Are food companies responsible for the epidemic in diabetes, cancer, dementia and chronic disease and do their products need to be regulated like tobacco? Is it time for a class action suit?
Posted: July 15, 2023 Filed under: behavior, cancer, Evolutionary perspective, health, Nutrition/diet, self-healing | Tags: dementia, diabetes, diet, high fructose corn syrup, mortality, obsity, smoking, sugar, ultra-processed foods, UPF 2 CommentsAdapted from: Peper, E. & Harvey, R. (2024). Are Food Companies Responsible for the Epidemic in Diabetes, Cancer, Dementia and Chronic Disease and Do Their Products Need to Be Regulated Like Tobacco? Is It Time for a Class Action Suit? Thownsend Letter-the examiner of alternative medicine. https://www.townsendletter.com/e-letter-26-ultra-processed-foods-and-health-issues/
Erik Peper, PhD and Richard Harvey, PhD

Why are one third of young Americans becoming obese and at risk for diabetes?
Why are heart disease, cancer, and dementias occurring earlier and earlier? Is it genetics, environment, foods, or lifestyle?
Is it individual responsibility or the result of the quest for profits by agribusiness and the food industry?
Like the tobacco industry that sells products regulated because of their public health dangers, is it time for a class action suit against the processed food industry? The argument relates not only to the regulation of toxic or hazardous food ingredients (e.g., carcinogenic or obesogenic chemicals) but also to the regulation of consumer vulnerabilities. Addressing vulnerabilities to tobacco products include regulations such as how cigarette companies may not advertise their products for sale within a certain distance from school grounds.
Is it time to regulate nationally the installation of vending machines on school grounds selling sugar-sweetened beverages? Students have sensitivity to the enticing nature of advertised, and/or conveniently available consumable products such as ‘fast foods’ that are highly processed (e.g., packaged, preserved and practically imperishable). Whereas ‘processed foods’ have some nutritive value, and may technically pass as ‘nutritious’ food, the quality of processed ‘nutrients’ can be called into question. For the purpose of this blog other important questions to raise relate to ingredients which, alone or in combination, may contribute to the onset of or, the acceleration of a variety of chronic health outcomes related to various kinds of cancers, cardiovascular diseases, and diabetes.
It may be an over statement to suggest that processed food companies are directly responsible for the epidemic in diabetes, cancer, dementia and chronic disease and need to be regulated like tobacco. On the other hand, processed food companies should become much more regulated than they are now.
More than 80 years ago, smoking was identified as a significant factor contributing to lung cancer, heart disease and many other disorders. In 1964 the Surgeon Generals’ report officially linked smoking to deaths of cancer and heart disease (United States Public Health Service, 1964). Another 34 years pased before California prohibited smoking in restaurants in 1998 and, eventually inside all public buildings. The harms of smoking tobacco products were well known, yet many years passed with countless deaths and suffering which could have been prevented before regulation of tobacco products took place. Reviewing historical data there is about a 20 year delay (e.g., a whole generation) before death rates decrease in relation to when regulations became effective and smoking rates decreased, as shown in figure 1.
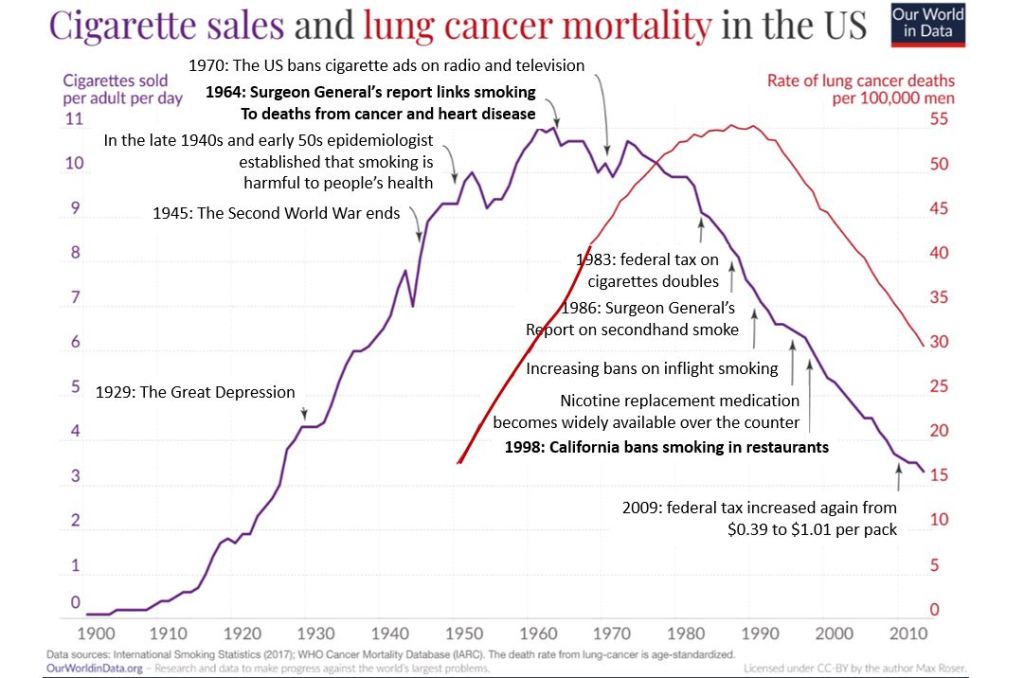
Figure 1. The relationship between smoking and lung cancer. Reproduced by permission from Roser, M. (2021). Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data.
During those interim years before government actions limited smoking more effectively, tobacco companies hid data regarding the harmful effects of smoking. Arguably, the ‘Big Tobacco’ industry paid researchers to publish data which could confuse readers about tobacco product harm. There is evidence of some published articles suggesting that the harm of cigarette smoking was a hoax– all for the sake of boosting corporate profits (Bero, 2005).
Now we are experiencing a similar problem with the processed food industry. It has been suggested that alongside smoking and vaping, opioid use, a sedentary ‘couch potato’ lifestyle, and lack of exercise, ultra-processed food (UPF) that we eat severely affects our health.
Ultra-processed foods, which for many constitutes a majority of calories ranging from 55% to over 80% of the food they eat, contain chemical additives that trick the tastebuds, mouth and eventually our brain to desire those processed foods and eat more of them (Srour et al., 2022).
What are ultra-processed foods? Any foods that your great grandmother would not recognize as food. This includes all soft drinks, highly processed chips, additives, food coloring, stabilizers, processed proteins, etc. Even oils such as palm oil, canola oil, or soybean are ultra processed since they heated, highly processed with phosphoric acid to remove gums and waxes, neutralized with chemicals, bleached, and deodorized with high pressure steam (van Tulleken, 2023).
The data is clear! Since the 1970s obesity and inflammatory disease have exploded after ultra-processed foods became the constituents of the modern diet as shown in figure 2.
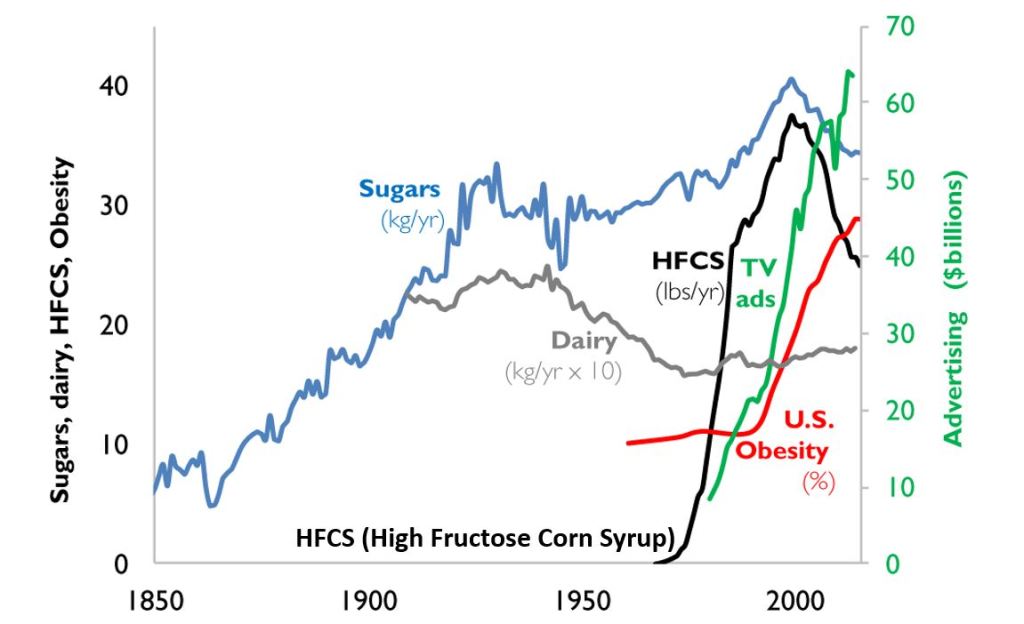
Figure 2. A timeline from 1850 to 2000 reflects the increase in use of refined sugar and high fructose corn syrup (HFCS) to the U.S. diet, together with the increase in U.S. obesity rate. The data for sugar, dairy and HFCS consumption per capita are from USDA Economic Research Service (Johnson et al., 2009) and reflects historical estimates before 1967 (Guyenet et al., 2017). The obesity data (% of U.S. adult population) are from the Robert Wood Johnson Foundation’s Trust for America’s Health. (stateofobesity.org). Total U.S. television advertising data are from the World Advertising Research Center (www.warc.com). The vertical measure (y–axis) for kilograms per year (kg/yr) on the left covers all data except advertising expenditures, which uses the vertical measure for advertising on the right. Reproduced by permission from Bentley et al, 2018.
This graph clearly shows a close association between the years that high fructose corn syrups (HFCS) were introduced into the American diet and an increase in TV advertising with corresponding increase in obesity. HFCS is an ultra-processed food and is a surrogate marker for all other ultra-processed foods. The best interpretation is that ultra-processed foods, which often contain HFCS, are a causal factor of the increase in obesity, and diabetes and in turn are risk factors for heart disease, cancers and dementias.
Ultra-processed foods are novel from an evolutionary perspective.
The human digestive system has only recently encountered sources of calories which are filled with so many unnatural chemicals, textures and flavors. Ultra-processed foods have been engineered, developed and product tested to increase the likelihood they are wanted by consumers and thereby increase sales and profits for the producers. These foods contain the ‘right amount’ processed materials to evoke the taste, flavor and feel of desired foods that ‘trick’ the consumer it eat them because they activate evolutionary preference for survival. Thus, these ultra-processed foods have become an ‘evolutionary trap’ where it is almost impossible not to eat them. We eat the food because it capitalized on our evolutionary preferences even though doing so is ultimately harmful for our health (for a detailed discussion on evolutionary traps, see Peper, Harvey & Faass, 2020).
An example is a young child wanting the candy while waiting with her parents at the supermarket checkout line. The advertised images of sweet foods trigger the cue to eat. Remember, breast milk is sweet and most foods in nature that are sweet in taste, provide calories for growth and survival and are not harmful. Calories are essential of growth. Thus, we have no intrinsic limit on eating sweets unlike foods that taste bitter.
As parents, we wish that our children (and even adults) have self-control and no desire to eat the candy or snacks that is displayed at eye level (eye candy) especially while waiting at the cashier. When reflecting about food advertising and the promotion of foods that are formulated to take advantage of ‘evolutionary traps’, who is responsible? Is it the child, who does not yet have the wisdom and self-control or, is it the food industry that ultra-processes the foods and adds ingredients into foods which can be harmful and then displays them to trigger an evolutionary preference for food that have been highly processed?
Every country that has adapted the USA diet of ultra-processed foods has experienced similar trends in increasing obesity, diabetes, cardiovascular disease, etc. The USA diet is replacing traditional diets as illustrated by the availability of Coca-Cola. It is sold in over 200 countries and territories (Coca-Cola, 2023).
An increase in ultra-processed foods by 10 percent was associated with a 25 percent increase in the risk of dementia and a 14 per cent increase in the risk of Alzheimers’s (Li et al., 2022). More importantly, people who eat the highest proportion of their diet in ultra-processed foods had a 22%-62% increased risk of death compared to the people who ate the lowest proportion of processed foods (van Tulleken, 2023). In the USA, counties with the highest food swamp scores (the availability of fast food outlets in a county) had a 77% increased odds of high obesity-related cancer mortality (Bevel et al., 2023). The increase risk has also been observed for cardiovascular disease, coronary heart disease, cerebrovascular disease and all cause mortality as is shown in figure 3 (Srour et al., 2019; Rico-Campà et al., 2019).
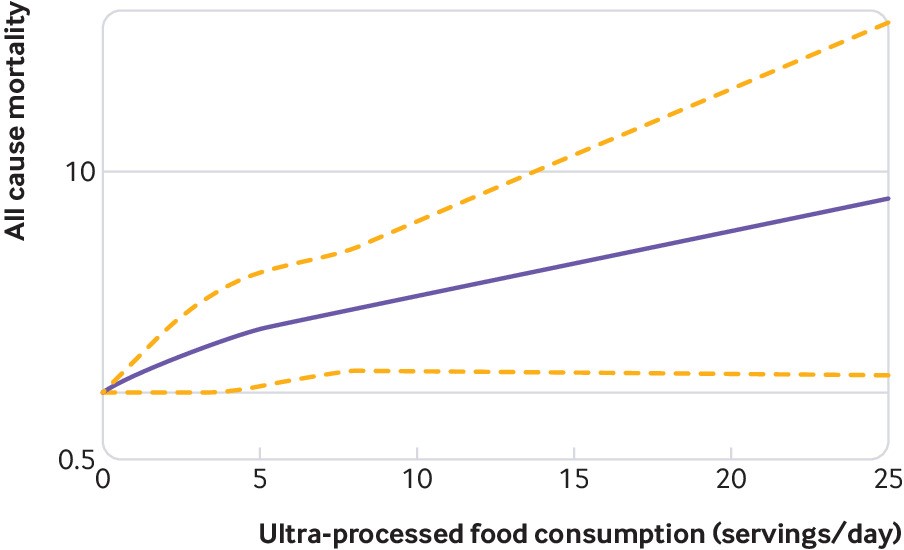
Figure 3. Association between consumption of ultra-processed foods and all cause mortality. Reproduced from Rico-Campà et al, 2019.
The harmful effects of UPF holds up even when correcting for the amount of sugars, carbohydrates or fats in the diet and controlling for socio economic variables.
The logic that underlies this perspective is based upon the writing by Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto). He provides an evolutionary perspective and offers broad and simple rules of health as well as recommendations for reducing UPF risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, added sugars, textured proteins, gums, stabilizers (guar gum, sodium alginate), emulsifiers (mono-and di-glycerides), modified starches, dextrose, palm stearin, and fats, colors and artificial flavoring or other ultra-processed food additives).
What can we do?
The solutions are simple and stated by Michael Pollan in his 2007 New York Times article, “Eat food. Not too much. Mostly Plants.” Eat foods that your great grandmother would recognize as foods (Pollan, 2009). Do not eat any of the processed foods that fill a majority of a supermarket’s space.
- Buy only whole organic natural foods and prepare them yourself.
- Request that food companies only buy and sell non-processed foods.
- Demand government action to tax ultra-processed food and limit access to these foods. In reality, it is almost impossible to expect people to choose healthy, organic foods when they are more expensive and not easily available in the American ‘food swamps and deserts’ (the presence of many fast food outlets or the absence of stores that have fresh produce and non-processed foods). We do have a choice. We can spend more money now for organic, health promoting foods or, pay much more later to treat illness related to UPF.
- It is time to take our cues from the tobacco wars that led to regulating tobacco products. We may even need to start class action suits against producers and merchants of UPF for causing increased illness and premature morbidity.
For more background information and the science behind this blog, read, the book, Ultra-processed people, by Chris van Tulleken.
Look at the following blogs for more background information.
References
Bentley, R.A., Ormerod, P. & Ruck, D.J. (2018). Recent origin and evolution of obesity-income correlation across the United States. Palgrave Commun 4, 146. https://doi.org/10.1057/s41599-018-0201-x
Bero, L. A. (2005). Tobacco Industry Manipulation of Research. Public Health Reports (1974-), 120(2), 200–208. http://www.jstor.org/stable/20056773
Bevel, M.S., Tsai, M., Parham, A., Andrzejak, S.E., Jones, S., & Moore, J.X. (2023). Association of Food Deserts and Food Swamps With Obesity-Related Cancer Mortality in the US. JAMA Oncol. 9(7), 909–916. https://doi.org/10.1001/jamaoncol.2023.0634
Coca-Cola. (2023). More on Coca-Cola. Accessed July 14, 2023. https://www.coca-cola.co.uk/our-business/faqs/how-many-countries-sell-coca-cola-is-there-anywhere-in-the-world-that-doesnt
Johnson, R.K., Appel, L.J., Brands, M., Howard, B.V., Lefevre, M., Lustig, R.H., Sacks, F., Steffen, L.M., & Wylie–Rosett, J. (2009). Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation, 120(10), 1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Li, H., Li, S., Yang, H., et al, 2022. Association of ultraprocessed food consumption with the risk of dementia: a prospective cohort study. Neurology, 99, e1056-1066. https://doi.org/10.1212/WNL.0000000000200871
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books, pp 18-22, 151. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/ref=sr_1_1?crid=1U9Y82YO4DKKP&keywords=erik+peper&qid=1689372466&sprefix=erik+peper%2Caps%2C187&sr=8-1
Pollan, M. (2007). Unhappy meals. The New York Times Magazine. https://www.nytimes.com/2007/01/28/magazine/28nutritionism.t.html
Pollan, M. (2009). Food Rules: An Eater’s Manual. New York: Penguin Books. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/014311638X/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1689373484&sr=8-2
Rico-Campà, A., Martínez-González, M. A., Alvarez-Alvarez, I., de Deus Mendonça, R., Carmen de la Fuente-Arrillaga, C., Gómez-Donoso, C., & Bes-Rastrollo, M. (2019). Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ; 365: l1949 https://doi.org/10.1136/bmj.l1949
Roser, M. (2021).Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data. Assessed July 13, 2023. https://ourworldindata.org/smoking-big-problem-in-brief
Srour, B., Fezeu, L.K., Kesse-Guyot, E.,Alles, B., Mejean, C…(2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé) BMJ,365:l1451. https://doi.org/10.1136/bmj.l1451
Srour, B., Kordahi, M. C., Bonazzi, E., Deschasaux-Tanguy, M., Touvier, M., & Chassaing, B. (2022). Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. The Lancet Gastroenterology & Hepatology. https://doi.org/10.1016/S2468-1253(22)00169-8
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. (Kindle Locations 5906-5908). https://www.amazon.com/Antifragile-Things-Disorder-ANTIFRAGILE-Hardcover/dp/B00QOJ6MLC/ref=sr_1_4?crid=3BISYYG0RPGW5&keywords=Antifragile%3A+Things+That+Gain+from+Disorder+%28Incerto%29&qid=1689288744&s=books&sprefix=antifragile+things+that+gain+from+disorder+incerto+%2Cstripbooks%2C158&sr=1-4
Van Tulleken, C. (2023). Ultra-processed people. The science behind food that isn’t food. New Yoerk: W.W. Norton & Company. https://www.amazon.com/gp/product/1324036729/ref=ox_sc_act_title_1?smid=ATVPDKIKX0DER&psc=1
United States Public Health Service. (1964). The 1964 Report on Smoking and Health. United States. Public Health Service. Office of the Surgeon General. https://profiles.nlm.nih.gov/spotlight/nn/catalog?f%5Bexhibit_tags%5D%5B%5D=smoking
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythm
Posted: July 4, 2023 Filed under: ADHD, behavior, computer, digital devices, education, emotions, Evolutionary perspective, health, laptops, screen fatigue, Uncategorized | Tags: anxiety, autism, bonding, circadian rhythms, depression, nature, still face experiment 3 Comments
Adapted from: Peper, E. Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation,10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Over the past two decades, there has been a significant increase in the prevalence of autism, Attention-Deficit/hyperactivity disorder (ADHD), anxiety, depression, and pediatric suicidal behavior. Autism rates have risen from 1 in 150 children in 2000 to 1 in 36 children in 2020 (CDC, 2023), while ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18-25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020), and depression rates for U.S. teens ages 12-17 have increased from 8% in 2007 to 13% in 2017 (Geiger & Davis, 2019; Walrave et al., 2022). Pediatric suicide attempts have also increased by 163% from 2009 to 2019 (Arakelyan et al., 2023), and during the COVID-19 pandemic, these rates have increased by more than 25% (WHO, 2022; Santomauro et al., 2021). In addition, the prevalence of these disorders has tripled for US adults during the pandemic compared to before (Ettman et al., 2020).
The rapid increase of these disorders is not solely due to improved diagnostic methods, genetic factors or the COVID-19 pandemic. The pandemic amplified pre-existing increasing trends. More likely, individuals who were at risk had their disorders triggered or amplified by harmful environmental and behavioral factors. Conceptually, Genetics loads the gun; epigenetics, behavior, and environment pull the trigger.
While behavioral strategies such as neurofeedback, Cognitive Behavior Therapy, biofeedback, meditation techniques, and pharmaceuticals can treat or ameliorate these disorders, the focus needs to be on risk reduction. In some ways, treatment can be likened to closing the barn doors after the horses have bolted.
Evolutionary perspective to reduce risk factors
Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto), provides an evolutionary perspective and offers simple rules of health by reducing risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, sugar, digital media).
- We do not need evidence of harm to claim that a drug or an unnatural procedure is dangerous. If evidence of harm does not exist, it does not mean harm does not exist.
- Only resort to medical techniques when the health payoff is very large (to save a life), exceeds its potential harm, such as incontrovertibly needed surgery or life-saving medicine (penicillin).
- Avoid the iatrogenics and negative side effects of prescribed medication.
Writer and scholar Taleb’s suggestions are reminiscent of the perspective described by the educator Joseph C. Pearce (1993) in his book, Evolution’s End. Pearce argued that modern lifestyles have negatively affected the secure attachment and bonding between caregivers and infants. The lack of nurturing and responsive caregiving in early childhood may lead to long-term emotional and psychological problems. He points out that we have radically adapted behaviors that differ from those that evolved over thousands of generations and that allowed us to thrive and survive. In the last 100 years, babies have often been separated from their mothers at birth or early infancy by being put in a nursery or separate room, limited or no breastfeeding with the use of formula, exposure to television for entertainment, lack of exploratory play outdoors, and the absence of constant caretakers in high-stress and unsafe environments.
As Pearce pointed out, “If you want true learning, learning that involves the higher frontal lobes – the intellectual, creative brain – then again, the emotional environment must be positive and supportive. This is because at the first sign of anxiety the brain shifts its functions from the high, prefrontal lobes to the old defenses of the reptilian brain… These young people need audio-vocal communication, nurturing, play, body movement, eye contact, sweet sounds and close heart contact on a physical level” (Mercogliano & Debus, 1999).
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past. The proposed recommendations are based upon Talib’s perspective that anything that was not part of our evolutionary past is probably harmful; thus, it is wise to remove the unnatural/unfamiliar and adopt the precautionary principle, which states that if evidence of harm does not exist, it does not mean harm does not exist (Kriebel et al., 2010).
This article is the first of a three-part series. Part 1 focuses on increasing reciprocal communication between infant and caretaker, reducing screen time, and re-establishing circadian rhythms; Part 2 focuses on reducing exposure to neurotoxins, eliminating processed foods, and supporting the human biome; and Part 3 focuses on respiration and movement.
Part 1- Increase bonding, reduce screen time, and re-establish circadian rhythms
Increase bonding between infant and caretaker
Infants develop emotional communication through reciprocal interactions with their caregivers, during which the caregiver responds to the infant’s expressions. When this does not occur, it can be highly stressful and detrimental to the infant’s development. Unfortunately, more and more babies are emotionally and socially isolated while their caregivers are focussed on, and captured by, the content on their digital screens. Moreover, infants and toddlers are entertained (babysat) by cellphones and tablets instead of dynamically interacting with their caretakers. Screens do not respond to the child’s expressions; the screen content is programmed to capture the infant’s attention through rapid scene changes. Without reciprocal interaction, babies often become stressed, as shown by the research of developmental psychologist Professor Edward Tronick, who conducted the “Still Face” experiment (Tronick & Beeghly, 2011; Weinberg et al, 2008).
The “Still Face” experiment illustrated what happens when caregivers are not responding to infants’ communication. The caregivers were asked to remain still and unresponsive to their babies, resulting in the infants becoming increasingly distressed and disengaged from their surroundings. Not only does this apply to infants but also to children, teenagers and older individuals. Watch the short Still Face experiment, which illustrates what happens when the caretaker is not responding to the infant’s communication.
Recommendation. Do not use cellphone and digital media while being with an infant in the first two years of life. It is important for caregivers to limit their cellphone use and prioritize reciprocal interactions with their infants for healthy emotional and psychological development.
Reduce screen time (television, social media, streaming videos, gaming)[1]
From an evolutionary perspective, screen time is an entirely novel experience. Television, computers, and cellphones are modern technologies that have significantly impacted infants’ and young people’s development. To grow, infants, toddlers, and children require opportunities to explore the environment through movement, touch, and play with others, which is not possible with screens. Research has shown that excessive screen time can negatively affect children’s motor development, attention span, socialization skills, and contribute to obesity and other health problems (Hinkley et al., 2014; Carson et al., 2016; Mark, 2023).
When four-year-olds watch fast-paced videos, they exhibit reduced executive functions and impulse control, which may be a precursor for ADHD, compared to children who engage in activities such as drawing (Lillard & Peterson, 2011; Mark, 2023).
Furthermore, excessive screen time and time spent on social media are causal in increasing depression in young adults-–as was discovered when Facebook became available at selected universities. Researchers compared the mental health of students at similar universities where Facebook was or was not available and observed how the students’ mental health changed when Facebook became available (Braghieri et al., 2022). Their research showed that “College-wide access to Facebook led to an increase in severe depression by 7% and anxiety disorders by 20%. In total, the negative effect of Facebook on mental health appeared to be roughly 20% the magnitude of what is experienced by those who lose their job” (Walsh, 2022).
Exposure to digital media has also significantly reduced our attention span from 150 seconds in 2004 to an average of 44 seconds in 2021. The shortening of attention span may contribute to the rise of ADHD and anxiety (Mark, 2022, p. 96).
Recommendations: Reduce time spent on social media, gaming, mindlessly following one link after the other, or watching episode after episode of streaming videos. Instead, set time limits for screen use, turn off notifications, and prioritize in-person interactions with friends, family and colleagues while engaging in collaborative activities. Encourage children to participate in physical and social activities and to explore nature.
To achieve this, follow the guidelines from the American Academy of Pediatrics’ recommendation on screen time (Council on Communications and Media, 2016), which suggest these limits on screen time for children of different age groups:
- Children under 18 months of age should avoid all screen time, except for video chatting with family and friends.
- Children aged 18-24 months should have limited screen time, and only when watched together with a caretaker.
- Children aged 2 to 5 years should have no more than one hour of screen time per day with parental supervision.
- For adolescents, screen and social media time should be limited to no more than an hour a day.
In our experience, when college students reduce their time spent on social media, streaming videos, and texting, they report that it is challenging; however, they then report an increase in well-being and performance over time (Peper et al., 2021). It may require more effort to provide children with actual experiential learning and entertainment than allowing them to use screens, but it is worthwhile. Having children perform activities and play outdoors–in a green nature environment–appears to reduce ADHD symptoms (Louv, 2008; Kuo & Taylor, 2004).
Reestablish circadian (daily) rhythms
Our natural biological and activity rhythms were regulated by natural light until the 19th century. It is hard to imagine not having light at night to read, to work on the computer, or to answer email. However, light not only illuminates, but also affects our physiology by regulating our biological rhythms. Exposure to light at night can interfere with the production of melatonin, which is essential for sleep. Insufficient sleep affects 30% of toddlers, preschoolers, and school-age children, as well as the majority of adolescents. The more media is consumed at bedtime, the more bedtime is delayed and total sleep time is reduced (Hale et al., 2018). Reduced sleep is a contributing factor to increased ADHD symptoms of inattention, hyperactivity and impulsivity (Cassoff et al., 2012).
Recommendations: Support the circadian rhythms. Avoid screen time one hour before bedtime. This will reduce exposure to blue light and reduce sympathetic arousal triggered by the content on the screen or reactions to social media and emails. Sleep in total darkness, and establish a regular bedtime and waking time to avoid “social jetlag,” which can negatively affect health and performance (Caliandro et al., 2021). Implement sleep hygiene strategies such as developing a bedtime ritual to improve sleep quality (Stager et al., 2023; Suni, 2023). Thus, go to bed and wake up at the same time each day, including weekends. Avoid large meals, caffeine, and alcohol before bedtime. Consistency is key to success.
Conclusion
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past, and explore strategies that support behaviors that have allowed the human being to thrive and survive. Improve clinical outcomes and optimize health by enhancing reciprocal communication interactions, reducing screen time and re-establishing the circadian rhythm.
References
Arakelyan, M., Freyleue, S., Avula, D., McLaren, J.L., O’Malley, A.J., & Leyenaar, J.K. (2023). Pediatric Mental Health Hospitalizations at Acute Care Hospitals in the US, 2009-2019. JAMA, 329(12), 1000–1011. https://doi.org/10.1001/jama.2023.1992
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Caliandro, R., Streng, A.A., van Kerkhof, L.W.M., van der Horst, G.T.J., & Chaves, I. (2021). Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients, 13(12), 4543. https://doi.org/10.3390/nu13124543
Carson, V., Tremblay, M.S., Chaput, J.P., & Chastin, S.F. (2016). Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab, 41(6 Suppl 3), S294-302. https://doi.org/10.1139/apnm-2016-0026
Cassoff, J., Wiebe, S.T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nat Sci Sleep, 4, 73-80. https://doi.org/10.2147/NSS.S31269
CDC. (2022). Attention-Deficit/hyperactivity disorder (ADHD): ADHD through the years. Centers for Disease Control and Prevention. Assessed March 27, 2023. https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. (2023). Data & Statistics on Autism Spectrum Disorder. CDC Centers for Disease Control and Prevention. Assessed March 25, 2023. https://www.cdc.gov/ncbddd/autism/data.html
Council on Communications and Media. (2016). Media and young minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M.,& Galea, S. (2020), Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Geiger, A.W. & Davis, L. (2019). A growing number of American teenagers-particularly girls-are facing depression. Pew Research Center. Accessed March 28, 2023.
Goodwin, R.D., Weinberger, A.H., Kim, J.H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. J Psychiatr Res. 130, 441-446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hale, L., Kirschen, G/W., LeBourgeois, M.K., Gradisar, M., Garrison, M.M., Montgomery-Downs, H., Kirschen, H., McHale, S.M., Chang, A.M., & Buxton, O.M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc Psychiatr Clin N Am, 27(2),229-245. https://doi.org/10.1016/j.chc.2017.11.014
Hinkley, T., Verbestel, V., Ahrens, W., Lissner, L., Molnár, D., Moreno, L.A., Pigeot, I., Pohlabeln, H., Reisch, L.A., Russo, P., Veidebaum, T., Tornaritis, M., Williams, G., De Henauw, S., De Bourdeaudhuij, I; IDEFICS Consortium. (2014). Early childhood electronic media use as a predictor of poorer well-being: a prospective cohort study. JAMA Pediatr,. May;168(5):485-92. https://doi.org/10.1001/jamapediatrics.2014.94
Kriebel, D., Tickner, J., Epstein, P., Lemons, J., Levins, R., Loechler, E.L., Quinn, M., Rudel, R., Schettler, T., Stoto, M. (2001). The precautionary principle in environmental science. Environ Health Perspect, 109(9):871-6. https://doi.org/10.1289/ehp.01109871
Kuo. F.E. & Taylor, A.F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 94(9),1580-6. https://doi.org/10.2105/ajph.94.9.1580
Lillard, A.S. & Peterson, J. The immediate impact of different types of television on young children’s executive function. Pediatrics, 128(4), 644-9. https://doi.org/10.1542/peds.2010-1919
Louv, R. (2008). Last Child in the Woods: Saving Our Children from Nature-Deficit Disorder. Algonquin Books. Chapel Hill, NC: Algonquin Books
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press.
Mercogliano, C. & Debus, K. (1999). Nurturing Heart-Brain Development Starting With Infants 1999 Interview with Joseph Chilton Pearce. Journal of Family Life, 5(1). https://www.michaelmount.co.za/nurturing-heart-brain-development-starting-with-infants-1999-interview-with-joseph-chilton-pearce/
Pearce, J.C. (1993). Evolutions’s End. New York: HarperOne.
Peper, E., Wilson, V., Martin, M., Rosegard, E., & Harvey, R. (2021). Avoid Zoom fatigue, be present and learn. NeuroRegulation, 8(1), 47–56. https://doi.org/10.15540/nr.8.1.47
Santomauro, D.F., Mantilla Herrera, A.M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D.M., Abbafati, C., Adolph, C., …. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(103121700-1712., https://doi.org/10.1016/S0140-6736(21)02143-7
Stager, L.M., Caldwell, A., Bates, C., & Laroche, H. (2023). Helping kids get the sleep they need. Society of Behavioral Medicine. Accessed March 29, 2023 https://www.sbm.org/healthy-living/helping-kids-get-the-sleep-they-need?gclid=Cj0KCQjww4-hBhCtARIsAC9gR3ZM7v9VSvqaFkLnceBOH1jIP8idiBIyQcqquk5y_RZaNdUjAR9Wpx4aAhTBEALw_wcB
Suni, E. (2023). Sleep hygiene- What it is, why it matters, and how to revamp your habits to get better nightly sleep. Sleep Foundation. Accessed March 29, 2023. https://www.sleepfoundation.org/sleep-hygiene
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto) Random House Publishing Group. (Kindle Locations 5906-5908).
Tronick, E. & Beeghly, M. (2011).Infants’ meaning-making and the development of mental health problems. Am Psychol, 66(2),107-19. https://doi.org/10.1037/a0021631
Walrave, R., Beerten, S.G., Mamouris, P. et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 23, 163 (2022). https://doi.org/10.1186/s12875-022-01769-w
Walsh, D. (2022 September 14). Study: Social media use linked to decline in mental health. MIT Management Ideas Made to Matter. Accessed March 28, 2023. https://mitsloan.mit.edu/ideas-made-to-matter/study-social-media-use-linked-to-decline-mental-health#:~:text=College%2Dwide%20access%20to%20Facebook,with%20either%20psychotherapy%20or%20antidepressants
Weinberg, M.K., Beeghly, M., Olson, K.L., & Tronick, E. (2008). A Still-face Paradigm for Young Children: 2½ Year-olds’ Reactions to Maternal Unavailability during the Still-face. J Dev Process, 3(1):4-22. https://pubmed.ncbi.nlm.nih.gov/22384309/
WHO (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. Assessed march 26, 2023. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
[1] The critique of social media does not imply that there are no benefits. If used judiciously, it is a powerful tool to connect with family and friends or access information.
Mouth breathing and tongue position: a risk factor for health
Posted: June 8, 2023 Filed under: ADHD, behavior, Breathing/respiration, cognitive behavior therapy, Evolutionary perspective, healing, health, Nutrition/diet, self-healing, Uncategorized | Tags: babies, breastfeedging, development, infants, jaw, mouth breathing, neurocognitive develoment, nose breathing, sleep, tongue-tie Leave a commentErik Peper, PhD, BCB and Ron Swatzyna, PhD, LCSW, BCB, BCN
Adapted from: Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512

Breathing usually occurs without awareness unless there are problems such as asthma, emphysema, allergies, or viral infections. Infant and child development may affect how we breathe as adults. This blog discusses the benefits of nasal breathing, factors that contribute to mouth breathing, how babies’ breastfeeding and chewing decreases the risk of mouth breathing, recommendations that parents may implement to support healthy development of a wider palate, and the embedded video presentation, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development, by Karindy Ong, MA, CCC-SLP, CFT, .
Benefits of nasal breathing
Breathing through the nose filters, humidifies, warms, or cools the inhaled air as well as reduces the air turbulence in the upper airways. In addition, the epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation. Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. This slower breathing also facilitates sympathetic parasympathetic balance and reduces airway irritation.
Mouth breathing
Some people breathe predominantly through their mouth although nose breathing is preferred and health promoting. Mouth breathing negatively impacts the ability to perform during the day as well as affect our cognitions and mood (Nestor, 2020). It contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded mis-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
One recommendation to reduce mouth breathing is to tape the mouths closed with mouth tape (McKeown, 2021). Using mouth tape while sleeping bolsters nose breathing and may help people improve sleep, reduce snoring, and improves alertness when awake (Lee et al, 2022).
Experience how mouth breathing affects the throat and upper airway
Inhale quickly, like a gasp, as much air as possible through your open mouth. Exhale letting the air flow out through your mouth. Repeat once more.
Inhale quickly as much air through the nose, then exhale by allow the airflow out through the nose. Repeat once more.
What did you observe? Many people report that rapidly inhaling through the mouth causes the back of the throat and even upper airways to feel drier and irritated. This does not occur when inhaling through the nose. This simple experiment illustrates how habitual mouth breathing may irritate the airways.
Developmental behavior that contributes to mouth breathing
The development of mouth breathing may begin right at birth when the mouth, tongue, jaw and nasal area are still developing. The arch of the upper palate forms the roof of the oral cavity that separates the oral and nasal cavities. When the palate and jaw narrows, the arch of the palate increases and pushes upwards into the nasal area. This reduces space in the nasal cavity for the air to flow and obstructs nasal breathing. The highly vaulted palate is not only genetically predetermined but also by how we use our tongue and jaw from birth. The highly arched palate is only a recent anatomical phenomena since the physical structure of the upper palate and jaw from the pre- industrial era was wider (less arched upper palate) than many of our current skulls (Kahn & Ehrlich, 2018).
The role of the tongue in palate development
After babies are born, they breastfeed by sucking with the appropriate tongue movements that help widen the upper palate and jaw. On the other hand, when babies are bottle fed, the tongue tends to move differently which causes the cheek to pull in and the upper palate to arch which may create a high narrow upper palate and making the jaw narrower. There are many other possible factors that could cause mouth breathing such as tongue-tie (ankyloglossia), septal deviation, congenital malformation, enlarged adenoids and tonsils (Aden tonsillar hyperplasia), inflammatory diseases such as allergic rhinitis (Trabalon et al, 2012). Whatever the reasons, the result of the impoverished tongue movement and jaw increases the risk for having a higher arched upper palate that impedes nasal breathing and contributes to habitual mouth breathing.
The forces that operate on the mouth, jaw and palate during bottle feeding may be similar to when you suck on straw and the cheeks coming in with the face narrowing. The way the infants are fed will change the development of the physical structure that may result in lifelong problems and may contribute to developing a highly arched palate with a narrow jaw and facial abnormalities such as long face syndrome (Tourne, 1990).
To widen the upper palate and jaw, the infant needs to chew, chew and tear the food with their gums and teeth. Before the industrialization of foods, children had to tear food with their teeth, chew fibrous foods or gnaw at the meat on bones. The chewing forces allows the jaw to widen and develop so that when the permanent teeth are erupting, they would more likely be aligned since there would be enough space–eliminating the need for orthodontics. On the other hand, when young children eat puréed and highly processed soft foods (e.g., cereals soaked in milk, soft breads), the chewing forces are not powerful enough to encourage the widening of the palate and jaw.
Although the solution in adults can be the use of mouth tape to keep the mouth closed at night to retrain the breathing pattern, we should not wait until we have symptoms. The focus needs to be on prevention. The first step is an assessment whether the children’s tongue can do its job effectively or limited by tongue-tie and the arch of the palate. These structures are not totally fixed and can change depending on our oral habits. The field of orthodontics is based upon the premise that the physical structure of the jaw and palate can be changed, and teeth can be realigned by applying constant forces with braces.
Support healthy development of the palate and jaw
Breastfeed babies (if possible) for the first year of life and do NOT use bottle feeding. When weaning, provide chewable foods (fruits, vegetable, roots, berries, meats on bone) that was traditionally part of our pre-industrial diet. These foods support in infants’ healthy tongue and jaw development, which helps to support the normal widening of the palate to provide space for nasal breathing.
Provide fresh organic foods that children must tear and chew. Avoid any processed foods which are soft and do not demand chewing. This will have many other beneficial health effects since processed foods are high in simple carbohydrates and usually contain color additives as well as traces of pesticides and herbicides. The highly processed foods increase the risk of developing depression, type 2 diabetes, inflammatory disease, and colon cancer (Srour et al., 2019).
Sadly, the USA allows much higher residues of pesticide and herbicides that act as neurotoxins than are allowed in by the European Union. For example, the acceptable level of the herbicide glyphosate (Round-Up) is 0.7 parts per million in the USA while in the acceptable level is 0.01 parts per million in European countries (Tano, 2016; EPA, 2023; European Commission, 2023). The USA allows this higher exposure even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbò et al., 2022).
The negative effects of herbicides and pesticides are harmful for growing infants. Even fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021) and organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010).
To implement these basic recommendations are very challenging. It means the mother has to breastfeed her infant during the first year of life. This is often not possible because of socioeconomic inequalities; work demands and medical complications. It also goes against the recent cultural norm that fathers should participate in caring for the baby by giving the baby a bottle of stored breast milk or formula.
From our perspective, women who give birth must have a year paid maternity leave to provide their infants with the best opportunity for health (e.g., breast-feeding, emotional bonding, and reduced financial stress). As a society, we have the option to pay the upfront cost now by providing a year- long maternity leave to mothers or later pay much more costs for treating chronic conditions that may have developed because we did not support the natural developmental process of babies.
Relevance to the field of neurofeedback and biofeedback
Clinicians often see clients, especially children with diagnostic labels such as ADHD who have failed to respond to numerous psychotherapies and pharmacotherapies. In the recent umbrella review and meta-analytic evaluation of recent meta-analyses, Leichsenring et al. (2022) found only small benefits overall for both types of intervention. They suggest that a paradigm shift in research seems to be required to achieve further progress in resolving mental health issues. As the past director of National Institute of Health, Dr. Thomas Insel pointed out that the Diagnostic and Statistical Manual of Mental Disorders (DSM) is not a valid instrument and should be a big wake up call for all of us to think outside the box (Insel, 2009). One factor that starts right at birth is the oral cavity development by dysfunctional tongue movements.
We want to make all of you aware of a serious issue in children that you may come across. For those of us who work with children children, we need to ask their parents about the following: tongue-tie, mouth breathing, bedwetting, high-vaulted palate, thumb sucking, abnormal eating issues, apraxia, dysarthria, and hypotonia. Research suggests that the palates of these children are so arched that the tongue cannot do its job effectively, causing multiple issues which may be related.
Please view the webinar from May 17, 2023. Presented by Karindy Ong, MA, CCC-SLP, CFT, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development. The presentation explains the developmental process of the role the tongue plays and how it contributes to nasal breathing. Please pass it on to others who may have interest.
References
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians.
Insel, T.R. (2009). Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry, 66(2), 128-133. https://doi.org/10.1001/archgenpsychiatry.2008.540
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lee, Y.C., Lu, C.T., Cheng, W.N., & Li, H.Y. (2022).The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare (Basel), 10(9), 1755. https://doi.org/10.3390/healthcare10091755
Leichsenring, F., Steinert, C., Rabung, S. and Ioannidis, J.P.A. (2022), The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry, 21: 133-145. https://doi.org/10.1002/wps.20941
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath/dp/0593191358/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1686191995&sr=8-1
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Srour, B. et al. (2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé).BMJ, 365. https://doi.org/10.1136/bmj.l1451
Tano, B. (2016). The Layman’s Guide to Integrative Immunity. Integrative Medical Press. https://www.amazon.com/Laymans-Guide-Integrative-Immunity-Discover/dp/0983419299/_
Tourne, L.P. (1990). The long face syndrome and impairment of the nasopharyngeal airway. Angle Orthod, 60(3):167-76. https://doi.org/10.1043/0003
Trabalon, M. & Schaal, B. (2012). It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr, 207605. https://doi.org/10.1155/2012/207605
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Healing from vulvodynia
Posted: May 4, 2023 Filed under: behavior, biofeedback, Breathing/respiration, emotions, healing, health, Pain/discomfort, relaxation, self-healing, Uncategorized | Tags: muscle tension, pelvic floor pain, therapeutic relationship, triggers for illness, vulvodynia Leave a commentPamela Jertberg and Erik Peper
Adapted from: Jertberg, P. & Peper, E. (2023). The healing of vulvodynia from the client’s perspective. Biofeedback, 51 (1), 18–21. https://doi.org/10.5298/1081-5937-51.01.02

This introspective report describes how a young woman who experienced a year-long struggle with vulvodynia, or vulvar vestibulitis, regained her health through biofeedback training and continues to be symptom-free 7 years after the intervention. This perspective may offer insight into factors that promote health and healing and provide an approach to reduce symptoms and promote health. The methodology of this case was described previously by Peper et al. (2015).
The Client’s Experience
I have been a healthy young woman my whole life. Growing up in a loving, dedicated family, I always ate home-cooked meals, went to bed at a reasonable time, and got plenty of exercise by playing with my family members and friends. I never once thought that at age 23 I might be at risk of undergoing vulvar surgery. There are many factors that contributed to the genesis of my vulvar pain, and many other factors that worsened this pain. Traditional medicine did not help me, and I did not find relief until I met my biofeedback practitioner, who taught me biofeedback. Through the many strategies I learned, such as visualization, diaphragmatic breathing techniques, diet tips, and skills to reframe my thoughts, I finally began to feel relief and hope. Practicing all these elements every day helped me overcome my physical pain and enjoy a normal life once again. Today, I do not have any vulvar discomfort. I am so grateful to my biofeedback practitioner for the many skills he taught me. I can enjoy my daily activities once again without experiencing pain. I have been given a second chance at loving life, and now I have learned the techniques that will help me sustain a more balanced path for the rest of my life. Seven years later, I am healthy and have no symptoms.
Triggers for Illness
Not Having a Positive Relationship with the Doctor
The first factor that aggravated my pain was having a doctor with whom I did not have a good relationship. Although the vulvar specialist I was referred to had treated hundreds of women with vulvar vestibulitis, his methods were very traditional: medicine, low oxalate diet, ointments, and surgery. Whenever I left his office, I would cry and feel like surgery was the only option. Vaginal surgery at 23 was one of the scariest and most unexpected thoughts my brain had ever considered. The doctor never thought of the impact that his words and treatment would have on my mental state.
Depression
Being depressed also triggered more pain. Whenever I would have feelings of hopelessness and create irrational beliefs in my mind (“I will never get better,” “I will never have sex again,” “I am not a woman anymore”), my physical pain would increase. Having depression only triggered more depression and pain, and this became a vicious cycle. The depression deeply affected my relationships with my boyfriend, friends, and family and my performance in my college classes.
Being Sedentary
Being sedentary and not exercising also increased my pain. At first, I believed that the mere act of sitting down hurt me due to the direct pressure on the area, but after a few months I came to realize that it was inactivity itself that triggered pain. Whenever I would sit for too long writing a paper or I would stay home all day because of my depression, my pain would increase, perhaps because I was inhibiting circulation. Still, when I am inactive most of the day, I feel lethargic and bloated. When I exercise, the pain goes away 100%. Exercise is almost magical.
Stress
Stress is the worst trigger for pain. Throughout my life, I always strived to be perfect in every way, meaning I was stressed about the way I looked, performed in school, drove, etc. Through the sessions with my biofeedback practitioner, I learned that my body was in a state of perpetual stress and tightness, which induced pain in certain areas. My body’s way of releasing such tension was to send pain signals to my vulvar area, perhaps because of a yeast infection a couple of months back. Still, if I become very stressed, I will feel pain or tightness in certain parts of my body, but now I have strategies for performing proper stress-relieving techniques.
Processed Foods
Junk food affects me instantly. When I eat processed foods for a week straight, I feel groggy, bloated, lethargic, and in pain. Processed sugar, white flour, and salt are a few of the foods that make the pain increase. I used to love sugar, so I would enjoy the occasional milkshake and cheeseburger and feel mostly okay. However, in times of stress it became crucial for me to learn to refrain from any junk food, because it would worsen my vulvar pain and increase my overall stress levels.
Menstruation
Menstruation is unavoidable, and unfortunately it would always worsen my vulvar pain. Right about the time of my period, my sensitivity and pain would massively increase. Sometimes as my pain would increase incredibly, I would question myself: “What am I doing wrong?” Then, I would remember: “Oh yes, I am getting my period in a few days.” The whole area became very sensitive and would get irritated easily. It became imperative to listen to my body and nurture myself especially around that time of the month.
Triggers for Healing
A Good Doctor
Just as I learned which factors triggered the pain, I also learned how to reduce it. The most important factor that helped me find true relief was meeting a good health professional (which could be a healer, nurse, or professor). The first time I met my biofeedback practitioner and told him about my issues, he really listened, gave me positive feedback, and even made jokes with me. To this day we still have a friendship, which has really aided me in getting better. In contrast to the vulvar specialist, I would leave the biofeedback practitioner’s office feeling powerful, able to defeat vulvodynia, and truly happy. Just having this support from a professional (or a friend, boyfriend, or relative) can make all the difference in the world. I don’t know where I would be right now if I hadn’t worked with him.
Positive Thoughts and Beliefs
Along with having a good support group, having positive thoughts and believing in a positive result helped me greatly. When I actually set my mind to feel “happy” and to believe that I was getting better, I began to really heal. After months of being depressed and feeling incomplete, when I began to practice mantras such as “I am healing,” “I am healthy,” and “I am happy,” my pain began to go away, and I was able to reclaim my life.
Journaling
One of the ways in which “happiness” became easier to achieve was to journal every day. I would write everything: from my secrets to what I ate, my pain levels, my goals for the day, and my symptoms. Writing down everything and knowing that no one would ever read it but me gave me relief, and my journal became my confidante. I still journal every day, and if I forget to write, the next day I will write twice as much. Now that writing has become a habit and a hobby, it is hard to imagine my life without that level of introspection.
Meditation
Although I would do yoga often, I would never sit and meditate. I began to use Dr. Peper’s guided meditations and Dr. Kabat-Zinn’s CD (Kabat-Zinn, 2006; Peper et al., 2002). The combination of these meditation techniques, whether on different days or on the same day, helped me focus on my breathing and relax my muscles and mind. Today, I meditate at least 20 min each day, and I feel that it helps me see life through a more willing and patient perspective. In addition, through meditation and deep breathing I have learned to control my pain levels, concentration, and awareness.
Imagery and Visualization
Imagery is a powerful tool that allowed me to heal faster. My biofeedback practitioner instructed me to visualize how I wanted to feel and look. In addition, he suggested that I draw and color how I was feeling at any given moment, my imagined healing process, and how I would look and feel after the healing process had traveled throughout my body (Peper et al., 2022). It is still amazing to me how much imagery helped me. Even visualizing here and there throughout the day helped. Now I envision how I want to feel as a healthy woman, I take a deep breath, and as a I breathe out I let my imagined healing process go through my body into all my tight areas along with the exhalation.
Biofeedback
Biofeedback is the single strategy that helped me the most. During my first session with my biofeedback practitioner, he pointed out that my muscles were always contracted and stressed and that I was not breathing diaphragmatically. As I learned how to take deep belly breaths, I began to feel the tight areas in my body loosen up. I started to practice controlled breathing 20 min every day. Through biofeedback, my body and muscles became more relaxed, promoting circulation and ultimately reducing the vulvar pain.
Regular Exercise and Yoga
Exercising daily decreased my pain and improved the quality of my life greatly. When I first started experiencing significant vulvar pain, I stopped exercising because I felt that movement would aggravate the pain. To my surprise, the opposite was true. Being sedentary increased the feelings of discomfort, whereas exercising released the tension. The exercise I found most helpful was yoga because it is meditation in movement. I became so focused on my breathing and the poses that my brain did not have time to think about anything else. After attending every yoga class, I felt like I could take on anything. Swimming, Pilates, and gentle cardiovascular exercises have also helped me greatly in reducing stress and feeling great.
Sex
Although sex was impossible for almost a year due to the pain, it became possible and even enjoyable after implementing other relaxation strategies. When I first reintroduced sex back into my life, my partner at the time and I would go gently and stop if it hurt my vulvar area at all. Today, sex again is joyful. Being able to engage in intercourse has boosted my self-esteem and helped me feel sexy again, which empowers me to keep practicing the relaxation techniques.
Listening to the Mind-Body Connection
The mind-body connection is present in all of us, but I am fortunate to have a very strong connection. My thoughts influence my body almost instantly, which is why when I would get depressed my pain would increase, and when I would see my biofeedback practitioner or believe in a good outcome, my pain would decrease. Being aware of this connection is crucial because it can help me or hurt me greatly. After a few months of practicing the relaxation strategies, I saw a different gynecologist and one dermatologist. Both professionals said that there was nothing wrong with my vulvar area—that maybe I just felt some irritation due to the medicines I had previously taken and my current stress. They said that there was no way I needed surgery. When I heard these opinions, I began to feel instantly better—thus proving that my thoughts (and even others’ thoughts) affect my body in significant ways.
Although today I am 100% better, I still experience pain and tightness in my body when I experience the “illness factors” I mentioned above. I still have to remember that feeling healthy and good is a process, not a result, and that even if I feel better one day that does not mean I can stop all my new healthy habits. To completely cure vulvodynia, I needed to change my life habits, perspective, and attitude toward the illness and life. I needed to make significant changes, and now my biggest challenge is to stick to those changes. Biofeedback, imagery, meditation, good food, and exercise are not just treatments that I begin and end on a certain day, but rather they have become essential components of my life forever.
My life with vulvodynia was ultimately a journey of introspection, decision making, and life-changing habits. I struggled with vulvar pain for over a year, and during that year I experienced severe symptoms, depression, and the loss of several friendships and relationships. I felt old, hopeless, useless, and powerless. When I began to incorporate biofeedback, relaxation techniques, journaling, visualization, a proper diet, and regular exercise, life took a turn for the better. Not only did my vulvar pain begin to decrease, but the quality of my overall life improved and I regained the self-confidence I had lost. I became happy, hopeful, and proactive. Even though I practiced the relaxation strategies every day, the pain did not go away in a day or even a month. It took me several months of diligent practice to truly heal my vulvar pain. Even today, such practices have carried on to all areas of my life, and now there is not a day when I do not meditate, even for 5 min.
As paradoxical as it may seem, vulvodynia was a blessing in disguise. I believe that vulvodynia was my body’s way of signaling to me that many areas of my life were in perpetual stress: my pelvic floor, my thoracic breathing, my romantic relationship at the time, etc. When I learned to let go and truly embrace my life, I began to feel relief. I became less irritable and more patient and understanding, with both my body and the outside world. The best advice I can give a woman with vulvar symptoms or any person with otherwise inexplicable chronic pain is to apply the strategies that work for you and stick to them every day—even on the days when you want to go astray. When I started to focus on what my body needed to be nurtured and to live my life and do the things I truly wanted to do, I became free. Today, I live in a way that allows me to find peace, serenity, pride, and fun. I live exactly the way I want to, and I find the time to follow my passions. Vulvodynia, or any kind of chronic pain, does not define who we are. We define who we are.
Conclusion
This introspective account of the client’s personal experience with biofeedback suggests that healing is multidimensional. We suggest that practitioners use a holistic approach, which can provide hope and relief to clients who suffer from vulvodynia or other disorders that are often misunderstood and underreported.
Useful blogs
References
Kabat-Zinn, J. (2006). Coming to our senses: Healing ourselves and the world through mindfulness. Hachette Books
Peper, E., Cosby, J. & Almendras, M. (2022). Healing chronic back pain. NeuroRegulation, 9(3), 164–172. https://doi.org/10.15540/nr.9.3.164
Peper, E., Gibney, K.H, & Holt, C.F. (2002. Make health happen: Training yourself to create wellness. Kendall/Hunt.
Peper, E. Martinex, Aranda, P. & Moss, D. (2015). Vulvodynia treated successfully with breathing biofeedback and integrated stress reduction: A case report. Biofeedback, 43(2), 103–109. https://doi.org/10.5298/1081-5937-43.2.04
Hope for menstrual cramps (dysmenorrhea) with breathing
Posted: April 22, 2023 Filed under: behavior, biofeedback, Breathing/respiration, healing, health, meditation, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: dysmenorrhea, Imagery, menstrual cramps, stroking, visualization 1 CommentAdapted from: Peper, E., Chen, S., Heinz, N., & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04

“I have always had extremely painful periods. They would get so painful that I would have to call in sick and take some time off from school. I have been to many doctors and medical professionals, and they told me there is nothing I could do. I am currently on birth control, and I still get some relief from the menstrual pain, but it would mess up my moods. I tried to do the diaphragmatic breathing so that I would be able to continue my life as a normal woman. And to my surprise it worked. I was simply blown away with how well it works. I have almost no menstrual pain, and I wouldn’t bloat so much after the diaphragmatic breathing.” -22 year old student
Each semester numerous students report that their cramps and dysmenorrhea symptoms decrease or disappear during the semester when they implement the relaxation and breathing practices that are taught in the semester long Holistic Health class. Given that so many young women suffer from dysmenorrhea, many young women could benefit by using this integrated approach as the first self-care intervention before relying on pain reducing medications or hormones to reduce pain or inhibit menstruation. Another 28-year-old student reported:
“Historically, my menstrual cramps have always required ibuprofen to avoid becoming distracting. After this class, I started using diaphragmatic breath after pain started for some relief. True benefit came when I started breathing at the first sign of discomfort. I have not had to use any pain medication since incorporating diaphragmatic breath work.”
This report describes students practicing self-regulation and effortless breathing to reduce stress symptoms, explores possible mechanisms of action, and suggests a protocol for reducing symptoms of menstrual cramps. Watch the short video how diaphragmatic breathing eliminated recurrent severe dysmenorrhea (pain and discomfort associated with menstruation).
Background: What is dysmenorrhea?
Dysmenorrhea is one of the most common conditions experienced by women during menstruation and affects more than half of all women who menstruate (Armour et al., 2019). Most commonly dysmenorrhea is defined by painful cramps in the lower abdomen often accompanied by pelvic pain that starts either a couple days before or at the start of menses. Symptoms also increase with stress (Wang et al., 2003) with pain symptoms usually decreasing in severity as women get older and, after pregnancy.
Economic cost of dysmenorrhea
Dysmenorrhea can significantly interfere with a women’s ability to be productive in their occupation and/or their education. It is “one of the leading causes of absenteeism from school or work, translating to a loss of 600 million hours per year, with an annual loss of $2 billion in the United States” (Itani et al, 2022). For students, dysmenorrhea has a substantial detrimental influence on academic achievement in high school and college (Thakur & Pathania, 2022). Despite the frequent occurrence and negative impact in women’s lives, many young women struggle without seeking or having access to medical advice or, without exploring non-pharmacological self-care approaches (Itani et al, 2022).
Treatment
The most common pharmacological treatments for dysmenorrhea are nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Aspirin, and Naproxen Sodium) along with hormonal contraceptives. NSAIDs act by preventing the action of cyclooxygenase which prevents the production of prostaglandins. Itani et al (2022) suggested that prostaglandin production mechanisms may be responsible for the disorder. Hormonal contraceptives also prevent the production of prostaglandins by suppressing ovulation and endometrial proliferation.
The pharmacological approach is predominantly based upon the model that increased discomfort appears to be due to an increase in intrauterine secretion of prostaglandins F2α and E2 that may be responsible for the pain that defines this condition (Itani et al, 2022). Pharmaceuticals which influence the presence of prostaglandins do not cure the cause but mainly treat the symptoms.
Treatment with medications has drawbacks. For example, NSAIDs are associated with adverse gastrointestinal and neurological effects and also are not effective in preventing pain in everyone (Vonkeman & van de Laar, 2010). Hormonal contraceptives also have the possibility of adverse side effects (ASPH, 2023). Acetaminophen is another commonly used treatment; however, it is less effective than other NSAID treatments.
Self-regulation strategies to reduce stress and influence dysmenorrhea
Common non-pharmacological treatments include topical heat application and exercise. Both non-medication approaches can be effective in reducing the severity of pain. According to Itani et al. (2022), the success of integrative holistic health treatments can be attributed to “several mechanisms, including increasing pelvic blood supply, inhibiting uterine contractions, stimulating the release of endorphins and serotonin, and altering the ability to receive and perceive pain signals.”
Although less commonly used, self-regulation strategies can significantly reduce stress levels associated menstrual discomfort as well as reduce symptoms. More importantly, they do not have adverse side effects, but the effectiveness of the intervention varies depending on the individual.
- Autogenic Training (AT), is a hundred year old treatment approach developed by the German psychiatrist Johannes Heinrich Schultz that involves three 15 minute daily practice of sessions, resulted in a 40 to 70 percent decrease of symptoms in patient suffering from primary and secondary dysmenorrhea (Luthe & Schultz, 1969). In a well- controlled PhD dissertation, Heczey (1978) compared autogenic training taught individually, autogenic training taught in a group, autogenic training plus vaginal temperature training and a no treatment control in a randomized controlled study. All treatment groups except the control group reported a decrease in symptoms and the most success was with the combined autogenic training and vaginal temperature training in which the subjects’ vaginal temperature increased by .27 F degrees.
- Progressive muscle relaxation developed by Edmund Jacobson in the 1920s and imagery are effective treatments for dysmenorrhea (Aldinda et al., 2022; Chesney & Tasto, 1975; Çelik, 2021; Jacobson, 1938; Proctor et al., 2007).
- Rhythmic abdominal massage as compared to non-treatment reduces dysmenorrhea symptoms (Suryantini, 2022; Vagedes et al., 2019):
- Biofeedback strategies such as frontalis electromyography feedback (EMG) and peripheral temperature training (Hart, Mathisen, & Prater, 1981); trapezius EMG training (Balick et al, 1982); lower abdominal EMG feedback training and relaxation (Bennink, Hulst, & Benthem, 1982); and integrated temperature feedback and autogenic training (Dietvorts & Osborne, 1978) all successfully reduced the symptoms of dysmenorrhea.
- Breathing relaxation for 5 to 30 minutes resulted in a decrease in pain or the pain totally disappeared in adolescents (Hidayatunnafiah et al., 2022). While slow deep breathing in combination with abdominal massage is more effective than applying hot compresses (Ariani et al., 2020). Slow pranayama (Nadi Shodhan) breathing the quality of life and pain scores improved as compared to fast pranayama (Kapalbhati) breathing and improved quality of life and reduces absenteeism and stress levels (Ganesh et al. 2015). When students are taught slow diaphragmatic breathing, many report a reduction in symptoms compared to the controls (Bier et al., 2005).
Observations from Integrated stress management program
This study reports on changes in dysmenorrhea symptoms by students enrolled in a University Holistic Health class that included homework assignment for practicing stress awareness, dynamic relaxation, and breathing with imagery.
Respondents: 32 college women, average age 24.0 years (S.D. 4.5 years)
Procedure: Students were enrolled in a three-unit class in which they were assigned daily home practices which changed each week as described in the book, Make Health Happen (Peper, Gibney & Holt, 2002). The first five weeks consisted of the following sequence: Week 1 focused on monitoring one’s reactions to stressor; week 2 consisted of daily practice for 30 minutes of a modified progressive relaxation and becoming aware of bracing and reducing the bracing during the day; Week 3 consisted of practicing slow diaphragmatic breathing for 30 minutes a day and during the day becoming aware of either breath holding or shallow chest breath and then use that awareness as cue to shift to lower slower diaphragmatic breathing; week 4 focused on evoking a memory of wholeness and relaxing; and week 5 focused on learning peripheral hand warming.
During the class, students observed lectures about stress and holistic health and met in small groups to discuss their self-regulation experiences. During the class discussion, some women discussed postures and practices that were beneficial when experiencing menstrual discomfort, such as breathing slowly while lying on their back, focusing on slow abdominal awareness in which their abdomen expanded during inhalation and contracted during exhalation. While exhaling they focused on imagining a flow of air initially going through their arms and then through their abdomen, down their legs and out their feet. This kinesthetic feeling was enhanced by first massaging down the arm while exhaling and then massaging down their abdomen and down their thighs when exhaling. In most cases, the women also experienced that their hands and feet warmed. In addition, they were asked to shift to slower diaphragmatic breathing whenever they observed themselves gasping, shallow breathing or holding their breath. After five weeks, the students filled out a short assessment questionnaire in which they rated the change in dysmenorrhea symptoms since the beginning of the class.
Results.
About two-thirds of all respondents reported a decrease in overall discomfort symptoms. In addition to any ‘treatment as usual’ (TAU) strategies already being used (e.g. medications or other treatments such as NSAIDs or birth control pills), 91% (20 out 22 women) who reported experiencing dysmenorrhea reported a decrease in symptoms when they practiced the self-regulation and diaphragmatic breathing techniques as shown in Figure 1.

Figure 1. Self-report in dysmenorrhea symptoms after 5 weeks.
Discussion
Many students reported that their symptoms were significantly reduced and they could be more productive. Generally, the more they practiced the relaxation and breathing self-regulation skills, the more they experienced a decrease in symptoms. The limitation of this report is that it is an observational study; however, the findings are similar to those reported by earlier self-care and biofeedback approaches. This suggests that women should be taught the following simple self-regulation strategies as the first intervention to prevent and when they experience dysmenorrhea symptoms.
Why would breathing reduce dysmenorrhea?
Many women respond by ‘curling up’ a natural protective defense response when they experience symptoms. This protective posture increases abdominal and pelvic muscle tension, inhibits lymph and blood flow circulation, increases shallow breathing rate, and decreases heart rate variability. Intentionally relaxing the abdomen with slow lower breathing when lying down with the legs extended is often the first step in reducing discomfort.
By focusing on diaphragmatic breathing with relaxing imagery, it is possible to restore abdominal expansion during inhalation and slight constriction during exhalation. This dynamic breathing while lying supine would enhance abdominal blood and lymph circulation as well as muscle relaxation (Peper et al., 2016). While practicing, participants were asked to wear looser clothing that did not constrict the waist to allow their abdomen to expand during inhalation; since, waist constriction by clothing (designer jean syndrome) interferes with abdominal expansion. Allowing the abdomen to fully extend also increased acceptance of self, that it was okay to let the abdomen expand instead of holding it in protectively. The symptoms were reduced most likley by a combination of the following factors.
- Abdominal movement is facilitated during the breathing cycle. This means reducing the factors that prevent the abdomen expanding during inhalation or constricting during exhalation (Peper et al., 2016).
- Eliminate‘Designer jean syndrome’ (the modern girdle). Increase the expansion of your abdomen by loosening the waist belt, tight pants or slimming underwear (MacHose & Peper, 1991).
- Accept yourself as you are. Allow your stomach to expand without pulling it in.
- Free up learned disuse: Allow the abdomen to expand and constrict instead of inhibiting movement to avoid pain that occurred following a prior abdominal injury/surgery (e.g., hernia surgery, appendectomy, or cesarean operation), abdominal pain (e.g., irritable bowel syndrome, recurrent abdominal pain, ulcers, or acid reflux), pelvic floor pain (e.g., pelvic floor pain, pelvic girdle pain, vulvodynia, or sexual abuse).
- The ‘defense response’ is reduced. Many students described that they often would curl up in a protective defense posture when experiencing menstrual cramps. This protective defense posture would maintain pelvic floor muscle contractions and inhibit blood and lymph flow in the abdomen, increase shallow rapid thoracic breathing and decrease pCO2 which would increase vasoconstriction and muscle constriction (Peper et al., 2015; Peper et al., 2016). By having the participant lie relaxed in a supine position with their legs extended while practicing slow abdominal breathing, the pelvic floor and abdominal wall muscles can relax and thereby increase abdominal blood and lymph circulation and parasympathetic activity. The posture of lying down implies feeling safe which is a state that facilitates healing.
- The pain/fear cycle is interrupted. The dysmenorrhea symptoms may trigger more symptoms because the person anticipates and reacts to the discomfort. The breathing and especially the kinesthetic imagery where the attention goes from the abdomen and area of discomfort to down the legs and out the feet acts as a distraction technique (not focusing on the discomfort).
- Support sympathetic-parasympathetic balance. The slow breathing and kinesthetic imagery usually increases heart rate variability and hand and feet temperature and supports sympathetic parasympathetic balance.
- Interrupt the classical conditioned response of the defense reaction. For some young girls, the first menstruation occurred unexpectedly. All of a sudden, they bled from down below without any understanding of what is going on which could be traumatic. For some this could be a defense reaction and a single trial condition response (somatic cues of the beginning of menstruation triggers the defense reaction). Thus, when the girl later experiences the initial sensations of menstruation, the automatic conditioned response causes her to tense and curl up which would amplify the discomfort. Informal interviews with women suggests that those who experienced their first menstruation experience as shameful, unexpected, or traumatic (“I thought I was dying”) thereafter framed their menstruation negatively. They also tended to report significantly more symptoms than those women who reported experiencing their first menstruation positively as a conformation that they have now entered womanhood.
How to integrate self-care to reduce dysmenorrhea
Be sure to consult your healthcare provider to rule out treatable underlying conditions before implementing learning effortless diaphragmatic breathing.
- Allow the abdomen to expand during inhalation and become smaller during exhalation. This often means, loosen belt and waist constriction, acceptance of allowing the stomach to be larger and reversing learned disuse and protective response caused by stress.
- Master diaphragmatic breathing (see: Peper & Tibbetts, 1994 and the blogs listed at the end of the article).
- Practice slow effortless diaphragmatic breathing lying down with warm water bottle on stomach in a place that feels safe.
- Include kinesthetic imagery as you breathe at about 6 breaths per minute (e.g. slowly inhale for 4 or 5 seconds and then exhale for 5 or 6 seconds, exhaling slightly longer than inhaling). Imaging that when you exhale you can sense healing energy flow through your abdomen, down the legs and out the feet.
- If possible, integrate actual touch with the exhalation can provide added benefit. Have a partner first stroke or massage down the arms from the shoulder to your fingertips as you exhale and, then on during next exhalation stroke gently from your abdomen down your legs and feet. Stroke in rhythm the exhalation.
- Exhale slowly and shift to slow and soft diaphragmatic breathing each time you become aware of neck and shoulder tension, breath holding, shallow breathing, or anticipating stressful situations. At the same time imagine /sense when exhaling a streaming going through the abdomen and out the feet when exhaling. Do this many times during the day.
- Practice and apply general stress reduction skills into daily life since stress can increase symptoms. Anticipate when stressful event could occur and implement stress reducing strategies.
- Be respectful of the biological changes that are part of the menstrual cycle. In some cases adjust your pace and slow down a bit during the week of the menstrual cycle; since, the body needs time to rest and regenerate. Be sure to get adequate amount of rest, hydration, and nutrition to optimize health.
- Use self-healing imagery and language to transform negative association with menstruation to positive associations (e.g., “curse” to confirmation “I am healthy”).
Conclusion
There are many ways to alleviate dysmenorrhea. Women can find ways to anticipate and empower themselves by practicing stress reduction, wearing more comfortable clothing, using heat compression, practicing daily diaphragmatic breathing techniques, visualizing relaxed muscles, and positive perception towards menstrual cycles to reduce the symptoms of dysmenorrhea. These self-regulation methods should be taught as a first level intervention to all young women starting in middle and junior high school so that they are better prepared for the changes that occur as they age.
“I have been practicing the breathing techniques for two weeks prior and I also noticed my muscles, in general, are more relaxed. Of course, I also avoided the skinny jeans that I like to wear and it definitely helped.
I have experienced a 90% improvement from my normal discomfort. I was still tired – and needed more rest and sleep but haven’t experienced any “terrible” physical discomfort. Still occasionally had some sharp pains or bloating but minor discomfort, unlike some days when I am bedridden and unable to move for half a day. – and this was a very positive experience for me “ — Singing Chen (Chen, 2023)
Useful blogs to learn diaphragmatic breathing
References
Aldinda, T. W., Sumarni, S., Mulyantoro, D. K., & Azam, M. (2022). Progressive muscle relaxation application (PURE App) for dysmenorrhea. Medisains Jurnal IlmiahLlmiah LLmu-LLmu Keshatan, 20(2), 52-57. https://doi.org/10.30595/medisains.v20i2.14351
Ariani, D., Hartiningsih, S.S., Sabarudin, U. Dane, S. (2020). The effectiveness of combination effleurage massage and slow deep breathing technique to decrease menstrual pain in university students. Journal of Research in Medical and Dental Science, 8(3), 79-84. https://www.jrmds.in/articles/the-effectiveness-of-combination-effleurage-massage-and-slow-deep-breathing-technique-to-decrease-menstrual-pain-in-university-stu-53607.html
Armour, M., Parry, K., Manohar, N., Holmes, K., Ferfolja, T., Curry, C., MacMillan, F., & Smith, C. A. (2019). The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. Journal of women’s health, 28(8), 1161-1171.https://doi.org/10.1089/jwh.2018.7615
ASPH. (2023). Estrogen and Progestin (Oral Contraceptives). MedlinePlus. Assessed March 3, 2023. https://medlineplus.gov/druginfo/meds/a601050.html
Balick, L., Elfner, L., May. J., Moore, J.D. (1982). Biofeedback treatment of dysmenorrhea. Biofeedback Self Regul, 7(4), 499-520. https://doi.org/10.1007/BF00998890
Bennink, C.D., Hulst, L.L. & Benthem, J.A. (1982). The effects of EMG biofeedback and relaxation training on primary dysmenorrhea. J Behav Med, 5(3), 329-341.https://doi.org/10.1007/BF00846160
Bier, M., Kazarian, D. & Peper, E. (2005). Reducing PMS through biofeedback and breathing. Poster presentation at the 36th Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Abstract published in: Applied Psychophysiology and Biofeedback. 30 (4), 411-412.
Çelik, A.S. & Apay, S.E. (2021). Effect of progressive relaxation exercises on primary dysmenorrhea in Turkish students: A randomized prospective controlled trial. Complement Ther Clin Pract, Feb 42,101280. https://doi.org/10.1016/j.ctcp.2020.101280
Chen, S. (2023). Diaphragmatic breathing reduces dysmenorrhea symptoms-a testimonial. YouTube. Accessed March 3, 2023. https://youtu.be/E45iGymVe3U
De Sanctis, V., Soliman, A., Bernasconi, S., Bianchin, L., Bona, G., Bozzola, M., Buzi, F., De Sanctis, C., Tonini, G., Rigon, F., & Perissinotto, E. (2015). Primary Dysmenorrhea in Adolescents: Prevalence, Impact and Recent Knowledge. Pediatr Endocrinol Rev. 13(2), 512-20. PMID: 26841639. https://pubmed.ncbi.nlm.nih.gov/26841639/
De Sanctis, V., Soliman, A. T., Daar, S., Di Maio, S., Elalaily, R., Fiscina, B., & Kattamis, C. (2020). Prevalence, attitude and practice of self-medication among adolescents and the paradigm of dysmenorrhea self-care management in different countries. Acta Bio Medica: Atenei Parmensis, 91(1), 182. https://doi.org/10.23750/abm.v91i1.9242
Dietvorst, T.F. & Osborne, D. (1978). Biofeedback-Assisted Relaxation Training
for Primary Dysmenorrhea: A Case Study. Biofeedback and Self-Regulation, 3(3), 301-305. https://doi.org/10.1007/BF00999298
Chesney, M. A., & Tasto, D. L. (1975).The effectiveness of behavior modification with spasmodic and congestive dysmenorrhea. Behaviour Research and Therapy, 13, 245-253. https://doi.org/10.1016/0005-7967(75)90029-7
Ganesh, B.R., Donde, M.P., & Hegde, A.R. (2015). Comparative study on effect of slow and fast phased pranayama on quality of life and pain in physiotherapy girls with primary dysmenorrhea: Randomize clinical trial. International Journal of Physiotherapy and Research, 3(2), 960-965. https://doi.org/10.16965/ijpr.2015.115
Hart, A.D., Mathisen, K.S. & Prater, J.S. A comparison of skin temperature and EMG training for primary dysmenorrhea. Biofeedback and Self-Regulation 6, 367–373 (1981). https://doi.org/10.1007/BF01000661
Heczey, M. D. (1978). Effects of biofeedback and autogenic training on menstrual experiences: relationship among anxiety, locus of control and dysmenorrhea. City University of New York ProQuest Dissertations Publishing, 7805763. https://www.proquest.com/openview/088e0d68511b5b59de1fa92dec832cc8/1?pq-origsite=gscholar&cbl=18750&diss=y
Hidayatunnafiah, F., Mualifah, L., Moebari, M., & Iswantiningsih, E. (2022). The Effect of Relaxation Techniques in Reducing Dysmenorrhea in Adolescents. The International Virtual Conference on Nursing. in The International Virtual Conference on Nursing, KnE Life Sciences, 473–480. https://doi.org/10.18502/kls.v7i2.10344
Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H.M.J. (2022). Primary Dysmenorrhea: Pathophysiology, Diagnosis, and Treatment Updates. Korean J Fam Med, 43(2), 101-108. https://doi.org/10.4082/kjfm.21.0103
Jacobson, E. (1938). Progressive Relaxation: A Physiological and Clinical Investigation of Muscular States and Their Significance in Psychology and Medical Practice. Chicago: University of Chicago Press
Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiol Rev, 36, 104-13. https://doi.org/10.1093/epirev/mxt009
Karout, S., Soubra, L., Rahme, D. et al. Prevalence, risk factors, and management practices of primary dysmenorrhea among young females. BMC Women’s Health 21, 392 (2021). https://doi.org/10.1186/s12905-021-01532-w
Iacovides, S., Avidon,I, & Baker, F.C. (2015).What we know about primary dysmenorrhea today: a critical review, Human Reproduction Update, 21(6), 762–778. https://doi.org/10.1093/humupd/dmv039
Luthe, W. & Schultz, J.H. (1969). Autogenic Therapy, Volume II Medical Applications. New York: Grune & Stratton, pp144-148.
MacHose, M. & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. ISBN: 978-0787293314 https://he.kendallhunt.com/make-health-happen
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. Also in: Electromyography: Applications in Physical Therapy. Montreal: Thought Technology Ltd. https://biofeedbackhealth.files.wordpress.com/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Proctor, M. & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ. 13, 332(7550), 1134-8. https://doi.org/10.1136/bmj.332.7550
Proctor, M.L, Murphy, P.A., Pattison, H.M., Suckling, J., & Farquhar, C.M. (2007). Behavioural interventions for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev, (3):CD002248. https://doi.org/10.1002/14651858.CD002248.pub3
Suryantini, N. P. (2022). Effleurage Massage: Alternative Non-Pharmacological Therapy in Decreasing Dysmenorrhea Pain. Women, Midwives and Midwifery, 2(3), 41-50. https://wmmjournal.org/index.php/wmm/article/view/71/45
Thakur, P. & Pathania, A.R. (2022). Relief of dysmenorrhea – A review of different types of pharmacological and non-pharmacological treatments. MaterialsToday: Proceedings.18, Part 5, 1157-1162. https://doi.org/10.1016/j.matpr.2021.08.207
Vagedes, J., Fazeli, A., Boening, A., Helmert, E., Berger, B. & Martin, D. (2019). Efficacy of rhythmical massage in comparison to heart rate variability biofeedback in patients with dysmenorrhea—A randomized, controlled trial. Complementary Therapies in Medicine, 42, 438-444. https://doi.org/10.1016/j.ctim.2018.11.009
Vonkeman, H.E. & van de Laar, M,A. (2010). Nonsteroidal anti-inflammatory drugs: adverse effects and their prevention, Semin Arthritis Rheum, 39(4), 294-312. https://doi.org/10.1016/j.semarthrit.2008.08.001
Wang, L., Wand, X., Wang, W., Chen, C. Ronnennberg, A.G., Guang, W. Huang, A. Fang, Z. Zang, T., Wang, L. & Xu, X. (2003).Stress and dysmenorrhoea: a population based prospective study. Occupation and Environmental Medicine, 61(12). http://dx.doi.org/10.1136/oem.2003.012302
Compassion supports healing: Case report how a “bad eye” became an “amazing eye”*
Posted: April 11, 2023 Filed under: behavior, cognitive behavior therapy, healing, health, mindfulness, Pain/discomfort, self-healing, stress management, Uncategorized, vision | Tags: compassion, self-image 2 CommentsErik Peper, PhD and Dana Yirmiyahu

“I completely changed my perception of having a bad eye, to having an amazing eye. After two months, my eye is totally normal and healthy”
When experiencing chronic discomfort or reduced function, we commonly describe that part of our body that causes problems as broken or bad. Sometimes we even wish that it did not exist. In other cases, especially if there is pain or disfigurement, the person may attempt to dissociate from that body part. The language the person uses creates a graphic imagery that may impact the healing process; since, language can also be seen as a self-hypnotic suggestion.
The negative labeling, plus being disgusted or frustrated with that part of the body that is the cause of discomfort, often increases stress, tension and sympathetic activity. This reduces our self-healing potential. In many cases, the language is both the description and the prognosis-a self-fulfilling prophecy. If the description is negative and judgmental, it may interfere with the healing/treatment process. The negative language may activate the nocebo process that inhibits regeneration. On the other hand, positive affirming language may implicitly activate the placebo process that enhances healing.
By reframing the experience as positive and appreciating what the problem area of the body had done for you in the past as well as incorporating a healing compassionate process, healing is supported. Our limiting beliefs limit our possibilities. See the TED talk, A broken body isn’t a broken person, by Janine Shepherd (2014) who, after a horrendous accident and being paralyzed, became an acrobatic pilot instructor. Another example of a remarkable recovery is that of Madhu Anziani. After falling from a second floor window, he was a quadriplegic and used Reiki, toning, self-compassion and hope to improve his health. He reframed the problem as an opportunity for growth. He can now walk, talk and play the most remarkable music (Anziani and Peper, 2021).
When a person can focus on what they can do instead of focusing on what they cannot do or on their suffering, pain may be reduced. For example, Jill Cosby describes undergoing two surgeries to replace her shattered L3 with a metal “cage” and fused this cage to the L4 and L2 vertebrae with bars. She used imagery to eliminate the pains in her back and stopped her pain medications (Peper et al., 2022). The healing process is similar to how children develop, growth, and learn–a process that is promoted through playfulness and support with an openness to possibilities.
Healing only goes forwards in time
After an injury, most people want to be the same as they were before the injury, and they keep comparing themselves to how they were. The person can never be what they were in the past, butthey can be different and even better.. Time flows only in a forward direction, and the person already has been changed by the experience. Instead, the person explores ways to accept where they are, appreciate how much the problem area has done for them in the past, and continue to work to improve. This is a dynamic process in which the person appreciates the very small positive changes that are occurring without setting limits on how much change can occur.
A useful tool while working with clients is to explore ways by which they can genuinely transform their negative beliefs and self-talk about the problem to appreciation and growth. This process is illustrated in the following report about the rapid healing of a 15-year problem with an eye that had become smaller following severe corneal abrasion.
Case report
On January 18th, 2023, I attended a workshop/ lecture by Professor Erik Peper.
During the break, I spoke to him and expressed my concern regarding my right eye. 15 years ago, the cornea of my eye was accidently scratched by my 3-year-old daughter. The eye suffered a trauma and was treated at the hospital. In addition, I had a patch over my eye for 3 weeks and suffered extrusion pain during the first 2 weeks. A scar remained on my eye, and doctors were not able to say if it would be permanent or whether the eye would heal itself eventually. An invasive operation was also suggested, which I refused. The trauma affected my eyesight for a few months, but after a year, the scar was gone and physically no permanent damage has remained.
Although it was certainly determined that my eye had healed completely, it didn’t feel that way at all. I always considered it ‘my bad eye’ and suffered irritation and pain every time I experienced tiredness, anxiety, or any other emotional discomfort. My eye was the first and only organ to reflect pain/itchiness/irritation. Over time, my eye ‘shrank’ as well. It became visibly smaller and it felt tense at all times.
For 15 years, that was my reality! I coped with it and haven’t thought of it much, until January 18, when I attended the workshop.
Professor Peper asked me to the front of the stage when we returned from break and conducted an exercise with me, where I used my imagination and words to comfort my eye and embrace it rather than call it ‘the defective/bad eye’. He pointed out that if you only describe your children as bad or evil, how can you expect them to grow? Then, he explored with me a few exercises such as evoking self-healing imagery. The self-healing imagery did not totally resonate; however, I felt I just needed to hug my eye. I thanked my eye for its being and stroked it gently in my mind. On stage and during the rest of the lecture I felt a sense of comfort. I felt if the muscles around my eye had finally loosened–a feeling I haven’t experienced for years. I continued to follow the instructions I got at the workshop for a couple of days, but unfortunately, I did not persist, and the negative sensations returned.
On a follow-up zoom meeting 10 days after the lecture with Prof. Peper, I received additional tools to practice ‘eye physiotherapy’ as well as mindfulness regarding the eye. This practice consisted of closing my eyes and covering the non-problem eye and then as I exhaled gently and softly opening my eyes, opening them more and more while looking all around. I completely changed my perception of having a bad eye, to having ‘an amazing eye’. At first talking to it didn’t come naturally to me but as I persisted it became easier and easier. I did it in the car, before going to sleep and when waking up in the morning. In addition, I practiced the exercises I got over zoom, where I covered my left eye (the undamaged one) and had my right eye look up and down to both sides.
It has been about three months since this zoom meeting and I am awed by the results. My eye has opened more, and no longer feels shrunk and small, I rarely feel negative sensations in it and when I do, I immediately know how to handle it.
I can say that attending this workshop has definitely been a life-changing event for my amazing right eye and for me.
Why did the healing occur?
The “bad eye” symptoms were most likely caused by “learned disuse”; namely, the chronic eye tension was the result of the protective response to reduce the discomfort after the injury to the cornea (Uswatte & Taub, 2005). After the injury and medical treatment, she would have unknowingly tensed her muscles around the eye to protect it. This process occurs automatically without conscious awareness. This protective response became her “new normal” and once her eye had healed, the bracing continued. The bracing pattern was amplified by the ongoing self-labeling of having a “bad eye.” By accepting the eye as it was, giving it compassionate caring and support, and following up with simple eye movement exercises to allow the eye to rediscover and experience the complete range of motion, the symptoms disappeared.
What can we take home from this case example?
Listen to the language a client uses to describe their problem. Does the language implicitly limit recovery, growth and hope (e.g., I will always have the problem)? Does the language inhibit caring and compassion for the problem area (e.g., I’m frustrated, angry, disgusted)? If that is the case, explore ways to reframe the language and emotional tone. A useful strategy is to incorporate self-healing imagery: the person first inspects the problem area, next imagines how it would look when it is healthy, and finally creates self-healing imagery that transforms what was observed to become well and whole. Then, each moment the client’s attention is drawn to the problem, he or she evokes the self-healing imagery (Peper, Gibney, & Holt, 2002). In many cases, combining this imagery with slower breathing to reduce stress promotes healing.
References
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. the peper perspective-ideas on illness, health and well-being from Erik Peper. Accessed March 22, 2023. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Mullins, A. (2009). The opportunity of adversity. TEDMED. Accessed March 22, 2023. https://www.ted.com/talks/aimee_mullins_the_opportunity_of_adversity?language=en
Peper, E. Cosby, J. & Amendras, M. (2022). Healing chronic back pain. NeuroRegulation, 9(3), 165-172. https://doi.org/10.15540/nr.9.3.164
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. pp. 193-236. https://he.kendallhunt.com/make-health-happen
Shepherd, J. (2014). A broken body isn’t a broken person. TEDxKC. Accessed March 20, 2023 https://www.ted.com/talks/janine_shepherd_a_broken_body_isn_t_a_broken_person?language=en
Uswatte, G. & Taub, E. (2005). Implications of the Learned Nonuse Formulation for Measuring Rehabilitation Outcomes: Lessons From Constraint-Induced Movement Therapy. Rehabilitation Psychology, 50(1), 34-42. https://doi.org/10.1037/0090-5550.50.1.34
*I thank Cathy Holt, MPH, for her supportive feedback.
Breathing: Informative YouTube videos and blogs
Posted: March 20, 2023 Filed under: behavior, Breathing/respiration, health, mindfulness, Pain/discomfort, relaxation, self-healing | Tags: anxiety, box breathing, carbon dioxide, exhaling, hickups 3 Comments
Breathing is a voluntary and involuntary process and affects our body, emotions, mind and performance. The focus of breathing is to bring oxygen into the body and eliminate carbon dioxide. This is the basic physiological process that underlies the concepts described in the videos; however, it does not included the concept as breathing as a pump to optimize abdominal venous and lymph circulation. The pumping action may reduce abdominal discomfort such as irritable bowel disease, acid reflux and pelvic floor discomfort. Effortless whole body breathing also supports pelvic floor muscle tone balance and spinal column dynamics. Effortless diaphragmatic breathing can only occur if the abdomen is able to expand and constrict in 360 degrees and not constricted by tight clothing around the waist (designer’s jean syndrome), self-image (holding the abdomen in to look slimmer), or learned disuse of abdominal movement (breathing shallowly and in the chest to avoid movement at the incisionsafter abdominal surgery).
The outstanding videos discuss the psychophysiology, mechanics, chemistry of respiration as well as useful practices practices to enhance health..
- How to Breathe Correctly for Optimal Health, Mood, Learning & Performance | Huberman Lab Podcast (Skip the advertisements embedded in this video)
- Dr. Jack Feldman: Breathing for Mental & Physical Health & Performance | Huberman Lab Podcast #54 (Skip the advertisements embedded in this video)
The videos provide additional approaches to improve breathing and health
- 5 Ways to Improve your Breathing with James Nestor
- Patrick McKeown-Why we breathe: How to improve your sleep, concentration, focus & performance
The blogs that explores how diaphragmatic breathing may reduce symptoms of irritable bowel syndrome, acid reflux, and pelvic floor pain.
- Healing irritable bowel syndrome with diaphragmatic breathing
- Breathing to reduce acid reflux and dysmenorrhea
- Enjoy sex: Breath away the pain
- Resolving pelvic floor pain-a casae report
Below are the descriptions of the youtube videos.
How to Breathe Correctly for Optimal Health, Mood, Learning & Performance | Huberman Lab Podcast
In this episode, I explain the biology of breathing (respiration), how it delivers oxygen and carbon dioxide to the cells and tissues of the body and how is best to breathe—nose versus mouth, fast versus slow, deliberately versus reflexively, etc., depending on your health and performance needs. I discuss the positive benefits of breathing properly for mood, to reduce psychological and physiological stress, to halt sleep apnea, and improve facial aesthetics and immune system function. I also compare what is known about the effects and effectiveness of different breathing techniques, including physiological sighs, box breathing and cyclic hyperventilation, “Wim Hof Method,” Prānāyāma yogic breathing and more. I also describe how to breath to optimize learning, memory and reaction time and I explain breathing at high altitudes, why “overbreathing” is bad, and how to breathe specifically to relieve cramps and hiccups. Breathwork practices are zero-cost and require minimal time yet provide a unique and powerful avenue to improve overall quality of life that is grounded in clear physiology. Anyone interesting in improving their mental and physical health or performance in any endeavor ought to benefit from the information and tools in this episode.
Dr. Jack Feldman: Breathing for Mental & Physical Health & Performance | Huberman Lab Podcast #54
This episode my guest is Dr. Jack Feldman, Distinguished Professor of Neurobiology at University of California, Los Angeles and a pioneering world expert in the science of respiration (breathing). We discuss how and why humans breathe the way we do, the function of the diaphragm and how it serves to increase oxygenation of the brain and body. We discuss how breathing influences mental state, fear, memory, reaction time, and more. And we discuss specific breathing protocols such as box-breathing, cyclic hyperventilation (similar to Wim Hof breathing), nasal versus mouth breathing, unilateral breathing, and how these each effect the brain and body. We discuss physiological sighs, peptides expressed by specific neurons controlling breathing, and magnesium compounds that can improve cognitive ability and how they work. This conversation serves as a sort of “Master Class” on the science of breathing and breathing related tools for health and performance.
5 Ways To Improve Your Breathing with James Nestor
James Nestor believes we’re all breathing wrong. Here he breaks down 5 ways to transform your breathing, from increasing your lung capacity to stopping breathing through your mouth. There is nothing more essential to our health and wellbeing than breathing: take air in, let it out, repeat 25,000 times a day. Yet, as a species, humans have lost the ability to breathe correctly, with grave consequences. In Breath, journalist James Nestor travels the world to discover the hidden science behind ancient breathing practices to figure out what went wrong and how to fix it. Modern research is showing us that making even slight adjustments to the way we inhale and exhale can: – jump-start athletic performance – rejuvenate internal organs – halt snoring, allergies, asthma and autoimmune disease, and even straighten scoliotic spines None of this should be possible, and yet it is. Drawing on thousands of years of ancient wisdom and cutting-edge studies in pulmonology, psychology, biochemistry and human physiology, Breath turns the conventional wisdom of what we thought we knew about our most basic biological function on its head. You will never breathe the same again.
Patrick McKeown – Why We Breathe: How to Improve Your Sleep, Concentration, Focus & Performance
Watch Oxygen Advantage founder and world-renowned breathing expert Patrick McKeown speak to an influential group of health professionals at the recent Health Optimisation Summit in London. Patrick was presenting his very well-received topic: ‘Why We Breathe: How to Improve Your Sleep, Concentration, Focus & Performance’. The aim of the event was to “unite the health, wellness and science disciplines”, and in doing so, it brought together thousands of industry professionals and members of the public. Patrick would like to take this opportunity to thank the organisers of The Health Optimisation Summit for an excellent event and for giving him the opportunity to speak among such luminaries of the health and wellbeing world and on a subject about which he is very passionate.
Breathing is more than gas exchange
Effortless diaphragmatic breathing is optimized when the abdomen is able to expand and constrict in 360 degrees like and not constricted by tight clothing (designer’s jean syndrome induced by the constriction of the waist), self-image (holding the abdomen in to look slimmer), or learned disuse of abdominal movement (breathing shallowly and in the chest to avoid movement at the incisions site after abdominal surgery).
Thoughts Have the Power to Create or Eliminate Body Tension
Posted: January 31, 2023 Filed under: Breathing/respiration, CBT, cognitive behavior therapy, computer, emotions, ergonomics, healing, health, Neck and shoulder discomfort, Pain/discomfort, posture, stress management, Uncategorized | Tags: Alexander Technique, mind-body connection 3 CommentsBy Tami Bulmash republished from: Medium-Body Wisdom
Photo by Jonathan Borba on Unsplash
The mind and body have long been regarded and treated as separate entities, yet this distinction does little to promote holistic health. Understanding the direct relationship between thoughts and body tension can illustrate how the mind and body either work dysfunctionally through separation, or optimally as a unit.
Mental and physical aren’t separate entities
Stress and pain existed long before the coronavirus, though it was highlighted during this isolating era. In the height of the pandemic nearly eight in 10 American adults cited COVID-19 as a significant stressor. Though it may no longer be front page news, the aftermath of COVID still lingers. Its toll on mental health continues to impact children and adults alike. The shift to remote work was appealing at first, but later created a more pervasive sedentary lifestyle. Now the concern has shifted to an emerging pandemic of back pain.
Yet, there is nothing novel about body tension brought forth by stressful thinking. In 2014, the American Institute of Stress reported 77 percent of people regularly experience physical symptoms caused by stress. Moreover, the findings of a 2018 Gallup poll suggest 55 percent of Americans report feeling stressed for a large part of their day. This is compounded by the American Academy of Orthopaedic Surgeons finding one in two Americans have a musculoskeletal condition. Discerning between mental and physical stress is becoming increasingly obscure.
While the mind and body have long been regarded and treated as separate entities, this distinction does little to promote holistic health. Understanding the direct relationship between thoughts and tension can illustrate how the mind and body either work dysfunctionally through separation, or optimally as a unit. What’s more, viewing the body as a whole being — in thought and activity — can promote better habits which eliminate tension.
The link between stress and pain
Dividing the self into parts is common practice in the Western world. Expressions such as “I’m mentally exhausted” vs. “I’m physically exhausted” provoke differing self-reflections. However, the psycho-physical relationship is evident in the tension stimulated by either thought. For example, sitting in front of a computer necessitates both thought and action. Viewing content on a screen lends itself to a reaction from behind the screen. This response can be minimal and inconsequential, or it can be subtle, yet critical.
Repeatedly engaging in certain thinking habits like, “I have to get this done and fast” are often reflected in forms of body tension such as stiff fingers at the keyboard, a clenched jaw after a meeting, or tense neck at the end of the day. These unconscious responses are common and have a pervasive effect.
The prevalence of technology has led to a plethora of occupational ailments, now referred to as technology diseases. These include carpal tunnel syndrome, mouse shoulder, and cervical pain syndrome and occur because of excessive work at the computer — especially keyboard and mouse usage. According to the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics, by Drs. Erik Peper, Richard Harvey and Nancy Faass, 45 million people suffer from tension headaches, carpal tunnel, and back injuries linked to computer use and more than 30 percent of North Americans who work at a computer develop a muscle strain injury every year.
Pushing through mental tasks is reflected in the physical
Dr. Peper, a biofeedback expert and Professor of Holistic Health at San Francisco State University, gives an illustration of the mind-body connection in relation to pain. His example requires the use of a computer mouse while trying to complete difficult mental tasks. He asks me to hold the mouse in my dominant hand and draw with it the last letter of an address. Then continue to go backward with each letter of the street name, making sure the letter height is only one-half of an inch. He tells me to perform the task as quickly as possible. As I’m drawing the address backwards trying to recall the letters and their order, Dr. Peper commands, “Do it quicker, quicker, quicker! Don’t make a mistake! Quicker, quicker, quicker!”
These commands reflect the endless to-do lists that pile up throughout the day and the stress associated with their efficacy and timely completion. While enacting this task, Dr. Peper asks me, “Are you tightening your shoulders? Are you tightening your trunk? Are you raising your shoulders possibly holding all this tension? If you are like most people who do this task, you did all of that and you were totally unaware. We are usually really unaware of our body posture.”
I have spent the past 20 years practicing the Alexander Technique, a method used to improve postural health. At its core the technique is about observation and utilizing psycho-physical awareness to stop repeating harmful habits. Dr. Peper’s words resonate because becoming aware of unconscious responses isn’t easy. Most people are completely unaware of the relationship between mind-body habits and how they contribute to stress-related pain.
Posture affects mood and energy levels
Posture is often thought of as a pose — most notably being associated with “sitting up straight”. Yet the health implications of good posture extend far beyond any held position. The agility and movement which are evident in good posture exemplify the mind-body connection.
It is well-known that feeling depressed has been linked to having less subjective energy. The American Psychiatric Association listed a variety of symptoms connected to depression including feeling sad or having a depressed mood, loss of interest in activities once enjoyed, and loss of energy or increased fatigue. While the treatment of depression hasn’t traditionally considered the role of posture in informing mood, researchers have started exploring this relationship.
A study by Dr. Peper and Dr. I-Mei Lin examined the subjective energy levels of university students and their corresponding expression of depression. Participants who walked in a slouched position reported lower energy levels and higher self-rated depression scores. In contrast, when those participants walked in a pattern of opposite arm and leg skipping, they experienced an increase in energy, allowing a positive mindset to ensue.
As mentioned in the study, the mind-body relationship is a two-way street: mind to body and body to mind. If thoughts are manifested in the way one holds their body, the inverse would also be true. Namely, changing the way one carries their body would also influence their thinking and subsequent mood. If stopping certain habits — such as walking in a slumped posture — could have a positive impact on mood and well-being, perhaps it’s worth exploring the mind-body relationship even further.
Supporting the mind-body connection
One of the best ways to improve the mind-body connection is through awareness. The more present you are in your activities, the more unified the relation becomes. Give yourself a couple of minutes to connect your thoughts with what you are doing at the moment.
Begin With Grounding
If you are sitting down, imagine coloring in the space of your whole body with an imaginary marker. Begin with your feet planted on the floor. Start to outline the footprints of your feet and then color in the bottom and top of each foot. Take your time. Fill in all the space. See if you discover new parts of your feet — like the spaces between your toes. Continue up through your ankles and toward your calves. Pay attention to the entire limb (front and back). Work your way upward through the knee and then the upper leg. See if you can find your sit bones along the way to the torso. Explore new joints — such as the hip joint.
Lengthen Your Body Through Thought
Continue up while circling the front and back of the torso. Extend the awareness of your thoughts through your shoulders. Allow for an exploration of the arms — noting the joints such as the elbows, wrists and fingers. Pay attention to their length and mobility. Come back up through the arms. Extend up through the shoulders again, this time noting the passage through the chest and neck. Observe the length and space within your entire being. Journey up to the head and travel around its circumference. Imagine filling your head space with air. Picture the wholeness of your head from top to bottom and side to side.
This two-minute mind-body meditation allows you to feel the full extent of the space your body takes up. It is a way to awaken the senses and include them in conscious thinking. This helps generate awareness in how to engage the mind-body relationship optimally. The next time you try it, use a visual aid like an anatomy diagram of the whole body. This can also introduce new parts and spaces of the body you may not have thought of before. However, don’t rely on the diagram each time, as it can pull away your attention from the mind-body meditation. Instead, use it as a reference or guide every once in a while.
Learn from other cultures
In Western cultures, it is common practice to divvy up musculoskeletal ailments into an array of categories such as tension headaches, tension neck syndrome, or mechanical back syndrome. For instance, in countries like the U.S., it is normal to seek a specialist for each area of concern — like a neurologist for a migraine, an orthopedist for neck strain, or chiropractors for back pain. In contrast, Eastern lifestyles have historically taken a more holistic approach to treating (and healing) their patients.
An article by Dr. Cecilia Chan, Professor of Social Sciences at the University of Hong Kong, explains how the Eastern philosophies of Buddhism, Taoism and traditional Chinese medicine adopt a holistic approach to the healing of an individual. Rather than diagnose and treat with medication, Chan and her colleagues explore health through the harmony and balance of the body-mind-spirit as a whole.
Because basic biology clearly delineates how the human head is attached to the body, it seems fitting that the entire being be regarded as a unit. By recognizing the relationship between thought stressors and their manifestation in the physical body, awareness is elevated. This, in turn, can prevent mindlessly engaging in harmful patterns that lead to stress and pain. Combating tension is possible through the realization of how thoughts — whether they are emotional or task oriented — directly impact the body as a whole.
This excerpt from Taro Gold’s book, Open Your Mind, Open Your Life: A Book of Eastern Wisdom, cites Mahatma Gandhi’s famous quote which beautifully elucidates the mind-body connection:
Keep your thoughts positive, because your thoughts become your words.
Keep your words positive, because your words become your behavior.
Keep your behavior positive, because your behavior becomes your habits.
Keep your habits positive, because your habits become your values.
Keep your values positive, because your values become your destiny.
Referring to the mind and body as separate entities perpetuates a disconnect in the being as a whole. This is why distinguishing the mental from the physical further exacerbates the notion that the two don’t work together as an indivisible unit. Understanding the relationship between stress and tension begins through the awareness of habits.
There are recurrent thinking habits like “I’ve got to get this done now” and their unconscious counterparts that become visible through posture. The unknown habits are the ones which accrue over time and often appear seemingly out of nowhere — in the form of tension or pain. Modern culture is quick to treat symptoms, such as those related to excessive technology use. However, a holistic approach to addressing the underlying issue would examine how stress and pain work hand in hand. Once the thoughts change, so will the tension.
Bring joy through kindness
Posted: December 31, 2022 Filed under: behavior, healing, meditation, mindfulness | Tags: generousity, kindness Leave a commentAs the New Year begins, bring support through simple acts of kindness. As we share generously, our own well-being improves. I wish you health, happiness and peace for the New Year. Enjoy the two videos on simple acts of kindness.
Biofeedback, posture and breath: Tools for health
Posted: December 1, 2022 Filed under: ADHD, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, computer, digital devices, education, emotions, ergonomics, Evolutionary perspective, Exercise/movement, healing, health, laptops, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, screen fatigue, self-healing, stress management, Uncategorized, vision, zoom fatigue 2 CommentsTwo recent presentations that that provide concepts and pragmatic skills to improve health and well being.
How changing your breathing and posture can change your life.
In-depth podcast in which Dr. Abby Metcalf, producer of Relationships made easy, interviews Dr. Erik Peper. He discusses how changing your posture and how you breathe may result in major improvement with issues such as anxiety, depression, ADHD, chronic pain, and even insomnia! In the presentation he explain how this works and shares practical tools to make the changes you want in your life.
How to cope with TechStress
A wide ranging discussing between Dr. Russel Jaffe and Dr Erik that explores the power of biofeedback, self-healing strategies and how to cope with tech-stress.
These concepts are also explored in the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics. You may find this book useful as we spend so much time working online. The book describes the impacts personal technology on our physical and emotional well-being. More importantly, “Tech Stress” provides all of the basic tools to be able not only to survive in this new world but also thrive in it.
Additiona resources:
Gonzalez, D. (2022). Ways to improve your posture at home.