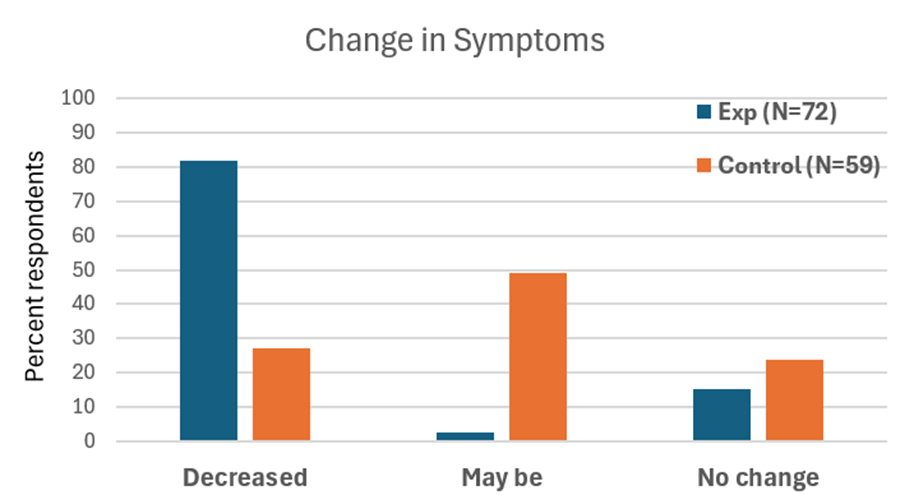
Figure 4. Change in symptoms after practicing a sequential relaxation and breathing techniques for four weeks.
Takeaway
Menstrual pain doesn’t have to be endured in silence or masked by medication alone. By practicing 30 minutes of slow diaphragmatic breathing daily and many times during the day, women may be able to reduce pain, stress, and discomfort — while building self-awareness and confidence in their body’s natural rhythms thereby having the opportunity to be more productive.
We recommend that schools and universities include self-care education—especially breathing and relaxation practices—as part of basic health curricula as this approach is scalable. Teaching young women to understand their bodies, manage stress, and talk openly about menstruation can profoundly improve well-being. It not only reduces physical discomfort but also helps dissolve the stigma that still surrounds this natural process,
Remember: Breathing is free—available anytime, anywhere and is helpful in reducing pain and discomfort. (Peper et al., 2025; Joseph et al., 2022)
See the following blogs for more in-depth information and practical tips on how to learn and apply diaphragmatic breathing:
REFERENCES
Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H.M.J. (2022). Primary Dysmenorrhea: Pathophysiology, Diagnosis, and Treatment Updates. Korean J Fam Med, 43(2), 101-108. https://doi.org/10.4082/kjfm.21.0103
Huang, G., Le, A. L., Goddard, Y., James, D., Thavorn, K., Payne, M., & Chen, I. (2022). A systematic review of the cost of chronic pelvic pain in women. Journal of Obstetrics and Gynaecology Canada, 44(3), 286–293.e3. https://doi.org/10.1016/j.jogc.2021.08.011
Joseph, A. E., Moman, R. N., Barman, R. A., Kleppel, D. J., Eberhart, N. D., Gerberi, D. J., Murad, M. H., & Hooten, W. M. (2022). Effects of slow deep breathing on acute clinical pain in adults: A systematic review and meta-analysis of randomized controlled trials. Journal of Evidence-Based Integrative Medicine, 27, 2515690X221078006. https://doi.org/10.1177/2515690X221078006
Peper, E., Booiman, A. & Harvey, R. (2025). Pain-There is Hope. Biofeedback, 53(1), 1-9. http://doi.org/10.5298/1081-5937-53.01.16
Peper, E., Chen, S., Heinz, N., & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E., Harvey, R., Chen, S., & Heinz, N. (2025). Practicing diaphragmatic breathing reduces menstrual symptoms both during in-person and synchronous online teaching. Applied Psychophysiology and Biofeedback. Published online: 25 October 2025. https://rdcu.be/eMJqt https://doi.org/10.1007/s10484-025-09745-7
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. https://doi.org/10.15540/nr.6.3.1533-1
Stroebel, C. (1982). The Quieting Reflex. New York: Putnam Pub Group. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570/
Thakur, P. & Pathania, A.R. (2022). Relief of dysmenorrhea – A review of different types of pharmacological and non-pharmacological treatments. MaterialsToday: Proceedings.18, Part 5, 1157-1162. https://doi.org/10.1016/j.matpr.2021.08.207
Tsai, H. Y., Peper, E., & Lin, I. M. (2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23-27. https://doi.org/10.15540/nr.3.1.23
*Edited with the help of ChatGPT 5
This May Save Your Life! Bacteriophage Treatment for Bacterial Diseases*
Posted: September 11, 2025 Filed under: Evolutionary perspective, healing, health, Pain/discomfort, self-healing | Tags: antibiotic resistance, antibiotics, bacteria, bacteriohage, health, Medicine Leave a commentRecently, I listened to a special episode featuring Lina Zeldovich on her book The Living Medicine, from This Podcast Will Kill You. I was totally inspired because it discussesd the healing power of bacteriophages, which apparently treat antibiotic-resistant bacterial infections successfully, reportedly without side effects. (Bacterial phages are viruses that selectively kill specific bacteria and have been used to treat multi-antibiotic-resistant conditions).
This emerging therapy is an aspect of individualized treatment. Zeldovich reports that it can not only be used to treat, but also to prevent the occurrence of bacterial illnesses. I rushed out to buy the book, The Living Medicine: How a lifesaving cure was nearly lost and why it will rescue us when antibiotics fail. Zeldovich is a great science storyteller and the book really captured me. I read it in two evenings and wanted to share this information, since a day may come when it could save your life.
This is a must-read for all of us, particularly for health professionals. It offers hope through a non-toxic strategy in the fight against antibiotic-resistant disease. The book provides a perspective on the challenges of bringing this effective healing strategy to acceptance and implementation when cultural biases and financial disincentives have stood in the way.;

Zeldovich, describes the development and history of bacterial phage medicine and why it has taken so many years to become accepted in the West. Only after several high-profile cases has this approach become of interest. A prime example is the 2016 treatment of Dr. Tom Patterson, a professor at UC San Diego, who contracted a life-threatening Acinetobacter baumannii infection while traveling (Garnett, 2019). The bacteria that caused his infection was resistant to every available antibiotic. After he slipped into a coma, his doctors feared the worst. As a last resort, his wife, Dr. Steffanie Strathdee, worked with scientists to identify phages that could target the infection. Within 48 hours of receiving intravenous phage therapy, Patterson woke up. He went on to make a full recovery, one of the first documented cases in the U.S. in which phages saved a patient’s life.
Pros and cons of antibiotics
Until antibiotics were discovered, bacterial infections were often fatal. This changed with the discovery of penicillin by Alexander Fleming in 1928. During World War II, antibiotics saved countless solders’ lives in the treatment of infected wounds, pneumonia, and blood poisoning. The antibiotic approach was quickly adopted in the United States, beginning in the early 1940’s, since penicillin could be mass-produced and thus was highly profitable for the pharmaceutical companies. Despite the initial success of the drug, bacteria quickly developed antibiotic resistance to penicillin due to the ability of bacteria to produce β-lactamase, an enzyme capable of breaking down the drug.
Antibiotics were and are extraordinary drugs. When a patient is becoming sicker and sicker as a bacterial infection spreads, the infection can be stopped in its tracks with an effective antibiotic. Before the era of antibiotic resistance, patients recovered as if by magic, simple by giving an antibiotic orally or intravenously,
I still remember when our son developed pneumonia at the age of 12, initially with coughing, a high fever, chest pain, and a great deal of congestion. But as the infection progressed, he began to have difficulty breathing and his energy was fading. We were initially hesitant to give the prescribed antibiotic because we hoped his immune system would be able to fight the infection. My hesitancy was based upon the fact that antibiotics do not selectively kill the bacteria causing the illness, but also destroy beneficial bacteria that are part of the human biome.
Millions of women who have taken an antibiotic for an infection subsequently experience chronic vaginal yeast infections. This occurs because antibiotics such as tetracyclines, which are used to treat UTIs, intestinal tract infections, eye infections, sexually transmitted infections, acne, and gum disease, also kill the healthy bacteria of the human biome in the vagina. Since nature abhors a vacuum, yeast then overgrow where healthy bacteria used to predominate, thus allowing a vaginal infection (candidiasis) to occur (Spinillo et al., 1999)
In the case of my son, as it became clear that he was getting weaker and his immune system was not successfully clearing the infection, we followed his doctor’s advice and gave him the antibiotic. Magically, within two days he was better, and we continued with the course of antibiotics to clear his body of all the bacteria that was causing the pneumonia. Treatment is always a decision that involves balancing risk and benefit, getting sicker or getting well, given the possible negative side effects of the treatment. At the same time, it was possible that the antibiotic would not work since there was no time to run a lab test for that specific bacteria. If it had not worked, he would have needed another, different antibiotic, and if that had failed, a third drug.
Today, antibiotic resistance has grown into a worldwide crisis. The World Health Organization estimates that antimicrobial resistance directly caused 1.27 million deaths and contributed to another 5 million deaths globally in 2019. In the United States alone, the CDC reports over 2.8 million antibiotic-resistant infections occur every year, leading to at least 35,000 deaths and more than 3 million cases of infection by Clostridioides difficile (C. diff) occur (CDC, 2019).
Potentially fatal diseases that have become antibiotic resistant include Staphylococcus aureus (such as methicillin-resistant Staph aureus or MRSA) and Streptococcus pneumoniae (strep), as well as Klebsiella pneumoniae, Acinetobacter baumannii, Escherichia coli, and Pseudomonas aeruginosa. These six pathogens alone were responsible for nearly 1 million deaths in 2019. Other dangerous resistant infections include multidrug-resistant tuberculosis (MDR-TB), extensively drug-resistant typhoid fever, and carbapenem-resistant Enterobacteriaceae (CRE), sometimes described as “nightmare bacteria” (Murray, et al., 2022).
Bacterial resistance develops because bacteria, like all living organisms, evolve. Antibiotics, which are typically chemicals produced by molds or other organisms, work by killing or interfering with the life cycle of specific types of bacteria. However, antibiotics are often a blunt instrument: they resemble a form of what has been referred to as carpet bombing in warfare, in which the enemy is destroyed, but the whole neighborhood is also destroyed. While antibiotics may eliminate the bacteria causing the infection, they can also damage or destroy many beneficial bacteria in the gut, on the skin, and other areas of the body.
One in five medication-related visits to the emergency room are from reactions to antibiotics (CDC, 2025). This collateral damage can disrupt the gut microbiome, weaken immunity, and create opportunities for other harmful microbes to flourish. In addition, frequent antibiotic use could possibly contribute to obesity, as evidenced by the fact that low dosages of antibiotics are often given to farm animals, not only to prevent disease, but to increase their weight. Antibiotics appear to alter the gut microbiome to make it more efficient at extracting nutrients and energy from feed (Cox, 2016).
Antibiotics have been one of the major focuses of pharmaceutical drug development; however, they can cause serious side effects and tend to become less effective over time as the bacteria develop antibiotic resistance. Many bacteria can develop antibiotic resistance in less than a 6 month time period (Poku et al., 2023). Once bacteria develop antibiotic resistance to one drug, a new antibiotic drug needs to be discovered, developed, and produced. Even the newer and stronger antibiotics rapidly loose their efficacy as the bacteria develop resistance to it. In the long term, it is a loosing battle, and a totally new approach is needed.
Bacteriophage therapy
One new approach worth closer consideration is bacteriophage therapy. In nature, bacteria and viruses have been locked in a constant evolutionary battle for billions of years. Bacteria are vulnerable to specific viruses, so a bacteriophage, or phage, refers to a virus that specifically infects and kills a particular strain of bacteria. As bacteria change to evade attack, phages evolve to counter them, maintaining an ongoing balance to some degree. The theory is that because phages are very specific and only act on one particular type of bacteria, that potentially makes them a uniquely precise form of medicine.
The challenge involves matching the phage to the pathogenic bacterium, and there are an astonishing number of different phages and bacteria. In two patients with the same symptoms or diagnosis, the causal bacteria could be a slightly different subspecies. When used clinically, bacteriophages work only against specific type of bacterium. This makes phage therapy a useful form of individualized medicine.
To be successful, the bacteria that causes the patient’s infection must first be identified. This is different from the way in which antibiotics are commonly used in primary care. When a patient develops symptoms, often an antibiotic is given before the bacteria has been identified, and if it does not work, another antibiotic is given.
In contrast, phage therapy depends on matching the specific disease-causing bacteria to a specific phage. Phage medicine requires a library of thousands of known phages as an essential prerequisite to treatment. Clinical care involves identifying the phage that can target and destroy that specific bacterium. Then the phage is cultured, purified, and administered in either a liquid preparation, capsule, ointment, intravenously or at a wound site depending on the type of infection.
Unlike antibiotics, which often damage beneficial microbes, phages only target the bacteria they evolved to destroy, leaving the rest of the human biome intact. Because viruses are capable of reproduction, once a phage reaches its bacterial host, it multiplies rapidly and produces hundreds of new phages that continue to attack the specific disease-causing bacteria as shown in Figure 1. According to reports from phage medicine, symptoms improve dramatically within 24 hours. The phages are self-limiting and their numbers naturally decline once the infection is cleared.

Figure 1. Electron micrograph of a phage attaching and injecting it viral genome into the cell and its life cycle
At present, phage therapy has already shown success against a variety of resistant infections, including methicillin-resistant Staphylococcus aureus (MRSA), Acinetobacter baumannii wound infections (a major problem in military medicine), multidrug-resistant Klebsiella pneumoniae, and even certain cases of tuberculosis. Instead of being the last line of defense, in the future this may become the first line of defense.
The initial research and clinical use has been concentrated in Russia and Eastern Europe. The United States largely abandoned phage therapy after the discovery of antibiotics. Several factors contributed to this trend.
- Funding barriers. Funding agencies in the West have not seen phage therapy as a credible option. In many cases, the review committees that decided which grant applications to approve have tended to fund research that supported their own biases and their interests in antibiotic research. As a result, research money was rarely allocated to study or develop phage therapies. Generally, high- risk, novel research ideas are almost never funded by federal agencies except DARPA which is more open to new concepts when they offer a high potential of success.
- Economic realities discourage investment. Unlike antibiotics, which can be mass-produced as a single chemical and sold at high volume for profit, phage therapy requires maintaining large, evolving phage libraries and tailoring treatments to each patient. This individualized model offered little appeal to large pharmaceutical companies seeking standardized products with a high payout.
- Development is not scalable. A specific bacteriophage must be selected for each specific pathogenic bacteria, and a large phage collection must be maintained to identify the correct phage.
- Scientific and cultural bias. American researchers have tended to dismiss work coming out of Russia and Georgia, failing to recognize the rigor and effectiveness of decades of phage therapy practiced there. Limited scientific exchange was also a factor during the Cold War. A similar bias, for example, has influenced the adoption of psychological treatment strategies developed in Russia. In the U.S., the focus was more on using instrumental learning while neglecting the power of Pavlov’s classical condition.
These scientific prejudices, financial disincentives, and geopolitical divides have meant that phage therapy was almost totally absent in Western medicine although it continued in Eastern Europe, where it has saved countless lives. Phage therapy is currently becoming recognized and desperately needed because of the increase in multi-drug-resistant infections.
Phage treatment challenges
The greatest challenge with phage therapy is that it must be individualized to the pathogen. Each patient’s infection may require a different phage, because phages are exquisitely specific to the bacterium they target. A phage that destroys one strain of E. coli, for example, may have no effect on another subspecies of E. coli. While the same phage can sometimes be used for multiple patients with the same infection, in most cases treatment must be customized to the individual patient.
This requires maintaining vast phage libraries that researchers and clinicians must be able to screen rapidly in order to find the right match. The scale of this challenge is staggering, although AI technology may be part of the solution. Scientists estimate that there are 10³¹ (ten million trillion trillion) specific phages on Earth, making them the most abundant biological entities known. Only a tiny fraction of these have been studied, and only a relatively smaller number are currently catalogued for medical use.
Specialized research institutes, particularly in Georgia, Poland, and Russia (and now in the U.S. and Europe) have developed large collections of phages that can be tested against samples of specific bacterium. Building, maintaining, and updating these libraries is labor-intensive and requires constant monitoring, since both bacteria and phages evolve. Phage therapy does not lend itself easily to large-scale commercialization. Nevertheless, phage therapy represents one of the most promising approaches to resistant infections.
Summary
Unlike antibiotics, which disrupt the human microbiome and can cause significant side effects, phages are naturally occurring, highly targeted, and generally well tolerated. Because they attack only a specific bacterium, without disturbing beneficial microbes, phages have the potential to be used not only as a treatment but also for prevention, helping to control bacterial populations before they cause disease. Harnessing this form of living medicine could mark an evolutionary shift in modern healthcare, offering a sustainable, balanced way to prevent and treat infections. Read the outstanding book by Lina Zeldovich, The Living Medicine: How a lifesaving cure was nearly lost and why it will rescue us when antibiotics fail.
References
admin. (2025, August 28). Special Episode: Lina Zeldovich & The Living Medicine. This Podcast Will Kill You. Accessed September 1, 2025. https://thispodcastwillkillyou.com/2025/08/28/special-episode-lina-zeldovich-the-living-medicine/
CDC. (2019). Antibiotic Resistance Threats in the United States, 2019. Atlanta, GA: U.S. Department of Health and Human Services, CDC. https://www.cdc.gov/antimicrobial-resistance/media/pdfs/2019-ar-threats-report-508.pdf
CDC. (2025). Do antibiotics have side effects. Atlanta, GA: U.S. Department of Health and Human Services, CDC Accessed September 5, 2025. https://www.cdc.gov/antibiotic-use/media/pdfs/Do-Antibiotics-Have-Side-Effects-508.pdf
Cox, L.M. (2016). Antibiotics shape microbiota and weight gain across the animal kingdom, Animal Frontiers, 6(3), 8–14. https://doi.org/10.2527/af.2016-0028
Garnett, C. (2019). Personal quest resurrects phage therapy in infection fight. NIH Record, LXXI(6). https://nihrecord.nih.gov/2019/03/22/personal-quest-resurrects-phage-therapy-infection-fight
Murray, C. J. L. et al. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet, 399(103250, 629 – 655. https://doi.org/10.1016/S0140-6736(21)02724-0
Poku, E., Cooper, K., Cantrell, A., Harnan, S., Sin, M.A., Zanuzdana, A., & Hoffmann, A. (2023). Systematic review of time lag between antibiotic use and rise of resistant pathogens among hospitalized adults in Europe. JAC Antimicrob Resist, 5(1), dlad001. https://doi.org/10.1093/jacamr/dlad001
Spinillo, A., Capuzzo, E., Acciano, S., De Santolo, A., & Zara, F. (1999). Effect of antibiotic use on the prevalence of symptomatic vulvovaginal candidiasis. Am J Obstet Gynecol, 180(1 Pt 1),14-7. https://doi.org/10.1016/s0002-9378(99)70141-9
Zeldovich, L. (2024). The Living Medicine: How a lifesaving cure was nearly lost and why it will rescue us when antibiotics fail. New York: St. Martin’s Press. https://www.amazon.com/Living-Medicine-Lifesaving-Lost_and-Antibiotics/dp/1250283388
*Created in part from the information in the book, The Living Medicine-How a lifesaving cure was nearly lost-and why it will rescue Us When Antibiotics Fail, by Linda Zeldovich and with the editorial help of ChatGPT5.
Exploring the pain-brain-breathing connection
Posted: August 30, 2025 Filed under: attention, behavior, Breathing/respiration, cognitive behavior therapy, education, emotions, healing, meditation, Pain/discomfort, placebo, self-healing, Uncategorized | Tags: deliberate harm Leave a commentIf you’re curious about how the mind and body interplay in shaping pain—or looking for real, actionable techniques grounded in research listen to this episode of the Heart Rate Variability Podcast, Matt Bennett interviews Dr. Erik Peper about his article and blogpost Pain – There Is Hope. The conversation takes listeners beyond the common perception of pain as merely a physical response. It is a balanced mix of scientific depth and real-life applications, especially valuable for anyone interested in self-healing, holistic health, or understanding mind-body medicine. Moreover, it explains how pain is shaped by posture, breathing, mindset, and emotional context. Finally, it provides practical strategies to shift the pain experience, offering an uplifting and science-backed blend of understanding and hope.
If you find this helpful, let me know! And feel free to share it with friends and post it on your social channels so more people can benefit.
Blogs that complement this interview
If you want to explore further, check out the companion blog posts I hve created to expand on the themes from this discussion. These blogs highlight practical strategies, scientific insights, and everyday applications.
Healing from the Inside Out: How Your Mind–Body Shapes Pain
Posted: June 9, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, healing, health, mindfulness, Pain/discomfort, placebo, self-healing, Uncategorized | Tags: health, meditation, mental-health, mindfulness, Sufism, yoga 2 CommentsAdapted from Peper, E., Booiman, A. C., & Harvey, R. (2025). Pain-There is Hope. Biofeedback, 53(1), 1-9. http://doi.org/10.5298/1081-5937-53.01.16
Pain is more than a physical sensation—it’s shaped by our breath, thoughts, emotions, and beliefs. A striking example: a four-year-old received a vaccination with no pain, revealing the disconnect between what science knows about pain relief and what’s practiced.
The article highlights five key ways to reduce pain:
- Exhale during the painful moment – This activates the parasympathetic nervous system, calming the body. A yogi famously demonstrated this by pushing skewers through his tongue without bleeding or feeling pain.
- Create a sense of safety – Feeling secure can lessen pain and speed healing. Sufi mystics have shown this by pushing knives through their chest muscles without long-term damage, often healing rapidly.
- Distract the mind – Shifting focus can ease discomfort.
- Reduce anticipation – Fear of pain often amplifies it.
- Explore the personal meaning of pain – Understanding what pain symbolizes can shift how we experience it.
The blog also explores how the body regulates pain through mechanisms which influence inflammation and pain signals. In the end, hope, trust, and acceptance, along with mindful breathing, healing imagery, and meaningful engagement, emerge as powerful tools not just to reduce pain—but to promote true healing.
Listen to the AI generated podcast created from this article by Google NotebookLM
I took my four-year-old daughter to the pediatrician for a vaccination. As the nurse prepared to administer the shot in her upper arm. I instructed my daughter to exhale while breathing, understanding that this technique could influence her perception of pain. Despite my efforts, my daughter did not follow my instructions. At that point, the nurse interjected and said, “Please sit in front of your daughter.” Then turned to my daughter and said, “Do you see your father’s curly hair? Do you think you could blow the curls to move them back and forth?” My daughter thought this playful game was fun! As she blew at my hair, the curls moved back and forth while the nurse administered the injection. My daughter was unaware that she had received the shot and felt no pain.
My experience as a father and as a biofeedback practitioner was enlightening–it demonstrated the difference between theoretical knowledge of breathing techniques associated with pain perception and practical applications of clinical skills used by a pediatric nurse practitioner while administering an injection with children. An obvious question raised is: What processes are involved in the perception of pain?
There are many factors influencing pain perception, such as physical/physiological, behavioral and psychological/emotional factors related to the injection as described by St Clair-Jones et al., (2020). Physical and physiological considerations include device type such as needle gauge size as well as formulation volume and ingredients (e.g., adjuvants, pH, buffers), fluid viscosity, temperature, as well as possible sensitivity to coincidental exposures associated with an injection (e.g., sensitivity to latex exam gloves or some other irritant in the injection room).
There are overlapping physical and behavioral-related moderators that include weight and body fat composition, proclivity towards movements (e.g., activity level or ‘squirminess’), as well as co-morbid factors such as whether the person has body sensitization due to rheumatoid arthritis and/or fibromyalgia, for example. Other behavioral factors include a clinician selecting the injection site, along with the angle, speed or duration of injection. Psychological influences center around patient expectations including injection-anxiety or needle phobia, pain catastrophizing, as well as any nocebo effects such as white-coat hypertension.
Although the physical, behavioral and psychological categories allow for considering many physical and physiological factors (e.g., product-related factors), behavioral factors (e.g., injection-related behaviors) and psychological factors (e.g., person-related psychological attitudes, beliefs, cognitions and emotions), this article focuses on a figurative recipe for success associated with benefits of simple breathing to reduce pain perceptions.
Of the many categories of consideration related to pain perceptions, following are five key ‘recipe ingredients’ that contributed to a relatively painless experience:
- Exhaling During Painful Stimuli: Exhaling during a painful stimulus can activate parts of the parasympathetic nervous system leading to promotion of self-healing.
- Creating a Sense of Safety: Ensuring that the child feels safe and secure is crucial in managing pain. My lack of worry and concern and the nurse’s gentle and engaging approach created a comforting environment for my daughter.
- Using Distraction: Distraction techniques, such as focusing on the movement of the curls of the hair served to redirect my daughter’s attention away from the anticipated pain.
- Reducing Anticipation of Pain: My daughter’s previous visits were always enjoyable and as a parent, I was not anxious and was looking forward to the pediatrician visit and their helpful advice.
- Understanding the Personal Meaning of Pain: The approach taken by the nurse allowed the injection to be perceived as a non-event, thereby minimizing the psychological impact of the pain.
Exhaling During Painful Stimuli
Exhaling during painful stimuli facilitates a reduction in discomfort through several physiological mechanisms. During exhalation the parasympathetic nervous system is activated, which slows the heart rate and promotes relaxation, regeneration, reduces anxiety, and may counteract the effects of pain (Magnon et al., 2021). Breathing moderation of discomfort is observable through heart rate variability associated with slow, resonant breathing patterns, where heart rate increases with inhalation and decreases with exhalation (Lehrer & Gevirtz, 2014; Steffen et al., 2017). Physiological studies show that slow, resonant breathing at approximately six breaths per minute for adults, and a little faster for young children, causes the heart rate to increase during inhalation and decrease during exhalation, as illustrated in Figure 1.

Figure 1. Changes in heart rate as modulated by slower breathing at about six breaths per minute
One can experience how breathing affects discomfort when taking a cold shower under two conditions: As the cold water hits your skin: (1) gasping and holding your breath versus (2) exhaling slowly as the cold water hits you. Most people will report that slowly exhaling feels less uncomfortable, though they may still prefer a warm shower.
An Exercise for Use During Medical Procedures: Paring the procedure with inhalation and exhalation
A simple breathing technique can be used to reduce the experience of pain during a procedure or treatment, or during uncomfortable movement post-injury or post-surgery. Physiologically, inhalation tends to increase heart rate and sympathetic activation while exhalation reduces heart rate and increases parasympathetic activity. Often inhalation increases tension in the body, while during exhalation, one tends to relax and let go. The goal is to have the patient practice longer and slower breathing so that a procedure that might be uncomfortable is initiated during the exhalation phase. Applications of long, slow breathing techniques include having blood drawn, insertion of acupuncture needles in tender points, or movement that causes discomfort or pain. Slowly breathing is helpful in reducing many kinds of discomfort and pain perceptions (Joseph et al., 2022; Jafari et al., 2020).
Implementing the technique of exhaling during painful experiences can be deceptively simple yet challenging. When initially practicing this technique, the participants often try too hard by quickly inhaling and exhaling as the pain stimulus occurs. The effective technique involves allowing the abdomen to expand while inhaling, then allowing exhaled air to flow out while simultaneously relaxing the body and smiling slightly, and initiating the painful procedure only after about 25 percent of the air is exhaled.
Some physiological mechanisms that explain how slow breathing influences on pain perceptions have focused on baroreceptors that are mechanically sensitive to pressure and breathing dynamics. According to Suarez-Roca et al. (2021, p 29): “Several physiological factors moderate the magnitude and the direction of baroreceptor modulation of pain perception, including: (a) resting systolic and diastolic AP, (b) pain modality and dimension, (c) type of activated vagal afferent, and (d) the presence of a chronic pain condition It supports the parasympathetic activity that exert an anti-inflammatory influence, whereas the sympathetic activity is mostly pro-inflammatory. Although there are complex physiological interactions between cardiorespiratory systems, arterial pressure and baroreceptor sensitivity that influence pain perceptions, this report focuses on simpler reminders, such as creating a sense of safety for people as a result of better breathing techniques.
Creating a Sense of Safety
My young daughter did not know what to expect and totally trusted me and I was relaxed because the purpose was to enhance my daughter’s future health by giving her a vaccination to prevent being sick at a future time. Often, a parent’s anxiety is contagious to the child since expectations and emotional states influence the experience of medical procedures and pain (Sullivan et al., 2021). For my daughter, the nurse’s calm and confident demeanor contributed to a safe and reassuring environment. As a result, she was more engaged in a playful distraction, blowing at my hair, rather than focusing on the impending shot. This observation underscores an important psychological principle: when individuals do not anticipate pain and feel safe, they are more likely to experience surprise rather than distress. Conversely, anticipation of pain can amplify the perception of discomfort.
For instance, many people have experienced heightened anxiety at the dentist, where they may feel the pain of the needle before it is inserted. Anticipation evocates a past memory of pain that triggers a defensive reaction, increasing sympathetic arousal and sharpening awareness of potential danger. By providing the experience of feeling of safety, parents, caretakers, and medical professionals can play a crucial role in reducing the perceived pain of medical interventions.
Using Distraction
It is inherently difficult to attend to two tasks simultaneously; thus, focusing one’s attention on one task often diminishes awareness of pain and other stimuli (Rischer et al., 2020). For instance, when the nurse asked my daughter to see if she could blow hard enough to make the curls move back and forth, this task captured her attention in a fun and multisensory way. She was engaged visually by the movement of the curls, audibly by the sound of the rushing air, physically by the act of exhalation, and cognitively by following the instructions. Additionally, her success in moving the curls reinforced the activity as a positive and enjoyable experience.
In contrast, it is challenging to allow oneself to be distracted when anticipating discomfort, as numerous cues can continuously refocus attention on the procedure that may induce pain. This experience is akin to attempting to tickle oneself, which typically fails to elicit laughter due to the predictability and lack of external stimulation. Most of us have experienced how challenging it is to be self-directive and not focus on the sensations during dental procedures as discussed in the overview of music therapy for use in dentistry by Bradt and Teague (2018). The challenges are illustrated by my own experience during a dental cleaning
During a dental cleaning, I often attempt to distract myself by mentally visualizing the sensation of breathing down my legs while repeating an internal mantra or evoking joyful memories. Despite these efforts, I frequently find myself attending to the sound of the ultrasonic probe and the sensations in my mouth. To manage this distraction more effectively, I have found that external interventions such as listening to music or an engaging audio story through earphones is more beneficial.
From this perspective, we wished that the dentist could implement an external intervention by collaborating with a massage therapist to provide a simultaneous foot massage during the teeth cleaning. This dual stimulation would offer enough competing sensations to divert attention from the dental procedure to the comfort of the foot massage.
Reducing Anticipation of Pain
A crucial factor in the experience of pain is the anticipation and expectation of discomfort, which is often shaped by previous experiences (Henderson et al., 2020; Reicherts et al., 2017). When encountering a novel experience, we might interpret the sensations as novel rather than painful. Similar phenomena can be observed in young children when they fall or get hurt on the playground. They may initially react with surprise or shock and may look for their caretaker. Depending the reaction of their caregiver, they may begin to cry or they might cry briefly, stop and resume playing.
Conversely, the anticipation of pain can heighten sensitivity to any stimuli, causing them to be automatically perceived as painful. Anticipatory responses function as a form of mental rehearsal, where the body responds in a manner similar to the actual experience of pain. For example, Peper, et al. (2015) showed that when a pianist imagined playing the piano, her forearm flexor and extensor muscles exhibited slight contractions, even though there was no observable movement in her arm and the pianist was unaware of these contractions (see Figure 2).

Figure 2. The covert SEMG increase in forearm SEMG as the participant imagined playing the piano (reproduced by permission from Peper et al., 2015).
These kind of muscle reactions are also visible in sportsmen. For example, while mentally racing a lap on a motorbike, the arm muscles act like as if the person is racing in the dust of the circuit (Booiman 2018). The blood flow (BVP) and blood vessels are reacting even quicker than muscle tension on thoughts and expected (negative) experiences.
These findings underscore how anticipatory responses can mirror actual physical experiences, providing insights into how anticipation and expectancy can modify pain perception (Henderson et al., 2020). Understanding these mechanisms allows for the development of interventions aimed at managing pain through the modification of expectations and the introduction of distraction techniques.
The Personal Meaning of Pain (adapted from Peper, 2015)
The personal meaning of pain is a complex construct that varies significantly based on context and individual perception. For example, consider the case of a heart attack. Initially, the person might experience chest pain and dismiss it, which can be attributed to societal norms where people are conditioned to ignore pain. However, once the pain is assumed or diagnosed to be a heart attack, the same pain may become terrifying as it may signify the potential for life-threatening consequences. Following bypass surgery, the pain might actually be worse, but it is now reframed positively as a sign of the surgery’s success and a symbol of hope for survival. Thus, the meaning of pain evolves from one of fear to one of reassurance and recovery.
This notion that pain is defined by the context in which it occurs is crucial (Carlino et al., 2014). For instance, childbirth, despite being intensely painful, is understood within the context of a natural and temporary process that leads to the birth of a child. This perception is often reinforced nonverbally by a supportive midwife or doula. It may be helpful if the midwife or doula has given birth herself. Without words she communicates, “This is an experience that you can transcend, just as I did.” Psychologically/emotionally, the pain serves a higher purpose, to deliver a child into the world, which may also make the pain more bearable. There is a reward, namely the child. In addition, women who have had training and information about the process of childbirth have a significant faster delivery (about 2 hours faster).
Piercing the body without reporting pain or bleeding
To further illustrate this concept, Peper et al. (2006) and Kakigi et al. (2005) physiologically monitored the experiences of a Japanese Yogi Master, Mitsumasa Kawakami,who performed voluntary body piercing with unsterilized skewers, as depicted in Figure 3 (Peper, 2015).

Figure 3. Demonstration Japanese Yogi Master, Mitsumasa Kawakami, voluntary piercing the tongue and neck with unsterilized skewers while experiencing no pain, bleeding or infection (reproduced by permission from Peper et al., 2006).
See the video recording of tongue piercing study recorded November 11, 2000, at the annual Biofeedback Society Meeting of California, Monterey, CA, https://youtu.be/f7hafkUuoU4 (Peper & Gunkelman, 2007).
Despite the visual discomfort of seeing this procedure, physiological data from pulse, EEG and breathing patterns revealed that the yogi did not experience pain. During the piercing, his heart rate was elevated, his electrodermal activity was low and unresponsive, and his EEG showed predominant alpha waves, indicating a state of focused meditation rather than pain. This study suggests that conscious self-regulation, rather than dissociation, can be employed to control attention and responsiveness to painful stimuli and possibly benefit individuals with chronic pain (Peper et al., 2005).
A similar phenomenon was observed among a spiritual gathering of Kasnazani Sufi initiates in Amman, Jordan and physiologically monitored during demonstrations as part of a scientific meeting. The Kasnazani order is a branch of Sufism that has gained widespread popularity in Iraq and Iran, particularly among the Kurdish population. What sets the Kasnazani order apart is its inclusive approach—it welcomes both Sunni and Shia Muslims, making no distinction between them. During spiritual gatherings, some followers perform acts that might seem extreme to outsiders: piercing their bodies. These acts are seen as expressions of deep spiritual devotion and are performed in a state believed to be beyond normal physical sensation. With the permission of their Sheikh Mohammed Abdul Kareem Kasnazani, they pierced their face, neck arms, or chest and reported no pain or bleeding and heal quickly, as shown in Figure 4.

Figure 4. Voluntary piercing and with unsterilized skewers by Sufi initiates and subsequent tissue healing after 14 hours.
See the video recording of the actual piercing study organized by Erik Peper and Howard Hall with Thomas Collura recording the QEEG at the 2013 Annual Scientific Meeting of the Association for Applied Psychophysiology and Biofeedback, Portland, OR (Peper & Hall, 2013; Collura et al., 2014), https://www.youtube.com/watch?v=56nLZyG87oc
What Factors Decrease the Experience of Pain and Promote Rapid Healing with the Absence of Bleeding?
In the case of the Kasnazani Sufis, they framed their experience as a normal, spiritual phenomenon that occurs in a setting of religious faith and total trust in their spiritual leader (Hall, 2011). The Sufis reported that they had permission and support from their master, Sheikh Mohammed Abdul Kareem Kasnazani. Thus, they felt totally safe and protected—they had no doubt they could experience the piercing with reasonable composure and that their bodies would totally heal. Even if pain occurred, it was not to be feared but part of the process. The experience may be modulated by the psychological context of the group, the drumming, and the chanting. The phenomenon was not simply a matter of belief; they knew that healing would occur because they had seen it many times in the past. The knowledge that healing would occur rapidly was transmitted as a felt sense in the group that this is possible and following the expected normal pattern.
The most impressive finding was that the physiology markers (heart rate, skin conductance, and breathing) were normal and there was no notable change (Booiman et al., 2015; Peper & Hall, 2013) and the QEEG indicated the inhibition of pain (Collura et al., 2014).
Clinical implications
These observations underscore that the context of pain—whether through personal meaning, spiritual belief, or communal support—can significantly alter its perception and management. This concept is also reflected in clinical settings, where a lack of diagnosis or acknowledgment of pain can exacerbate suffering. An isolated individual, alone at night with the physical sensation of pain, may find the pain tremendously stressful, which tends to intensify the experience. In this situation, there are concerns about the future: “It may get worse, it will not go away, I’m going to die from this, maybe I’ll die alone,” and the worry continues.
If one can let go of these thoughts, breathe through the pain, relax the muscles and experience a feeling of hope, the pain is often reduced. On the other hand, focusing on the pain may intensify it. On the other hand, the meaning of pain implies survival or hope as sometimes is observed in injured soldiers. In context of the hospital setting: “I have survived and I am safe.”
What are the implications of these experiences in clinical settings in which the patient is in constant pain and yet has not received an accurate diagnosis? Or, in cases in which the patient has a diagnosis, such as fibromyalgia, but treatment has not reduced the pain significantly? Experiencing pain or illness that goes undiagnosed, and/or that is not acknowledged, may increase the level of stress and tension, which can contribute to more pain and discomfort. As long as we are resentful/angry/resigned to the pain or especially to the event that we believe has caused the pain, the pain often increases. Another way to phrase this is that chronic sympathetic arousal increases the sensitivity to pain and reduces healing potential (Kyle & McNeil, 2014).
Acknowledgement means having an accurate diagnosis, validating that the pain experience is legitimate and that it is not psychosomatic (imagined), because that simply makes the experience of pain worse. Once the patient has a more accurate diagnosis, treatment may be possible.
When one has constant, chronic, or unrelenting pain, this evokes hopelessness and the patient is more likely to get depressed (Sheng et al., 2017; Meda et al., 2022). The question is, What can be done? The first step for the patients is to acknowledge to themselves that it does not mean that the situation is unsolvable. It is important to focus on other options for diagnosis and treatment and take one’s own lead in the healing/recovery process. We have observed that a creative activity that uses the signals of pain to evoke images and thoughts to promote healing may reduce pain (Peper et al., 2022). Pain awareness may be reduced when the person initiates actions that contribute to improving the well-being of others.
Overall, pain appears to decrease when a person accepts without resignation what has happened or is happening. A useful practice that may change the pain experience is to do an appreciation practice. Namely, appreciate what that part of the body has done for you and how so often in the past you may have abused it. For example, if you experience hip pain, each time you are aware of the pain, thank the hip for all the work it has done for you in the past and how often you may have neglected it. Keep thanking it for how it has supported you.
Pain often increases when the person is resentful or wished that what has happened had not happened (Burns et al., 2011). If the person can accept where they are and focus on the new opportunities and new goals can achieve, pain may still occur; however, the quality is different. Focus on what you can do and not on what you cannot do. See Janine Shepherd’s 2012 empowering TED talk, “A broken body isn’t a broken person.”
Conclusion
The primary lessons from studying the yogi and the Sufis are the concepts that a sense of safety, acceptance, and purpose can transform the experience of pain. Expressing confidence in a patient’s recovery prospects places the focus on their ability to recover. Incorporating these elements into clinical care may offer new avenues for addressing chronic pain and improving patient outcomes (Booiman & Peper, 2021).
We propose the first step is to create an atmosphere of hope, trust and safety and to emphasize the improvements made (even small ones). Then master effortless breathing to increase slow diaphragmatic breathing and teach clients somato-cognitive techniques to refocus their attention during painful stimuli (mindfulness) (Pelletier & Peper, 1977; Peper et al., 2022). Using the slow breathing as the overlearned response would facilitate the recovery and regeneration following the painful situation. To develop mastery and be able to apply it under stressful situations requires training and over-learning. Yoga masters overlearned these skills with many years of meditation. With mastery, patients may learn to abort the escalating cycle of pain, worry, exhaustion, more pain, and hopelessness by shifting their attention and psychophysiological responses. In clinical practice, strategies such as hypnotic induction, multisensory distraction, self-healing visualizations, and mindfulness techniques can be employed to manage pain. A foundational principle is that healing is promoted when the participant feels safe and accepted, experiences suffering without blame, and looks forward to life with meaning and purpose.
Acknowledgement
We thank Mitsumasa Kawakami, Sheikh Mohammed Abdul Kareem Kasnazani, and Safaa Saleh for their generous participation in this research and I thank our research collegues Thomas Collura, Howard Hall and Jay Gunkelman for their support and collaboration.
References
Booiman, A.C. (2018) Posture corrections and muscle control can prevent arm pump during motocross, a case study. Beweegreden, 14(3), 24–27. https://www.researchgate.net/publication/382853342
Booiman, A. C. & Peper, E. (2021) De pijnbeleving van Kaznazanisoefi’s, wat kan de fysiotherapeut daarvan leren? Physios Vol 13 (3) pp. 32–35. https://www.physios.nl/tijdschrift/editie/artikel/t/de-pijnbeleving-van-kaznazani-soefi-s-wat-kan-de-fysiotherapeut-daarvan-leren
Booiman, A., Peper, E., Saleh, S., Collura, T., & Hall, H. (2015). Soefi piercing een andere kijk op pijnervaring en pijnmanagement. https://biofeedbackhealth.files.wordpress.com/2011/01/soefi-en-pijn-management-08-12-20131.pdf
Bradt. J. & Teague, A. (2018). Music interventions for dental anxiety. Oral Diseases, 24(3), 300–306. https://doi.org/10.1111/odi.12615
Burns, J.W., Quartana, P., & Bruehl, S. (2011). Anger suppression and subsequent pain behaviors among chronic low back pain patients: moderating effects of anger regulation style. Annals of Behavioral Medicine, 42(1), 42–54. https://doi.org/10.1007/s12160-011-9270-4
Carlino, E., Frisaldi, E., & Benedetti, F. (2014). Pain and the context. Nature Reviews Rheumatology, 10(6), 348–355. https://doi.org/10.1038/nrrheum.2014.17
Collura, T. F., Hall, H., & Peper, E. (2014). A Sufi self-piercing analyzed with EEG and sLORETA. Applied Psychophysiology and Biofeedback, 39(3–4), 293–293. https://brainmaster.com/wp-content/uploads/2020/08/AAPB_BOS05_2015_Pain_Controll.pdf
Hall, H. (2011). Sufism and healing. In Neuroscience, Consciousness and Spirituality (pp. 263–278). Springer Netherlands. https://doi.org/10.1007/978-94-007-2079-4_16
Henderson, L. A., Di Pietro, F., Youseff, A. M. , Lee, S., Tam, S., Akhter, R., Mills, E.P., Murray, G. M., Peck, C.C., & Macey, P.M. (2020). Effect of expectation on pain processing: A psychophysics and functional MRI analysis. Frontiers in Neuroscience, 14. https://doi.org/10.3389/fnins.2020.00006
Jafari, H., Gholamrezaei, A., Franssen, M., Van Oudenhove, L., Aziz, Q., Van den Bergh, O., Vlaeyen, J. W. S., & Van Diest, I. (2020). The Journal of Pain, 21(9–10), 1018−1030. https://doi.org/10.1016/j.jpain.2019.12.010
Joseph, A. E., Moman, R. N., Barman, R. A., Kleppel, D. J., Eberhart, N. D., Gerberi, D. J., Murad, M. H., & Hooten, W. M. (2022). Effects of slow deep breathing on acute clinical pain in adults: A systematic review and meta-analysis of randomized controlled trials. Journal of Evidence-Based Integrative Medicine, 27, 2515690X221078006. https://doi.org/10.1177/2515690X221078006
Kakigi, R. Nakata, H., Inui, K., Hiroe,N. Nagata, O., Honda, M., Tanaka, S., Sadato, N. & Kawakami, M. (2005). Intracerebral pain processing in a Yoga Master who claims not to feel pain during meditation. European Journal of Pain. 9(5), 581–581. https://doi.org/10.1016/j.ejpain.2004.12.006
Kyle, B. N., & McNeil, D. W. (2014). Autonomic arousal and experimentally induced pain: a critical review of the literature. Pain Research Management, 19(3),159–167. https://doi.org/10.1155/2014/536859
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Magnon, V., Dutheil, F. & Vallet, G. T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11, 19267. https://doi.org/10.1038/s41598-021-98736-9
Meda, R. T., Nuguru, S .P., Rachakonda, S., Sripathi, S., Khan, M. I., & Patel, N. (2022). Chronic paininduced depression: A review of prevalence and management. Cureus,14(8):e28416. https://doi.org/10.7759/cureus.28416
Pelletier, K. R. and Peper, E. (1977). Developing a biofeedback model: Alpha EEG as a means for pain control. International Journal of Clinical and Experimental Hypnosis, 24(4), 361–371. https://doi.org/10.1080/00207147708415991
Peper, E. (2015). Pain as a contextual experience. Townsend Letter—The Examiner of Alternative Medicine, 388, 63–66. https://www.researchgate.net/profile/Erik-Peper/publication/284721706_Pain_as_a_contextual_experience/links/5657483908ae1ef9297bab71/Pain-as-a-contextual-experience.pdf
Peper, E., Cosby, J., & Almendras, M. (2022). Healing chronic back pain. NeuroRegulation, 9(3), 164–172. https://doi.org/10.15540/nr.9.3.164
Peper, E. & Gunkelman, J. (2007). Tongue piercing by a yogi: QEEG observations and implications for pain control and health. Presented at the 2007 meeting of the Biofeedback Society of California. https://www.researchgate.net/publication/382394304_Tongue_Piercing_by_a_Yogi_QEEG_Observations_and_Implications_for_Pain_Control_and_Health
Peper, E. & Hall, H. (2013). What is possible: A discussion, physiological recording and actual demonstration in voluntary pain control by Kasnazani Sufis. Presented at the 44st Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Portland, OR.
Peper, E., Kawakami, M., Sata, M. & Wilson, V.S. (2005). The physiological correlates of body piercing by a yoga master: Control of pain and bleeding. Subtle Energies & Energy Medicine Journal, 14(3), 223–237. https://biofeedbackhealth.org/wp-content/uploads/2011/01/366-663-1-sm.pdf
Peper, E., Nemoto, S., Lin, I-M., & Harvey, R. (2015). Seeing is believing: Biofeedback a tool to enhance motivation for cognitive therapy. Biofeedback, 43(4), 168–172. https://doi.org/10.5298/1081-5937-43.4.03
Peper, E., Wilson, V.E., Gunkelman, J., Kawakami, M. Sata, M., Barton, W. & Johnston, J. (2006). Tongue piercing by a yogi: QEEG observations. Applied Psychophysiology and Biofeedback. 34(4), 331–338. https://doi.org/10.1007/s10484-006-9025-3
Reicherts, P., Wiemer, J., Gerdes, A.B.M., Schulz, S.M., Pauli, P., & Wieser, M.J. (2017). Anxious anticipation and pain: The influence of instructed vs conditioned threat on pain. Social Cognitive and Affective Neuroscience, 12(4), 544–554. https://doi.org/10.1093/scan/nsw181
Rischer, K. M., González-Roldán, A. M., Montoya, P., Gigl, S., Anton, F., & van der Meulen, M. (2020). Distraction from pain: The role of selective attention and pain catastrophizing. European Journal of Pain, 24(10),1880–1891. https://doi.org/10.1002/ejp.1634
Sheng, J., Liu, S., Wang, Y., Cui, R., & Zhang, X. (2017). The link between depression and chronic pain: Neural mechanisms in the brain. Neural Plasticity, 9724371. https://doi.org/10.1155/2017/9724371
Shepherd, J. (2012). A broken body isn’t a broken person. TEDxKC. Accessed July 19, 2024. https://www.ted.com/talks/janine_shepherd_a_broken_body_isn_t_a_broken_person?subtitle=en
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The impact of resonance frequency breathing on measures of heart rate variability, blood pressure, and mood. Frontiers in Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
St Clair-Jones, A., Prignano, F., Goncalves, J., Paul, M., & Sewerin, P. (2020). Understanding and minimising injection-site pain following subcutaneous administration of biologics: A narrative review. Rheumatology and therapy, 7, 741–757. https://doi.org/10.6084/m9.figshare.13034609
Suarez-Roca, H., Mamoun, N., Sigurdson, M. I., & Maixner, W. (2021). Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Comprehensive Physiology, 11(2), 1373. https://doi.org/10.1002/cphy.c190038
Sullivan, V., Sullivan, D. H. & Weatherspoon, D. (2021). Parental and child anxiety perioperatively: Relationship, repercussions, and recommendations. Journal of PeriAnesthesia Nursing, 36(3), 305–309. https://doi.org/10.1016/j.jopan.2020.08.015
Wilber, K. (1997). An integral theory of consciousness. Journal of Consciousness Studies, 4(1), 71–92. https://www.ingentaconnect.com/content/imp/jcs/1997/00000004/00000001/748
The Power of No
Posted: March 6, 2025 Filed under: behavior, Breathing/respiration, CBT, cognitive behavior therapy, emotions, healing, health, self-healing, stress management, Uncategorized | Tags: assertiveness, emotional awareness, HIV, immune resilence, surviaval 1 CommentBrenda Stockdale, PhD and Erik Peper, PhD
Adapted from: Stockdale, B. & Peper, E. (2025). How the Power of No Supports Health and Healing. Townsend Letter-Innovative Health Perspectives, March15, 2025 https://townsendletter.com/the-power-of-no/

I felt exhausted and just wanted to withdraw to recharge. Just then, my partner asked me to go to the store to get some olive oil. I paused, took a deep breath, and checked in with myself. I realized that I needed to take care of myself. After a few seconds, I responded, “No, I cannot do it at this time.”
It was challenging to say this because, in the past, I would have automatically said “yes” to avoid disappointing my partner. However, by saying “yes” and ignoring my own needs, I would have become even more exhausted, hindering my recovery. I felt proud that I had said “no.” By listening to myself, I took charge and prioritized my own healing.
For many people, saying “no” feels unkind, and we want to be kind while avoiding burdening others. Nevertheless, how you answer this question may have implications for your health! Consider the following question and rate it on a scale from 1 (never) to 5 (always):
How often do you do favors for people when you really don’t want to? Namely, things you really don’t want to do but do anyway because someone asks you to and you don’t want to or can’t say “No.“
In analysis of numerous studies, Prof. George Solomon and Dr. Lydia Temoshok reported that a low score on this question (indicating the ability to say No) was the best predictor of related outcomes across studies, such as survivorship with AIDS as well as more favorable HIV immune measures (Solomon, et al, 1987). This aligns with research suggesting that excessive compliance, self-sacrifice, and conflict avoidance (i.e., people-pleasing) in individuals with cancer and chronic illness may weaken, rather than strengthen, their immune systems (Temoshok, & Dreher, 1992).
Unconsciously avoiding or suppressing distressing thoughts, emotions, or memories instead of dealing with them––a process known as repressive coping–– may even contribute to an increased risk of cancer and cardiovascular disease (Mund & Mitte, 2012). Avoiding emotional cues or dismissing feelings may seem self-protective but can lead to reflexive or automatic behavior such as saying “yes” when individuals would rather say “no.” Although the conflict may not be consciously recognized, it can manifest physiologically (Mund & Mitte, 2012). Paying attention to states of tension, or symptoms such as headache or loss of appetite can serve as a doorway to exploring unacknowledged feelings.
Automatically saying “yes” and sacrificing yourself may contribute to poor boundaries, leading to chronic stress which is linked to numerous health issues, including hypertension and immune dysfunction (Dai et al., 2020; Segerstrom et al., 2004; Deci & Ryan, 2008). Conversely, research indicates that individuals who assertively manage stress—rather than suppress emotions and avoid conflict—demonstrate stronger immune resilience (Ironson et al., 2005; Dantzer et al, 2018) and are better protected against burnout and prolonged emotional distress (Deci & Ryan, 2018).
When faced with illness––or even the possibly death––ask yourself: “Do I really want to do this, or am I doing it just to please my partner, children, parents, doctors, or society? By doing what truly brings me joy and meaning, what do I have to lose?” Altruism is valuable and an important part of maintaining health. At the same time boundaries and assertiveness are essential.
Psychologist Lawrence LeShan (1994) reported that when cancer patients began to seek and start singing their “own song,” their cancer regressed in numerous cases, and some experienced total remission. Living your own song means doing what you truly desire rather than following the expectations of parents, society, or economic pressures. It is important to keep in mind that while psychological factors can influence overall health, the development of cancer is a multifaceted process involving genetic, lifestyle and environmental factors.
The Key Question: When and How to Say “No”?
The answer lies in emotional awareness and acting on it. One woman with cancer confided, “I’ve operated in the realm of expected behavior for so long that I no longer know what I want or feel” (Stockdale, 2009). Teasing out our true feelings—hour by hour, as Bernie Siegel, M.D., recommends—helps us recognize where we stand (Siegel, 1986; Siegel & August, 2004). This practice fosters a sense of agency, a cornerstone of resilience that directly contributes to well-being.
For those accustomed to prioritizing others’ needs over their own, learning to say “No” takes practice. Although one may have feelings of vulnerability and even guilt by disappointing someone, one person shared that only after he stopped exclusively prioritizing others–and instead learned to love himself as well as his neighbor–did he realize how much people genuinely cared for him. Authentic connection is essential for well-being, but trust cannot develop without agency and the freedom to say “no.”
What to Do Before Automatically Saying Yes
When someone asks you for help or a favor, pause. Look up, take a slow, diaphragmatic breath, and ask yourself, “Do I want to do this? What would I recommend to another person to do in this situation?”
(In cases where you are asked or ordered to harm another person or do something illegally, ask yourself, “What would a moral person do?”)
If you feel that you would rather not—whether because you are tired or it interferes with your own priorities—say “No.” Saying “No” does not mean you are unwilling to help; it simply means that, at this moment, you are listening to yourself. When we listen to ourselves and act accordingly, we enhance our immune competence and self-healing.
Obviously, if saying “No” would put another person in danger or in crisis, then say “Yes,” if possible. However, true crises are rare. If emergencies happen frequently, they are not true crises or emergencies but rather a result of poor planning.
Saying “No” can be challenging, but if you constantly say “Yes,” you may eventually become resentful and exhausted, increasing your stress and decreasing your ability to heal. You may even notice that when your own well-being is appropriately prioritized you will be in a better position to show up for others in a whole-hearted way, when it is right for them and for you.
Saying “No” Can Be Life-Saving
Beyond personal relationships, saying “No” can be crucial in medical settings. Anthony Kaveh, M.D., a Stanford- and Harvard-trained anesthesiologist and integrative medicine specialist, asserts, “Nice patients come out last” (Kaveh, 2024). Kaveh emphasizes that trusting our instincts is crucial, as the fear of displeasing others can lead to dangerous “fake nice” behavior.
See the YouTube video #1 Mistake You Make with Doctors: Medical Secrets (https://www.youtube.com/watch?v=9-E3CHHX05c)
A case example is illustrated by Tracy who was hospitalized with complex fractures of the tibia and fibula. After five surgeries, she felt something was terribly wrong–she knew she was dying. However, the nurses dismissed her concerns. Taking control, she infuriated the staff by calling 911, which prompted a doctor to check on her. It was discovered that excessive negative pressure applied to the drain caused five pints of her blood to flow into her leg causing compartment syndrome.
She was bleeding to death. Tracy’s intuition, resilience, and refusal to comply saved her life. Kaveh argues that those who don’t trust their instincts are more likely to err on the side of “nice” and suffer as a result.
Learning to say “No” is empowering as illustrated by one woman who discovered its importance in a cancer educational group she attended. She shared her success in saying “No” with humor, explaining, “I just tell people it’s this group’s fault because I used to be a nice person.”
Learning to listen to yourself before agreeing or disagreeing to do something, may also help you maintain your integrity when faced with pressure to follow an immoral suggestion or order. So often due to social, economic, corporate, or political pressure, people may be asked to do something they later regret (Sah, 2025). The courage to disagree and act according to your moral consciousness is the bases of the Nuremberg Code, established by the American judges in 1947 at the Nuremberg trials for Nazi doctors (Shuster, 1997).
Finally, learning to say “No” and listen to your needs takes practice and time. Explore the following Body Dialogue technique to tap into your intuitive wisdom. You can use it anytime you need clarity about your feelings and responses to life’s challenges.
Breathe in deeply and engage all your senses. When you are ready, focus on the sensation of breathing. You don’t have to make anything happen, just feel the air moving in and out. Your lungs, vital to energy production, obtain oxygen from the atmosphere and bring it to millions of specialized cells. All without your conscious awareness, your breath moves in and out, removing toxins and waste from your body and bringing oxygen in.
The beautiful filtering process even protects your heart. That great organ, pumping rhythmically, picks up the oxygen and delivers it to all the vessels of your body, contracting more than two billion times during a normal lifespan. With deep appreciation for this magnificent pump, move your attention down into your abdomen. On the right side is the largest organ in your body, your liver. This amazing organ filters toxins and chemicals, and aids in digestion. This powerhouse of function can even regenerate itself after losing as much as three quarters of its tissue. With a sense of admiration, imagine all that these great and vital organs accomplish. With gratitude, slowly move on to your spleen, your pancreas and all the other organs and systems of your body, taking your time to appreciate and acknowledge all that they do for you.
Consider the multitude of vital functions that take place every minute of every day and thank your body for all that is right with you. All of these complex functions take place without effort or even awareness on your behalf––they just happen. Ask now if there something you can do for your body to help it heal, repair or regenerate more completely. Listen closely to your own intuitive awareness. Is there anything you can do to make your body’s job easier or reduce a burden of some kind? Gently notice if there are any thoughts or behaviors that make some symptoms worse or better. What feels heavy or burdensome? Who or what in your life feels supportive? As you review the past few days or weeks what would you like to adjust? When might saying ‘no’ would bring a sense of relief? Imagine what it would be like to operate in your own best interest. What might that include?
Are there positive feelings you would like to experience more often? If you had to choose just one, what would it be? In what way could you bring more of that quality into your life? In your mind’s eye, see that happening now. Feel the peace or the joy or whatever it is you have chosen radiate throughout your being. And if it seems good to you, carry it with you, back to the present moment and enjoy the fullness of that sensation. When it seems right to you, again focus gently on your body, bringing your attention back to the chair or the place you happen to be. And filled with gratitude, stretch your arms wide with appreciation for all that is right with you.
Additional useful blogs
References
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., Li, X., Li, Y., Xiong, W., Li, G., Guo, C., & Zeng, Z. (2020). Chronic Stress Promotes Cancer Development. Frontiers in oncology, 10, 1492. https://doi.org/10.3389/fonc.2020.01492
Dantzer, R., Cohen, S., Russo, S. J., & Dinan, T. G. (2018). Resilience and immunity. Brain, behavior, and immunity, 74, 28–42. https://doi.org/10.1016/j.bbi.2018.08.010
Deci, E. L., & Ryan, R. M. (2008). Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology / Psychologie canadienne, 49(3), 182–185. https://doi.org/10.1037/a0012801
Deci, E. L., & Ryan, R. M. (2018). Self-determination theory: Basic psychological needs in motivation, development, and wellness. New York: Guilford Publications. https://www.amazon.com/Self-Determination-Theory-Psychological-Motivation-Development/dp/1462538967
Ironson, G., O’Cleirigh, C., Fletcher, M. A., Laurenceau, J. P., Balbin, E., Klimas, N., Schneiderman, N., & Solomon, G. (2005). Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosomatic medicine, 67(6), 1013–1021. https://doi.org/10.1097/01.psy.0000188569.58998.c8
Kaveh, A. (2024). #1 Mistake You Make With Doctors. Medical Secrets, YouTube, https://www.youtube.com/watch?v=9-E3CHHX05c
LeShan, L. (1994). Cancer As a Turning Point: A Handbook for People with Cancer, Their Families, and Health Professionals – Revised Edition. New York: Penguin Publishing Group. https://www.amazon.com/Cancer-As-Turning-Point-Professionals/dp/0452271371
Mund, M., & Mitte, K. (2012). The costs of repression: a meta-analysis on the relation between repressive coping and somatic diseases. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 31(5), 640–649. https://doi.org/10.1037/a0026257
Sah, S. (2025. Defy: The power of no in a world that demands yes. London: One World Publications. https://www.amazon.com/Defy-Power-World-That-Demands/dp/0593445775
Shuster, E. (1997). Fifty years later: The significance of the Nuremberg code. The New England Journal of Medicine, 337(20), 1436-1440. https://doi.org/10.1056/NEJM199711133372006
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological bulletin, 130(4), 601–630. https://doi.org/10.1037/0033-2909.130.4.601
Siegel, B. (1986). Love, medicine & miracles. New York: William Morrow Paperbacks; https://www.amazon.com/Love-Medicine-Miracles-Bernie-Siegel-dp-B00A2KKOBI
Siegel, B. & August, Y. (2004). Help Me Heal. Hay House. https://www.amazon.com/Help-Heal-Bernie-Siegel-M-D/dp/1401900607/
Solomon, G. F., Temoshok, L., O’Leary, A., & Zich, J. (1987). An intensive psychoimmunologic study of long-surviving persons with AIDS. Pilot work, background studies, hypotheses, and methods. Annals of the New York Academy of Sciences, 496, 647–655. https://doi.org/10.1111/j.1749-6632.1987.tb35825.x
Stockdale, B. (2009). You can beat the odds: Surprising factors behind chronic illness and cancer––the 6-week program for Optimal Immunity. Boulder, CO: Sentient Publications. https://www.amazon.com/You-Can-Beat-Odds-Surprising-ebook/dp/B00KMDKOVA
Temoshok L. (1987). Personality, coping style, emotion and cancer: towards an integrative model. Cancer surveys, 6(3), 545–567. https://pubmed.ncbi.nlm.nih.gov/3326661/
Temoshok, L., & Dreher, H. (1992). The type C connection: The behavioral links to cancer and immune dysfunction. New York: Random House. https://www.amazon.com/Type-Connection-Behavioral-Cancer-Health/dp/0394575237
Implement your New Year’s resolution successfully[1]
Posted: December 29, 2024 Filed under: attention, behavior, CBT, cognitive behavior therapy, education, emotions, Exercise/movement, healing, health, self-healing | Tags: goal setting, health, lifestyle, motivation, performance, personal-development Leave a comment
Adapted from: Peper, E. Pragmatic suggestions to implement behavior change. Biofeedback.53(2), 41-45. https://doi.org/10.5298/1081-5937-53.02.05
Ready to crush your New Year’s resolutions and actually stick to them this time? Whether you’re determined to quit vaping or smoking, cut back on sugar and processed foods, reduce screen time, get moving, volunteer more, or land that dream job, sticking to your goals is the real challenge. We’ve all been there: kicking off the year with ambitious plans like, “I’ll work out every day,” or “I’m done with junk food for good.” But a few weeks in? The gym is a distant memory, the junk food stash is back, and those cigarettes are harder to let go of than expected.
So, how can you make this year different? Here are some tried-and-true tips to help you turn those resolutions into lasting habits:
Be clear of your goal and state exactly what you want to do (Pilcher et al., 2022; Latham & Locke, 2006).
Did you know your brain is super literal and doesn’t process “not” the way you think it does? For example, if you say, “I will not smoke,” your brain has to first imagine you smoking, then mentally cross it out. Guess what? By rehearsing the act of smoking in your mind, you’re actually increasing the chances that you’ll light up again.
Think of it like this: hand a four-year-old a cup of hot chocolate and ask them to walk it over to someone across the room. Halfway there, you call out, “Be careful, don’t spill it!” What usually happens? Yep, the hot chocolate spills. That’s because the brain focuses on “spill,” not the “don’t.” Now, imagine instead you say, “You’re doing great! Keep walking steadily.” Positive framing reinforces the action you want to see. The lesson is to reframe your goals in a way that focuses on what you want to achieve, not what you’re trying to avoid. Let’s look at some examples to get you started:
| Negative framing | Positive framing |
| I plan to stop smoking | I choose to become a nonsmoker |
| I will eat less sugar and ultra-processed foods | I will shop at the farmer’s market, buy more fresh vegetable and prepare my own food. |
| I will reduce my negative thinking (e.g., the glass is half empty). | I will describe events and thoughts positively (e.g., the class is half full). |
Describe what you want to do positively.
Be precise and concrete.
The more specific you can describe what you plan to do, the more likely will it occur as illustrated in the following examples.
| Imprecise | Concrete and specific |
| I will begin exercising. | I will buy the gym membership next week Monday and will go to the gym on Monday, Wednesday and Friday right after work at 5:30pm for 45 minutes. |
| I will reduce my angry outbursts, | Before I respond, I will take a slow breath, look up, relax my shoulders and remind myself that the other person is doing their best. |
| I want to limit watching streaming videos | At home, I will move the couch so that it does not face the large TV screen, and I have enrolled in a class to learn another language and I will spent 30 minutes in the evening practicing the new language. |
| I will stop smoking | When I feel the initial urge to smoke, I stand up, do a few stretches, and practice box breathing and remind myself that I am a nonsmoker. |
Describe in detail what you will do.
Identify the benefits of the old behavior that you want to change and how you can achieve the same benefits with your new behavior. (Peper et al, 2002)
When setting a New Year’s resolution, it’s easy to focus on the perks of the new behavior and the harms of the old behavior while overlooking the benefits your old habit provided. However, if you don’t plan ways to achieve the same benefits, the old behavior provided, it’s much harder to stick to your goal.
Before diving into your new resolution, take a moment to reflect. What did your old behavior do for you? What needs did it meet? Once you identify those, you can develop strategies to achieve the same benefits in healthier, more constructive ways.
For example, let’s say your goal is to stop smoking. Smoking might have helped you relax during stressful moments or provided a social activity with friends. To make the switch, you’ll need to find alternatives that deliver similar results, like practicing deep-breathing exercises to manage stress or inviting friends for a walk instead of a smoke break. By creating a plan to meet those needs, you’ll set yourself up for lasting success.
| Benefits of smoking | How to achieve the same benefits when being a none smoker |
| Stress reduction | I will learn relaxation and diaphragmatic breathing. The moment, I feel the urge to smoke, I sit up, look up, raise my shoulder and dropped them, and breathe slowly |
| Breaks during work | I will install a reminder on my cellphone to ping and each time it pings, I stop, stand up, walk around and stretch. |
| Meeting with friends | I will tell my friends, not to offer me a cigarette and I will spent time with friends who are non-smokers. |
| Rebelling against my parents who were opposed to smoking | I will explore how to be independent without smoking |
Describe your benefits and how you will achieve them.
Reduce the cues that evoke the old behavior and create new cues that will trigger the new behavior (Peper & Wilson, 2021).
A lot of our behavior is automatic—shaped by classical conditioning, just like Pavlov’s dog. Remember the famous experiment? Pavlov paired the sound of a bell with food, and after a while, the bell alone made the dog salivate (McLeod, 2024). We’re not so different.
Think about it: if you’ve gotten into the habit of smoking in your car, simply sitting in the driver’s seat can trigger the automatic urge to grab a cigarette. Or, if you tend to feel depressed when you’re home but better when you’re out with friends, your home environment might be acting as a cue for those feelings.
Interestingly, many people find it easier to change habits in a new environment. Why? Because there are no built-in triggers to reinforce the behavior they’re trying to change. This highlights how much of what we often call “addiction” might actually be conditioned behavior, reinforced by familiar cues in our surroundings. By recognizing the power of these triggers can help you disrupt old patterns. By creating a fresh environment or consciously changing your responses to cues, you can take control and start forming new, healthier habits.
This concept has been understood for centuries by some hunting and gathering societies. When something tragic happened—like the death of a family member in a hut—the community would often burn the hut to “eliminate the evil spirit.” Beyond the spiritual aspect, this practice served a practical purpose: it removed all the physical cues that reminded people of their loss, making it easier to focus on the present and move forward.
Of course, I’m not suggesting you destroy your home. But the underlying principle still holds true in modern times. In fact, many Northern European cultures incorporate a version of this idea through the ritual of Spring Cleaning. By decluttering, rearranging furniture, and refreshing the home, the old cues are removed and create a sense of renewal.
So often we forget that cues in our environment play a powerful role in triggering our behavior. By identifying the triggers that evoke old habits and finding ways to remove or change them, you can create a fresh environment that supports your goals. For example, if you’re trying to stop snacking on junk food late at night, consider rearranging your pantry so the tempting items are out of sight—or better yet, replace them with healthier options. Small changes like this can have a big impact on your ability to stay on track.
| Cues that triggered the behavior | How cues were changed |
| In the evening going to the kitchen and getting the chocolate from the cupboard. | Buying fruits and have them on the table and not buying chocolate. If I do buy chocolate store it on the top shelf away so that I do not see it or store it in the freezer. |
| Getting home and being depressed. | Clean the house, change the furniture around and put positive picture high up on the wall. |
| Smoking in the car. | Replace the car with another car that no one had smoked in and spray the care with pine scent. |
Identify the cues that trigger your behavior and how you changed them.
Identify the first sensation that triggered the behavior you would like to change.
Whether it’s smoking, drinking, scratching your skin, spiraling into negative thoughts, or eating too many pastries, once a behavior starts, it can feel nearly impossible to stop. That’s why the key is to catch yourself before the habit takes over., t’s much easier to interrupt a pattern at the very first sign—the initial trigger—rather than after you’ve fully dived into the behavior. Yet how often do we find ourselves saying, “Next time, I’ll do it differently”?
Here’s the strategy: identify the first trigger. This could be a physical sensation, an emotion, a thought, or an external cue. Once you’re aware of that first flicker of a trigger, redirect your thoughts and actions toward what you actually want, rather than letting the automatic behavior take control. For example:
I just came home at 10:15 PM and felt lonely and slightly depressed. I walked into the kitchen, opened the fridge, grabbed a beer, and drank it. Then, I reached for another bottle.
Observing this behavior, the first trigger was the loneliness and slight depression upon arriving home. Recognizing that feeling in the moment offers an opportunity to pause and make a conscious choice. Instead of heading to the fridge, you could redirect your actions—call a friend, go for a quick walk, or write down your thoughts in a journal. By catching that initial trigger, you can focus yourself toward healthier behaviors and break the cycle.
| First sensation | Changed response to the sensation |
| I observed that the first sensation was feeling tired and lonely. | When I entered the house, instead of going to the kitchen, I stretched, looked up and took a deep breath and then called a close friend of mine. We talked for ten minutes and then I went to bed. |
Identify your first sensation and how you changed your behavior.
Incorporate social support and social accountability (Drageset, 2021).
Doing something on your own often requires a lot of willpower, and sticking to it every time can feel like an uphill battle. Take this example:
My goal is to exercise every other morning. But last night, I stayed up late and felt tired in the morning, so I skipped my workout.
Sound familiar? Now imagine if I’d planned to meet a workout buddy. Knowing someone was counting on me would’ve gotten me out of bed, even if I was tired, because I wouldn’t want to let them down.
Accountability can make all the difference. Another powerful strategy is sharing your goals publicly. When you announce your plans on social media or to friends and family, you create a sense of commitment—not just to yourself but to others. It’s like having a built-in support system cheering you on and holding you accountable. Whether it’s finding a partner, joining a group, or sharing your progress online, involving others can help turn your resolutions into habits you’re more likely to stick with.
Describe a strategy to increase social support and accountability.
Be honest in identifying what motivates you.
Exercising, eating healthy foods, thinking positively, or being on time are laudable goals; however, it often feels like work doing the “right” thing. To increase success, analyze what really helped you be successful. For example:
Many years ago, I decided that I should exercise more. Thus, I drove from house to the track and ran eight laps. I did this for the next three weeks and then stopped exercising. Eventually, I pushed myself again to exercise and after a while stopped again. The same pattern kept repeating. I would exercise and fall off the wagon and stop. Later that fall, I met a woman who was a jogger and we became friends and for the next year we jogged together and even did races. During this time, I did not experience any effort to go jogging. After a year, she broke up with me and once again, I had to use willpower to go jogging and my old pattern emerged and after a few days I stopped jogging even though I felt much better after having jogged.
I finally, asked what is going on? I realized that the joy of the jogging was running with a friend. Once, I recognized this, instead using will power to go running, I spent my willpower finding people with whom I could exercise. With these new friends, running did not depend upon my willpower– It only depended on making running dates with my new friends.
Explore factors that will allow you to do your activity without having to use willpower.
Conclusion
These seven strategies are just a starting point—there are countless other techniques that can help you stick to your New Year’s resolutions. For example, keeping a log, setting reminders, or rewarding yourself for progress are all powerful ways to stay on track. The real magic happens when your new behavior becomes part of your routine—embedded in your habitual patterns. The more automatic it feels, the greater your chances of long-term success.
So, take joy in identifying, implementing, and maintaining your resolutions. Let them enhance your well-being and become second nature. Share your successful strategies with me and others—it could be just the inspiration someone else needs to achieve their goals, too.
References
Drageset, J. (2021). Social Support. In: Haugan G, Eriksson M, editors. Health Promotion in Health Care – Vital Theories and Research [Internet]. Cham (CH): Springer, Chapter 11. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585650/ https://doi.org/10.1007/978-3-030-63135-2_11
Latham, G. P., & Locke, E. A. (2006). Enhancing the Benefits and Overcoming the Pitfalls of Goal Setting. Organizational Dynamics, 35(4), 332–340. https://doi.org/10.1016/j.orgdyn.2006.08.008
McLeod, S. (2024). Classical Conditioning: How It Works With Examples.Simple Psychology. Accessed December 29, 2024. https://www.simplypsychology.org/classical-conditioning.html
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. (Pp 185-192). https://he.kendallhunt.com/make-health-happen
Peper, E. & Wilson, V. (2021). Optimize the learning state: techniques and habits. Biofeedback, 9(2), 46-49. https://doi.org/10.5298/1081-5937-49-2-04
Pilcher, S., Schweickle, M. J., Lawrence, A., Goddard, S. G., Williamson, O., Vella, S. A., & Swann, C. (2022). The effects of open, do-your-best, and specific goals on commitment and cognitive performance. Sport, Exercise, and Performance Psychology, 11(3), 382–395. https://doi.org/10.1037/spy0000301
For detailed suggestions, see the following blogs:
[1] Edited with the help of ChatGPT.
Pragmatic techniques for monitoring and coaching breathing
Posted: December 14, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, emotions, meditation, mindfulness, neurofeedback, Pain/discomfort, posture, relaxation, self-healing, Uncategorized | Tags: art, books, Breathing rate, coaching, FlowMD app, nasal breathing, personal-development, self-monitoring, writing 4 CommentsDaniella Matto, MA, BCIA BCB-HRV , Erik Peper, PhD, BCB, and Richard Harvey, PhD
Adapted from: Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
This blog aims to describe several practical strategies to observe and monitor breathing patterns to promote effortless diaphragmatic breathing. The goal of these strategies is to foster effortless, whole-body diaphragmatic breathing that promote health.
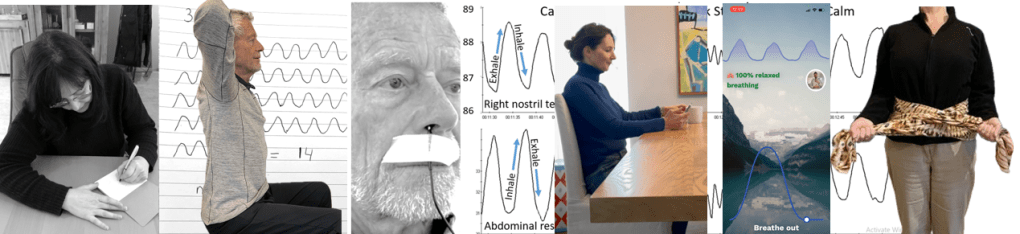
Breathing is usually covert and people are not usually aware of their breathing rate (breaths per minute) or pattern (abdominal or thoracic, breath holding or shallow breathing) unless they have an illness such as asthma, emphysema or are performing physical activity (Boulding et al, 2015)). Observing breathing is challenging; awareness of respiration often leads to unaware changes in the breath pattern or to an attempt to breathe perfectly (van Dixhoorn, 2021). Ideally breathing patterns should be observed/monitored when the person is unaware of their breathing pattern and the whole body participates (van Dixhoorn, 2008). A useful strategy is to have the person perform a task and then ask, “What happened to your breathing?”. For example, ask a person to simulate putting a thread through the eye of a needle or quickly look to the extreme right and left while keeping their head still. In almost all cases, the person holds their breath (Peper et al., 2002).
Teaching effortless slow diaphragmatic breathing is a precursor of Heart rate variability (HRV) biofeedback and is based on slow paced breathing (Lehrer & Gevirtz, 2014; Steffen et al., 2017; Shaffer and Meehan, 2020). Mastering effortless diaphragmatic breathing is a powerful tool in the treatment of a variety of physical, behavioural, and cognitive conditions; however, to integrate this method into clinical or educational practice is easier said than done. Clients with dysfunctional breathing patterns often have difficulty following a breath pacer or mastering effortless breathing at a slower pace.
The purpose of this paper is to describe a few simple strategies that can be used to observe and monitor breathing patterns, provide economic strategies for observation and training, and suggestions to facilitate effortless diaphragmatic breathing.
Strategies to observe and monitor breathing pattern
Observation of the breathing patterns
- Is the breathing through the nose or mouth? Nose is usually better (Watso et al., 2023; Nestor, 2020).
- Does the abdomen expand during inhalation and constricts during exhalation or does the chest expand and rise during inhalation and fall during exhalation? Abdominal movement is usually better.
- Is exhalation flow softly or explosively like a sigh? Slow flow exhalation is preferred.
- Is the breath held or continues during activities? In most cases continued breathing is usually better.
- Does the person gasp before speaking or allows to speak while normally exhaling?
- What is the breathing rate (breaths per minute)? When sitting peacefully less than 14 breaths/minute is usually better and about 6 breaths per minute to optimize HRV
Physiological monitoring.
- Monitoring breathing with strain gauges around the abdomen and chest, and heart rate is the most common approach to identify the location of breath, the breathing pattern and heart rate variability. The strain gauges are placed around the chest and abdomen and heart rate is monitored with a blood volume pulse amplitude sensor from the finger. representative recording shows the effect of thoughts on breathing, heartrate and pulse amplitude of which the participant is totally unaware as shown in Figure 1.
Figure 1. Physiological recording of breathing patterns with strain gauges.
- Monitoring breathing with a thermistor placed at the entrance of the nostril that has the most airflow (nasal patency) (Jovanov et al., 2001; Lerman et al., 2016). When the person exhales through the nose, the thermistor temperature increases and decreases when they inhale. A representative recording of a person being calm, thinking a stressful thought. and being calm. Although there were significant changes as indicated by the change in breathing patterns, the person was unaware of the changes as shown in Figure 2.
Figure 2. Use of a thermistor to monitor breathing from the dominant nostril compared to the abdominal expansion as monitored by a strain gauge around the abdomen.
- Additional physiological monitoring approaches. There are many other physiological measures can be monitored to such as end-tidal carbon dioxide (EtCO2), a non-invasive measurement of the amount of carbon dioxide (CO2) in exhaled breath (Meuret et al., 2008; Meckley, 2013); scalene/trapezius EMG to identify thoracic breathing (Peper & Tibbett, 1992; Peper & Tibbets, 1994); low abdominal EMG to identify transfers and oblique tightening during exhalation and relaxation during inhalation (Peper et al., 2016; and heart rate to monitor cardiorespiratory synchrony (Shaffer & Meehan, 2020). Physiological monitoring is useful; since, the clinician and the participant can observe the actual breathing pattern in real time, how the pattern changes in response the cognitive and physical tasks, and used for feedback training. The recorded data can document breathing problems and evidence of mastery.
The challenges of using physiological monitoring arethat the equipment may be expensive, takes skill to operate and interpret the data, and is usually located in the office and not at home.
Economic strategies for observation and training breathing
To complement the physiological monitoring and allow observations outside the office and at home, some of the following strategies may be used to observe breathing pattern (rate and expansion of the breath in the body), and suggestion to facilitate effortless diaphragmatic breathing. These exercises make excellent homework for the client. Practicing awareness and internal self-regulation by the client outside the clinic contributes enormously to the effect of biofeedback training (Wilson et al., 2023),
Observe breathing rate: Draw the breathing pattern
Take a piece of paper, a pen and a timer, set to 3 minutes. Start the timer. Upon inhalation draw the line up and upon exhalation draw the line down, creating a wave. When the timer stops, after 3 minutes, calculate the breathing rate per minute by dividing the number of waves by 3 as shown in Figure 3.
Figure 3. Drawing the breathing pattern for three minutes during two different days.
From these drawings, the breathing rate become evident. Many individuals are often surprised to discover that their breathing rate increased during periods of stress, such as a busy day with no breaks, compared to their normal days.
Monitoring and training diaphragmatic breathing
The scarf technique for abdominal feedback
Many participants are unaware that they are predominantly breathing in their chest and their abdomen expansion is very limited during inhalation. Before beginning, have participant loosen their belt and or stand upright since sitting collapsed/slouched or having the waist constriction such as a belt of tight constrictive clothing that inhibits abdominal expansion during inhalation.
Place the middle part of a long scarf or shawl on your lower back, take the ends in both hands and cross the ends: your left hand is holding the right part of the scarf, and the right hand is holding the left end of the scarf. Give a bit of a pull, so you can feel any movement of the scarf. When breathing more abdominally you will feel a pull at the ends of the scarf as you lower back, and flanks will expand as shown in Figure 4.

Figure 4. Using a scarf as feedback.
FlowMD app
A recent cellphone app, FlowMD, is unique because it uses the cellphone camera to detect the subtle movements of the chest and abdomen (FlowMD, 2024). It provides real time feedback of the persons breathing pattern. Using this app, the person sits in front of their cellphone camera and after calibration, the breathing pattern is displayed as shown in Figure 5.

Figure 5. Training breathing with FlowMD,.
Suggestions to optimize abdominal breathing that may lead to a slower breath rate when the client practices the technique
Beach pose
By locking the upper chest and sitting up straight it is often easier to breathe so that the abdomen can expand and constrict. Place your hands behind your head and Interlock your finger of both hands, pull your elbows back and up. The person can practice this either laying down on their back or sitting straight up at the edge of the chair as shown in Figure 6.

Figure 6. Sitting erect with the shoulders pulled back and up to allow abdominal expansion and constriction as the breathing pattern.
Observe the effect of posture on breathing
Have the person sit slouched/collapsed like a letter C and take a few slow breath, then have them sit up in a tall and erect position and take a few slow breaths. Usually they will observe that it is easier to breathe slower and lower and tall and erect.
Using your hands for feedback to guide natural breathing
Holding your hands with index fingers and thumbs touching the lower abdomen. When inhaling the fingers and thumbs separate and when exhaling they touch again (ensuring a full exhale and avoiding over breathing). The slight increase in lower abdominal muscle tension during the exhalation and relaxation during inhalation and the abdominal wall expands can also be felt with fingertips as shown in Figure 7.
Figure 7. Using your hands and finger for feedback to guide the natural breathing of expansion and constriction of the abdomen. Reproduced by permission from Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Coaching suggestions
There are many strategies to observe, teach and implement effortless breathing (Peper et al., 2024).. Even though breathing is natural and babies and young children breathe diaphragmatically as their large belly expands and constricts. Yet, in many cases the natural breathing shifts to dysfunctional breathing for multiple reasons such as chronic triggering defense reactions to avoiding pain following abdominal surgery (Peper et al, 2015). When participants initially attempt to relearn this natural pattern, it can be challenging especially, if the person habitually breathes shallowly, rapidly and predominantly in their chest.
When initially teaching effortless breathing, have the person exhale more air than normal without the upper chest compressing down and instead allow the abdomen comes in and up thereby exhaling all the air. If the person is upright then allow inhalation to occur without effort by letting the abdominal wall relaxes and expands. Initially inhale more than normal by expanding the abdomen without lifting the chest. Then exhale very slowly and continue to breathe so that the abdomen expands in 360 degrees during inhalation and constricts during exhalation. Let the breathing go slower with less and less effort. Usually, the person can feel the anus dropping and relaxing during inhalation.
Another technique is to ask the person to breathe in more air than normal and then breathe in a little extra air to completely fill the lungs, before exhaling fully. Clients often report that it teaches them to use the full capacity of the lungs.
The goal is to breath without effort. Indirectly this can be monitored by finger temperature. If the finger temperature decreases, the participant most likely is over-breathing or breathing with too much effort, creating sympathetic activity; if the finger temperature increases, breathing occurs slower and usually with less effort indicating that the person’s sympathetic activation is reduced.
Conclusion
There are many strategies to monitor and coach breathing. Relearning diaphragmatic breathing can be difficult due to habitual shallow chest breathing or post-surgical adaptations. Initial coaching may involve extended exhalations, conscious abdominal expansion, and gentle inhalation without chest movement. Progress can be monitored through indirect physiological markers like finger temperature, which reflects changes in sympathetic activity. The integration of these techniques into clinical or educational practice enhances self-regulation, contributing significantly to therapeutic outcomes. In this article we provided a few strategies which may be useful for some clients.
Additional blogs on breathing
https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
REFERENCES
Boulding, R., Stacey, R., & Niven, N. (2016). Dysfunctional breathing: a review of the literature and proposal for classification. European Respiratory Review, 25(141),: 287-294. https://doi.org/10.1183/16000617.0088-2015
FlowMD. (2024). FlowMD app. Accessed December 13, 2024. https://desktop.flowmd.co/
Jovanov, E., Raskovic, D., & Hormigo, R. (2001). Thermistor-based breathing sensor for circadian rhythm evaluation. Biomedical sciences instrumentation, 37, 493–497. https://pubmed.ncbi.nlm.nih.gov/11347441/
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Lerman, J., Feldman, D., Feldman, R. et al. Linshom respiratory monitoring device: a novel temperature-based respiratory monitor. (2016). Can J Anesth/J Can Anesth, 63, 1154–1160. https://doi.org/10.1007/s12630-016-0694-y
Meckley, A. (2013). Balancing Unbalanced Breathing: The Clinical Use of Capnographic Biofeedback. Biofeedback, 41(4), 183–187. https://doi.org/10.5298/1081-5937-41.4.02
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (2008). Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of psychiatric research, 42(7), 560–568. https://doi.org/10.1016/j.jpsychires.2007.06.005
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath-New-Science-Lost-Art/dp/0735213615/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make Health Happen. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Peper, E., & Tibbetts, V. (1992). Fifteen-month follow-up with asthmatics utilizing EMG/incentive inspirometer feedback. Biofeedback and self-regulation, 17(2), 143–151. https://doi.org/10.1007/BF01000104
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. https://biofeedbackhealth.org/wp-content/uploads/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Shaffer, F. and Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., and Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
van Dixhoorn, J.V. (2008). Whole-body breathing. Biofeedback, 36,54–58. https://www.euronet.nl/users/dixhoorn/L.513.pdf
van Dixhoorn, J.V. (2021). Functioneel ademen-Adem-en ontspannings oefeningen voor gevorderden. Amersfoort: Uiteveriy Van Dixhoorn. https://www.bol.com/nl/nl/p/functioneel-ademen/9300000132165255/
Watso, J. C., Cuba, J.N., Boutwell, S.L, Moss, J…(2023). Acute nasal breathing lowers diastolic blood pressure and increases parasympathetic contributions to heart rate variability in young adults. American Journal of Physiology Regulatory, Integrative and Comparative Physiology.
325I(6), R797-R80. https://doi.org/10.1152/ajpregu.00148.2023
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Health Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 415 338 7683 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com
Suggestions for mastering and generalizing breathing skills
Posted: October 30, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cellphone, cognitive behavior therapy, emotions, ergonomics, healing, health, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: abdominal beathing, anxiety, diaphragmatic braething, health, hyperventilation, meditation, mental-health, mindfulness, mouth breathing, Toning 3 CommentsAdapted from: Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/

Breathing techniques are commonly employed with complimentary treatments, biofeedback, neurofeedback or adjunctive therapeutic strategies to reduce stress and symptoms associated with excessive sympathetic arousal such as anxiety, high blood pressure, insomnia, or gastrointestinal discomfort. Even though it seems so simple, some participants experience difficulty in mastering effortless breathing and/or transferring slow breathing skills into daily life. The purpose of this article is to describe: 1) factors that may interfere with learning slow diaphragmatic breathing (also called cadence or paced breathing, HRV or resonant frequency breathing along with other names), 2) challenges that may occur when learning diaphragmatic breathing, and 3) strategies to generalize the effortless breathing into daily life.
Background
A simple two-item to-do list could be: ‘Breathe in, breathe out.’ Simple things are not always easy to master. Mastering and implementing effortless ‘diaphragmatic’ or ‘abdominal belly’ breathing may be simple, yet not easy. Breathing is a dynamic process that involves the diaphragm, abdominal, pelvic floor and intercostal muscles that can include synchronizing the functions of the heart and lungs and may result in cardio-respiratory synchrony or coupling, as well as ‘heart-rate variability breathing training (Codrons et al., 2014; Dick et al., 2014; Elstad et al., 2018; Maric et al., 2020; Matic et al., 2020). Improving heart-rate variability is a useful approach to reduce symptoms of stress and promotes health and reduce anxiety, asthma, blood pressure, insomnia, gastrointestinal discomfort and many other symptoms associated with excessive sympathetic activity (Lehrer & Gevirtz, 2014; Xiao et al., 2017; Jerath et al., 2019; Chung et al., 2021; Magnon et al., 2021; Peper et al., 2022).
Breathing can be effortful and In some cases people have dysfunctional breathing patterns such as breath holding, rapid breathing (hyperventilation), shallow breathing and lack of abdominal movement. This usually occurs without awareness and may contribute to illness onset and maintenance. When participants learn and implement effortless breathing, symptoms often are reduced. For example, when college students are asked to practice effortless diaphragmatic breathing twenty-minutes a day for one week, as well as transform during the day dysfunction breathing patterns into diaphragmatic breathing, they report a reduction in shallow breathing, breath holding,, and a decrease of symptoms as shown in Fig 1 (Peper et al, 2022).

Figure 1. Percent of people who reported that their initial symptoms improved after practicing slow diaphragmatic breathing for twenty minutes per day over the course of a week (reproduced from: Peper et al, 2022).
Most students became aware of their dysfunctional breathing and substituted slow, diaphragmatic breathing whenever they realized they were under stress; however, some students had difficulty mastering ‘effortless’ (e.g., automated, non-volitional) slow, diaphragmatic breathing that allowed abdominal expansion during inhalation.
Among those had more difficulty, they tended to have almost no abdominal movement (expansion during inhalation and abdominal constriction during exhalation). They tended to breathe shallowly as well as quickly in their chest using the accessory muscles of breathing (sternocleidomastoid, pectoralis major and minor, serratus anterior, latissimus dorsi, and serratus posterior superior).
The lack of abdominal movement during breathing reduced the movement of lymph as well as venous blood return in the abdomen; since; the movement of the diaphragm (the expansion and constriction of the abdomen) acts a pump. Breathing predominantly in the chest may increase the risk of anxiety, neck, back and shoulder pain as well as increase abdominal discomfort, acid reflux, irritable bowel, dysmenorrhea and pelvic floor pain (Banushi et al., 2023; Salah et al., 2023; Peper & Cohen, 2017; Peper et al., 2017; Peper et al., 2020, Peper et al., 2023). Learning slow, diaphragmatic or effortless breathing at about six breaths per minute (resonant frequency ) is also an ‘active ingredient’ in heartrate variability (HRV) training (Steffen et al., 2017; Shaffer & Meehan, 2020).
1. Factors that interfere with slow, diaphragmatic breathing
Difficulty allowing the skeletal and visceral muscles in the abdomen to expand or constrict in ‘three-dimensions’ (e.g., all around you in 360 degrees) during inhalation or exhalation. Whereas internal factors under volitional control and will mediate breathing practices, external factors can restrict and moderate the movement of the muscles. For example:
Clothing restrictions (designer jeans syndrome). The clothing is too tight around the abdomen; thereby, the abdomen cannot expand (MacHose & Peper, 1991; Peper et al., 2016). An extreme example were the corsets worn in the late 19th century that was correlated with numerous illnesses.
Suggested solutions and recommendations: Explain the physiology of breathing and how breathing occurs by the diaphragmatic movement. Discuss how babies and dogs breathe when they are relaxed; namely, the predominant movement is in the abdomen while the chest is relaxed. This would also be true when a person is sitting or standing tall. Discuss what happens when the person is eating and feels full and how they feel better when they loosen their waist constriction. When their belt is loosened or the waist button of their pants is undone, they usually feel better.
Experiential practice. If the person is wearing a belt, have the person purposely tighten their belt so that the circumference of the stomach is made much smaller. If the person is not wearing a belt, have them circle their waist with their hands and compress it so that the abdomen can not expand. Have them compare breathing with the constricted waist versus when the belt is loosened and then describe what they experienced.
Most participants will feel it is easier to breathe and much more comfortable when the abdomen is not constricted.
Previous abdominal injury. When a person has had abdominal surgery (e.g., Cesarean section, appendectomy, hernia repair, or episiotomy), they unknowingly may have learned to avoid pain by not moving (relaxing or tensing) the abdomen muscles (Peper et al., 2015; Peper et al., 2016). Each time the abdomen expands or constricts, it would have pulled on the injured area or stitches that would have cause pain. The body immediately learns to limit movement in the affected area to avoid pain. The reduction in abdominal movement becomes the new normal ‘feeling’ of abdominal muscle inactivity and is integrated in all daily activities. This is a process known as ‘learned disuse’ (Taub et al., 2006). In some cases, learned disuse may be combined with fear that abdominal movement may cause harm or injury such as after having a kidney transplant. The reduction in abdominal movement induces shallow thoracic breathing which could increase the risk of anxiety and would reduce abdominal venous and lymph circulation that my interfere with the healing.
Suggested solutions and recommendations. Discuss the concept of learned disuse and have participant practice abdominal movement and lower and slower breathing.
Experiential practices: Practicing abdominal movements
Sit straight up and purposely exhale while pulling the abdomen in and upward and inhale while expanding the abdomen. Even with these instructions, some people may continue to breathe in their chest. To limit chest movement, have the person interlock their hands and bring them up to the ceiling while going back as far as possible. This would lock the shoulders and allows the abdomen to elongate and thereby increase the diaphragmatic movement by allowing the abdomen to expand. If people initially have held their abdomen chronically tight then the initial expansion of abdomen by relaxing those muscle occurs with staccato movement. When the person becomes more skilled relaxing the abdominal muscles during inhalation the movement becomes smoother.
Make a “psssssst” sound while exhaling. Sit tall and erect and slightly pull in and up the abdominal wall and feel the anus tightening (pulling the pelvic floor up) while making the sound. Then allow inhalation to occur by relaxing the stomach and feeling the anus go down.
Use your hands as feedback. Sit up straight, placing one hand on the chest and another on the abdomen. While breathing feel the expansion of the abdomen and the contraction of the abdomen during exhalation. Use a mirror to monitor the chest-muscle movement to ensure there is limited rising and falling in this area.
Observe the effect of collapsed sitting. When sitting with the lower back curled, there is limited movement in the lower abdomen (between the pubic region and the umbilicus/belly button) and the breathing movement is shallower without any lower pelvic involvement (Kang et al., 2016). This is a common position of people who are working at their computer or looking at their cellphone.
Experiential practice: looking at your cellphone
Sit in a collapsed position and look down at your cellphone. Look at the screen and text as quickly as possible.
Compare this to sitting up and then lift the cell phone at eye level while looking straight ahead at the cellphone. Look at the screen and text as quickly as possible.
Observe how the position effected your breathing and peripheral awareness. Most likely, your experience is similar those reported by students. Close to 85%% of students who complete this activity reported that their breathing was shallower sitting slouched versus erect and about 85% of the students reported that their peripheral awareness and vision improved when sitting erect (Peper et al., 2024).
Suggested solutions and recommendations. Be aware how posture affect breathing. While sitting, place a rolled-up towel against the lower back so that the person sits more erect which would allow the abdomen to expand when inhaling.
Self-image, self-esteem, and confidence. Participants may hold their abdomen in because they want to look slim (sometimes labeled as the “hourglass syndrome” associate expanding the abdomen as unattractive (PTI, 2023). A flat abdomen is culturally reinforced by social media and fashion models and encouraged in some activities such as ballet. On the other hand, some people purposely puff up their chest to increase size and dominance (Cohen & Leung, 2009).
Suggested solutions and recommendations. Discuss the benefits of diaphragmatic breathing including its ability to reduce anxiety in social settings that may enhance confidence. Similar to an earlier suggestion, have the person explore clothing with a looser waist that still supports feelings of attractiveness and power.
Feeling anxious, fearful or threatened. The normal physiological stress reaction is a slight gasp with the tightening of the abdomen muscles for protection when a stressor occurs (Gilbert, 1998; Ekerholt & Bergland., 2008). The stressor can be an actual physical event, social situation or thoughts and emotions. Shallow breathing is a natural self-protective response. This pattern is often maintained until one feels ‘safe’ enough to relax, which for many can have a duration of the entire day or until finding the relative safety of sleep.
Suggested solutions and recommendations. Discuss how the physiological stress reaction is a normal response pattern that the person most likely learned in early childhood for self-protection. This pattern is often observed in clients who are emotionally sensitive and/or react excessively to a variety of stimuli. Note that some people have learned not to show their reactivity on their face or in the overt behaviors, yet they continue to breathe shallowly as a telltale sign of ‘distress.’ People who breath shallowly may experience this response as burdensome. Discuss with them how to reframe their sensitivity as a gift; namely, they are more aware of other people’s reactions and emotions. They just need to learn how not to respond automatically. Encourage awareness of their breath-holding and shallow breathing. Follow this by teaching them to replace the dysfunctional breathing with slow, diaphragmatic breathing at 6-breaths-per-minute. A possible training sequence is the following:
- Teach slow, diaphragmatic breathing
- Practice evoking a stressor and the moment the client senses the stress response, shallow breaths or holds their breath have them shift to slow, diaphragmatic breathing.
- If the person slouches in response to stress, the moment they become aware of slouching, have then sit erect, look up and then breathe diaphragmatically. (Peper et al., 2019)
Experiential practice: Transform stressful thoughts by looking up, breathing, and changing thoughts.
Evoke a stressor and then attempt to reframe the experience (cognitive behavior therapy or CBT approach).
Compare this to evoking a stressor, then shift to an upright position while looking up, take a few slow, diaphragmatic breaths, and reframe the experience.
In almost all cases, when the client shifts position, looks up and then reframes, the stress reaction is significantly reduced and it is much easier to reframe the experiences positively compared to when only attempting to reframe the experience (Peper et al., 2019).
Diaphragmatic breathing feels abnormal. How you breathe habitually is what feels normal unless there is overt illness such as asthma or emphysema. Any new pattern usually feels abnormal. When the person shifts their breathing pattern, such as in a transition from habitual shallow chest breathing to slower diaphragmatic abdominal breathing, it feels strange and wrong.
Suggested solutions and recommendations. Discuss the concept that habitual patterns are normal (e.g., a person who typically slouches when standing straight may experience that they are going to fall backwards). Emphasize the importance of making a shift in posture and leaning into the discomfort of the new experience. Often after practicing slow diaphragmatic breathing, the person may report feeling much more relaxed (e.g., sensing heaviness and warmth) with their fingers increasing in temperature.
2. Challenges that may occur when learning diaphragmatic breathing
Ideally, breathing is an effortless diaphragmatic process as described by the phrase, “it breathes me” (Luthe & Schultz, 1970; Luthe, 1979); however, some participants struggle to achieve this type of breathing. The following are common challenges and possible solutions:
Distraction and internal dialogue. Many people struggle with thoughts jumping from one area to another. Some people refer to this mental state as “monkey mind.”
Suggested solutions and recommendations. Validate that distraction and internal dialogue are normal and require continual managing and practice to overcome. Experimental Practice: Have the person train focus during diaphragmatic breathing techniques by focusing on 1 item in the room. Remind them that when thoughts arise, note them briefly instead of engaging with them and then refocus on the item. Start with increments of time and increase with practice.
Effect of gravity on breathing. In the vertical position, exhalation occurs when the abdomen constricts (slight tightening of the transverse and oblique abdominal muscles and the pelvic floor) pushes the diaphragm up, allowing the air to go out. It needs to push against gravity.
In the vertical position, inhalation occurs when the abdominal muscles and pelvic floor muscles relax and the abdomen widens in all directions (360 degrees) which causes the diaphragm to descend as it is being pulled down by gravity. This process allows effortless inhalation. The experience is the opposite when lying supine on one’s back. While lying down, gravity pulls on the abdomen that cause the diaphragm to go upward allowing the air to flow out during exhalation. Inhalation takes work because as the diaphragm descends it has to push the abdominal content upward against gravity.
Experiential practice: Erect versus supine
- Vertical position. Begin by exhaling completely by pulling the abdomen in and up while staying erect and not pressing/contracting the chest downward. At the end of exhalation, allow the abdomen to relax (pop out) and feel how the air is sucked in without trying to inhale
- Horizontal position. Begin by lying down, with the face pointing up. Inhale by expanding your abdomen and pushing your abdomen upward against gravity. Then let exhalation occur while totally relaxing as gravity pushes the abdomen downward, which pushes the diaphragm upward into the chest allowing the air to flow out. Optionally, place a small bag of rice/beans (e.g., approximately one to five pound or. One-half to two kilograms) on your lower abdomen while lying down. When you inhale, push the weight upward and away from you by allowing the stomach, but not the chest, to expand. Allow exhalation to occur as the weight pushes your abdomen down and upward into your chest. The weight is useful as it allows the mind to focus more easily on the task of feeling the movement of the abdomen.
Over breathing/hyperventilation. Even breathing at about six breaths per minute can cause hyperventilation can occur. Hyperventilation occurs when a person is breathing in excess of the metabolic needs of the body and thereby eliminating more carbon dioxide. The result is respiratory alkalosis and an elevated blood pH as the dissolved carbon dioxide (pCO2) in the blood is reduced (Folgering, 1999).
The most common symptoms of over breathing are colder sweaty hands and light-headedness. If this starts to occur, focus on decreasing the airflow during exhalation by exhaling through pursed lips making the sound, “Pssssssst.” While making this sound, make the sound softer with less airflow. Alternatively, have them imagine a holding a dandelion flower a few inches from their lips and blow so softly the seeds do not blow away. The blowing away of the seed is the feedback that you are blowing to hard as shown in Figure 2.

Figure 2. Dandelion seeds as feedback when the person is blowing with too much effort. Alternatively, we recommend that the client imagine smelling the scent/fragrance of a flower that usually causes nose inhalation and then exhale gently through pursed lips ast if the air flows over a candle and, the flame does not move back and forth.
Mouth breathing. Mouth breathing contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded miss-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. Nose breathing reduces airway irritation since the nose filters, humidifies, warms/cools the inhaled air as well as reduces the air turbulence in the upper airways. The epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation (McKeown, 2019; Allen, 2024). Note that alternate nostril breathing, such as breathing in one nostril for 5-seconds and out of the other for 5-seconds is another technique which some people find beneficial.
Slower breathing approaches also facilitates sympathetic parasympathetic balance and reduces airway irritation. If the person breathes habitually through their mouth, refer them to health care provider to explore factors that may contribute to mouth breathing such as enlarged tonsils and adenoids or deviated septum. In addition, explore environmental factors that could contribute nasal inflammation such as allergies or foods such as dairy (Al-Raby, 2016).
Performance anxiety. Many participants are concerned about their performance. The direct instructions such as “follow the graphic” causes the person to try hard to breathe with too much effort. Explore some of the following indirect strategies to interrupt ongoing cognitive judgements and self-talk.
- Toning or humming (Peper et al., 2019a). While exhaling, have the person hum a sound with their mouth closed. Let the sound go for about 6 seconds, relax, inhale and hum again. Toning is very similar except you verbalize a tone such as “Oammm.” (For detailed instructions on toning, see: Anziani & Peper (2021)).
- Stroking down arms and legs during exhalation. Have a partner gently stroke down your arms from your shoulder past your fingertips as you are exhaling. The downward stroking is in rhythm with the exhalation. As the arm is being stroked, attend to the sensations going down the arms. Be sure that the toucher exhales at the same time and the stroking down the arm takes about six seconds. After being stroked for a few times, have the person imagine that each time they exhale they feel a flow down through their arms and out their fingers.
- Repeat the same process while stroking down the legs from the side of their hips to their toes.
- Finally, have the person imagine/feel the sensation streaming down their legs with each exhalation.
- Many participants will report that they sense a steaming going down their arms, that they hands warm up, and their thought have stopped.
- Integrated body movement with breathing especially flexion and contraction (Meehan & Shaffer, 2023). Integrate the normal response of flexion that induces exhalation and extension evokes inhalation. Be careful that the flexion movement does not encourage participants to compress their chest during exhalation, which tends to encourage chest breathing. Have the person focus on their head staying tall and erect. Have the person sit straight up with their feet slight apart and their hands palm down on their lap. Allow inhaling to initiate as the person simultaneously arches their lower back expanding the stomach, separating the knees and turning the hands palm up. Initiate exhalation while simultaneously bringing the knees together, turning the palms face down on the thighs and rolling the pelvic back slightly rounding the lower back. Do the movements smoothly while keeping the legs and shoulders relaxed.
Flooded by emotions. Although very rare, at times when the person allows the abdomen to relax, they may experience by the emotions from a past trauma as the habitual bracing patterns are relaxed.
Suggested solutions and recommendations. Validate these emotions for the person. Explain that this is a normal process that may occur if past trauma has occurred. Clients who have had past trauma often experience hypervigilance, which may interfere with the relaxation response that occurs during more optimal states of breathing. Transitioning to a more optimal rest state may be uncomfortable for a person who has experienced trauma because it reduces hypervigilance. This can feel uncomfortable as hypervigilance in these cases serves a protective role, even if it is an illusory feeling of protection from future harm. Since persistent hypervigilance can interfere with the relaxation response, the benefits of allowing a relaxation response to occur through slower breathing should be highlighted. Grounding techniques as described by Peper et al (2024a) can be useful to become centered.
3. Strategies to generalize the effortless breathing into daily life.
Generalizing the skill occurs after having mastered diaphragmatic breathing in different positions (sitting, standing, lying down, and while performing tasks). It is important to remember that our breathing patterns are conditioned with our behavior. Become aware how breathing affects cognitions and emotions and how emotions and cognitions affects breathing. The following are some strategies that may facilitate learning and generalizing the slower breathing skills.
Observing how our behavior affects our breathing: Anything that may evoke the alarm or defense reaction tends to cause the person gasp and/or hold their breath. For example, when a person is sitting peacefully, make an unexpected noise behind their back or movement in their periphery of vision. In most cases they will gasp or hold their breath. Usually, they are unaware of this process unless they are asked what happened to their breathing. The major reason for the breath holding is that the stimuli triggers an alarm/defense reaction and when we hold our breath our hearing is more acute (we can hear approaching danger earlier). The problem is that we give this response when there is no actual, immediate or present threat.
Experiential practice. Sit comfortably. Now as quickly as possible without rotating the head, look with your eyes to the extreme right and then left and back and forth as if trying to identify danger at the periphery. Do this for a few eye movements. Almost everyone holds their breath when doing this exercise. For generalizing the skill, ask the person to observe during the day situations in which they hold their breath, ask them if it was necessary and encourage them to start diaphragmatic breathing.
Observing how breathing affects our thoughts and emotions. Breathing patterns are intrinsically linked to our emotions and thoughts as illustrated in the many language phrases such as sigh of relief, full of hot air, waiting with bated breath. At the same time, our breathing patterns also affect our thoughts. For instance, when we breathe shallowly and more rapidly, we can induce feelings of fear or anxiety. If we gasp, we can experience thought stopping.
Experiential practices: Incomplete exhalation: Observe what happens when you exhale less than you inhale. Begin by exhaling only 70% of the air you inhaled, then inhale and exhale again only 70% of the air you just inhaled continue this for 30 seconds. Many people will experience the onset of anxiety symptoms, lightheadedness, dizziness, neck and shoulder tension, etc. (Peper & MacHose, 1993). If you experience symptoms during this exercise and you have experienced these symptoms in the past, it is likely that unknowingly breathing in a dysfunctional pattern could have evoked them. Therefore, practicing effortless breathing may interrupt and reduce the symptoms. Do this practice while observing the person carefully and immediately interrupt and distract the person if they start feeling dizzy, too anxious, or trigger the beginning of a panic attack or PTSD symptoms.
Experiential practice: Gasp or sniff-hold sniff. Observe what happens when you are performing a cognitive task and you rapidly gasp or do sniff-hold-sniff again before exhaling. Begin by sequentially subtracting mentally, the number 7 from 146 (e.g., 146, 139, 132….). Do this as rapidly as possible and do not make a mistake. While doing the subtracting, take a rapid gasp (such as one is triggered by surprise or fear), alternatively, take a quick sniff through your nose, hold your breath and take another sniff on top of the first one, then exhale. Whereas subtrating numbers is a skill most adults can perform, the ‘time pressure’ along with the direction to avoid mistakes may be the ‘immediate’ source of strain. Whether it was the time pressure, the direction to avoid mistakes or the direction to gasp, observe what happened to your thinking process. In almost all cases, your higher-order thoughts (doing the sequential subtraction under time pressure while gasping) have disappeared, replaced by the immediate thoughts of ‘performance anxiety.’
If you blank out on exams or experience anxiety, gasping and breath holding may be one of the factors that increases symptoms and affects your performance. If you are aware that you are holding your breath or gasped, use that as the cue to shift to slow diaphragmatic breathing and you may find that your performance improves. Therefore, observe when and where you were blanking out, gasping and/or holding your breathing then substitute slow, effortless diaphragmatic breathing.
How to develop awareness and interrupting of dysfunctional breathing response. Most participants are unaware of their somatic responses until symptoms occur. Being aware of the initiation of a somatic response may assist you in identifying triggers and interrupting the developing process. A significant component of the training is symptom prescription rehearsal.
Symptom prescription is a practice in which the participant simulates/acts out the psychophysiological pattern associated with their symptoms. They amplify the body pattern until they feel the onset of the actual symptoms. The moment the person feels the beginning of the symptom, they stop the practice and initiate slow breathing and relaxation. After practicing the symptom rehearsal, they are instructed to become aware of the onset of the symptom and then use that signal to trigger the effortless breathing while looking up and shifting the body into an upright sitting position (Peper et al., 2019). Gasping and breath holding are normal responses to unexpected stimuli; however, they may trigger sympathetic activation even when there is no actual danger.
Experiential practice: Developing awareness on neck and shoulder tension:
Sit comfortably and practice effortless breathing for a minute. Take a fearful gasp and observe what happens in your body (e.g., slight neck and upper chest tension, light headedness, slight radiating pain into the eye, etc.). Shift back to effortless breathing until all symptoms /sensations have disappeared.
- Now gasp with less effort and observe the first sensations, use the awareness of first sensations to trigger the effortless breathing and continue to breathe until symptoms have disappeared
- Continue this practice. Reduce the gasping effort each time.
- After having developed the initial somatic sensation then during the day observe what triggers this response and immediately shift to slower diaphragmatic breathing. After you have shifted to effortless breathing, reflect on the trigger. Was it necessary to react? If yes, explore strategies to resolve the issue.
The same process can be done to assist with desensitization to painful memories or stressful events. Each time the person becomes aware of their somatic reaction to an evoked memory or stressful event, they shift to effortless diaphragmatic breathing. If they find that it is difficult to interrupt the emotional memories and it triggers more and more negative thoughts and associations, use the sniff-hold-sniff technique and follow that with box-breathing or any of the other quick somatic rescue techniques (Peper et al., 2024a). Box-breathing in this context could include a brief breath-holding. A typical box-breathing technique is to breath in for a count of four, hold for a count of four, breath out for a count of four, then breath in again for a count of four, continuing the figurative 4-4-4-4 count of breathing.
Practice slower diaphragmatic breathing during the day. Implement effortless diaphragmatic breathing through regeneration and interrupting the stress response.
- Support regeneration. Each day set aside 10 to 20 minutes to practice slow effortless diaphragmatic breathing at about 6-breaths-per-minute. In the beginning 10 to 20 minutes may be too long, thus in some cases have the person practice a few times a day for two minutes and slowly build up to 10 or more minutes. The practice is not just a mechanical process of breathing it includes mindfulness training. Namely, as you are breathing each time you exhale imagine a flow doing down your arms and legs and as you inhale an energy coming into you. Whenever your attention drifts bring it back to the breathing.
- Integrate breathing with daily activities. Practice slower breather before eating, after putting the seat belt on in the car, or whenever a notification pops up on the cell phone.
- Set reminders and alarms on your phone to check how you are feeling and breathing. Leave notes on nearby furniture such as a nightstand, on the shower door, and/or on the kitchen table as reminders to be mindful of your breath. If stressed or breathing shallowly, take a moment to breathe slowly.
- Interrupt the stress response. During the day when you are aware that you shallow breathe, are holding your breath, feel anxious, experience neck and shoulder tightness, or worry and use that as a cue to shift position by sitting or standing more erect, looking upward and take a few slow diaphragmatic breaths.
- Use cue condition to facilitate this process. Each time you begin the practice smell a specific aroma or do some behavioral movement and then do the breathing. After a while the aroma or behavioral movement will become the classically conditioned cue to trigger the effortless breathing.
- Use role rehearsal and conditioning to generalize the skill. Generalizing the skills often takes more time than what may be expected. In a culture where instant relief is expected— implied message associated with medication— self-mastery techniques are different and challenging as they take time to master the skill and implement them during daily life. The process of mastery is similar to learning to play a musical instrument or sports. Learning to play the violin requires practice as well as practice with failures along the way until one is ready for more challenging musical pieces, recitals, or performances.
A useful strategy to implement the learning is role rehearsal in the office, at home at work, and in real life. It is usually much easier to practice these skills in a safe space such as your own room or, with a therapist compared to with other people or, at work. To generalize the skill most efficiently, it can be helpful to practice in a safe environment while imagining being in the actual stressful location This process is illustrated by the strategy to reduce social anxiety and menstrual cramps.
Social anxiety when seeing my supervisor. Master effortless breathing in a safe environment. Role rehearsal in imagery. If you observed that you held your breath when your supervisor is around, begin with imagery when your supervisor is not present. Sit, comfortably. Let go of muscle tension and breathe effortlessly, evoking a scenario where your supervisor is walking by and continue to breathe slowly as you imagine the scene. Role rehearsal in action. Ask another person to role-play your supervisor. Sit, comfortably. Let go of muscle tension and breathe effortlessly. Have this person walk into the room in a similar way that your supervisor would. Imagine that person is your supervisor while practicing your effortless breathing. Repeat until the effortless breathing is more automatic. Practice many times in real life. Whenever the rehearsed situation occurs, implement slower paced breathing.
Menstrual cramps that causes most women to curl up and breathe shallowly when experiencing menstrual cramps (Peper et al., 2023). Master effortless breathing in a safe environment. Practice breathing lying down. While lying down, breathe diaphragmatically by having a three-to-five-pound weight such as a bag of rice or hot water pad on your abdomen. If you have a partner, have the person stroke your legs from the abdomen to your toes while you exhale. Role rehearse experiencing pain and then practice lower diaphragmatic breathing. Namely, tighten your abdomen as if you have discomfort, then focus on relaxing the buttocks and sensing the air flowing down your legs and out your feet as you exhale. Practice in real life. A few days before you expected menstruation, practice slow diaphragmatic breathing several times for at least 5-10 minutes during the day. When your menstruation starts practice the slower and lower breathing while imagining the air flowing down the abdomen, through the legs and out the feet.
Summary/Conclusion
Breathing is the mind-body bridge. It usually occurs without awareness and breathing changes affect our thought, emotions and body. Mastering and implementing slower breathing during the day takes time and practice. By observing when breathing patterns change, participants may identify internal and external factors that affect breathing which provides an opportunity to implement effortless diaphragmatic breathing to optimize health as well as resolve some of the triggers. As one 20-year-old, female student reported,
The biggest benefit from learning diaphragmatic breathing was that it gave me the feeling of safety in many moments. My anxiety tended to make me feel unsafe in many situations but homing in and mastering diaphragmatic breathing helped tremendously. I shifted from constant chest breathing to acknowledging it and in turn, reminding myself to breathe with my diaphragm.
References
Allen, R. (2024). The health benefits of nose breathing. Nursing in General Practice. http://hdl.handle.net/10147/559021
Al-Rabia, M.W. (2016). Food-induced immunoglobulin E-mediated allergic rhinitis. J Microsc Ultrastruct, 4(2), 69-75. https://doi.org/doi.org/10.1016/j.jmau.2015.11.004
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. Peperperspective –ideas on illness, health and well-being from Erik Peper. Accessed April 16, 2024. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Banushi, B., Brendle, M., Ragnhildstveit, A., Murphy, T., Moore, C., Egberts, J., & Robison, R. (2023). Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sci. 13(2), 256. https://doi.org/10.3390/brainsci13020256
Chung, A.H., Gevirtz, R.N., Gharbo, R.S. et al. (2021).Pilot Study on Reducing Symptoms of Anxiety with a Heart Rate Variability Biofeedback Wearable and Remote Stress Management Coach. Appl Psychophysiol Biofeedback 46, 347–358. https://doi.org/10.1007/s10484-021-09519-x
Cohen, D. & Leung, A.K.Y. (2009). The hard embodiment of culture. European Journal of Social Psychology, 9, 1278–1289 https://doi.org/10.1002/ejsp.671
Codrons, E., Bernardi, N. F., Vandoni, M., & Bernardi, L. (2014). Spontaneous group synchronization of movements and respiratory rhythms. PloS one, 9(9), e107538. https://doi.org/10.1371/journal.pone.0107538
Dick, T. E., Mims, J. R., Hsieh, Y. H., Morris, K. F., & Wehrwein, E. A. (2014). Increased cardio-respiratory coupling evoked by slow deep breathing can persist in normal humans. Respiratory physiology & neurobiology, 204, 99-111. https://doil.org/10.1016/j.resp.2014.09.013
Ekerholt, K. & Bergland, A. (2008). Breathing: A sign of life and a unique area for reflection and action. Physical therapy, 88(7), 832-840. https://doi.org/10.2522/ptj.20070316
Elstad, M., O’Callaghan, E. L., Smith, A. J., Ben-Tal, A., & Ramchandra, R. (2018). Cardiorespiratory interactions in humans and animals: rhythms for life. American Journal of Physiology-Heart and Circulatory Physiology, 315(1), H6-H17. https://doi.org/10.1152/ajpheart.00701.2017
Folgering, H. (1999). The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis, 54(4), 365-72. https://pubmed.ncbi.nlm.nih.gov/10546483/
Gilbert, C. (1998). Emotional sources of dysfunctional breathing. Journal of bodywork and movement therapies, 2(4), 224-23. https://doi.org/10.1016/S1360-8592(98)80019-3
Jerath, R., Beveridge, C., & Barnes, V.A. (2019). Self-Regulation of Breathing as an Adjunctive Treatment of Insomnia. Front Psychiatry, 9(780). https://doi.org/10.3389/fpsyt.2018.00780
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Kang, K.W., Jung, S.I., Lee, do Y., Kim, K., & Lee, N.K. (2016) Effect of sitting posture on respiratory function while using a smartphone. J Phys Ther Sci, 28(5), 1496-8. https://doi.org/10.1589/jpts.28.1496
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol. 5, 756. https://doi.org/10.3389/fpsyg.2014.00756
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
MacHose, M., & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Magnon. V., Dutheil, F., & Vallet, G.T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 11(1),19267. https://doi.org/10.1038/s41598-021-98736-9
Maric, V., Ramanathan, D., & Mishra, J. (2020). Respiratory regulation & interactions with neuro-cognitive circuitry. Neuroscience & Biobehavioral Reviews, 112, 95-106. https://doi.org/10.1016/j.neubiorev.2020.02.001
Matić, Z., Platiša, M. M., Kalauzi, A., & Bojić, T. (2020). Slow 0.1 Hz breathing and body posture induced perturbations of RRI and respiratory signal complexity and cardiorespiratory coupling. Frontiers in physiology, 11, 24. https://doi.org/10.3389/fphys.2020.00024
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Meehan, Z.M. & Shaffer, F. (2023). Adding Core Muscle Contraction to Wrist-Ankle Rhythmical Skeletal Muscle Tension Increases Respiratory Sinus Arrhythmia and Low-Frequency Power. Appl Psychophysiol Biofeedback. 48(1), 127-134. https://doi.org/10.1007/s10484-022-09568-w
McKeown, P. (2021). The breathing cure: Develop new habits for a healthier, happier, and longer life. Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E. & Cohen, T. (2017). Inhale to Breathe Away Pelvic Floor Pain and Enjoy Intercourse. Biofeedback, 45 (1), 21–24. https://doi.org/10.5298/1081-5937-45.1.04
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. https://doi.org/10.15540/nr.6.3.153
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07 or https://www.researchgate.net/publication/383151816_WHAT_ABOUT_THIS_Increase_Attention_Concentration_and_School_Performance_with_Posture_Feedback
Peper, E. & MacHose, M. (1993). Symptom prescription: Inducing anxiety by 70% exhalation. Applied Psychophysiology and Biofeedback, 18(3), 133-138. https://doi.org/10.1007/BF00999790
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. 45(4), 83–87. https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019a). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128-133. https://doi.org/10.15540/nr.6.3.12
Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512
PTI. (2023 August 3). Often suck your stomach in to look slimmer in pictures? It can lead to ‘hourglass syndrome.’ The Economic Times Panache. Accessed March 26, 2024. https://economictimes.indiatimes.com/magazines/panache/often-suck-your-stomach-in-to-look-slimmer-in-pictures-it-can-lead-to-hourglass-syndrome/articleshow/102392681.cms?from=mdr
Salah, H.M., Goldberg, L.R., Molinger, J., Felker, G.M., Applefeld, W., Rassaf, T., Tedford, R.J., Mirro, M., Cleland, J.GF., & Fudim, M. (2022). Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week, Journal of the American College of Cardiology, 80(17), 1647-1659. https://doi.org/10.1016/j.jacc.2022.08.760
Shaffer, F. & Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience,14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
Taub, E., Uswatte, G., Mark, V. W., Morris, D. M. (2006). The learned nonuse phenomenon: Implications for rehabilitation. Europa Medicophysica, 42(3), 241-256. https://pubmed.ncbi.nlm.nih.gov/17039223/
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Xiao, M., Zi-Qi, Y., Gong, Z.Q., Zhang, H., Duan, N.Y., Shi, Y.T,, Wei, G.X., Li, Y.F. (2017).The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front Psychol. 8(874). https://doi.org/10.3389/fpsyg.2017.00874