Welcome the New Year with Inspiration
Posted: December 22, 2025 Filed under: attention, behavior, CBT, cognitive behavior therapy, emotions, healing, health, mindfulness, self-healing | Tags: hope, Inspreiation, meaning, post=traumatic growth, purpose, resilience 1 CommentAs the holiday season begins, I find myself looking back on all that has unfolded this year and looking forward with hope to the year ahead. My social media feed is full of touching, uplifting messages and videos—reminders of resilience, creativity, and the simple goodness in the world. Best wishes for the holidays and the New Year and I hope you will enjoy the two inspiring videos.
1. Nine life lessons from comedian Tim Minchin, presented at the University of Western Australia. His humor and wisdom offer a refreshing take on what truly matters.
2. A powerful story about transforming disaster into blessing.
If you ever feel stuck or unsure about the future, this video is a beautiful reminder that unexpected turns can lead to new possibilities.
Wishing you a healthy and inspiring New Year!
Erik
Reduce Interpersonal Stress*
Posted: December 4, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, Exercise/movement, healing, health, meditation, mindfulness, Pain/discomfort, stress management | Tags: health, mental-health, nutrition, wellness 2 CommentsAdapted from: Peper, E. & Harvey, R. Adjunctive techniques to reduce interpersonal stress at home. Biofeedback. 53(3), 54-57. https://rdcu.be/eMJqt

Stress often triggers defensive reactions—manifesting as anger, frustration, or anxiety that may mirror fight-or-flight responses. These reactions can reduce rational thinking, increase long-term health risks, and contribute to psychological and physiological disorders. and complicate the management of specific symptoms. Outlined are some pragmatic techniques that can be implemented during the day to interrupt and reduce stress.
After we had been living in our house for a few years, a new neighbor moved in next door. Within months, she accused us of moving things in her yard, blamed us when there was a leak in her house, claimed we were blowing leaves from her property onto other neighbors’ properties, and even screamed at her tenants to the extent that the police were called numerous times. Just looking at her house through the window was enough to make my shoulders tighten and leave me feeling upset.
When I drove home and saw her standing in front of her house, I would drive around the block one more time to avoid her while . . . feeling my body contract. Often, when I woke up in the morning, I would already anticipate conflict with my neighbor. I would share stories of my disturbing neighbor and her antics with my friends. They were very supportive and agreed with me that she was crazy. However, the acknowledgment and validation from my friends did not resolve my anger or indignation or the anxiety that was triggered whenever I saw my neighbor or thought of her. I spent far too much time anticipating and thinking about her, which resulted in tension in my own body—my heart rate would increase, and my neck and shoulders would tighten.
I decided to change. I knew I could not change her; however, I could change my reactivity and perspective. Thus, I practiced a “pause and recenter” technique. At the first moment of awareness that I was thinking about her or her actions, I would change my posture by sitting up straight, begin looking upward, breathe lower and slower, and then, in my mind’s eye, send a thought of goodwill streaming to her like an ocean wave flowing through and around her in the distance. I chose to do this series of steps because I believe that within every person, no matter how crazy or cruel, there is a part that is good, and it is that part I want to support.
I repeated this pause and recenter technique many times, especially whenever I looked in the direction of her house or saw her in her yard. I also reframed and reappraised her aggressive, negative behavior as her way of coping with her own demons. Three months later, I no longer reacted defensively. When I see her, I can say hello and discuss the weather without triggering my defensive reaction. I feel so much more at peace living where I am.
When stressed, angry, rejected, frustrated, or hurt, we so often blame the other person (Leary, 2015). The moment we think about that person or event, our anger, indignation, resentment, and frustration are triggered. We keep rehashing what happened. As we relive the experiences in our mind, we are unaware that we are also reliving bodily reactions to past events.
We are often unaware of the harm we are doing to ourselves until we experience physical symptoms such as high blood pressure, gastrointestinal distress, and muscle tightness along with behavioral and psychological symptoms such as insomnia, anxiety, or depression (Carney et al., 2006; Gerin et al., 2012). As we think of past events or interact again with a person involved in those past events, our body automatically responds with a defense reaction as if we were being threatened again in the present moment.
This defense reaction to memory of past threats from a “crazy” neighbor activates our fight-or-flight responses and increases sympathetic activation so that we can run faster and fight more ferociously to survive; however, this reaction also reduces blood flow through the frontal cortex—a process that reduces our ability to think rationally (van Dinther et al., 2024; Willeumier, et al., 2011). When we become so upset and stressed that our mind is captured by the other person, this reaction contributes to symptoms of chronic stress such as an increase in hypertension, myofascial pain, depression, insomnia, cardiovascular disease, and other chronic disorders (Duan et al., 2022; Russell et al., 2015; Suls, 2013).
Sharing our frustrations with friends and others is normal. It feels good to blame people for their personal limitations or mental illness; however, over time, blaming others avoids building adaptive capacity in strengthening skills that reduce chronic stress reactions (Fast & Tiedens, 2010; Lou et al., 2023). The time spent rehashing and justifying our feelings diminishes the time we spend in the present moment and our focus on upcoming opportunities.
In the moment of an encounter with a difficult neighbor, we may not realize that we have a choice. Some people keep living and reacting to past hurts or losses perpetually. Some people can learn to let go and/or forgive and make space in favor of considering new opportunities for learning and growth. Although the choice is ours, it is often very challenging to implement—even with the best intentions—because we react automatically when reminded of past hurts (seeing that person, anticipating meeting or actually meeting that person who caused the hurt, or being triggered by other events that evoke memories of the pain).
What Can You Do
Choose to change your response. Choose to reduce reactivity. Choosing adaptive reactions does not mean you condone what happened or agree that the other person was right. You are just choosing to live your life and not continue to be captured by nor react to the previous triggers. Many people report that after implementing some of the practices described below along with many other stress management techniques, their automatic reactivity was noticeably decreased. They report that their chronic stress symptoms were reduced and they have the freedom to live in present instead of being captured by the painful past.
Pause and Recenter by Sending Goodwill
Our automatic reaction to the trigger elicits a defense reaction that reduces our ability to think rationally. Therefore, the moment you anticipate or begin to react, take three very slow diaphragmatic breaths, inhaling for approximately 4–5 seconds and exhaling for about 5–6 seconds, where one in-and-out breath takes about 10 seconds to complete. As you inhale, allow your abdomen to expand; then as you exhale, slowly make yourself tall and look up. Looking up allows easier access to empowering and positive memories (Peper et al., 2017).
Continue looking up, inhaling slowly to allow the abdomen to expand. Repeat this slow breath again. On the third long, slow breath, while looking up, evoke a memory of someone in whose presence you felt at peace and who loves you, such as your grandmother, aunt, uncle, or even a pet. Reawaken positive feelings associated with memories of being loved. Allow a smile inwardly or outwardly and soften your eyes as you experience the loving memory.
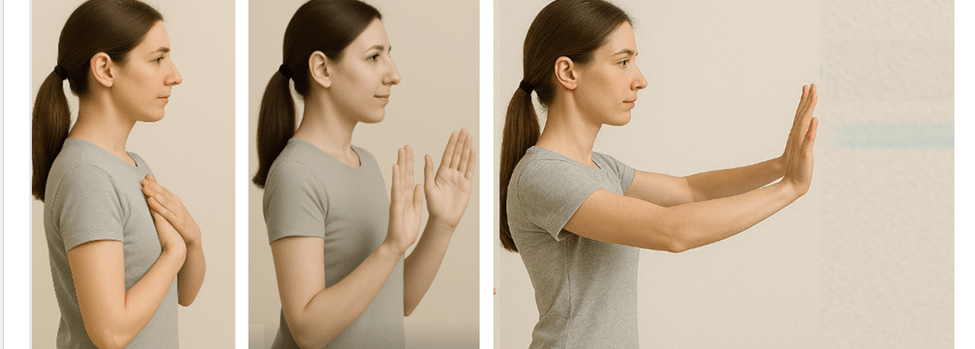
Next, put your hands on your chest, take another long slow breath as your abdomen expands, and as you exhale bring your hands away from your chest and stretch them out in front of you. At the same time in your mind’s eye, imagine sending goodwill to that person involved in the interpersonal conflict that previously evoked your stress response. As if you are sending an ocean wave that is streaming outward to the person.
As you do the pause and recenter technique, remember you are not condoning what happened; instead, you are sending goodwill to that person’s positive aspect. From this perspective, everyone has an intrinsic component—however small—that some label as the individual’s human potential, Christ nature or Buddha nature.
Why would this be effective? This practice short-circuits the automatic stress response and provides time to recenter, interrupting ongoing rumination by shifting the mind away from thoughts about the person or event that induced stress toward a positive memory. By evoking a loving memory from the past, we facilitate a reduction in arousal, evoke a positive mood, and decrease sympathetic nervous system activation (Speer & Delgado, 2017). Slower diaphragmatic breathing also reduces sympathetic activation (Birdee et al., 2023; Siedlecki et al., 2022). By combining body-centered and mind-centered techniques, we can pause and create the opportunity to respond positively rather than reacting with anger and hurt.
Practice Sending Goodwill the Moment You Wake Up
So often when we wake up, we anticipate the challenges, and even the prospect of interacting with a person or event heightens our defense reaction. Therefore, as soon as you wake up, sit at the edge of the bed, repeat the previous practice, pause, and center. Then, as you sit at the edge of the bed, slightly smile with soft eyes, look up, and inhale as your abdomen expands. Then, stamp a foot into the floor while saying, “Today is a new day.” Next, inhale, allowing your abdomen to expand; as you look up, stamp the opposite foot on the floor while saying, “Today is a new day.” Finally, send goodwill to the person who previously triggered your defensive reaction.
Why would this be effective? Looking up makes it easier to access positive memories and thoughts. Stamping your foot on the ground is a nonverbal expression of determination and anchors the thought of a new day, thereby focusing on new opportunities (Feldman, 2022).
Interrupt the Stress Response with the ABCs
The moment you notice discomfort, pain, stress, or negative thoughts, interrupt the cycle with a simple ABC strategy (Peper, 2025):
- Adjust posture and look up
- Breathe by allowing your abdomen to relax and expand while inhaling
- Change your internal dialogue, smile and focus on what you want to do
Why would this be effective? By shifting your posture and gently looking upward, you make it easier to access positive and empowering memories and thoughts (Peper et al., 2019). This simple change in body position can interrupt habitual stress responses and open the doorway to more constructive states.
Slow, diaphragmatic breathing further supports this process by reducing sympathetic arousal and restoring a sense of calm. As your breathing deepens, clarity of mind increases, allowing you to respond rather than react (Peper et al, 2024b; Matto et al, 2025).
Equally important is transforming critical, judgmental, or negative self-talk into affirmative, supportive statements. Describe what you want to do—rather than what you want to avoid. This reframing creates a clear internal guide and significantly increases the likelihood that you will achieve your desired goals.
Complete the Alarm Reaction a Burst of Physical Activity
When you feel overwhelmed and fully captured by a stress reaction, one of the most effective strategies is to complete the fight-flight response with a brief burst of intense physical activity. This momentary action such as running in place, vigorously shaking your arms, or doing a few rapid push-offs from a wall (Peper et al., 2024a). After completing the physical activity implement your stress management strategies such as breathing, cognitive reframing, meditation, etc.
Why would this be effective? The intense physical activity discharges the excessive physiological arousal and interrupts the cycle of rumination. For practical examples and step-by-step guidance, see the article Quick Rescue Techniques When Stressed (Peper et al., 2024a) or the accompanying blog post: https://peperperspective.com/2024/02/04/quick-rescue-techniques-when-stressed/
Discuss Your Issue from the Third-Person Perspective
When thinking, ruminating, talking, texting, or writing about the event, discuss it from the third-person perspective. Replace the first-person pronoun “I” with “she” or “he.” For example, instead of saying “I was really pissed off when my boss criticized my work without giving any positive suggestions for improvement,” say “He was really pissed off when his boss criticized his work without offering any positive suggestions for improvement.”
Why would this be effective? The act of substituting the third-person pronoun for the first-person pronoun interrupts our automatic reactivity because it requires us to observe and change our language, which activates parts of the frontal cortex. This third-person/first-person process creates a psychological distance from our feelings, allowing for a more objective and calmer perspective on the situation, effectively reducing stress by stepping back from the immediate emotional response (Moser et al., 2017). This process can be interpreted as meaning that you are no longer fully captured by the emotions, as you are simultaneously the observer of your own inner language and speech.
Compare Yourself with Others Who are less Fortunate
When you feel sorry for yourself or hurt, take a breath, look upward, and compare yourself with others who are suffering much more. In that moment, consider yourself incredibly lucky compared with people enduring extreme poverty, bombings, or severe disfigurement. Be grateful for what you have.
Why would this be effective? Research shows that when we compare ourselves with people who are more successful, we tend to feel worse—especially when we have low self-esteem. However, when we compare ourselves with others who are suffering more, we tend to feel better (Aspinwall, & Taylor, 1993). This comparison relativizes our perspective on suffering, making our own hardships and suffering seem less significant compared with the severe suffering of others.
Conclusion
It is much easier to write and talk about these practices than to implement them. Reminding yourself to implement them can be very challenging. It requires significant effort and commitment. In some cases, the benefits are not experienced immediately; however, when practiced many times during the day for six to eight weeks, many people report feeling less resentment and experience a reduction in symptoms and improvements in health and relationships.
*This blog was inspired by the podcast “No Hard Feelings,” an episode on Hidden Brain produced by Shankar Vedantam (2025) that featured psychologist Fred Luskin, and the wisdom taught by Dora Kunz (Kunz & Peper, 1983, 1984a, 1984b, 1987).
See the following posts for more relevant information
References
Aspinwall, L. G., & Taylor, S. E. (1993). Effects of social comparison direction, threat, and self-esteem on affect, self-evaluation, and expected success. Journal of Personality and Social Psychology, 64(5), 708–722. https://doi.org/10.1037/0022-3514.64.5.708
Birdee, G., Nelson, K.,Wallston, K., Nian, H., Diedrich, A., Paranjape, S., Abraham, R., & Gamboa, A. (2023). Slow breathing for reducing stress: The effect of extending exhale. Complementary Therapies in Medicine, 73. https://doi.org/10.1016/j.ctim.2023.102937
Carney, C. E., Edinger, J. D., Meyer, B., Lindman, L., & Istre, T. (2006). Symptom-focused rumination and sleep disturbance. Behavioral Sleep Medicine, 4(4), 228–241. https://doi.org/10.1207/s15402010bsm0404_3
Defayette, A. B., Esposito-Smythers, C., Cero, I., Harris, K. M.,Whitmyre, E. D., & López, R. (2023). Interpersonal stress and proinflammatory activity in emerging adults with a history of suicide risk: A pilot study. Journal of Mood and Anxiety Disorders, 2. https://doi.org/10.1016/j.xjmad.2023.100016
Dienstbier, R. A. (1989). Arousal and physiological toughness: Implications for mental and physical health. Psychological Review, 96(1), 84. https://doi.org/10.1037/0033-95x.96.1.84
Duan, S., Lawrence, A., Valmaggia, L., Moll, J., & Zahn, R. (2022). Maladaptive blame-related action tendencies are associated with vulnerability to major depressive disorder. Journal of Psychiatric Research, 145, 70–76. https://doi.org/10.1016/j.jpsychires.2021.11.043
Fast, N. J., & Tiedens, L. Z. (2010). Blame contagion: The automatic transmission of self-serving attributions. Journal of Experimental Social Psychology, 46(1), 97–106. https://doi.org/10.1016/j.jesp.2009.10.007
Feldman, Y. (2022). The dialogical dance–A relational embodied approach to supervision. In C. Butte & T. Colbert (Eds.), Embodied approaches to supervision: The listening body (chap. 2). Routledge. https://www.amazon.com/Embodied-Approaches-Supervision-C%C3%A9line-Butt%C3%A9/dp/0367473348
Gerin,W., Zawadzki,M. J., Brosschot, J. F., Thayer, J. F., Christenfeld, N. J., Campbell, T. S., & Smyth, J. M. (2012). Rumination as a mediator of chronic stress effects on hypertension: A causal model. International Journal of Hypertension, 2012, 453465. https://doi.org/10.1155/2012/453465
Hase, A., O’Brien, J., Moore, L. J., & Freeman, P. (2019). The relationship between challenge and threat states and performance: A systematic review. Sport, Exercise, and Performance Psychology, 8(2), 123. https://doi.org/10.1037/spy0000132
Hassamal, S. (2023). Chronic stress, neuroinflammation, and depression: An overview of pathophysiological mechanisms and emerging anti-inflammatories. Frontiers in Psychiatry,
14, 1130989. https://doi.org/10.3389/fpsyt.2023.1130989
Kunz, D., & Peper, E. (1983). Fields and their clinical implications—Part III: Anger and how it affects human interactions. The American Theosophist, 71(6), 199–203. https://www.researchgate.net/publication/280777019_Fields_and_their_clinical_implications-Part_III_Anger_and_how_it_affects_human_interactions
Kunz, D., & Peper, E. (1984a). Fields and their clinical implications IV: Depression from the energetic perspective: Etiological underpinnings. The American Theosophist, 72(8), 268–275. https://www.researchgate.net/publication/280884054_Fields_and_their_clinical_implications_Part_IV_Depression_from_the_energetic_perspective-Etiological_underpinnings
Kunz, D., & Peper, E. (1984b). Fields and their clinical implications V: Depression from the energetic perspective: Treatment strategies. The American Theosophist, 72(9), 299–306. https://www.researchgate.net/publication/280884158_Fields_and_their_clinical_implications_Part_V_Depression_from_the_energetic_perspective-Treatment_strategies
Kunz, D., & Peper, E. (1987). Resentment: A poisonous undercurrent. The Theosophical Research Journal, IV(3), 54–59. Also in: Cooperative Connection, IX(1), 1–5. https://www.researchgate.net/publication/387030905_Resentment_Continued_from_page_4
Leary, M. R. (2015). Emotional responses to interpersonal rejection. Dialogues in Clinical Neuroscience, 17(4), 435–441. https://doi.org/10.31887/DCNS.2015.17.4/mleary
Lou, Y., Wang, T., Li, H., Hu, T. Y., & Xie, X. (2023). Blame others but hurt yourself: Blaming or sympathetic attitudes toward victims of COVID-19 and how it alters one’s health status. Psychology & Health, 39(13), 1877–1898. https://doi.org/10.1080/08870446.2023.2269400
Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
Moser, J. S., Dougherty, A., Mattson, W. I., Katz, B., Moran, T. P.,Guevarra, D., Shablack, H.,Ayduk,O., Jonides, J., Berman, M. G., & Kross, E. (2017). Third-person self-talk facilitates emotion regulation without engaging cognitive control: Converging evidence from ERP and fMRI. Scientific Reports, 7(1), 4519. https://doi.org/10.1038/s41598-017-04047-3
Peper, E. (2025). Breathe Away Menstrual Pain- A Simple Practice That Brings Relief. the peper perspective-ideas on illness, health and well-being from Erik Peper. https://peperperspective.com/2025/11/22/6825/
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3), 153-169. https://doi.org/10.15540/nr.6.3.1533-1
Peper, E., Lin, I.-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024b). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Russell, M. A., Smith, T. W., & Smyth, J. M. (2015). Anger expression, momentary anger, and symptom severity in patients with chronic disease. Annals of Behavioral Medicine, 50(2), 259–271. https://doi.org/10.1007/s12160-015-9747-7
Siedlecki, P., Ivanova, T. D., Shoemaker, J. K., & Garland, S. J. (2022). The effects of slow breathing on postural muscles during standing perturbations in young adults. Experimental Brain Research, 240, 2623–2631. https://doi.org/10.1007/s00221-022-06437-0
Speer, M. E., & Delgado, M. R. (2017). Reminiscing about positive memories buffers acute stress responses. Nature Human Behaviour, 1, 0093. https://doi.org/10.1038/s41562-017-0093
Suls, J. (2013). Anger and the heart: Perspectives on cardiac risk, mechanisms and interventions. Progress in Cardiovascular Diseases, 55(6), 538–547. https://doi.org/10.1016/j.pcad.2013.03.002
van Dinther, M., Hooghiemstra, A. M., Bron, E. E., Versteeg, A., et al. (2024). Lower cerebral blood flow predicts cognitive decline in patients with vascular cognitive impairment. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 20(1), 136–144. https://doi.org/10.1002/alz.13408
Vedantam, S. (2025). No hard feelings. Hidden brain. Accessed February 5, 2025. https://hiddenbrain.org/podcast/no-hard-feelings/
Willeumier, K., Taylor, D. V., & Amen, D. G. (2011). Decreased cerebral blood flow in the limbic and prefrontal cortex using SPECT imaging in a cohort of completed suicides. Translational Psychiatry, 1(8), e28. https://doi.org/10.1038/tp.2011.28
Zannas, A. S., & West, A. E. (2014). Epigenetics and the regulation of stress vulnerability and resilience. Neuroscience, 264, 157–170. https://doi.org/10.1016/j.neuroscience.2013.12.003
Healing from the Inside Out: How Your Mind–Body Shapes Pain
Posted: June 9, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, healing, health, mindfulness, Pain/discomfort, placebo, self-healing, Uncategorized | Tags: health, meditation, mental-health, mindfulness, Sufism, yoga 2 CommentsAdapted from Peper, E., Booiman, A. C., & Harvey, R. (2025). Pain-There is Hope. Biofeedback, 53(1), 1-9. http://doi.org/10.5298/1081-5937-53.01.16
Pain is more than a physical sensation—it’s shaped by our breath, thoughts, emotions, and beliefs. A striking example: a four-year-old received a vaccination with no pain, revealing the disconnect between what science knows about pain relief and what’s practiced.
The article highlights five key ways to reduce pain:
- Exhale during the painful moment – This activates the parasympathetic nervous system, calming the body. A yogi famously demonstrated this by pushing skewers through his tongue without bleeding or feeling pain.
- Create a sense of safety – Feeling secure can lessen pain and speed healing. Sufi mystics have shown this by pushing knives through their chest muscles without long-term damage, often healing rapidly.
- Distract the mind – Shifting focus can ease discomfort.
- Reduce anticipation – Fear of pain often amplifies it.
- Explore the personal meaning of pain – Understanding what pain symbolizes can shift how we experience it.
The blog also explores how the body regulates pain through mechanisms which influence inflammation and pain signals. In the end, hope, trust, and acceptance, along with mindful breathing, healing imagery, and meaningful engagement, emerge as powerful tools not just to reduce pain—but to promote true healing.
Listen to the AI generated podcast created from this article by Google NotebookLM
I took my four-year-old daughter to the pediatrician for a vaccination. As the nurse prepared to administer the shot in her upper arm. I instructed my daughter to exhale while breathing, understanding that this technique could influence her perception of pain. Despite my efforts, my daughter did not follow my instructions. At that point, the nurse interjected and said, “Please sit in front of your daughter.” Then turned to my daughter and said, “Do you see your father’s curly hair? Do you think you could blow the curls to move them back and forth?” My daughter thought this playful game was fun! As she blew at my hair, the curls moved back and forth while the nurse administered the injection. My daughter was unaware that she had received the shot and felt no pain.
My experience as a father and as a biofeedback practitioner was enlightening–it demonstrated the difference between theoretical knowledge of breathing techniques associated with pain perception and practical applications of clinical skills used by a pediatric nurse practitioner while administering an injection with children. An obvious question raised is: What processes are involved in the perception of pain?
There are many factors influencing pain perception, such as physical/physiological, behavioral and psychological/emotional factors related to the injection as described by St Clair-Jones et al., (2020). Physical and physiological considerations include device type such as needle gauge size as well as formulation volume and ingredients (e.g., adjuvants, pH, buffers), fluid viscosity, temperature, as well as possible sensitivity to coincidental exposures associated with an injection (e.g., sensitivity to latex exam gloves or some other irritant in the injection room).
There are overlapping physical and behavioral-related moderators that include weight and body fat composition, proclivity towards movements (e.g., activity level or ‘squirminess’), as well as co-morbid factors such as whether the person has body sensitization due to rheumatoid arthritis and/or fibromyalgia, for example. Other behavioral factors include a clinician selecting the injection site, along with the angle, speed or duration of injection. Psychological influences center around patient expectations including injection-anxiety or needle phobia, pain catastrophizing, as well as any nocebo effects such as white-coat hypertension.
Although the physical, behavioral and psychological categories allow for considering many physical and physiological factors (e.g., product-related factors), behavioral factors (e.g., injection-related behaviors) and psychological factors (e.g., person-related psychological attitudes, beliefs, cognitions and emotions), this article focuses on a figurative recipe for success associated with benefits of simple breathing to reduce pain perceptions.
Of the many categories of consideration related to pain perceptions, following are five key ‘recipe ingredients’ that contributed to a relatively painless experience:
- Exhaling During Painful Stimuli: Exhaling during a painful stimulus can activate parts of the parasympathetic nervous system leading to promotion of self-healing.
- Creating a Sense of Safety: Ensuring that the child feels safe and secure is crucial in managing pain. My lack of worry and concern and the nurse’s gentle and engaging approach created a comforting environment for my daughter.
- Using Distraction: Distraction techniques, such as focusing on the movement of the curls of the hair served to redirect my daughter’s attention away from the anticipated pain.
- Reducing Anticipation of Pain: My daughter’s previous visits were always enjoyable and as a parent, I was not anxious and was looking forward to the pediatrician visit and their helpful advice.
- Understanding the Personal Meaning of Pain: The approach taken by the nurse allowed the injection to be perceived as a non-event, thereby minimizing the psychological impact of the pain.
Exhaling During Painful Stimuli
Exhaling during painful stimuli facilitates a reduction in discomfort through several physiological mechanisms. During exhalation the parasympathetic nervous system is activated, which slows the heart rate and promotes relaxation, regeneration, reduces anxiety, and may counteract the effects of pain (Magnon et al., 2021). Breathing moderation of discomfort is observable through heart rate variability associated with slow, resonant breathing patterns, where heart rate increases with inhalation and decreases with exhalation (Lehrer & Gevirtz, 2014; Steffen et al., 2017). Physiological studies show that slow, resonant breathing at approximately six breaths per minute for adults, and a little faster for young children, causes the heart rate to increase during inhalation and decrease during exhalation, as illustrated in Figure 1.

Figure 1. Changes in heart rate as modulated by slower breathing at about six breaths per minute
One can experience how breathing affects discomfort when taking a cold shower under two conditions: As the cold water hits your skin: (1) gasping and holding your breath versus (2) exhaling slowly as the cold water hits you. Most people will report that slowly exhaling feels less uncomfortable, though they may still prefer a warm shower.
An Exercise for Use During Medical Procedures: Paring the procedure with inhalation and exhalation
A simple breathing technique can be used to reduce the experience of pain during a procedure or treatment, or during uncomfortable movement post-injury or post-surgery. Physiologically, inhalation tends to increase heart rate and sympathetic activation while exhalation reduces heart rate and increases parasympathetic activity. Often inhalation increases tension in the body, while during exhalation, one tends to relax and let go. The goal is to have the patient practice longer and slower breathing so that a procedure that might be uncomfortable is initiated during the exhalation phase. Applications of long, slow breathing techniques include having blood drawn, insertion of acupuncture needles in tender points, or movement that causes discomfort or pain. Slowly breathing is helpful in reducing many kinds of discomfort and pain perceptions (Joseph et al., 2022; Jafari et al., 2020).
Implementing the technique of exhaling during painful experiences can be deceptively simple yet challenging. When initially practicing this technique, the participants often try too hard by quickly inhaling and exhaling as the pain stimulus occurs. The effective technique involves allowing the abdomen to expand while inhaling, then allowing exhaled air to flow out while simultaneously relaxing the body and smiling slightly, and initiating the painful procedure only after about 25 percent of the air is exhaled.
Some physiological mechanisms that explain how slow breathing influences on pain perceptions have focused on baroreceptors that are mechanically sensitive to pressure and breathing dynamics. According to Suarez-Roca et al. (2021, p 29): “Several physiological factors moderate the magnitude and the direction of baroreceptor modulation of pain perception, including: (a) resting systolic and diastolic AP, (b) pain modality and dimension, (c) type of activated vagal afferent, and (d) the presence of a chronic pain condition It supports the parasympathetic activity that exert an anti-inflammatory influence, whereas the sympathetic activity is mostly pro-inflammatory. Although there are complex physiological interactions between cardiorespiratory systems, arterial pressure and baroreceptor sensitivity that influence pain perceptions, this report focuses on simpler reminders, such as creating a sense of safety for people as a result of better breathing techniques.
Creating a Sense of Safety
My young daughter did not know what to expect and totally trusted me and I was relaxed because the purpose was to enhance my daughter’s future health by giving her a vaccination to prevent being sick at a future time. Often, a parent’s anxiety is contagious to the child since expectations and emotional states influence the experience of medical procedures and pain (Sullivan et al., 2021). For my daughter, the nurse’s calm and confident demeanor contributed to a safe and reassuring environment. As a result, she was more engaged in a playful distraction, blowing at my hair, rather than focusing on the impending shot. This observation underscores an important psychological principle: when individuals do not anticipate pain and feel safe, they are more likely to experience surprise rather than distress. Conversely, anticipation of pain can amplify the perception of discomfort.
For instance, many people have experienced heightened anxiety at the dentist, where they may feel the pain of the needle before it is inserted. Anticipation evocates a past memory of pain that triggers a defensive reaction, increasing sympathetic arousal and sharpening awareness of potential danger. By providing the experience of feeling of safety, parents, caretakers, and medical professionals can play a crucial role in reducing the perceived pain of medical interventions.
Using Distraction
It is inherently difficult to attend to two tasks simultaneously; thus, focusing one’s attention on one task often diminishes awareness of pain and other stimuli (Rischer et al., 2020). For instance, when the nurse asked my daughter to see if she could blow hard enough to make the curls move back and forth, this task captured her attention in a fun and multisensory way. She was engaged visually by the movement of the curls, audibly by the sound of the rushing air, physically by the act of exhalation, and cognitively by following the instructions. Additionally, her success in moving the curls reinforced the activity as a positive and enjoyable experience.
In contrast, it is challenging to allow oneself to be distracted when anticipating discomfort, as numerous cues can continuously refocus attention on the procedure that may induce pain. This experience is akin to attempting to tickle oneself, which typically fails to elicit laughter due to the predictability and lack of external stimulation. Most of us have experienced how challenging it is to be self-directive and not focus on the sensations during dental procedures as discussed in the overview of music therapy for use in dentistry by Bradt and Teague (2018). The challenges are illustrated by my own experience during a dental cleaning
During a dental cleaning, I often attempt to distract myself by mentally visualizing the sensation of breathing down my legs while repeating an internal mantra or evoking joyful memories. Despite these efforts, I frequently find myself attending to the sound of the ultrasonic probe and the sensations in my mouth. To manage this distraction more effectively, I have found that external interventions such as listening to music or an engaging audio story through earphones is more beneficial.
From this perspective, we wished that the dentist could implement an external intervention by collaborating with a massage therapist to provide a simultaneous foot massage during the teeth cleaning. This dual stimulation would offer enough competing sensations to divert attention from the dental procedure to the comfort of the foot massage.
Reducing Anticipation of Pain
A crucial factor in the experience of pain is the anticipation and expectation of discomfort, which is often shaped by previous experiences (Henderson et al., 2020; Reicherts et al., 2017). When encountering a novel experience, we might interpret the sensations as novel rather than painful. Similar phenomena can be observed in young children when they fall or get hurt on the playground. They may initially react with surprise or shock and may look for their caretaker. Depending the reaction of their caregiver, they may begin to cry or they might cry briefly, stop and resume playing.
Conversely, the anticipation of pain can heighten sensitivity to any stimuli, causing them to be automatically perceived as painful. Anticipatory responses function as a form of mental rehearsal, where the body responds in a manner similar to the actual experience of pain. For example, Peper, et al. (2015) showed that when a pianist imagined playing the piano, her forearm flexor and extensor muscles exhibited slight contractions, even though there was no observable movement in her arm and the pianist was unaware of these contractions (see Figure 2).

Figure 2. The covert SEMG increase in forearm SEMG as the participant imagined playing the piano (reproduced by permission from Peper et al., 2015).
These kind of muscle reactions are also visible in sportsmen. For example, while mentally racing a lap on a motorbike, the arm muscles act like as if the person is racing in the dust of the circuit (Booiman 2018). The blood flow (BVP) and blood vessels are reacting even quicker than muscle tension on thoughts and expected (negative) experiences.
These findings underscore how anticipatory responses can mirror actual physical experiences, providing insights into how anticipation and expectancy can modify pain perception (Henderson et al., 2020). Understanding these mechanisms allows for the development of interventions aimed at managing pain through the modification of expectations and the introduction of distraction techniques.
The Personal Meaning of Pain (adapted from Peper, 2015)
The personal meaning of pain is a complex construct that varies significantly based on context and individual perception. For example, consider the case of a heart attack. Initially, the person might experience chest pain and dismiss it, which can be attributed to societal norms where people are conditioned to ignore pain. However, once the pain is assumed or diagnosed to be a heart attack, the same pain may become terrifying as it may signify the potential for life-threatening consequences. Following bypass surgery, the pain might actually be worse, but it is now reframed positively as a sign of the surgery’s success and a symbol of hope for survival. Thus, the meaning of pain evolves from one of fear to one of reassurance and recovery.
This notion that pain is defined by the context in which it occurs is crucial (Carlino et al., 2014). For instance, childbirth, despite being intensely painful, is understood within the context of a natural and temporary process that leads to the birth of a child. This perception is often reinforced nonverbally by a supportive midwife or doula. It may be helpful if the midwife or doula has given birth herself. Without words she communicates, “This is an experience that you can transcend, just as I did.” Psychologically/emotionally, the pain serves a higher purpose, to deliver a child into the world, which may also make the pain more bearable. There is a reward, namely the child. In addition, women who have had training and information about the process of childbirth have a significant faster delivery (about 2 hours faster).
Piercing the body without reporting pain or bleeding
To further illustrate this concept, Peper et al. (2006) and Kakigi et al. (2005) physiologically monitored the experiences of a Japanese Yogi Master, Mitsumasa Kawakami,who performed voluntary body piercing with unsterilized skewers, as depicted in Figure 3 (Peper, 2015).

Figure 3. Demonstration Japanese Yogi Master, Mitsumasa Kawakami, voluntary piercing the tongue and neck with unsterilized skewers while experiencing no pain, bleeding or infection (reproduced by permission from Peper et al., 2006).
See the video recording of tongue piercing study recorded November 11, 2000, at the annual Biofeedback Society Meeting of California, Monterey, CA, https://youtu.be/f7hafkUuoU4 (Peper & Gunkelman, 2007).
Despite the visual discomfort of seeing this procedure, physiological data from pulse, EEG and breathing patterns revealed that the yogi did not experience pain. During the piercing, his heart rate was elevated, his electrodermal activity was low and unresponsive, and his EEG showed predominant alpha waves, indicating a state of focused meditation rather than pain. This study suggests that conscious self-regulation, rather than dissociation, can be employed to control attention and responsiveness to painful stimuli and possibly benefit individuals with chronic pain (Peper et al., 2005).
A similar phenomenon was observed among a spiritual gathering of Kasnazani Sufi initiates in Amman, Jordan and physiologically monitored during demonstrations as part of a scientific meeting. The Kasnazani order is a branch of Sufism that has gained widespread popularity in Iraq and Iran, particularly among the Kurdish population. What sets the Kasnazani order apart is its inclusive approach—it welcomes both Sunni and Shia Muslims, making no distinction between them. During spiritual gatherings, some followers perform acts that might seem extreme to outsiders: piercing their bodies. These acts are seen as expressions of deep spiritual devotion and are performed in a state believed to be beyond normal physical sensation. With the permission of their Sheikh Mohammed Abdul Kareem Kasnazani, they pierced their face, neck arms, or chest and reported no pain or bleeding and heal quickly, as shown in Figure 4.

Figure 4. Voluntary piercing and with unsterilized skewers by Sufi initiates and subsequent tissue healing after 14 hours.
See the video recording of the actual piercing study organized by Erik Peper and Howard Hall with Thomas Collura recording the QEEG at the 2013 Annual Scientific Meeting of the Association for Applied Psychophysiology and Biofeedback, Portland, OR (Peper & Hall, 2013; Collura et al., 2014), https://www.youtube.com/watch?v=56nLZyG87oc
What Factors Decrease the Experience of Pain and Promote Rapid Healing with the Absence of Bleeding?
In the case of the Kasnazani Sufis, they framed their experience as a normal, spiritual phenomenon that occurs in a setting of religious faith and total trust in their spiritual leader (Hall, 2011). The Sufis reported that they had permission and support from their master, Sheikh Mohammed Abdul Kareem Kasnazani. Thus, they felt totally safe and protected—they had no doubt they could experience the piercing with reasonable composure and that their bodies would totally heal. Even if pain occurred, it was not to be feared but part of the process. The experience may be modulated by the psychological context of the group, the drumming, and the chanting. The phenomenon was not simply a matter of belief; they knew that healing would occur because they had seen it many times in the past. The knowledge that healing would occur rapidly was transmitted as a felt sense in the group that this is possible and following the expected normal pattern.
The most impressive finding was that the physiology markers (heart rate, skin conductance, and breathing) were normal and there was no notable change (Booiman et al., 2015; Peper & Hall, 2013) and the QEEG indicated the inhibition of pain (Collura et al., 2014).
Clinical implications
These observations underscore that the context of pain—whether through personal meaning, spiritual belief, or communal support—can significantly alter its perception and management. This concept is also reflected in clinical settings, where a lack of diagnosis or acknowledgment of pain can exacerbate suffering. An isolated individual, alone at night with the physical sensation of pain, may find the pain tremendously stressful, which tends to intensify the experience. In this situation, there are concerns about the future: “It may get worse, it will not go away, I’m going to die from this, maybe I’ll die alone,” and the worry continues.
If one can let go of these thoughts, breathe through the pain, relax the muscles and experience a feeling of hope, the pain is often reduced. On the other hand, focusing on the pain may intensify it. On the other hand, the meaning of pain implies survival or hope as sometimes is observed in injured soldiers. In context of the hospital setting: “I have survived and I am safe.”
What are the implications of these experiences in clinical settings in which the patient is in constant pain and yet has not received an accurate diagnosis? Or, in cases in which the patient has a diagnosis, such as fibromyalgia, but treatment has not reduced the pain significantly? Experiencing pain or illness that goes undiagnosed, and/or that is not acknowledged, may increase the level of stress and tension, which can contribute to more pain and discomfort. As long as we are resentful/angry/resigned to the pain or especially to the event that we believe has caused the pain, the pain often increases. Another way to phrase this is that chronic sympathetic arousal increases the sensitivity to pain and reduces healing potential (Kyle & McNeil, 2014).
Acknowledgement means having an accurate diagnosis, validating that the pain experience is legitimate and that it is not psychosomatic (imagined), because that simply makes the experience of pain worse. Once the patient has a more accurate diagnosis, treatment may be possible.
When one has constant, chronic, or unrelenting pain, this evokes hopelessness and the patient is more likely to get depressed (Sheng et al., 2017; Meda et al., 2022). The question is, What can be done? The first step for the patients is to acknowledge to themselves that it does not mean that the situation is unsolvable. It is important to focus on other options for diagnosis and treatment and take one’s own lead in the healing/recovery process. We have observed that a creative activity that uses the signals of pain to evoke images and thoughts to promote healing may reduce pain (Peper et al., 2022). Pain awareness may be reduced when the person initiates actions that contribute to improving the well-being of others.
Overall, pain appears to decrease when a person accepts without resignation what has happened or is happening. A useful practice that may change the pain experience is to do an appreciation practice. Namely, appreciate what that part of the body has done for you and how so often in the past you may have abused it. For example, if you experience hip pain, each time you are aware of the pain, thank the hip for all the work it has done for you in the past and how often you may have neglected it. Keep thanking it for how it has supported you.
Pain often increases when the person is resentful or wished that what has happened had not happened (Burns et al., 2011). If the person can accept where they are and focus on the new opportunities and new goals can achieve, pain may still occur; however, the quality is different. Focus on what you can do and not on what you cannot do. See Janine Shepherd’s 2012 empowering TED talk, “A broken body isn’t a broken person.”
Conclusion
The primary lessons from studying the yogi and the Sufis are the concepts that a sense of safety, acceptance, and purpose can transform the experience of pain. Expressing confidence in a patient’s recovery prospects places the focus on their ability to recover. Incorporating these elements into clinical care may offer new avenues for addressing chronic pain and improving patient outcomes (Booiman & Peper, 2021).
We propose the first step is to create an atmosphere of hope, trust and safety and to emphasize the improvements made (even small ones). Then master effortless breathing to increase slow diaphragmatic breathing and teach clients somato-cognitive techniques to refocus their attention during painful stimuli (mindfulness) (Pelletier & Peper, 1977; Peper et al., 2022). Using the slow breathing as the overlearned response would facilitate the recovery and regeneration following the painful situation. To develop mastery and be able to apply it under stressful situations requires training and over-learning. Yoga masters overlearned these skills with many years of meditation. With mastery, patients may learn to abort the escalating cycle of pain, worry, exhaustion, more pain, and hopelessness by shifting their attention and psychophysiological responses. In clinical practice, strategies such as hypnotic induction, multisensory distraction, self-healing visualizations, and mindfulness techniques can be employed to manage pain. A foundational principle is that healing is promoted when the participant feels safe and accepted, experiences suffering without blame, and looks forward to life with meaning and purpose.
Acknowledgement
We thank Mitsumasa Kawakami, Sheikh Mohammed Abdul Kareem Kasnazani, and Safaa Saleh for their generous participation in this research and I thank our research collegues Thomas Collura, Howard Hall and Jay Gunkelman for their support and collaboration.
References
Booiman, A.C. (2018) Posture corrections and muscle control can prevent arm pump during motocross, a case study. Beweegreden, 14(3), 24–27. https://www.researchgate.net/publication/382853342
Booiman, A. C. & Peper, E. (2021) De pijnbeleving van Kaznazanisoefi’s, wat kan de fysiotherapeut daarvan leren? Physios Vol 13 (3) pp. 32–35. https://www.physios.nl/tijdschrift/editie/artikel/t/de-pijnbeleving-van-kaznazani-soefi-s-wat-kan-de-fysiotherapeut-daarvan-leren
Booiman, A., Peper, E., Saleh, S., Collura, T., & Hall, H. (2015). Soefi piercing een andere kijk op pijnervaring en pijnmanagement. https://biofeedbackhealth.files.wordpress.com/2011/01/soefi-en-pijn-management-08-12-20131.pdf
Bradt. J. & Teague, A. (2018). Music interventions for dental anxiety. Oral Diseases, 24(3), 300–306. https://doi.org/10.1111/odi.12615
Burns, J.W., Quartana, P., & Bruehl, S. (2011). Anger suppression and subsequent pain behaviors among chronic low back pain patients: moderating effects of anger regulation style. Annals of Behavioral Medicine, 42(1), 42–54. https://doi.org/10.1007/s12160-011-9270-4
Carlino, E., Frisaldi, E., & Benedetti, F. (2014). Pain and the context. Nature Reviews Rheumatology, 10(6), 348–355. https://doi.org/10.1038/nrrheum.2014.17
Collura, T. F., Hall, H., & Peper, E. (2014). A Sufi self-piercing analyzed with EEG and sLORETA. Applied Psychophysiology and Biofeedback, 39(3–4), 293–293. https://brainmaster.com/wp-content/uploads/2020/08/AAPB_BOS05_2015_Pain_Controll.pdf
Hall, H. (2011). Sufism and healing. In Neuroscience, Consciousness and Spirituality (pp. 263–278). Springer Netherlands. https://doi.org/10.1007/978-94-007-2079-4_16
Henderson, L. A., Di Pietro, F., Youseff, A. M. , Lee, S., Tam, S., Akhter, R., Mills, E.P., Murray, G. M., Peck, C.C., & Macey, P.M. (2020). Effect of expectation on pain processing: A psychophysics and functional MRI analysis. Frontiers in Neuroscience, 14. https://doi.org/10.3389/fnins.2020.00006
Jafari, H., Gholamrezaei, A., Franssen, M., Van Oudenhove, L., Aziz, Q., Van den Bergh, O., Vlaeyen, J. W. S., & Van Diest, I. (2020). The Journal of Pain, 21(9–10), 1018−1030. https://doi.org/10.1016/j.jpain.2019.12.010
Joseph, A. E., Moman, R. N., Barman, R. A., Kleppel, D. J., Eberhart, N. D., Gerberi, D. J., Murad, M. H., & Hooten, W. M. (2022). Effects of slow deep breathing on acute clinical pain in adults: A systematic review and meta-analysis of randomized controlled trials. Journal of Evidence-Based Integrative Medicine, 27, 2515690X221078006. https://doi.org/10.1177/2515690X221078006
Kakigi, R. Nakata, H., Inui, K., Hiroe,N. Nagata, O., Honda, M., Tanaka, S., Sadato, N. & Kawakami, M. (2005). Intracerebral pain processing in a Yoga Master who claims not to feel pain during meditation. European Journal of Pain. 9(5), 581–581. https://doi.org/10.1016/j.ejpain.2004.12.006
Kyle, B. N., & McNeil, D. W. (2014). Autonomic arousal and experimentally induced pain: a critical review of the literature. Pain Research Management, 19(3),159–167. https://doi.org/10.1155/2014/536859
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Magnon, V., Dutheil, F. & Vallet, G. T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11, 19267. https://doi.org/10.1038/s41598-021-98736-9
Meda, R. T., Nuguru, S .P., Rachakonda, S., Sripathi, S., Khan, M. I., & Patel, N. (2022). Chronic paininduced depression: A review of prevalence and management. Cureus,14(8):e28416. https://doi.org/10.7759/cureus.28416
Pelletier, K. R. and Peper, E. (1977). Developing a biofeedback model: Alpha EEG as a means for pain control. International Journal of Clinical and Experimental Hypnosis, 24(4), 361–371. https://doi.org/10.1080/00207147708415991
Peper, E. (2015). Pain as a contextual experience. Townsend Letter—The Examiner of Alternative Medicine, 388, 63–66. https://www.researchgate.net/profile/Erik-Peper/publication/284721706_Pain_as_a_contextual_experience/links/5657483908ae1ef9297bab71/Pain-as-a-contextual-experience.pdf
Peper, E., Cosby, J., & Almendras, M. (2022). Healing chronic back pain. NeuroRegulation, 9(3), 164–172. https://doi.org/10.15540/nr.9.3.164
Peper, E. & Gunkelman, J. (2007). Tongue piercing by a yogi: QEEG observations and implications for pain control and health. Presented at the 2007 meeting of the Biofeedback Society of California. https://www.researchgate.net/publication/382394304_Tongue_Piercing_by_a_Yogi_QEEG_Observations_and_Implications_for_Pain_Control_and_Health
Peper, E. & Hall, H. (2013). What is possible: A discussion, physiological recording and actual demonstration in voluntary pain control by Kasnazani Sufis. Presented at the 44st Annual Meeting of the Association for Applied Psychophysiology and Biofeedback. Portland, OR.
Peper, E., Kawakami, M., Sata, M. & Wilson, V.S. (2005). The physiological correlates of body piercing by a yoga master: Control of pain and bleeding. Subtle Energies & Energy Medicine Journal, 14(3), 223–237. https://biofeedbackhealth.org/wp-content/uploads/2011/01/366-663-1-sm.pdf
Peper, E., Nemoto, S., Lin, I-M., & Harvey, R. (2015). Seeing is believing: Biofeedback a tool to enhance motivation for cognitive therapy. Biofeedback, 43(4), 168–172. https://doi.org/10.5298/1081-5937-43.4.03
Peper, E., Wilson, V.E., Gunkelman, J., Kawakami, M. Sata, M., Barton, W. & Johnston, J. (2006). Tongue piercing by a yogi: QEEG observations. Applied Psychophysiology and Biofeedback. 34(4), 331–338. https://doi.org/10.1007/s10484-006-9025-3
Reicherts, P., Wiemer, J., Gerdes, A.B.M., Schulz, S.M., Pauli, P., & Wieser, M.J. (2017). Anxious anticipation and pain: The influence of instructed vs conditioned threat on pain. Social Cognitive and Affective Neuroscience, 12(4), 544–554. https://doi.org/10.1093/scan/nsw181
Rischer, K. M., González-Roldán, A. M., Montoya, P., Gigl, S., Anton, F., & van der Meulen, M. (2020). Distraction from pain: The role of selective attention and pain catastrophizing. European Journal of Pain, 24(10),1880–1891. https://doi.org/10.1002/ejp.1634
Sheng, J., Liu, S., Wang, Y., Cui, R., & Zhang, X. (2017). The link between depression and chronic pain: Neural mechanisms in the brain. Neural Plasticity, 9724371. https://doi.org/10.1155/2017/9724371
Shepherd, J. (2012). A broken body isn’t a broken person. TEDxKC. Accessed July 19, 2024. https://www.ted.com/talks/janine_shepherd_a_broken_body_isn_t_a_broken_person?subtitle=en
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The impact of resonance frequency breathing on measures of heart rate variability, blood pressure, and mood. Frontiers in Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
St Clair-Jones, A., Prignano, F., Goncalves, J., Paul, M., & Sewerin, P. (2020). Understanding and minimising injection-site pain following subcutaneous administration of biologics: A narrative review. Rheumatology and therapy, 7, 741–757. https://doi.org/10.6084/m9.figshare.13034609
Suarez-Roca, H., Mamoun, N., Sigurdson, M. I., & Maixner, W. (2021). Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Comprehensive Physiology, 11(2), 1373. https://doi.org/10.1002/cphy.c190038
Sullivan, V., Sullivan, D. H. & Weatherspoon, D. (2021). Parental and child anxiety perioperatively: Relationship, repercussions, and recommendations. Journal of PeriAnesthesia Nursing, 36(3), 305–309. https://doi.org/10.1016/j.jopan.2020.08.015
Wilber, K. (1997). An integral theory of consciousness. Journal of Consciousness Studies, 4(1), 71–92. https://www.ingentaconnect.com/content/imp/jcs/1997/00000004/00000001/748
The Power of No
Posted: March 6, 2025 Filed under: behavior, Breathing/respiration, CBT, cognitive behavior therapy, emotions, healing, health, self-healing, stress management, Uncategorized | Tags: assertiveness, emotional awareness, HIV, immune resilence, surviaval 1 CommentBrenda Stockdale, PhD and Erik Peper, PhD
Adapted from: Stockdale, B. & Peper, E. (2025). How the Power of No Supports Health and Healing. Townsend Letter-Innovative Health Perspectives, March15, 2025 https://townsendletter.com/the-power-of-no/

I felt exhausted and just wanted to withdraw to recharge. Just then, my partner asked me to go to the store to get some olive oil. I paused, took a deep breath, and checked in with myself. I realized that I needed to take care of myself. After a few seconds, I responded, “No, I cannot do it at this time.”
It was challenging to say this because, in the past, I would have automatically said “yes” to avoid disappointing my partner. However, by saying “yes” and ignoring my own needs, I would have become even more exhausted, hindering my recovery. I felt proud that I had said “no.” By listening to myself, I took charge and prioritized my own healing.
For many people, saying “no” feels unkind, and we want to be kind while avoiding burdening others. Nevertheless, how you answer this question may have implications for your health! Consider the following question and rate it on a scale from 1 (never) to 5 (always):
How often do you do favors for people when you really don’t want to? Namely, things you really don’t want to do but do anyway because someone asks you to and you don’t want to or can’t say “No.“
In analysis of numerous studies, Prof. George Solomon and Dr. Lydia Temoshok reported that a low score on this question (indicating the ability to say No) was the best predictor of related outcomes across studies, such as survivorship with AIDS as well as more favorable HIV immune measures (Solomon, et al, 1987). This aligns with research suggesting that excessive compliance, self-sacrifice, and conflict avoidance (i.e., people-pleasing) in individuals with cancer and chronic illness may weaken, rather than strengthen, their immune systems (Temoshok, & Dreher, 1992).
Unconsciously avoiding or suppressing distressing thoughts, emotions, or memories instead of dealing with them––a process known as repressive coping–– may even contribute to an increased risk of cancer and cardiovascular disease (Mund & Mitte, 2012). Avoiding emotional cues or dismissing feelings may seem self-protective but can lead to reflexive or automatic behavior such as saying “yes” when individuals would rather say “no.” Although the conflict may not be consciously recognized, it can manifest physiologically (Mund & Mitte, 2012). Paying attention to states of tension, or symptoms such as headache or loss of appetite can serve as a doorway to exploring unacknowledged feelings.
Automatically saying “yes” and sacrificing yourself may contribute to poor boundaries, leading to chronic stress which is linked to numerous health issues, including hypertension and immune dysfunction (Dai et al., 2020; Segerstrom et al., 2004; Deci & Ryan, 2008). Conversely, research indicates that individuals who assertively manage stress—rather than suppress emotions and avoid conflict—demonstrate stronger immune resilience (Ironson et al., 2005; Dantzer et al, 2018) and are better protected against burnout and prolonged emotional distress (Deci & Ryan, 2018).
When faced with illness––or even the possibly death––ask yourself: “Do I really want to do this, or am I doing it just to please my partner, children, parents, doctors, or society? By doing what truly brings me joy and meaning, what do I have to lose?” Altruism is valuable and an important part of maintaining health. At the same time boundaries and assertiveness are essential.
Psychologist Lawrence LeShan (1994) reported that when cancer patients began to seek and start singing their “own song,” their cancer regressed in numerous cases, and some experienced total remission. Living your own song means doing what you truly desire rather than following the expectations of parents, society, or economic pressures. It is important to keep in mind that while psychological factors can influence overall health, the development of cancer is a multifaceted process involving genetic, lifestyle and environmental factors.
The Key Question: When and How to Say “No”?
The answer lies in emotional awareness and acting on it. One woman with cancer confided, “I’ve operated in the realm of expected behavior for so long that I no longer know what I want or feel” (Stockdale, 2009). Teasing out our true feelings—hour by hour, as Bernie Siegel, M.D., recommends—helps us recognize where we stand (Siegel, 1986; Siegel & August, 2004). This practice fosters a sense of agency, a cornerstone of resilience that directly contributes to well-being.
For those accustomed to prioritizing others’ needs over their own, learning to say “No” takes practice. Although one may have feelings of vulnerability and even guilt by disappointing someone, one person shared that only after he stopped exclusively prioritizing others–and instead learned to love himself as well as his neighbor–did he realize how much people genuinely cared for him. Authentic connection is essential for well-being, but trust cannot develop without agency and the freedom to say “no.”
What to Do Before Automatically Saying Yes
When someone asks you for help or a favor, pause. Look up, take a slow, diaphragmatic breath, and ask yourself, “Do I want to do this? What would I recommend to another person to do in this situation?”
(In cases where you are asked or ordered to harm another person or do something illegally, ask yourself, “What would a moral person do?”)
If you feel that you would rather not—whether because you are tired or it interferes with your own priorities—say “No.” Saying “No” does not mean you are unwilling to help; it simply means that, at this moment, you are listening to yourself. When we listen to ourselves and act accordingly, we enhance our immune competence and self-healing.
Obviously, if saying “No” would put another person in danger or in crisis, then say “Yes,” if possible. However, true crises are rare. If emergencies happen frequently, they are not true crises or emergencies but rather a result of poor planning.
Saying “No” can be challenging, but if you constantly say “Yes,” you may eventually become resentful and exhausted, increasing your stress and decreasing your ability to heal. You may even notice that when your own well-being is appropriately prioritized you will be in a better position to show up for others in a whole-hearted way, when it is right for them and for you.
Saying “No” Can Be Life-Saving
Beyond personal relationships, saying “No” can be crucial in medical settings. Anthony Kaveh, M.D., a Stanford- and Harvard-trained anesthesiologist and integrative medicine specialist, asserts, “Nice patients come out last” (Kaveh, 2024). Kaveh emphasizes that trusting our instincts is crucial, as the fear of displeasing others can lead to dangerous “fake nice” behavior.
See the YouTube video #1 Mistake You Make with Doctors: Medical Secrets (https://www.youtube.com/watch?v=9-E3CHHX05c)
A case example is illustrated by Tracy who was hospitalized with complex fractures of the tibia and fibula. After five surgeries, she felt something was terribly wrong–she knew she was dying. However, the nurses dismissed her concerns. Taking control, she infuriated the staff by calling 911, which prompted a doctor to check on her. It was discovered that excessive negative pressure applied to the drain caused five pints of her blood to flow into her leg causing compartment syndrome.
She was bleeding to death. Tracy’s intuition, resilience, and refusal to comply saved her life. Kaveh argues that those who don’t trust their instincts are more likely to err on the side of “nice” and suffer as a result.
Learning to say “No” is empowering as illustrated by one woman who discovered its importance in a cancer educational group she attended. She shared her success in saying “No” with humor, explaining, “I just tell people it’s this group’s fault because I used to be a nice person.”
Learning to listen to yourself before agreeing or disagreeing to do something, may also help you maintain your integrity when faced with pressure to follow an immoral suggestion or order. So often due to social, economic, corporate, or political pressure, people may be asked to do something they later regret (Sah, 2025). The courage to disagree and act according to your moral consciousness is the bases of the Nuremberg Code, established by the American judges in 1947 at the Nuremberg trials for Nazi doctors (Shuster, 1997).
Finally, learning to say “No” and listen to your needs takes practice and time. Explore the following Body Dialogue technique to tap into your intuitive wisdom. You can use it anytime you need clarity about your feelings and responses to life’s challenges.
Breathe in deeply and engage all your senses. When you are ready, focus on the sensation of breathing. You don’t have to make anything happen, just feel the air moving in and out. Your lungs, vital to energy production, obtain oxygen from the atmosphere and bring it to millions of specialized cells. All without your conscious awareness, your breath moves in and out, removing toxins and waste from your body and bringing oxygen in.
The beautiful filtering process even protects your heart. That great organ, pumping rhythmically, picks up the oxygen and delivers it to all the vessels of your body, contracting more than two billion times during a normal lifespan. With deep appreciation for this magnificent pump, move your attention down into your abdomen. On the right side is the largest organ in your body, your liver. This amazing organ filters toxins and chemicals, and aids in digestion. This powerhouse of function can even regenerate itself after losing as much as three quarters of its tissue. With a sense of admiration, imagine all that these great and vital organs accomplish. With gratitude, slowly move on to your spleen, your pancreas and all the other organs and systems of your body, taking your time to appreciate and acknowledge all that they do for you.
Consider the multitude of vital functions that take place every minute of every day and thank your body for all that is right with you. All of these complex functions take place without effort or even awareness on your behalf––they just happen. Ask now if there something you can do for your body to help it heal, repair or regenerate more completely. Listen closely to your own intuitive awareness. Is there anything you can do to make your body’s job easier or reduce a burden of some kind? Gently notice if there are any thoughts or behaviors that make some symptoms worse or better. What feels heavy or burdensome? Who or what in your life feels supportive? As you review the past few days or weeks what would you like to adjust? When might saying ‘no’ would bring a sense of relief? Imagine what it would be like to operate in your own best interest. What might that include?
Are there positive feelings you would like to experience more often? If you had to choose just one, what would it be? In what way could you bring more of that quality into your life? In your mind’s eye, see that happening now. Feel the peace or the joy or whatever it is you have chosen radiate throughout your being. And if it seems good to you, carry it with you, back to the present moment and enjoy the fullness of that sensation. When it seems right to you, again focus gently on your body, bringing your attention back to the chair or the place you happen to be. And filled with gratitude, stretch your arms wide with appreciation for all that is right with you.
Additional useful blogs
References
Dai, S., Mo, Y., Wang, Y., Xiang, B., Liao, Q., Zhou, M., Li, X., Li, Y., Xiong, W., Li, G., Guo, C., & Zeng, Z. (2020). Chronic Stress Promotes Cancer Development. Frontiers in oncology, 10, 1492. https://doi.org/10.3389/fonc.2020.01492
Dantzer, R., Cohen, S., Russo, S. J., & Dinan, T. G. (2018). Resilience and immunity. Brain, behavior, and immunity, 74, 28–42. https://doi.org/10.1016/j.bbi.2018.08.010
Deci, E. L., & Ryan, R. M. (2008). Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology / Psychologie canadienne, 49(3), 182–185. https://doi.org/10.1037/a0012801
Deci, E. L., & Ryan, R. M. (2018). Self-determination theory: Basic psychological needs in motivation, development, and wellness. New York: Guilford Publications. https://www.amazon.com/Self-Determination-Theory-Psychological-Motivation-Development/dp/1462538967
Ironson, G., O’Cleirigh, C., Fletcher, M. A., Laurenceau, J. P., Balbin, E., Klimas, N., Schneiderman, N., & Solomon, G. (2005). Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosomatic medicine, 67(6), 1013–1021. https://doi.org/10.1097/01.psy.0000188569.58998.c8
Kaveh, A. (2024). #1 Mistake You Make With Doctors. Medical Secrets, YouTube, https://www.youtube.com/watch?v=9-E3CHHX05c
LeShan, L. (1994). Cancer As a Turning Point: A Handbook for People with Cancer, Their Families, and Health Professionals – Revised Edition. New York: Penguin Publishing Group. https://www.amazon.com/Cancer-As-Turning-Point-Professionals/dp/0452271371
Mund, M., & Mitte, K. (2012). The costs of repression: a meta-analysis on the relation between repressive coping and somatic diseases. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 31(5), 640–649. https://doi.org/10.1037/a0026257
Sah, S. (2025. Defy: The power of no in a world that demands yes. London: One World Publications. https://www.amazon.com/Defy-Power-World-That-Demands/dp/0593445775
Shuster, E. (1997). Fifty years later: The significance of the Nuremberg code. The New England Journal of Medicine, 337(20), 1436-1440. https://doi.org/10.1056/NEJM199711133372006
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological bulletin, 130(4), 601–630. https://doi.org/10.1037/0033-2909.130.4.601
Siegel, B. (1986). Love, medicine & miracles. New York: William Morrow Paperbacks; https://www.amazon.com/Love-Medicine-Miracles-Bernie-Siegel-dp-B00A2KKOBI
Siegel, B. & August, Y. (2004). Help Me Heal. Hay House. https://www.amazon.com/Help-Heal-Bernie-Siegel-M-D/dp/1401900607/
Solomon, G. F., Temoshok, L., O’Leary, A., & Zich, J. (1987). An intensive psychoimmunologic study of long-surviving persons with AIDS. Pilot work, background studies, hypotheses, and methods. Annals of the New York Academy of Sciences, 496, 647–655. https://doi.org/10.1111/j.1749-6632.1987.tb35825.x
Stockdale, B. (2009). You can beat the odds: Surprising factors behind chronic illness and cancer––the 6-week program for Optimal Immunity. Boulder, CO: Sentient Publications. https://www.amazon.com/You-Can-Beat-Odds-Surprising-ebook/dp/B00KMDKOVA
Temoshok L. (1987). Personality, coping style, emotion and cancer: towards an integrative model. Cancer surveys, 6(3), 545–567. https://pubmed.ncbi.nlm.nih.gov/3326661/
Temoshok, L., & Dreher, H. (1992). The type C connection: The behavioral links to cancer and immune dysfunction. New York: Random House. https://www.amazon.com/Type-Connection-Behavioral-Cancer-Health/dp/0394575237
Use the power of your mind to transform health and aging
Posted: February 18, 2025 Filed under: attention, behavior, cancer, CBT, cognitive behavior therapy, COVID, education, health, meditation, mindfulness, Pain/discomfort, placebo, stress management, Uncategorized | Tags: health, imimune function, longevity, mental-health, mind-body, nutrition, Reframing, wellness Leave a commentMost of the time when I drive or commute by BART, I listen to podcasts (e.g., Freakonomics, Hidden Brain, this podcast will kill you, Science VS, Huberman Lab). although many of the podcasts are highly informative; , rarely do I think that everyone could benefit from it. The recent podcast, Using your mind to control your health and longevity, is an exception. In this podcast, neuroscientist Andrew Huberman interviews Professor Ellen Langer. Although it is three hours and twenty-two minute long, every minute is worth it (just skip the advertisements by Huberman which interrupts the flow). Dr. Langer delves into how our thoughts, perceptions, and mindfulness practices can profoundly influence our physical well-being.
She presents compelling evidence that our mental states are intricately linked to our physical health. She discusses how our perceptions of time and control can significantly impact healing rates, hormonal balance, immune function, and overall longevity. By reframing our understanding of mindfulness—not merely as a meditative practice but as an active, moment-to-moment engagement with our environment—we can harness our mental faculties to foster better health outcomes. The episode also highlights practical applications of Dr. Langer’s research, offering insights into how adopting a mindful approach to daily life can lead to remarkable health benefits. By noticing new things and embracing uncertainty, individuals can break free from mindless routines, reduce stress, and enhance their overall quality of life. This podcast is a must-listen for anyone interested in the profound connection between mind and body. It provides valuable tools and perspectives for those seeking to take an active role in their health and well-being through the power of mindful thinking. It will change your perspective and improve your health. Listen to or watch the interview:
Youtube: https://www.youtube.com/watch?v=QYAgf_lfio4

Useful blogs to reduce stress
From Conflict to Calm: Reframing Stress and Finding Peace with Difficult People
Posted: February 6, 2025 Filed under: attention, behavior, Breathing/respiration, CBT, emotions, healing, health, Neck and shoulder discomfort, Pain/discomfort, stress management | Tags: anger, anger management, conflict resolution, Reframing, resentment 8 Comments
Adapted from: Peper, E. (2025, Feb 15). From Conflict to Calm: Reframing Stress and Finding Peace with Difficult People. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/from-conflict-to-calm-reframing-stress-and-finding-peace-with-difficult-people/
After living in our house for a few years, a new neighbor moved in next door. Within months, she accused us of moving things in her yard, blamed us when there was a leak in her house, dumped her leaves from her property onto other neighbors’ properties, and even screamed at her tenants to the extent that the police were called numerous times.
Just looking at her house through the window was enough to make my shoulders tighten and leave me feeling upset. When I drove home and saw her standing in front of her house, I would drive around the block one more time to avoid her while feeling my body contract. Often, when I woke up in the morning, I would already anticipate conflict with my neighbor. I would share stories of my disturbing neighbor and her antics with my friends. They were very supportive and agreed with me that she was crazy.
However, this did not resolve my anger, indignation, or the anxiety that was triggered whenever I saw her or thought of her. I spent far too much time anticipating and thinking about her, which resulted in tension in my own body—my heart rate would increase, and my neck and shoulders would tighten. I decided to change. I knew I could not change her; however, I could change my reactivity and perspective.
Thus, I practiced the “Pause and Recenter” technique described in the blog. At the first moment of awareness that I was thinking about her or her actions, I would change my posture by sitting up straight and looking upward, breathe lower and slower, and then, in my mind’s eye, send a thought of goodwill streaming to her like an ocean wave flowing through and around her in the distance. I choose to do this because I believe that within every person, no matter how crazy or cruel, there is a part that is good, and it is that part I want to support.
I repeated this many times—whenever I looked in the direction of her house or saw her in her yard. I also reframed her aggressive, negative behavior as her way of coping with her own demons. Three months later, I no longer react defensively. When I see her, I can say hello and discuss the weather without triggering my defensive reaction. I feel so much more at peace living where I am.
When stressed, angry, rejected, frustrated, or hurt, we so often blame the other person. The moment we think about that person or event, our anger, indignation, resentment, and frustration are triggered. We keep rehashing what happened. As we do this, we are unaware that we are reliving the past event and are often unaware of the harm we are doing to ourselves until we experience symptoms such as high blood pressure, gastrointestinal distress, insomnia, anxiety, or muscle tightness. As we think of the event or interact again with that person, our body automatically responds with a defense reaction as if we are actually being threatened. This response activates the defense to protect ourselves from harm— the person is not a threat like the saber-toothed tiger ready to attack. Yet we respond as if the person is the tiger.
This defense reaction activates our “fight or flight” responses and increases sympathetic activation so that we can run faster and fight more ferociously to survive; however, it reduces blood flow through the frontal cortex—a process that reduces our ability to think rationally (Willeumier, et al., 2011; van Dinther et al., 2024). When we become so upset and stressed that our mind is captured by the other person, it contributes to an increase in hypertension, myofascial pain, depression, insomnia, cardiovascular disease, and other chronic disorders (Russel et al., 2015; Suls, 2013; Duan et al., 2022).
Our initial response of sharing our frustrations with others is normal. It feels good to blame the other; however, over time, the only person who gets hurt is yourself (Fast & Tiedens, 2010; Lou et al., 2023). The time spent rehashing and justifying our feelings diminishes our time we are in the present moment or focus on upcoming opportunities.
We may not realize that we have a choice. We can keep living and reacting to past hurt or losses, or we can let go and/or forgive and make space for new opportunities. Although the choice is ours, it is often very challenging to implement—even with the best intentions—as we react automatically when reminded of the past hurt (seeing that person, anticipating meeting or actually meeting that person who caused the hurt, or being triggered by other events that evoke memories of the pain).
What can you do
If choose to change your response and reactivity, it does not mean you condone what happened or agree that the other person was right. You are just choosing to live your life and not continue to be captured and react to the previous triggers. Many people report that after implementing some of the practices described below or others stress management techniques frequently their automatic reactivity was significantly reduced. They report that their symptoms are reduced and have the freedom to live in present instead of being captured by the painful past.
Pause and recenter
Our automatic reaction to the trigger elicits a defense reaction that reduces our ability to think rationally. Therefore, the moment you anticipate or begin to react, take three very slow diaphragmatic breaths. As you inhale, allow your abdomen to expand; then, as you exhale slowlymake your yourself tall and look up. Looking up allows easier access to empowering and positive memories (Peper et al., 2017). Continue looking up and inhale slowly allow the abdomen to expand. Repeat this slow breath again.
On the third breath, while looking up, evoke a memory of someone in whose presence you felt at peace and who loves –you such as your grandmother, aunt or uncle or your dog. Reawaken that feeling associated with that memory. Allow a smile with soft eyes to come to your face as you experience the loving memory. Then, put your hands on your chest, take a breath as your abdomen to expands, and as you exhale, bring your hands away from your chest and stretch them out in front of you. At the same time, in your mind’s eye imagine sending good will to that person or conflict that previously evoked your stress response.
As you do this, you are not condoning what happened; instead, you are sending goodwill to that person’s positive aspect. From this perspective, everyone has an intrinsic component—however small—that some label as Christ nature or Buddha nature.
Why could this be effective? This practice short-circuits the automatic stress response and provides time to recenter. It interrupts ongoing rumination by shifting the mind away from thoughts about the person or event that induces stress and toward a positive memory. Evoking a loving memory from the past facilitates a reduction in arousal, evokes a positive mood, and decreases sympathetic nervous system activation (Speer & Delgado, 2017). Additionally, slower diaphragmatic breathing reduces sympathetic activation (Birdee et al., 2023; Siedlecki et al., 2022). By combining body and mind, we can pause and create the opportunity to respond positively rather than reacting with anger and hurt.
Practice sending goodwill the moment you wake up
So often when we wake up, we already anticipate the challenges and even the prospect of interacting with person or event heightens our defense reaction. Therefore, as soon as you wake up, sit at the edge of the bed, repeat the previous practice, Pause and Center. Then, as you sit at the edge of the bed, slightly smile with soft eyes, look up, inhale as your abdomen expand. Then, stamp your right foot into the floor while saying, “Today is a new day.” Next, inhale allowing your abdomen expand; as you look up, stamp your left foot on the floor while saying, “Today is a new day.” Finally, send goodwill to the person who previously triggered your defensive reaction.
Why could this be effective?
Looking up makes it easier to access positive memories and thoughts. Stamping your foot on the ground is a non-verbal expression of determination and anchors the thought of a new day, thereby focuses on new opportunities (Feldman, 2022).
Discuss your issue from the third-person perspective instead of the first-person perspective
When thinking, ruminating, talking, texting, or writing about the event, discuss it from the third-person perspective. Replace the first-person pronoun “I” with “she” or “he.” For example, instead of saying:
I was really pissed off when my boss criticized my work without giving any positive suggestions for improvement,
Say:
He was really pissed off when his boss criticized his work without offering any positive suggestions for improvement.
Why could this be effective? The act of substituting the third person pronoun for the first-person pronoun interrupts our automatic reactivity because it requires us to observe and change our language, which activating the frontal cortex. This process creates a psychological distance from our feelings, allowing for a more objective and calmer perspective on the situation. It effectively reducing stress by stepping back from the immediate emotional response (Moser et al., 2017). It means that you are no longer fully captured by the emotions, as you are simultaneously the observer of your own inner language and speech.
Compare yourself to others who are suffering more
When you feel sorry for yourself or hurt, take a breath, look upward, and compare yourself to others who are suffering much more. In that moment, consider yourself incredibly lucky compared to people enduring extreme poverty, bombings, or severe disfigurement. Be grateful for what you have.
Why could this be effective? The research data shows that if we have low self-esteem when we compare ourselves to people who are more successful (healthier, richer, or successful), we feel worse in comparison and if we compare ourselves to other who are suffering more we feel better (Aspinwall, & Taylor, 1993). The comparision relativize our suffering. Thus our own suffering become less significant compared to the other people’s severe suffering.
Research shows that when we compare ourselves to people who are more successful (healthier, richer, or more accomplished), we tend to feel worse—especially if we have low self-esteem. However, when we compare ourselves to others who are suffering more, we tend to feel better (Aspinwall, & Taylor, 1993). This comparison relativizes our suffering, making our own hardships and suffering seem less significant compared to the severe suffering of others.
Interrupt the stress response
When overwhelmed by a stress reaction, implement the recue techniques described in the article, Quick rescue techniques when stress (Peper, Oded and Harvey, 2024) and the blog to help reduce stress. https://peperperspective.com/2024/02/04/quick-rescue-techniques-when-stressed/
Conclusion
It is much easier to write and talk about these practices than to actually do them. Remembering and reminding yourself to implement them can be very challenging. It requires significant effort and commitment. In most cases, the benefits are not experienced immediately. However, when practiced many times over weeks and months, many people report feeling less resentment, experience a reduction in symptoms, and improvements in health and relationships.
*This blog was inspired by the podcast, No hard feelings, that featured psychologist Fred Luskin. It is an episode on Hidden Brain, produced by Shankar Vedantam (2025) and the wisdom taught by Dora Kunz (Kunz & Peper, 1983; Kunz and Peper, 1984a; Kunz and Peper, 1984b; Kunz and Peper, 1987).
Useful blog that complement the concepts in this blog
References
Aspinwall, L. G., & Taylor, S. E. (1993). Effects of social comparison direction, threat, and self-esteem on affect, self-evaluation, and expected success. Journal of Personality and Social Psychology, 64(5), 708–722. https://doi.org/10.1037/0022-3514.64.5.708
Birdee, G., Nelson, K., Wallston, K., Nian, H., Diedrich, A., Paranjape, S., Abraham, R., & Gamboa, A. (2023). Slow breathing for reducing stress: The effect of extending exhale. Complementary Therapies in Medicine, 73. https://doi.org/10.1016/j.ctim.2023.102937
Duan, S., Lawrence, A., Valmaggia, L., Moll, J. & Zahn, R. (2022). Maladaptive blame-related action tendencies are associated with vulnerability to major depressive disorder. Journal of Psychiatric Research, 145, 70-76. https://doi.org/10.1016/j.jpsychires.2021.11.043
Fast, N.J. & Tiedens, L.Z. (2010). Blame contagion: The automatic transmission of self-serving attributions. Journal of Experimental Social Psychology, 46(1), 97-106. https://doi.org/10.1016/j.jesp.2009.10.007
Feldman, Y. (2022). The Dialogical Dance-A Relational Embodied Approach to Supervision. In Butte, C. & Colbert, T. (Eds). Embodied Approaches to Supervision-The Listening Body. London: Routledge. https://www.amazon.com/Embodied-Approaches-Supervision-C%C3%A9line-Butt%C3%A9/dp/0367473348
Kunz, D. & Peper, E. (1983). Fields and Their Clinical Implications-Part III: Anger and How It Affects Human Interactions. The American Theosophist, 71(6), 199-203. https://www.researchgate.net/publication/280777019_Fields_and_their_clinical_implications-Part_III_Anger_and_how_it_affects_human_interactions
Kunz, D. & Peper, E. (1984a). Fields and Their Clinical Implications IV: Depression from the Energetic Perspective: Etiological Underpinnings. The American Theosophist, 72(8), 268-275. https://biofeedbackhealth.org/wp-content/uploads/2011/01/fields-and-their-clinical-implications-iv-depression-from-the-energetic-perspectivive.pdf
Kunz, D. & Peper, E. (1984b). Fields and Their Clinical Implications V: Depression from the Energetic Perspective: Treatment Strategies. The American Theosophist, 72(9), 299-306. https://biofeedbackhealth.org/wp-content/uploads/2011/01/fields-and-their-clinical-implications-part-v-depression-treatment-strategies.pdf
Kunz, D. & Peper, E. (1987). Resentment: A poisonous undercurrent. The Theosophical Research Journal. IV (3), 54-59. Also in: Cooperative Connection. IX (1), 1-5. https://www.researchgate.net/publication/387030905_Resentment_Continued_from_page_4
Lou, Y., Wang, T., Li, H., Hu, T. Y., & Xie, X. (2023). Blame others but hurt yourself: blaming or sympathetic attitudes toward victims of COVID-19 and how it alters one’s health status. Psychology & Health, 39(13), 1877–1898. https://doi.org/10.1080/08870446.2023.2269400
Moser, J. S., Dougherty, A., Mattson, W. I., Katz, B., Moran, T. P., Guevarra, D., Shablack, H., Ayduk, O., Jonides, J., Berman, M. G., & Kross, E. (2017). Third-person self-talk facilitates emotion regulation without engaging cognitive control: Converging evidence from ERP and fMRI. Scientific reports, 7(1), 4519. https://doi.org/10.1038/s41598-017-04047-3
Oneda, B., Ortega, K., Gusmão, J. et al. (2010). Sympathetic nerve activity is decreased during device-guided slow breathing. Hypertens Res, 33, 708–712. https://doi.org/10.1038/hr.2010.74
Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41. https://doi.org/10.5298/1081-5937-45.2.01
Russell, M. A., Smith, T. W., & Smyth, J. M. (2016). Anger Expression, Momentary Anger, and Symptom Severity in Patients with Chronic Disease. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 50(2), 259–271. https://doi.org/10.1007/s12160-015-9747-7
Siedlecki, P., Ivanova, T.D., Shoemaker, J.K. et al. (2022). The effects of slow breathing on postural muscles during standing perturbations in young adults. Exp Brain Res, 240, 2623–2631. https://doi.org/10.1007/s00221-022-06437-0
Speer, M. & Delgado, M. (2017).Reminiscing about positive memories buffers acute stress responses. Nat Hum Behav 1, 0093 (2017). https://doi.org/10.1038/s41562-017-0093
Suls J. (2013). Anger and the heart: perspectives on cardiac risk, mechanisms and interventions. Progress in cardiovascular diseases, 55(6), 538–547. https://doi.org/10.1016/j.pcad.2013.03.002
van Dinther, M., Hooghiemstra, A. M., Bron, E. E., Versteeg, A., Leeuwis, A. E., Kalay, T., Moonen, J. E., Kuipers, S., Backes, W. H., Jansen, J. F. A., van Osch, M. J. P., Biessels, G. J., Staals, J., van Oostenbrugge, R. J., & Heart-Brain Connection consortium (2024). Lower cerebral blood flow predicts cognitive decline in patients with vascular cognitive impairment. Alzheimer’s & dementia : the journal of the Alzheimer’s Association, 20(1), 136–144. https://doi.org/10.1002/alz.13408
Vedantma, S. (2025). Hidden Brain episode, No hard feelings. Accessed February 5, 2025. https://hiddenbrain.org/podcast/no-hard-feelings/
Willeumier, K., Taylor, D. V., & Amen, D. G. (2011). Decreased cerebral blood flow in the limbic and prefrontal cortex using SPECT imaging in a cohort of completed suicides. Translational psychiatry, 1(8), e28. https://doi.org/10.1038/tp.2011.28
Implement your New Year’s resolution successfully[1]
Posted: December 29, 2024 Filed under: attention, behavior, CBT, cognitive behavior therapy, education, emotions, Exercise/movement, healing, health, self-healing | Tags: goal setting, health, lifestyle, motivation, performance, personal-development Leave a comment
Adapted from: Peper, E. Pragmatic suggestions to implement behavior change. Biofeedback.53(2), 41-45. https://doi.org/10.5298/1081-5937-53.02.05
Ready to crush your New Year’s resolutions and actually stick to them this time? Whether you’re determined to quit vaping or smoking, cut back on sugar and processed foods, reduce screen time, get moving, volunteer more, or land that dream job, sticking to your goals is the real challenge. We’ve all been there: kicking off the year with ambitious plans like, “I’ll work out every day,” or “I’m done with junk food for good.” But a few weeks in? The gym is a distant memory, the junk food stash is back, and those cigarettes are harder to let go of than expected.
So, how can you make this year different? Here are some tried-and-true tips to help you turn those resolutions into lasting habits:
Be clear of your goal and state exactly what you want to do (Pilcher et al., 2022; Latham & Locke, 2006).
Did you know your brain is super literal and doesn’t process “not” the way you think it does? For example, if you say, “I will not smoke,” your brain has to first imagine you smoking, then mentally cross it out. Guess what? By rehearsing the act of smoking in your mind, you’re actually increasing the chances that you’ll light up again.
Think of it like this: hand a four-year-old a cup of hot chocolate and ask them to walk it over to someone across the room. Halfway there, you call out, “Be careful, don’t spill it!” What usually happens? Yep, the hot chocolate spills. That’s because the brain focuses on “spill,” not the “don’t.” Now, imagine instead you say, “You’re doing great! Keep walking steadily.” Positive framing reinforces the action you want to see. The lesson is to reframe your goals in a way that focuses on what you want to achieve, not what you’re trying to avoid. Let’s look at some examples to get you started:
| Negative framing | Positive framing |
| I plan to stop smoking | I choose to become a nonsmoker |
| I will eat less sugar and ultra-processed foods | I will shop at the farmer’s market, buy more fresh vegetable and prepare my own food. |
| I will reduce my negative thinking (e.g., the glass is half empty). | I will describe events and thoughts positively (e.g., the class is half full). |
Describe what you want to do positively.
Be precise and concrete.
The more specific you can describe what you plan to do, the more likely will it occur as illustrated in the following examples.
| Imprecise | Concrete and specific |
| I will begin exercising. | I will buy the gym membership next week Monday and will go to the gym on Monday, Wednesday and Friday right after work at 5:30pm for 45 minutes. |
| I will reduce my angry outbursts, | Before I respond, I will take a slow breath, look up, relax my shoulders and remind myself that the other person is doing their best. |
| I want to limit watching streaming videos | At home, I will move the couch so that it does not face the large TV screen, and I have enrolled in a class to learn another language and I will spent 30 minutes in the evening practicing the new language. |
| I will stop smoking | When I feel the initial urge to smoke, I stand up, do a few stretches, and practice box breathing and remind myself that I am a nonsmoker. |
Describe in detail what you will do.
Identify the benefits of the old behavior that you want to change and how you can achieve the same benefits with your new behavior. (Peper et al, 2002)
When setting a New Year’s resolution, it’s easy to focus on the perks of the new behavior and the harms of the old behavior while overlooking the benefits your old habit provided. However, if you don’t plan ways to achieve the same benefits, the old behavior provided, it’s much harder to stick to your goal.
Before diving into your new resolution, take a moment to reflect. What did your old behavior do for you? What needs did it meet? Once you identify those, you can develop strategies to achieve the same benefits in healthier, more constructive ways.
For example, let’s say your goal is to stop smoking. Smoking might have helped you relax during stressful moments or provided a social activity with friends. To make the switch, you’ll need to find alternatives that deliver similar results, like practicing deep-breathing exercises to manage stress or inviting friends for a walk instead of a smoke break. By creating a plan to meet those needs, you’ll set yourself up for lasting success.
| Benefits of smoking | How to achieve the same benefits when being a none smoker |
| Stress reduction | I will learn relaxation and diaphragmatic breathing. The moment, I feel the urge to smoke, I sit up, look up, raise my shoulder and dropped them, and breathe slowly |
| Breaks during work | I will install a reminder on my cellphone to ping and each time it pings, I stop, stand up, walk around and stretch. |
| Meeting with friends | I will tell my friends, not to offer me a cigarette and I will spent time with friends who are non-smokers. |
| Rebelling against my parents who were opposed to smoking | I will explore how to be independent without smoking |
Describe your benefits and how you will achieve them.
Reduce the cues that evoke the old behavior and create new cues that will trigger the new behavior (Peper & Wilson, 2021).
A lot of our behavior is automatic—shaped by classical conditioning, just like Pavlov’s dog. Remember the famous experiment? Pavlov paired the sound of a bell with food, and after a while, the bell alone made the dog salivate (McLeod, 2024). We’re not so different.
Think about it: if you’ve gotten into the habit of smoking in your car, simply sitting in the driver’s seat can trigger the automatic urge to grab a cigarette. Or, if you tend to feel depressed when you’re home but better when you’re out with friends, your home environment might be acting as a cue for those feelings.
Interestingly, many people find it easier to change habits in a new environment. Why? Because there are no built-in triggers to reinforce the behavior they’re trying to change. This highlights how much of what we often call “addiction” might actually be conditioned behavior, reinforced by familiar cues in our surroundings. By recognizing the power of these triggers can help you disrupt old patterns. By creating a fresh environment or consciously changing your responses to cues, you can take control and start forming new, healthier habits.
This concept has been understood for centuries by some hunting and gathering societies. When something tragic happened—like the death of a family member in a hut—the community would often burn the hut to “eliminate the evil spirit.” Beyond the spiritual aspect, this practice served a practical purpose: it removed all the physical cues that reminded people of their loss, making it easier to focus on the present and move forward.
Of course, I’m not suggesting you destroy your home. But the underlying principle still holds true in modern times. In fact, many Northern European cultures incorporate a version of this idea through the ritual of Spring Cleaning. By decluttering, rearranging furniture, and refreshing the home, the old cues are removed and create a sense of renewal.
So often we forget that cues in our environment play a powerful role in triggering our behavior. By identifying the triggers that evoke old habits and finding ways to remove or change them, you can create a fresh environment that supports your goals. For example, if you’re trying to stop snacking on junk food late at night, consider rearranging your pantry so the tempting items are out of sight—or better yet, replace them with healthier options. Small changes like this can have a big impact on your ability to stay on track.
| Cues that triggered the behavior | How cues were changed |
| In the evening going to the kitchen and getting the chocolate from the cupboard. | Buying fruits and have them on the table and not buying chocolate. If I do buy chocolate store it on the top shelf away so that I do not see it or store it in the freezer. |
| Getting home and being depressed. | Clean the house, change the furniture around and put positive picture high up on the wall. |
| Smoking in the car. | Replace the car with another car that no one had smoked in and spray the care with pine scent. |
Identify the cues that trigger your behavior and how you changed them.
Identify the first sensation that triggered the behavior you would like to change.
Whether it’s smoking, drinking, scratching your skin, spiraling into negative thoughts, or eating too many pastries, once a behavior starts, it can feel nearly impossible to stop. That’s why the key is to catch yourself before the habit takes over., t’s much easier to interrupt a pattern at the very first sign—the initial trigger—rather than after you’ve fully dived into the behavior. Yet how often do we find ourselves saying, “Next time, I’ll do it differently”?
Here’s the strategy: identify the first trigger. This could be a physical sensation, an emotion, a thought, or an external cue. Once you’re aware of that first flicker of a trigger, redirect your thoughts and actions toward what you actually want, rather than letting the automatic behavior take control. For example:
I just came home at 10:15 PM and felt lonely and slightly depressed. I walked into the kitchen, opened the fridge, grabbed a beer, and drank it. Then, I reached for another bottle.
Observing this behavior, the first trigger was the loneliness and slight depression upon arriving home. Recognizing that feeling in the moment offers an opportunity to pause and make a conscious choice. Instead of heading to the fridge, you could redirect your actions—call a friend, go for a quick walk, or write down your thoughts in a journal. By catching that initial trigger, you can focus yourself toward healthier behaviors and break the cycle.
| First sensation | Changed response to the sensation |
| I observed that the first sensation was feeling tired and lonely. | When I entered the house, instead of going to the kitchen, I stretched, looked up and took a deep breath and then called a close friend of mine. We talked for ten minutes and then I went to bed. |
Identify your first sensation and how you changed your behavior.
Incorporate social support and social accountability (Drageset, 2021).
Doing something on your own often requires a lot of willpower, and sticking to it every time can feel like an uphill battle. Take this example:
My goal is to exercise every other morning. But last night, I stayed up late and felt tired in the morning, so I skipped my workout.
Sound familiar? Now imagine if I’d planned to meet a workout buddy. Knowing someone was counting on me would’ve gotten me out of bed, even if I was tired, because I wouldn’t want to let them down.
Accountability can make all the difference. Another powerful strategy is sharing your goals publicly. When you announce your plans on social media or to friends and family, you create a sense of commitment—not just to yourself but to others. It’s like having a built-in support system cheering you on and holding you accountable. Whether it’s finding a partner, joining a group, or sharing your progress online, involving others can help turn your resolutions into habits you’re more likely to stick with.
Describe a strategy to increase social support and accountability.
Be honest in identifying what motivates you.
Exercising, eating healthy foods, thinking positively, or being on time are laudable goals; however, it often feels like work doing the “right” thing. To increase success, analyze what really helped you be successful. For example:
Many years ago, I decided that I should exercise more. Thus, I drove from house to the track and ran eight laps. I did this for the next three weeks and then stopped exercising. Eventually, I pushed myself again to exercise and after a while stopped again. The same pattern kept repeating. I would exercise and fall off the wagon and stop. Later that fall, I met a woman who was a jogger and we became friends and for the next year we jogged together and even did races. During this time, I did not experience any effort to go jogging. After a year, she broke up with me and once again, I had to use willpower to go jogging and my old pattern emerged and after a few days I stopped jogging even though I felt much better after having jogged.
I finally, asked what is going on? I realized that the joy of the jogging was running with a friend. Once, I recognized this, instead using will power to go running, I spent my willpower finding people with whom I could exercise. With these new friends, running did not depend upon my willpower– It only depended on making running dates with my new friends.
Explore factors that will allow you to do your activity without having to use willpower.
Conclusion
These seven strategies are just a starting point—there are countless other techniques that can help you stick to your New Year’s resolutions. For example, keeping a log, setting reminders, or rewarding yourself for progress are all powerful ways to stay on track. The real magic happens when your new behavior becomes part of your routine—embedded in your habitual patterns. The more automatic it feels, the greater your chances of long-term success.
So, take joy in identifying, implementing, and maintaining your resolutions. Let them enhance your well-being and become second nature. Share your successful strategies with me and others—it could be just the inspiration someone else needs to achieve their goals, too.
References
Drageset, J. (2021). Social Support. In: Haugan G, Eriksson M, editors. Health Promotion in Health Care – Vital Theories and Research [Internet]. Cham (CH): Springer, Chapter 11. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585650/ https://doi.org/10.1007/978-3-030-63135-2_11
Latham, G. P., & Locke, E. A. (2006). Enhancing the Benefits and Overcoming the Pitfalls of Goal Setting. Organizational Dynamics, 35(4), 332–340. https://doi.org/10.1016/j.orgdyn.2006.08.008
McLeod, S. (2024). Classical Conditioning: How It Works With Examples.Simple Psychology. Accessed December 29, 2024. https://www.simplypsychology.org/classical-conditioning.html
Peper, E., Gibney, H. K. & Holt, C. (2002). Make Health Happen. Dubuque, Iowa: Kendall-Hunt. (Pp 185-192). https://he.kendallhunt.com/make-health-happen
Peper, E. & Wilson, V. (2021). Optimize the learning state: techniques and habits. Biofeedback, 9(2), 46-49. https://doi.org/10.5298/1081-5937-49-2-04
Pilcher, S., Schweickle, M. J., Lawrence, A., Goddard, S. G., Williamson, O., Vella, S. A., & Swann, C. (2022). The effects of open, do-your-best, and specific goals on commitment and cognitive performance. Sport, Exercise, and Performance Psychology, 11(3), 382–395. https://doi.org/10.1037/spy0000301
For detailed suggestions, see the following blogs:
[1] Edited with the help of ChatGPT.
Suggestions for mastering and generalizing breathing skills
Posted: October 30, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cellphone, cognitive behavior therapy, emotions, ergonomics, healing, health, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: abdominal beathing, anxiety, diaphragmatic braething, health, hyperventilation, meditation, mental-health, mindfulness, mouth breathing, Toning 3 CommentsAdapted from: Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/

Breathing techniques are commonly employed with complimentary treatments, biofeedback, neurofeedback or adjunctive therapeutic strategies to reduce stress and symptoms associated with excessive sympathetic arousal such as anxiety, high blood pressure, insomnia, or gastrointestinal discomfort. Even though it seems so simple, some participants experience difficulty in mastering effortless breathing and/or transferring slow breathing skills into daily life. The purpose of this article is to describe: 1) factors that may interfere with learning slow diaphragmatic breathing (also called cadence or paced breathing, HRV or resonant frequency breathing along with other names), 2) challenges that may occur when learning diaphragmatic breathing, and 3) strategies to generalize the effortless breathing into daily life.
Background
A simple two-item to-do list could be: ‘Breathe in, breathe out.’ Simple things are not always easy to master. Mastering and implementing effortless ‘diaphragmatic’ or ‘abdominal belly’ breathing may be simple, yet not easy. Breathing is a dynamic process that involves the diaphragm, abdominal, pelvic floor and intercostal muscles that can include synchronizing the functions of the heart and lungs and may result in cardio-respiratory synchrony or coupling, as well as ‘heart-rate variability breathing training (Codrons et al., 2014; Dick et al., 2014; Elstad et al., 2018; Maric et al., 2020; Matic et al., 2020). Improving heart-rate variability is a useful approach to reduce symptoms of stress and promotes health and reduce anxiety, asthma, blood pressure, insomnia, gastrointestinal discomfort and many other symptoms associated with excessive sympathetic activity (Lehrer & Gevirtz, 2014; Xiao et al., 2017; Jerath et al., 2019; Chung et al., 2021; Magnon et al., 2021; Peper et al., 2022).
Breathing can be effortful and In some cases people have dysfunctional breathing patterns such as breath holding, rapid breathing (hyperventilation), shallow breathing and lack of abdominal movement. This usually occurs without awareness and may contribute to illness onset and maintenance. When participants learn and implement effortless breathing, symptoms often are reduced. For example, when college students are asked to practice effortless diaphragmatic breathing twenty-minutes a day for one week, as well as transform during the day dysfunction breathing patterns into diaphragmatic breathing, they report a reduction in shallow breathing, breath holding,, and a decrease of symptoms as shown in Fig 1 (Peper et al, 2022).

Figure 1. Percent of people who reported that their initial symptoms improved after practicing slow diaphragmatic breathing for twenty minutes per day over the course of a week (reproduced from: Peper et al, 2022).
Most students became aware of their dysfunctional breathing and substituted slow, diaphragmatic breathing whenever they realized they were under stress; however, some students had difficulty mastering ‘effortless’ (e.g., automated, non-volitional) slow, diaphragmatic breathing that allowed abdominal expansion during inhalation.
Among those had more difficulty, they tended to have almost no abdominal movement (expansion during inhalation and abdominal constriction during exhalation). They tended to breathe shallowly as well as quickly in their chest using the accessory muscles of breathing (sternocleidomastoid, pectoralis major and minor, serratus anterior, latissimus dorsi, and serratus posterior superior).
The lack of abdominal movement during breathing reduced the movement of lymph as well as venous blood return in the abdomen; since; the movement of the diaphragm (the expansion and constriction of the abdomen) acts a pump. Breathing predominantly in the chest may increase the risk of anxiety, neck, back and shoulder pain as well as increase abdominal discomfort, acid reflux, irritable bowel, dysmenorrhea and pelvic floor pain (Banushi et al., 2023; Salah et al., 2023; Peper & Cohen, 2017; Peper et al., 2017; Peper et al., 2020, Peper et al., 2023). Learning slow, diaphragmatic or effortless breathing at about six breaths per minute (resonant frequency ) is also an ‘active ingredient’ in heartrate variability (HRV) training (Steffen et al., 2017; Shaffer & Meehan, 2020).
1. Factors that interfere with slow, diaphragmatic breathing
Difficulty allowing the skeletal and visceral muscles in the abdomen to expand or constrict in ‘three-dimensions’ (e.g., all around you in 360 degrees) during inhalation or exhalation. Whereas internal factors under volitional control and will mediate breathing practices, external factors can restrict and moderate the movement of the muscles. For example:
Clothing restrictions (designer jeans syndrome). The clothing is too tight around the abdomen; thereby, the abdomen cannot expand (MacHose & Peper, 1991; Peper et al., 2016). An extreme example were the corsets worn in the late 19th century that was correlated with numerous illnesses.
Suggested solutions and recommendations: Explain the physiology of breathing and how breathing occurs by the diaphragmatic movement. Discuss how babies and dogs breathe when they are relaxed; namely, the predominant movement is in the abdomen while the chest is relaxed. This would also be true when a person is sitting or standing tall. Discuss what happens when the person is eating and feels full and how they feel better when they loosen their waist constriction. When their belt is loosened or the waist button of their pants is undone, they usually feel better.
Experiential practice. If the person is wearing a belt, have the person purposely tighten their belt so that the circumference of the stomach is made much smaller. If the person is not wearing a belt, have them circle their waist with their hands and compress it so that the abdomen can not expand. Have them compare breathing with the constricted waist versus when the belt is loosened and then describe what they experienced.
Most participants will feel it is easier to breathe and much more comfortable when the abdomen is not constricted.
Previous abdominal injury. When a person has had abdominal surgery (e.g., Cesarean section, appendectomy, hernia repair, or episiotomy), they unknowingly may have learned to avoid pain by not moving (relaxing or tensing) the abdomen muscles (Peper et al., 2015; Peper et al., 2016). Each time the abdomen expands or constricts, it would have pulled on the injured area or stitches that would have cause pain. The body immediately learns to limit movement in the affected area to avoid pain. The reduction in abdominal movement becomes the new normal ‘feeling’ of abdominal muscle inactivity and is integrated in all daily activities. This is a process known as ‘learned disuse’ (Taub et al., 2006). In some cases, learned disuse may be combined with fear that abdominal movement may cause harm or injury such as after having a kidney transplant. The reduction in abdominal movement induces shallow thoracic breathing which could increase the risk of anxiety and would reduce abdominal venous and lymph circulation that my interfere with the healing.
Suggested solutions and recommendations. Discuss the concept of learned disuse and have participant practice abdominal movement and lower and slower breathing.
Experiential practices: Practicing abdominal movements
Sit straight up and purposely exhale while pulling the abdomen in and upward and inhale while expanding the abdomen. Even with these instructions, some people may continue to breathe in their chest. To limit chest movement, have the person interlock their hands and bring them up to the ceiling while going back as far as possible. This would lock the shoulders and allows the abdomen to elongate and thereby increase the diaphragmatic movement by allowing the abdomen to expand. If people initially have held their abdomen chronically tight then the initial expansion of abdomen by relaxing those muscle occurs with staccato movement. When the person becomes more skilled relaxing the abdominal muscles during inhalation the movement becomes smoother.
Make a “psssssst” sound while exhaling. Sit tall and erect and slightly pull in and up the abdominal wall and feel the anus tightening (pulling the pelvic floor up) while making the sound. Then allow inhalation to occur by relaxing the stomach and feeling the anus go down.
Use your hands as feedback. Sit up straight, placing one hand on the chest and another on the abdomen. While breathing feel the expansion of the abdomen and the contraction of the abdomen during exhalation. Use a mirror to monitor the chest-muscle movement to ensure there is limited rising and falling in this area.
Observe the effect of collapsed sitting. When sitting with the lower back curled, there is limited movement in the lower abdomen (between the pubic region and the umbilicus/belly button) and the breathing movement is shallower without any lower pelvic involvement (Kang et al., 2016). This is a common position of people who are working at their computer or looking at their cellphone.
Experiential practice: looking at your cellphone
Sit in a collapsed position and look down at your cellphone. Look at the screen and text as quickly as possible.
Compare this to sitting up and then lift the cell phone at eye level while looking straight ahead at the cellphone. Look at the screen and text as quickly as possible.
Observe how the position effected your breathing and peripheral awareness. Most likely, your experience is similar those reported by students. Close to 85%% of students who complete this activity reported that their breathing was shallower sitting slouched versus erect and about 85% of the students reported that their peripheral awareness and vision improved when sitting erect (Peper et al., 2024).
Suggested solutions and recommendations. Be aware how posture affect breathing. While sitting, place a rolled-up towel against the lower back so that the person sits more erect which would allow the abdomen to expand when inhaling.
Self-image, self-esteem, and confidence. Participants may hold their abdomen in because they want to look slim (sometimes labeled as the “hourglass syndrome” associate expanding the abdomen as unattractive (PTI, 2023). A flat abdomen is culturally reinforced by social media and fashion models and encouraged in some activities such as ballet. On the other hand, some people purposely puff up their chest to increase size and dominance (Cohen & Leung, 2009).
Suggested solutions and recommendations. Discuss the benefits of diaphragmatic breathing including its ability to reduce anxiety in social settings that may enhance confidence. Similar to an earlier suggestion, have the person explore clothing with a looser waist that still supports feelings of attractiveness and power.
Feeling anxious, fearful or threatened. The normal physiological stress reaction is a slight gasp with the tightening of the abdomen muscles for protection when a stressor occurs (Gilbert, 1998; Ekerholt & Bergland., 2008). The stressor can be an actual physical event, social situation or thoughts and emotions. Shallow breathing is a natural self-protective response. This pattern is often maintained until one feels ‘safe’ enough to relax, which for many can have a duration of the entire day or until finding the relative safety of sleep.
Suggested solutions and recommendations. Discuss how the physiological stress reaction is a normal response pattern that the person most likely learned in early childhood for self-protection. This pattern is often observed in clients who are emotionally sensitive and/or react excessively to a variety of stimuli. Note that some people have learned not to show their reactivity on their face or in the overt behaviors, yet they continue to breathe shallowly as a telltale sign of ‘distress.’ People who breath shallowly may experience this response as burdensome. Discuss with them how to reframe their sensitivity as a gift; namely, they are more aware of other people’s reactions and emotions. They just need to learn how not to respond automatically. Encourage awareness of their breath-holding and shallow breathing. Follow this by teaching them to replace the dysfunctional breathing with slow, diaphragmatic breathing at 6-breaths-per-minute. A possible training sequence is the following:
- Teach slow, diaphragmatic breathing
- Practice evoking a stressor and the moment the client senses the stress response, shallow breaths or holds their breath have them shift to slow, diaphragmatic breathing.
- If the person slouches in response to stress, the moment they become aware of slouching, have then sit erect, look up and then breathe diaphragmatically. (Peper et al., 2019)
Experiential practice: Transform stressful thoughts by looking up, breathing, and changing thoughts.
Evoke a stressor and then attempt to reframe the experience (cognitive behavior therapy or CBT approach).
Compare this to evoking a stressor, then shift to an upright position while looking up, take a few slow, diaphragmatic breaths, and reframe the experience.
In almost all cases, when the client shifts position, looks up and then reframes, the stress reaction is significantly reduced and it is much easier to reframe the experiences positively compared to when only attempting to reframe the experience (Peper et al., 2019).
Diaphragmatic breathing feels abnormal. How you breathe habitually is what feels normal unless there is overt illness such as asthma or emphysema. Any new pattern usually feels abnormal. When the person shifts their breathing pattern, such as in a transition from habitual shallow chest breathing to slower diaphragmatic abdominal breathing, it feels strange and wrong.
Suggested solutions and recommendations. Discuss the concept that habitual patterns are normal (e.g., a person who typically slouches when standing straight may experience that they are going to fall backwards). Emphasize the importance of making a shift in posture and leaning into the discomfort of the new experience. Often after practicing slow diaphragmatic breathing, the person may report feeling much more relaxed (e.g., sensing heaviness and warmth) with their fingers increasing in temperature.
2. Challenges that may occur when learning diaphragmatic breathing
Ideally, breathing is an effortless diaphragmatic process as described by the phrase, “it breathes me” (Luthe & Schultz, 1970; Luthe, 1979); however, some participants struggle to achieve this type of breathing. The following are common challenges and possible solutions:
Distraction and internal dialogue. Many people struggle with thoughts jumping from one area to another. Some people refer to this mental state as “monkey mind.”
Suggested solutions and recommendations. Validate that distraction and internal dialogue are normal and require continual managing and practice to overcome. Experimental Practice: Have the person train focus during diaphragmatic breathing techniques by focusing on 1 item in the room. Remind them that when thoughts arise, note them briefly instead of engaging with them and then refocus on the item. Start with increments of time and increase with practice.
Effect of gravity on breathing. In the vertical position, exhalation occurs when the abdomen constricts (slight tightening of the transverse and oblique abdominal muscles and the pelvic floor) pushes the diaphragm up, allowing the air to go out. It needs to push against gravity.
In the vertical position, inhalation occurs when the abdominal muscles and pelvic floor muscles relax and the abdomen widens in all directions (360 degrees) which causes the diaphragm to descend as it is being pulled down by gravity. This process allows effortless inhalation. The experience is the opposite when lying supine on one’s back. While lying down, gravity pulls on the abdomen that cause the diaphragm to go upward allowing the air to flow out during exhalation. Inhalation takes work because as the diaphragm descends it has to push the abdominal content upward against gravity.
Experiential practice: Erect versus supine
- Vertical position. Begin by exhaling completely by pulling the abdomen in and up while staying erect and not pressing/contracting the chest downward. At the end of exhalation, allow the abdomen to relax (pop out) and feel how the air is sucked in without trying to inhale
- Horizontal position. Begin by lying down, with the face pointing up. Inhale by expanding your abdomen and pushing your abdomen upward against gravity. Then let exhalation occur while totally relaxing as gravity pushes the abdomen downward, which pushes the diaphragm upward into the chest allowing the air to flow out. Optionally, place a small bag of rice/beans (e.g., approximately one to five pound or. One-half to two kilograms) on your lower abdomen while lying down. When you inhale, push the weight upward and away from you by allowing the stomach, but not the chest, to expand. Allow exhalation to occur as the weight pushes your abdomen down and upward into your chest. The weight is useful as it allows the mind to focus more easily on the task of feeling the movement of the abdomen.
Over breathing/hyperventilation. Even breathing at about six breaths per minute can cause hyperventilation can occur. Hyperventilation occurs when a person is breathing in excess of the metabolic needs of the body and thereby eliminating more carbon dioxide. The result is respiratory alkalosis and an elevated blood pH as the dissolved carbon dioxide (pCO2) in the blood is reduced (Folgering, 1999).
The most common symptoms of over breathing are colder sweaty hands and light-headedness. If this starts to occur, focus on decreasing the airflow during exhalation by exhaling through pursed lips making the sound, “Pssssssst.” While making this sound, make the sound softer with less airflow. Alternatively, have them imagine a holding a dandelion flower a few inches from their lips and blow so softly the seeds do not blow away. The blowing away of the seed is the feedback that you are blowing to hard as shown in Figure 2.

Figure 2. Dandelion seeds as feedback when the person is blowing with too much effort. Alternatively, we recommend that the client imagine smelling the scent/fragrance of a flower that usually causes nose inhalation and then exhale gently through pursed lips ast if the air flows over a candle and, the flame does not move back and forth.
Mouth breathing. Mouth breathing contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded miss-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. Nose breathing reduces airway irritation since the nose filters, humidifies, warms/cools the inhaled air as well as reduces the air turbulence in the upper airways. The epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation (McKeown, 2019; Allen, 2024). Note that alternate nostril breathing, such as breathing in one nostril for 5-seconds and out of the other for 5-seconds is another technique which some people find beneficial.
Slower breathing approaches also facilitates sympathetic parasympathetic balance and reduces airway irritation. If the person breathes habitually through their mouth, refer them to health care provider to explore factors that may contribute to mouth breathing such as enlarged tonsils and adenoids or deviated septum. In addition, explore environmental factors that could contribute nasal inflammation such as allergies or foods such as dairy (Al-Raby, 2016).
Performance anxiety. Many participants are concerned about their performance. The direct instructions such as “follow the graphic” causes the person to try hard to breathe with too much effort. Explore some of the following indirect strategies to interrupt ongoing cognitive judgements and self-talk.
- Toning or humming (Peper et al., 2019a). While exhaling, have the person hum a sound with their mouth closed. Let the sound go for about 6 seconds, relax, inhale and hum again. Toning is very similar except you verbalize a tone such as “Oammm.” (For detailed instructions on toning, see: Anziani & Peper (2021)).
- Stroking down arms and legs during exhalation. Have a partner gently stroke down your arms from your shoulder past your fingertips as you are exhaling. The downward stroking is in rhythm with the exhalation. As the arm is being stroked, attend to the sensations going down the arms. Be sure that the toucher exhales at the same time and the stroking down the arm takes about six seconds. After being stroked for a few times, have the person imagine that each time they exhale they feel a flow down through their arms and out their fingers.
- Repeat the same process while stroking down the legs from the side of their hips to their toes.
- Finally, have the person imagine/feel the sensation streaming down their legs with each exhalation.
- Many participants will report that they sense a steaming going down their arms, that they hands warm up, and their thought have stopped.
- Integrated body movement with breathing especially flexion and contraction (Meehan & Shaffer, 2023). Integrate the normal response of flexion that induces exhalation and extension evokes inhalation. Be careful that the flexion movement does not encourage participants to compress their chest during exhalation, which tends to encourage chest breathing. Have the person focus on their head staying tall and erect. Have the person sit straight up with their feet slight apart and their hands palm down on their lap. Allow inhaling to initiate as the person simultaneously arches their lower back expanding the stomach, separating the knees and turning the hands palm up. Initiate exhalation while simultaneously bringing the knees together, turning the palms face down on the thighs and rolling the pelvic back slightly rounding the lower back. Do the movements smoothly while keeping the legs and shoulders relaxed.
Flooded by emotions. Although very rare, at times when the person allows the abdomen to relax, they may experience by the emotions from a past trauma as the habitual bracing patterns are relaxed.
Suggested solutions and recommendations. Validate these emotions for the person. Explain that this is a normal process that may occur if past trauma has occurred. Clients who have had past trauma often experience hypervigilance, which may interfere with the relaxation response that occurs during more optimal states of breathing. Transitioning to a more optimal rest state may be uncomfortable for a person who has experienced trauma because it reduces hypervigilance. This can feel uncomfortable as hypervigilance in these cases serves a protective role, even if it is an illusory feeling of protection from future harm. Since persistent hypervigilance can interfere with the relaxation response, the benefits of allowing a relaxation response to occur through slower breathing should be highlighted. Grounding techniques as described by Peper et al (2024a) can be useful to become centered.
3. Strategies to generalize the effortless breathing into daily life.
Generalizing the skill occurs after having mastered diaphragmatic breathing in different positions (sitting, standing, lying down, and while performing tasks). It is important to remember that our breathing patterns are conditioned with our behavior. Become aware how breathing affects cognitions and emotions and how emotions and cognitions affects breathing. The following are some strategies that may facilitate learning and generalizing the slower breathing skills.
Observing how our behavior affects our breathing: Anything that may evoke the alarm or defense reaction tends to cause the person gasp and/or hold their breath. For example, when a person is sitting peacefully, make an unexpected noise behind their back or movement in their periphery of vision. In most cases they will gasp or hold their breath. Usually, they are unaware of this process unless they are asked what happened to their breathing. The major reason for the breath holding is that the stimuli triggers an alarm/defense reaction and when we hold our breath our hearing is more acute (we can hear approaching danger earlier). The problem is that we give this response when there is no actual, immediate or present threat.
Experiential practice. Sit comfortably. Now as quickly as possible without rotating the head, look with your eyes to the extreme right and then left and back and forth as if trying to identify danger at the periphery. Do this for a few eye movements. Almost everyone holds their breath when doing this exercise. For generalizing the skill, ask the person to observe during the day situations in which they hold their breath, ask them if it was necessary and encourage them to start diaphragmatic breathing.
Observing how breathing affects our thoughts and emotions. Breathing patterns are intrinsically linked to our emotions and thoughts as illustrated in the many language phrases such as sigh of relief, full of hot air, waiting with bated breath. At the same time, our breathing patterns also affect our thoughts. For instance, when we breathe shallowly and more rapidly, we can induce feelings of fear or anxiety. If we gasp, we can experience thought stopping.
Experiential practices: Incomplete exhalation: Observe what happens when you exhale less than you inhale. Begin by exhaling only 70% of the air you inhaled, then inhale and exhale again only 70% of the air you just inhaled continue this for 30 seconds. Many people will experience the onset of anxiety symptoms, lightheadedness, dizziness, neck and shoulder tension, etc. (Peper & MacHose, 1993). If you experience symptoms during this exercise and you have experienced these symptoms in the past, it is likely that unknowingly breathing in a dysfunctional pattern could have evoked them. Therefore, practicing effortless breathing may interrupt and reduce the symptoms. Do this practice while observing the person carefully and immediately interrupt and distract the person if they start feeling dizzy, too anxious, or trigger the beginning of a panic attack or PTSD symptoms.
Experiential practice: Gasp or sniff-hold sniff. Observe what happens when you are performing a cognitive task and you rapidly gasp or do sniff-hold-sniff again before exhaling. Begin by sequentially subtracting mentally, the number 7 from 146 (e.g., 146, 139, 132….). Do this as rapidly as possible and do not make a mistake. While doing the subtracting, take a rapid gasp (such as one is triggered by surprise or fear), alternatively, take a quick sniff through your nose, hold your breath and take another sniff on top of the first one, then exhale. Whereas subtrating numbers is a skill most adults can perform, the ‘time pressure’ along with the direction to avoid mistakes may be the ‘immediate’ source of strain. Whether it was the time pressure, the direction to avoid mistakes or the direction to gasp, observe what happened to your thinking process. In almost all cases, your higher-order thoughts (doing the sequential subtraction under time pressure while gasping) have disappeared, replaced by the immediate thoughts of ‘performance anxiety.’
If you blank out on exams or experience anxiety, gasping and breath holding may be one of the factors that increases symptoms and affects your performance. If you are aware that you are holding your breath or gasped, use that as the cue to shift to slow diaphragmatic breathing and you may find that your performance improves. Therefore, observe when and where you were blanking out, gasping and/or holding your breathing then substitute slow, effortless diaphragmatic breathing.
How to develop awareness and interrupting of dysfunctional breathing response. Most participants are unaware of their somatic responses until symptoms occur. Being aware of the initiation of a somatic response may assist you in identifying triggers and interrupting the developing process. A significant component of the training is symptom prescription rehearsal.
Symptom prescription is a practice in which the participant simulates/acts out the psychophysiological pattern associated with their symptoms. They amplify the body pattern until they feel the onset of the actual symptoms. The moment the person feels the beginning of the symptom, they stop the practice and initiate slow breathing and relaxation. After practicing the symptom rehearsal, they are instructed to become aware of the onset of the symptom and then use that signal to trigger the effortless breathing while looking up and shifting the body into an upright sitting position (Peper et al., 2019). Gasping and breath holding are normal responses to unexpected stimuli; however, they may trigger sympathetic activation even when there is no actual danger.
Experiential practice: Developing awareness on neck and shoulder tension:
Sit comfortably and practice effortless breathing for a minute. Take a fearful gasp and observe what happens in your body (e.g., slight neck and upper chest tension, light headedness, slight radiating pain into the eye, etc.). Shift back to effortless breathing until all symptoms /sensations have disappeared.
- Now gasp with less effort and observe the first sensations, use the awareness of first sensations to trigger the effortless breathing and continue to breathe until symptoms have disappeared
- Continue this practice. Reduce the gasping effort each time.
- After having developed the initial somatic sensation then during the day observe what triggers this response and immediately shift to slower diaphragmatic breathing. After you have shifted to effortless breathing, reflect on the trigger. Was it necessary to react? If yes, explore strategies to resolve the issue.
The same process can be done to assist with desensitization to painful memories or stressful events. Each time the person becomes aware of their somatic reaction to an evoked memory or stressful event, they shift to effortless diaphragmatic breathing. If they find that it is difficult to interrupt the emotional memories and it triggers more and more negative thoughts and associations, use the sniff-hold-sniff technique and follow that with box-breathing or any of the other quick somatic rescue techniques (Peper et al., 2024a). Box-breathing in this context could include a brief breath-holding. A typical box-breathing technique is to breath in for a count of four, hold for a count of four, breath out for a count of four, then breath in again for a count of four, continuing the figurative 4-4-4-4 count of breathing.
Practice slower diaphragmatic breathing during the day. Implement effortless diaphragmatic breathing through regeneration and interrupting the stress response.
- Support regeneration. Each day set aside 10 to 20 minutes to practice slow effortless diaphragmatic breathing at about 6-breaths-per-minute. In the beginning 10 to 20 minutes may be too long, thus in some cases have the person practice a few times a day for two minutes and slowly build up to 10 or more minutes. The practice is not just a mechanical process of breathing it includes mindfulness training. Namely, as you are breathing each time you exhale imagine a flow doing down your arms and legs and as you inhale an energy coming into you. Whenever your attention drifts bring it back to the breathing.
- Integrate breathing with daily activities. Practice slower breather before eating, after putting the seat belt on in the car, or whenever a notification pops up on the cell phone.
- Set reminders and alarms on your phone to check how you are feeling and breathing. Leave notes on nearby furniture such as a nightstand, on the shower door, and/or on the kitchen table as reminders to be mindful of your breath. If stressed or breathing shallowly, take a moment to breathe slowly.
- Interrupt the stress response. During the day when you are aware that you shallow breathe, are holding your breath, feel anxious, experience neck and shoulder tightness, or worry and use that as a cue to shift position by sitting or standing more erect, looking upward and take a few slow diaphragmatic breaths.
- Use cue condition to facilitate this process. Each time you begin the practice smell a specific aroma or do some behavioral movement and then do the breathing. After a while the aroma or behavioral movement will become the classically conditioned cue to trigger the effortless breathing.
- Use role rehearsal and conditioning to generalize the skill. Generalizing the skills often takes more time than what may be expected. In a culture where instant relief is expected— implied message associated with medication— self-mastery techniques are different and challenging as they take time to master the skill and implement them during daily life. The process of mastery is similar to learning to play a musical instrument or sports. Learning to play the violin requires practice as well as practice with failures along the way until one is ready for more challenging musical pieces, recitals, or performances.
A useful strategy to implement the learning is role rehearsal in the office, at home at work, and in real life. It is usually much easier to practice these skills in a safe space such as your own room or, with a therapist compared to with other people or, at work. To generalize the skill most efficiently, it can be helpful to practice in a safe environment while imagining being in the actual stressful location This process is illustrated by the strategy to reduce social anxiety and menstrual cramps.
Social anxiety when seeing my supervisor. Master effortless breathing in a safe environment. Role rehearsal in imagery. If you observed that you held your breath when your supervisor is around, begin with imagery when your supervisor is not present. Sit, comfortably. Let go of muscle tension and breathe effortlessly, evoking a scenario where your supervisor is walking by and continue to breathe slowly as you imagine the scene. Role rehearsal in action. Ask another person to role-play your supervisor. Sit, comfortably. Let go of muscle tension and breathe effortlessly. Have this person walk into the room in a similar way that your supervisor would. Imagine that person is your supervisor while practicing your effortless breathing. Repeat until the effortless breathing is more automatic. Practice many times in real life. Whenever the rehearsed situation occurs, implement slower paced breathing.
Menstrual cramps that causes most women to curl up and breathe shallowly when experiencing menstrual cramps (Peper et al., 2023). Master effortless breathing in a safe environment. Practice breathing lying down. While lying down, breathe diaphragmatically by having a three-to-five-pound weight such as a bag of rice or hot water pad on your abdomen. If you have a partner, have the person stroke your legs from the abdomen to your toes while you exhale. Role rehearse experiencing pain and then practice lower diaphragmatic breathing. Namely, tighten your abdomen as if you have discomfort, then focus on relaxing the buttocks and sensing the air flowing down your legs and out your feet as you exhale. Practice in real life. A few days before you expected menstruation, practice slow diaphragmatic breathing several times for at least 5-10 minutes during the day. When your menstruation starts practice the slower and lower breathing while imagining the air flowing down the abdomen, through the legs and out the feet.
Summary/Conclusion
Breathing is the mind-body bridge. It usually occurs without awareness and breathing changes affect our thought, emotions and body. Mastering and implementing slower breathing during the day takes time and practice. By observing when breathing patterns change, participants may identify internal and external factors that affect breathing which provides an opportunity to implement effortless diaphragmatic breathing to optimize health as well as resolve some of the triggers. As one 20-year-old, female student reported,
The biggest benefit from learning diaphragmatic breathing was that it gave me the feeling of safety in many moments. My anxiety tended to make me feel unsafe in many situations but homing in and mastering diaphragmatic breathing helped tremendously. I shifted from constant chest breathing to acknowledging it and in turn, reminding myself to breathe with my diaphragm.
References
Allen, R. (2024). The health benefits of nose breathing. Nursing in General Practice. http://hdl.handle.net/10147/559021
Al-Rabia, M.W. (2016). Food-induced immunoglobulin E-mediated allergic rhinitis. J Microsc Ultrastruct, 4(2), 69-75. https://doi.org/doi.org/10.1016/j.jmau.2015.11.004
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. Peperperspective –ideas on illness, health and well-being from Erik Peper. Accessed April 16, 2024. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Banushi, B., Brendle, M., Ragnhildstveit, A., Murphy, T., Moore, C., Egberts, J., & Robison, R. (2023). Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sci. 13(2), 256. https://doi.org/10.3390/brainsci13020256
Chung, A.H., Gevirtz, R.N., Gharbo, R.S. et al. (2021).Pilot Study on Reducing Symptoms of Anxiety with a Heart Rate Variability Biofeedback Wearable and Remote Stress Management Coach. Appl Psychophysiol Biofeedback 46, 347–358. https://doi.org/10.1007/s10484-021-09519-x
Cohen, D. & Leung, A.K.Y. (2009). The hard embodiment of culture. European Journal of Social Psychology, 9, 1278–1289 https://doi.org/10.1002/ejsp.671
Codrons, E., Bernardi, N. F., Vandoni, M., & Bernardi, L. (2014). Spontaneous group synchronization of movements and respiratory rhythms. PloS one, 9(9), e107538. https://doi.org/10.1371/journal.pone.0107538
Dick, T. E., Mims, J. R., Hsieh, Y. H., Morris, K. F., & Wehrwein, E. A. (2014). Increased cardio-respiratory coupling evoked by slow deep breathing can persist in normal humans. Respiratory physiology & neurobiology, 204, 99-111. https://doil.org/10.1016/j.resp.2014.09.013
Ekerholt, K. & Bergland, A. (2008). Breathing: A sign of life and a unique area for reflection and action. Physical therapy, 88(7), 832-840. https://doi.org/10.2522/ptj.20070316
Elstad, M., O’Callaghan, E. L., Smith, A. J., Ben-Tal, A., & Ramchandra, R. (2018). Cardiorespiratory interactions in humans and animals: rhythms for life. American Journal of Physiology-Heart and Circulatory Physiology, 315(1), H6-H17. https://doi.org/10.1152/ajpheart.00701.2017
Folgering, H. (1999). The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis, 54(4), 365-72. https://pubmed.ncbi.nlm.nih.gov/10546483/
Gilbert, C. (1998). Emotional sources of dysfunctional breathing. Journal of bodywork and movement therapies, 2(4), 224-23. https://doi.org/10.1016/S1360-8592(98)80019-3
Jerath, R., Beveridge, C., & Barnes, V.A. (2019). Self-Regulation of Breathing as an Adjunctive Treatment of Insomnia. Front Psychiatry, 9(780). https://doi.org/10.3389/fpsyt.2018.00780
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Kang, K.W., Jung, S.I., Lee, do Y., Kim, K., & Lee, N.K. (2016) Effect of sitting posture on respiratory function while using a smartphone. J Phys Ther Sci, 28(5), 1496-8. https://doi.org/10.1589/jpts.28.1496
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol. 5, 756. https://doi.org/10.3389/fpsyg.2014.00756
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
MacHose, M., & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Magnon. V., Dutheil, F., & Vallet, G.T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 11(1),19267. https://doi.org/10.1038/s41598-021-98736-9
Maric, V., Ramanathan, D., & Mishra, J. (2020). Respiratory regulation & interactions with neuro-cognitive circuitry. Neuroscience & Biobehavioral Reviews, 112, 95-106. https://doi.org/10.1016/j.neubiorev.2020.02.001
Matić, Z., Platiša, M. M., Kalauzi, A., & Bojić, T. (2020). Slow 0.1 Hz breathing and body posture induced perturbations of RRI and respiratory signal complexity and cardiorespiratory coupling. Frontiers in physiology, 11, 24. https://doi.org/10.3389/fphys.2020.00024
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Meehan, Z.M. & Shaffer, F. (2023). Adding Core Muscle Contraction to Wrist-Ankle Rhythmical Skeletal Muscle Tension Increases Respiratory Sinus Arrhythmia and Low-Frequency Power. Appl Psychophysiol Biofeedback. 48(1), 127-134. https://doi.org/10.1007/s10484-022-09568-w
McKeown, P. (2021). The breathing cure: Develop new habits for a healthier, happier, and longer life. Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E. & Cohen, T. (2017). Inhale to Breathe Away Pelvic Floor Pain and Enjoy Intercourse. Biofeedback, 45 (1), 21–24. https://doi.org/10.5298/1081-5937-45.1.04
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. https://doi.org/10.15540/nr.6.3.153
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07 or https://www.researchgate.net/publication/383151816_WHAT_ABOUT_THIS_Increase_Attention_Concentration_and_School_Performance_with_Posture_Feedback
Peper, E. & MacHose, M. (1993). Symptom prescription: Inducing anxiety by 70% exhalation. Applied Psychophysiology and Biofeedback, 18(3), 133-138. https://doi.org/10.1007/BF00999790
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. 45(4), 83–87. https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019a). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128-133. https://doi.org/10.15540/nr.6.3.12
Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512
PTI. (2023 August 3). Often suck your stomach in to look slimmer in pictures? It can lead to ‘hourglass syndrome.’ The Economic Times Panache. Accessed March 26, 2024. https://economictimes.indiatimes.com/magazines/panache/often-suck-your-stomach-in-to-look-slimmer-in-pictures-it-can-lead-to-hourglass-syndrome/articleshow/102392681.cms?from=mdr
Salah, H.M., Goldberg, L.R., Molinger, J., Felker, G.M., Applefeld, W., Rassaf, T., Tedford, R.J., Mirro, M., Cleland, J.GF., & Fudim, M. (2022). Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week, Journal of the American College of Cardiology, 80(17), 1647-1659. https://doi.org/10.1016/j.jacc.2022.08.760
Shaffer, F. & Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience,14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
Taub, E., Uswatte, G., Mark, V. W., Morris, D. M. (2006). The learned nonuse phenomenon: Implications for rehabilitation. Europa Medicophysica, 42(3), 241-256. https://pubmed.ncbi.nlm.nih.gov/17039223/
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Xiao, M., Zi-Qi, Y., Gong, Z.Q., Zhang, H., Duan, N.Y., Shi, Y.T,, Wei, G.X., Li, Y.F. (2017).The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front Psychol. 8(874). https://doi.org/10.3389/fpsyg.2017.00874
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods
Posted: June 30, 2024 Filed under: ADHD, attention, behavior, CBT, digital devices, education, emotions, Evolutionary perspective, health, mindfulness, neurofeedback, Nutrition/diet, Uncategorized | Tags: ADHD, anxiety, depression, diet, glyphosate, herbicide, herbicites, mental-health, neurofeedback, pesticides, supplements', ultraprocessed foods, vitamins 4 CommentsAdapted from: Peper, E. & Shuford, J. (2024). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods. NeuroRegulation, 11(2), 219–228. https://doi.org/10.15540/nr.11.2.219
Look at your hand and remember that every cell in your body including your brain is constructed out the foods you ingested. If you ingested inferior foods (raw materials to be built your physical structure), then the structure can only be inferior. If you use superior foods, you have the opportunity to create a superior structure which provides the opportunity for superior functioning. -Erik Peper
Summary
Mental health symptoms of attention deficit hyperactivity disorder (ADHD), Autism, anxiety and depression have increased over the last 15 years. An additional risk factor that may affect mental and physical health is the foods we eat. Even though, our food may look and even taste the same as compared to 50 years ago, it contains herbicide and pesticide residues and often consist of ultra-processed foods. These foods (low in fiber, and high in sugar, animal fats and additives) are a significant part of the American diet and correlate with higher levels of inattention and hyperactivity in children with ADHD. Due to affluent malnutrition, many children are deficient in essential vitamins and minerals. We recommend that before beginning neurofeedback and behavioral treatments, diet and lifestyle are assessed (we call this Grandmother therapy assessment). If the diet appears low in organic foods and vegetable, high in ultra-processed foods and drinks, then nutritional deficiencies should be assessed. Then the next intervention step is to reduce the nutritional deficiencies and implement diet changes from ultra-processed foods to organic whole foods. Meta-analysis demonstrates that providing supplements such as Vitamin D, etc. and reducing simple carbohydrates and sugars and eating more vegetables, fruits and healthy fats during regular meals can ameliorate the symptoms and promote health.
The previous article and blog, Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms, pointed out how the changes in bonding, screen time and circadian rhythms affected physical and mental health (Peper, 2023a; Peper, 2023b). However, there are many additional factors including genetics that may contribute to the increase is ADHD, autism, anxiety, depression, allergies and autoimmune illnesses (Swatzyna et al., 2018). Genetics contribute to the risk of attention deficit hyperactivity disorder (ADHD); since, family, twin, and adoption studies have reported that ADHD runs in families (Durukan et al., 2018; Faraone & Larsson, 2019). Genetics is in most cases a risk factor that may or may not be expressed. The concept underlying this blog is that genetics loads the gun and environment and behavior pulls the trigger as shown in Figure 1.

Figure 1. Interaction between Genetics and Environment
The pandemic only escalated trends that already was occurring. For example, Bommersbach et al (2023) analyzed the national trends in mental health-related emergency department visits among USA youth, 2011-2021. They observed that in the USA, Over the last 10 years, the proportion of pediatric ED visits for mental health reasons has approximately doubled, including a 5-fold increase in suicide-related visits. The mental health-related emergency department visits increased an average of 8% per year while suicide related visits increased 23.1% per year. Similar trends have reported by Braghieri et al (2022) from the National Survey on Drug Use and Health as shown in Figure 2.

Figure 2. Mental health trends in the United States by age group in 2008–2019. The data come from the National Survey on Drug Use and Health. Reproduced with permission from Braghieri, Luca and Levy, Ro’ee and Makarin, Alexey, Social Media and Mental Health (July 28, 2022) https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
The trends reported from this data shows an increase in mental health illnesses for young people ages 18-23 and 24-29 and no changes for the older groups which could be correlated with the release of the first iPhone 2G on June 29, 2007. Thus, the Covid 19 pandemic and social isolation were not THE CAUSE but an escalation of an ongoing trend. For the younger population, the cellphone has become the vehicle for personal communication and social connections, many young people communicate more with texting than in-person and spent hours on screens which impact sleep (Peper, 2023a). At the same time, there are many other concurrent factors that may contributed to increase of ADHD, autism, anxiety, depression, allergies and autoimmune illnesses.
Without ever signing an informed consent form, we all have participated in lifestyle and environmental changes that differ from that evolved through the process of evolutionary natural selection and promoted survival of the human species. Many of those changes in lifestyle are driven by demand for short-term corporate profits over long-term health of the population. As exemplified by the significant increase in vaping in young people as a covert strategy to increase smoking (CDC, 2023) or the marketing of ultra-processed foods (van Tulleken, 2023).
This post focusses how pesticides and herbicides (exposure to neurotoxins) and changes in our food negatively affects our health and well-being and is may be another contributor to the increase risk for developing ADHD, autism, anxiety and depression. Although our food may look and even taste the same compared to 50 years ago, it is now different–more herbicide and pesticide residues and is often ultra-processed. lt contains lower levels of nutrients and vitamins such as Vitamin C, Vitamin B2, Protein, Iron, Calcium and Phosphorus than 50 years ago (Davis et al, 2004; Fernandez-Cornejo et al., 2014). Non-organic foods as compared to organic foods may reduce longevity, fertility and survival after fasting (Chhabra et al., 2013).
Being poisoned by pesticide and herbicide residues in food
Almost all foods, except those labeled organic, are contaminated with pesticides and herbicides. The United States Department of Agriculture reported that “Pesticide use more than tripled between 1960 and 1981. Herbicide use increased more than tenfold (from 35 to 478 million pounds) as more U.S. farmers began to treat their fields with these chemicals” (Fernandez-Cornejo, et al., 2013, p 11). The increase in herbicides and pesticides is correlated with a significant deterioration of health in the United States (Swanson, et al., 2014 as illustrated in the following Figure 3.


Figure 3. Correlation between Disease Prevalence and Glyphosate Applications (reproduced with permission from Swanson et al., 2014.
Although correlation is not causation and similar relationships could be plotted by correlating consumption of ultra-refined foods, antibiotic use, decrease in physical activity, increase in computer, cellphone and social media use, etc.; nevertheless, it may suggest a causal relationship. Most pesticides and herbicides are neurotoxins and can accumulate in the person over time this could affect physical and mental health (Bjørling-Poulsen et al., 2008; Arab & Mostaflou, 2022). Even though the United States Environmental Protection Agency (EPA) has determined that the residual concentrations in foods are safe, their long-term safety has not been well established (Leoci & Ruberti, 2021). Other countries, especially those in which agribusiness has less power to affect legislation thorough lobbying, and utilize the research findings from studies not funded by agribusiness, have come to different conclusions…
For example, the USA allows much higher residues of pesticides such as, Round-Up, with a toxic ingredient glyphosate (0.7 parts per million) in foods than European countries (0.01 parts per million) (Wahab et al., 2022; EPA, 2023; European Commission, 2023) as is graphically illustrated in figure 4.

Figure 4: Percent of Crops Sprayed with Glyphosate and Allowable Glyphosate Levels in the USA versus the EU
The USA allows this higher exposure than the European Union even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbo et al., 2022). The negative effects most likely would be more harmful in a rapidly growing infant than for an adult. Most likely, some individuals are more vulnerable than others and are the “canary in mine.” They are the early indicators for possible low-level long-term harm. Research has shown that fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021). Also, organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010). We hypothesize this exposure is one of the co-factors that have contributed to the decrease in mental health of adults 18 to 29 years.
At the same time as herbicides and pesticides acreage usage has increased, ultra-processed food have become a major part of the American diet (van Tulleken, 2023). Eating a diet high in ultra-processed foods, low in fiber, high sugar, animal fats and additives has been associated with higher levels of inattention and hyperactivity in children with ADHD; namely, high consumption of sugar, candy, cola beverages, and non-cola soft drinks and low consumption of fatty fish were also associated with a higher prevalence of ADHD diagnosis (Ríos-Hernández et al., 2017).
In international studies, less nutritional eating behaviors were observed in ADHD risk group as compared to the normal group (Ryu et al., 2022). Artificial food colors and additives are also a public health issue and appear to increase the risk of hyperactive behavior (Arnold et al., 2012). In a randomized double-blinded, placebo controlled trial 3 and 8/9 year old children had an increase in hyperactive behavior for those whose diet included extra additives (McCann et al., 2007). The risk may occur during fetal development since poor prenatal maternal is a critical factor in the infants neurodevelopment and is associated with an increased probability of developing ADHD and autism (Zhong et al., 2020; Mengying et al., 2016).
Poor nutrition even affects your unborn grandchild
Poor nutrition not only affects the mother and the developing fetus through epigenetic changes, it also impacts the developing eggs in the ovary of the fetus that can become the future granddaughter (Wilson, 2015). At birth, the baby has all of her eggs. Thus, there is a scientific basis for the old wives tale that curses may skip a generation. Providing maternal support is even more important since it affects the new born and the future grandchild. The risk may even begin a generation earlier since the grandmother’s poor nutrition as well as stress causes epigenetic changes in the fetus eggs. Thus 50% of the chromosomes of the grandchild were impacted epigenetically by the mother’s and grandmother’s dietary and health status .
Highly processed foods
Highly refined foods have been processed to remove many of their nutrients. These foods includes white bread, white rice, pasta, and sugary drinks and almost all the fast foods and snacks. These foods are low in fiber, vitamins, and minerals, and they are high in sugars, unhealthy fats, and calories. In addition, additives may have been added to maximize taste and mouth feel and implicitly encourage addiction to these foods. A diet high in refined sugars and carbohydrates increases the risk of diabetes and can worsen the symptoms of ADHD, autism, depression, anxiety and increase metabolic disease and diabetes (Woo et al., 2014; Lustig, 2021; van Tulleken, 2023). Del-Ponte et al. (2019) noted that a diet high in refined sugar and saturated fat increased the risk of symptoms of ADHD, whereas a healthy diet, characterized by high consumption of fruits and vegetables, would protect against the symptoms.
Most likely, a diet of highly refined foods may cause blood sugar to spike and crash, which can lead to mood swings, irritability, anxiety, depression and cognitive decline and often labeled as “hangryness” (the combination of anger and hunger) (Gomes et al., 2023; Barr et al., 2019). At the same time a Mediterranean diet improves depression significantly more than the befriending control group (Bayles et al., 2022). In addition, refined foods are low in essential vitamins and minerals as well as fiber. Not enough fiber can slow down digestion, affect the human biome, and makes it harder for the body to absorb nutrients. This can lead to nutrient deficiencies, which can contribute to the symptoms of ADHD, autism, depression, and anxiety. Foods do impact our mental and physical health as illustrated by foods that tend to reduce depression (LaChance & Ramsey, 2018; MacInerney et al., 2017). By providing appropriate micronutrients such as minerals (Iron, Magnesium Zinc), vitamins (B6, B12, B9 and D), Omega 3s (Phosphatidylserine) and changing our diet, ADHD symptoms can be ameliorated.
Many children with ADHD, anxiety, depression are low on essential vitamins and minerals. For example, low levels of Omega-3 fatty acids and vitamin D may be caused by eating ultra-refined foods, fast foods, and drinking soft drink. At the same time, the children are sitting more in indoors in front of the screen and thereby have lower sun exposure that is necessary for the vitamin D production.
“Because of lifestyle changes and sunscreen use, about 42% of Americans are deficient in vitamin D. Among children between 1 to 11 years old, an estimated 15% have vitamin D deficiency. And researchers have found that 17% of adolescents and 32% of young adults were deficient in vitamin D.” (Porto and Abu-Alreesh, 2022).
Reduced sun exposure is even more relevant for people of color (and older people); since, their darker skin (increased melanin) protects them from ultraviolet light damage but at the same time reduces the skins production of vitamin D. Northern Europeans were aware of the link between sun exposure and vitamin D production. To prevent rickets (a disease caused by vitamin D deficiency) and reduce upper respiratory tract infections the children were given a tablespoon of cod liver oil to swallow (Linday, 2010). Cod liver oil, although not always liked by children, is more nutritious than just taking a Vitamin D supplements. It is a whole food and a rich source of vitamin A and D as well as containing a variety of Omega 3 fatty acids (eicosapentaenoic acid (EPA) (USDA, 2019).
Research studies suggest that ADHD can be ameliorated with nutrients, and herbs supplements (Henry & CNS, 2023). Table 1 summarizes some of the nutritional deficits observed and the reduction of ADHD symptoms when nutritional supplements were given (adapted from Henry, 2023; Henry & CNS, 2023).
| Nutritional deficits observed in people with ADHD | Decrease in ADHD symptoms with nutritional supplements |
| Vitamin D: In meta-analysis with a total number of 11,324 children, all eight trials reported significantly lower serum concentrations of 25(OH)D in patients diagnosed with ADHD compared to healthy controls. (Kotsi et al, 2019) | After 8 weeks children receiving vitamin D (50,000 IU/week) plus magnesium (6 mg/kg/day) showed a significant reduction in emotional problems as observed in a randomized, double blind, placebo-controlled clinical trial (Hemamy et al., 2021). |
| Iron: In meta-analysis lower serum ferritin was associated with ADHD in children (Wang et al., 2017) and the mean serum ferritin levels are lower in the children with ADHD than in the controls (Konofal et al., 2004). | After 12 weeks of supplementation with Iron (ferrous sulfate) in double-blind, randomized placebo-controlled clinical trial, clinical trials symptoms of in children with ADHD as compared to controls were reduced (Tohidi et al., 2021; Pongpitakdamrong et all, 2022). |
| Omega 3’s: Children with ADHD are more likely to be deficient in omega 3’s than children without ADHD (Chang et al., 2017). | Adding Omega-3 supplements to their diet resulted in an improvement in hyperactivity, impulsivity, learning, reading and short term memory as compared to controls in 16 randomized controlled trials including 1514 children and young adults with ADHD (Derbyshire, 2017) |
| Magnesium: In meta-analysis, subjects with ADHD had lower serum magnesium levels compared with to their healthy controls (Effatpahah et al., 2019) | 8 weeks of supplementation with Vitamin D and magnesium caused a significant decrease in children with conduct problems, social problems, and anxiety/shy scores (Hemamy et al., 2020). |
| Vitamin B2, B6, B9 and B12deficiency has been found in many patients with Attention Deficit and Hyperactivity Disorder (Landaas et al, 2016; Unal et al., 2019). | Vitamin therapy appears to reduce symptoms of ADHD and ASD (Poudineh et al., 2023; Unal et al., 2019). An 8 weeks supplementing with Vitamin B6 and magnesium decreased hyperactivity and hyperemotivity/aggressiveness. When supplementation was stopped, clinical symptoms of the disease reappeared in few weeks (Mousain-Bosc et al., 2006). |
Table 1. Examples of vitamin and mineral deficiencies associated with symptoms of ADHD and supplementation to reduction of ADHD symptoms.
Supplementation of vitamins and minerals in many cases consisted of more than one single vitamin or mineral. For an in-depth analysis and presentation, see the superb webinar by Henry & CNS (2023): https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback? (Henry & CNS, 2023).
Whole foods are more than the sum of individual parts (the identified individual constituents/nutrients). The process of digestion is much more complicated than ingesting simple foods with added vitamins or minerals. Digestion is the interaction of many food components (many of which we have not identified) which interact and affect the human biome. A simple added nutrient can help; however, eating whole organic foods it most likely be healthier. For example, whole-wheat flour is much more nutritious. Whole wheat is rich in vitamins B-1, B-3, B-5, riboflavin, folate well as fiber while refined white flour has been bleached and stripped of fiber and nutrients to which some added vitamins and iron are added.
Recommendation
When working with clients, follow Talib’s principles as outlined in Part 1 by Peper (2023) which suggests that to improve health first remove the unnatural which in this case are the ultra-processed foods, simple carbohydrates, exposure to pesticides and herbicides (Taleb, 2014). The approach is beneficial for prevention and treatment. This recommendation to optimize health is both very simple and very challenging. The simple recommendation is to eat only organic foods and as much variety as possible as recommended by Professor Michael Pollan in his books, Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules (Pollan, 2006; Pollan, 2011).
Do not eat foods that contain herbicides and pesticide residues or are ultra-processed. Although organic foods especially vegetable and fruits are often much more expensive, you have choice: You can pay more now to optimize health or pay later to treat disease. Be safe and not sorry. This recommendation is similar to the quote, “Let food be thy medicine and medicine be thy food,” that has been attributed falsely since the 1970s to Hippocrates, the Greek founder of western medicine (5th Century, BC) (Cardenas, 2013).
There are many factors that interfere with implementing these suggestions; since, numerous people live in food deserts (no easy access to healthy unprocessed foods ) or food swamps (a plethora of fast food outlets) and 54 million Americans are food insecure (Ney, 2022). In addition, we and our parents have been programmed by the food industry advertising to eat the ultra- processed foods and may no longer know how to prepare healthy foods such as exemplified by a Mediterranean diet. Recent research by Bayles et al (2022) has shown that eating a Mediterranean diet improves depression significantly more than the befriending control group. In addition, highly processed foods and snacks are omnipresent, often addictive and more economical.
Remember that clients are individuals and almost all research findings are based upon group averages. Even when the data implies that a certain intervention is highly successful, there are always some participants for whom it is very beneficial and some for whom it is ineffective or even harmful. Thus, interventions need to be individualized for which there is usually only very limited data. In most cases, the original studies did not identify the characteristics of those who were highly successful or those who were unsuccessful. In addition, when working with specific individuals with ADHD, anxiety, depression, etc. there are multiple possible causes.
Before beginning specific clinical treatment such as neurofeedback and/or medication, we recommend the following:
- “Grandmother assessment” that includes and assessment of screen time, physical activity, outdoor sun exposure, sleep rhythm as outlined in Part 1 by Peper (2023). Then follow-up with a dietary assessment that investigates the prevalence of organic/non organic foods, ingestion of fast foods, ultra-processed foods, soft drinks, high simple carbohydrate and sugar, salty/sugary/fatty snacks, fruits, vegetables, and eating patterns (eating with family or by themselves in front of screens). Be sure to include an assessment of emotional reactivity and frequency of irritability and “hangryness”.
- If the assessment suggest low level of organic whole foods and predominance of ultra- refined foods, it may be possible that the person is deficient in vitamins and minerals. Recommend that the child is tested for the vitamin deficiencies. If vitamin deficiencies identified, recommend to supplement the diet with the necessary vitamins and mineral and encourage eating foods that naturally include these substances (Henry & CNS, 2023). If there is a high level of emotional reactivity and “hangryness,” a possible contributing factor could be hypoglycemic rebound from a high simple carbohydrate (sugar) intake or not eating breakfast combined with hyperventilation (Engel et al., 1947; Barr et al., 2019). Recommend eliminating simple carbohydrate breakfast and fast food snacks and substitute organic foods that include complex carbohydrates, protein, fats, vegetables and fruit. Be sure to eat breakfast.
- Implement “Grandmother Therapy”. Encourage the family and child to change their diet to eating a whide variety of organic foods (vegetables, fruits, some fish, meat and possibly dairy) and eliminate simple carbohydrates and sugars. This diet will tend to reduce nutritional deficits and may eliminate the need for supplements.
- Concurrent with the stabilization of the physiology begin psychophysiological treatment strategies such as neurofeedback biofeedback and cognitive behavior therapy.
Relevant blogs
Author Disclosure
Authors have no grants, financial interests, or conflicts to disclose.
References
Arnold, L, Lofthouse, N., & Hurt, E. (2012). Artificial food colors and attention-deficit/hyperactivity symptoms: conclusions to dye for. Neurotherapeutics, 9(3), 599-609. https://doi.org/10.1007/s13311-012-0133-x
Arab, A. & Mostafalou, S. (2022). Neurotoxicity of pesticides in the context of CNS chronic diseases. International Journal of Environmental Health Research, 32(12), 2718-2755. https://doi.org/10.1080/09603123.2021.1987396
Barr, E.A., Peper, E., & Swatzyna, R.J. (2019). Slouched Posture, Sleep Deprivation, and Mood Disorders: Interconnection and Modulation by Theta Brain Waves. NeuroRegulation, 6(4), 181–189. https://doi.org/10.15540/nr.6.4.181
Bayes. J., Schloss, J., Sibbritt, D. (2022). The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND: A Mediterranean Diet in MEN with Depression” study): a randomized controlled trial. Am J Clin Nutr. 116(2), 572-580. https://doi.org/10.1093/ajcn/nqac106
Bjørling-Poulsen, M., Andersen, H.R. & Grandjean, P. Potential developmental neurotoxicity of pesticides used in Europe. Environ Health 7, 50 (2008). https://doi.org/10.1186/1476-069X-7-50
Bommersbach, T.J., McKean, A.J., Olfson, M., Rhee, T.G. (2023). National Trends in Mental Health–Related Emergency Department Visits Among Youth, 2011-2020. JAMA, 329(17):1469–1477. https://doi.org/10.1001/jama.2023.4809
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Cardenas, D. (2013). Let not thy food be confused with thy medicine: The Hippocratic misquotation. e-Spen Journal, 8(6), 3260-3262. https://doi.org/10.1016/j.clnme.2013.10.002
CDC, (2023). Quick Facts on the Risks of E-cigarettes for Kids, Teens, and Young Adults. CDC. Centers for Disease Control and Prevention. Accessed September 23, 2023. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html
Chang, J.C., Su, K.P., Mondelli, V. et al. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: a Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacol. 43, 534–545. https://doi.org/10.1038/npp.2017.160
Chhabra, R., Kolli, S., & Bauer, J.H. (2013). Organically Grown Food Provides Health Benefits to Drosophila melanogaster. PLoS ONE, 8(1): e52988. https://doi.org/10.1371/journal.pone.0052988
Davis, D. R., Epp, M. D., & Riordan, H. D. (2004). Changes in USDA food composition data for 43 garden crops, 1950 to 1999. Journal of the American College of Nutrition, 23(6), 669-682. https://doi.org/10.1080/07315724.2004.10719409
Derbyshire, E. (2017). Do Omega-3/6 Fatty Acids Have a Therapeutic Role in Children and Young People with ADHD? J Lipids. 6285218. https://doi.org/10.1155/2017/6285218
Del-Ponte, B., Quinte, G.C., Cruz, S., Grellert, M., & Santos, I. S. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): A systematic review and meta-analysis. Journal of Affective Disorders, 252, 160-173. https://doi.org/10.1016/j.jad.2019.04.061
Durukan, İ., Kara, K., Almbaideen, M., Karaman, D., & Gül, H. (2018). Alexithymia, depression and anxiety in parents of children with neurodevelopmental disorder: Comparative study of autistic disorder, pervasive developmental disorder not otherwise specified and attention deficit-hyperactivity disorder. Pediatrics International, 60(3), 247–253. https://doi.org/10.1111/ped.13510
Effatpanah, M., Rezaei, M., Effatpanah, H., Effatpanah, Z., Varkaneh, H.K., Mousavi. S.M., Fatahi, S., Rinaldi, G., & Hashemi, R. (2019). Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Res, 274, 228-234. https://doi.org/10.1016/j.psychres.2019.02.043
Engel, G.L., Ferris, E.B., & Logan, M. (1947). Hyperventilation; analysis of clinical symptomatology. Ann Intern Med, 27(5), 683-704. https://doi.org/10.7326/0003-4819-27-5-683
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians
Faraone, S.V. & Larsson, H. (2019). Genetics of attention deficit hyperactivity disorder. Mol Psychiatry, 24(4), 562-575. https://doi.org/10.1038/s41380-018-0070-0
Fernandez-Cornejo, J. Nehring, R, Osteen, C., Wechsler, S., Martin, A., & Vialou, A. (2014). Pesticide use in the U.S. Agriculture: 21 Selected Crops, 1960-2008. Economic Information Bulletin Number 123, United State Department of Agriculture. https://www.ers.usda.gov/webdocs/publications/43854/46734_eib124.pdf
Gomes, G. N., Vidal, F. N., Khandpur. N., et al. (2023). Association Between Consumption of Ultraprocessed Foods and Cognitive Decline. JAMA Neurol, 80(2),142–150. https://doi.org/10.1001/jamaneurol.2022.4397
Hemamy, M., Heidari-Beni, M., Askari, G., Karahmadi, M., & Maracy, M. (2020). Effect of Vitamin D and Magnesium Supplementation on Behavior Problems in Children with Attention-Deficit Hyperactivity Disorder. Int J Prev Med, 11(1), 4. https://doi.org/10.4103/ijpvm.IJPVM_546_17
Henry, K. (2023). An Integrative Medicine Approach to ADHD. Rupa Health. Accessed September 30, 2023. https://www.rupahealth.com/post/an-integrative-medicine-approach-to-adhd
Henry, K. & CNS, L.A. (2023). Natural treatments for ADHD. Webinar Presentation by IntegrativePractitioner.com and sponsored by Rupa Health, June 6, 2023 https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback?
Hemamy, M., Pahlavani, N., Amanollahi, A. et al. (2021). The effect of vitamin D and magnesium supplementation on the mental health status of attention-deficit hyperactive children: a randomized controlled trial. BMC Pediatr, 21, 178. https://doi.org/10.1186/s12887-021-02631-1
Konofal, E., Lecendreux, M., Arnulf, I., & Mouren, M. (2004). Iron Deficiency in Children With Attention-Deficit/Hyperactivity Disorder. Arch Pediatr Adolesc Med, 158(12), 1113–1115. https://doi.org/10.1001/archpedi.158.12.1113
Kotsi, E., Kotsi, E. & Perrea, D.N. (2019). Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): a meta-analysis. ADHD Atten Def Hyp Disord, 11, 221–232. https://doi.org/10.1007/s12402-018-0276-7
LaChance, L.R. & Ramsey, D. (2018). Antidepressant foods: An evidence-based nutrient profiling system for depression. World J Psychiatr, 8(3): 97-104. World J Psychiatr., 8(3): 97-104. https://doi.org/10.5498/wjp.v8.i3.97
Landaas, E.T., Aarsland, T.I., Ulvik, A., Halmøy, A., Ueland. P.M., & Haavik, J. (20166). Vitamin levels in adults with ADHD. BJPsych Open, 2(6), 377-384. https://doi.org/10.1192/bjpo.bp.116.003491
Linday, L.A. (2010). Cod liver oil, young children, and upper respiratory tract infections. J Am Coll Nutr, 29(6), 559-62. https://doi.org/10.1080/07315724.2010.10719894
Leoci, R. & Ruberti, M. (2021) Pesticides: An Overview of the Current Health Problems of Their Use. Journal of Geoscience and Environment Protection, 9, 1-20. https://doi.org/10.4236/gep.2021.98001
Lustig, R.H. (2021). Metaboical: The lure and the lies of processed food, nutrition, and modern medicine. New York: Harper Wave. https://www.amazon.com/Metabolical-processed-poisons-people-planet/dp/1529350077
MacInerney, E. K., Swatzyna, R. J., Roark, A. J., Gonzalez, B. C., & Kozlowski, G. P. (2017). Breakfast choices influence brainwave activity: Single case study of a 12-year-old female. NeuroRegulation, 4(1), 56–62. https://doi.org/10.15540/nr.4.1.56
McCann, D., Barrett, A., Cooper, A., Crumpler, D., Dalen, L., Grimshaw, K., et al. (2007). Food additives and hyperactive behavior in 3-year old and 8/9-year-old children in the community: a randomized, double-blinded, placebo-controlled trial. Lancet, 370(9598), 1560-1567. https://doi.org/10.1016/S0140-6736(07)61306-3
Mengying, L.I, Fallin, A, D., Riley,A., Landa, R., Walker, S.O., Silverstein, M., Caruso, D., et al. (2016). The Association of Maternal Obesity and Diabetes With Autism and Other Developmental Disabilities. Pediatrics, 137(2), e20152206. https://doi.org/10.1542/peds.2015-2206
Mousain-Bosc, M., Roche, M., Polge, A., Pradal-Prat, D., Rapin, J., & Bali, J.P. (2006). Improvement of neurobehavioral disorders in children supplemented with magnesium-vitamin B6. I. Attention deficit hyperactivity disorders. Magnes Res. 19(1), 46-52. https://pubmed.ncbi.nlm.nih.gov/16846100/#:~:text=In%20almost%20all%20cases%20of,increase%20in%20Erc%2DMg%20values.
Ney, J. (2022). Food Deserts and Inequality. Social Policy Data Lab. Updated: Jan 24, 2022. Accessed September, 23, 2023. https://www.socialpolicylab.org/post/grow-your-blog-community
Peper, E. (2023a). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. the peperperspective July 2, 2023. Accessed august 8, 2024, https://peperperspective.com/2023/07/04/reflections-on-the-increase-in-autism-adhd-anxiety-and-depression-part-1-bonding-screen-time-and-circadian-rhythms/
Peper, E. (2023b). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation, 10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Pollan, M. (2006). Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules. New York Penguin Press. https://www.amazon.com/Omnivores-Dilemma-Natural-History-Meals/dp/1594200823/ref=tmm_hrd_swatch_0?_
Pollan, M. (2011). Food rules. New York Penguin Press. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/B00VSBILFG/ref=tmm_hrd_swatch_0?
Pongpitakdamrong, A., Chirdkiatgumchai, V., Ruangdaraganon, N., Roongpraiwan, R., Sirachainan, N., Soongprasit, M., & Udomsubpayakul, U. (2022). Effect of Iron Supplementation in Children with Attention-Deficit/Hyperactivity Disorder and Iron Deficiency: A Randomized Controlled Trial. Journal of Developmental & Behavioral Pediatrics, 43(2), 80-86., https://doi.org/10.1097/DBP.0000000000000993
Porto, A. & Abu-Alreesh, S. (2022). Vitamin D for babies, children & adolescents. Health Living. Healthychildren.org. Accessed September 24, 2023. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/vitamin-d-on-the-double.aspx#
Poudineh, M., Parvin, S., Omidali, M., Nikzad, F., Mohammadyari, F., Sadeghi Poor Ranjbar, F., F., Nanbakhsh, S., & Olangian-Tehrani, S. (2023). The Effects of Vitamin Therapy on ASD and ADHD: A Narrative Review. CNS & Neurological Disorders – Drug Targets (Formerly Current Drug Targets – CNS & Neurological Disorders), (22), 5, 2023, 711-735. https://doi.org/10.2174/1871527321666220517205813
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Ríos-Hernández, A., Alda, J.A., Farran-Codina, A., Ferreira-García, E., & Izquierdo-Pulido, M. (2017). The Mediterranean Diet and ADHD in Children and Adolescents. Pediatrics, 139(2):e20162027. https://doi.org/10.1542/peds.2016-2027
Ryu, S.A., Choi, Y.J., An, H., Kwon, H.J., Ha, M., Hong, Y.C., Hong, S.J., & Hwang, H.J. (2022). Associations between Dietary Intake and Attention Deficit Hyperactivity Disorder (ADHD) Scores by Repeated Measurements in School-Age Children. Nutrients, 14(14), 2919. https://doi.org/10.3390/nu14142919
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Swanson, N.L., Leu, A., Abrahamson, J., & Wallet, B. (2014). Genetically engineered crops, glyphosate and the deterioration of health in the United States of America. Journal of Organic Systems, 9(2), 6-17. https://www.organic-systems.org/journal/92/JOS_Volume-9_Number-2_Nov_2014-Swanson-et-al.pdf
Swatzyna, R. J., Boutros, N. N., Genovese, A. C., MacInerney, E. K., Roark, A. J., & Kozlowski, G. P. (2018). Electroencephalogram (EEG) for children with autism spectrum disorder: Evidential considerations for routine screening. European Child & Adolescent Psychiatry, 28(5), 615–624. https://doi.org/10.1007/s00787-018-1225-x
Taleb, N. N. (2014). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. https://www.amazon.com/Antifragile-Things-That-Disorder-Incerto/dp/0812979680/ref=tmm_pap_swatch_0
Tohidi, S., Bidabadi, E., Khosousi, M.J., Amoukhteh, M., Kousha, M., Mashouf, P., Shahraki, T. (2021). Effects of Iron Supplementation on Attention Deficit Hyperactivity Disorder in Children Treated with Methylphenidate. Clin Psychopharmacol Neurosci, 19(4), 712-720. https://doi.org/10.9758/cpn.2021.19.4.712
Unal, D. Çelebi, F., Bildik,H.N., Koyuncu, A., & Karahan, S. (2019). Vitamin B12 and haemoglobin levels may be related with ADHD symptoms: a study in Turkish children with ADHD, Psychiatry and Clinical Psychopharmacology, 29(4), 515-519. https://doi.org/10.1080/24750573.2018.1459005
USDA. (2019). Fish oil, cod liver. FoodData Central. USDA U.S> Department of Agriculture. Published 4/1/2019. Accessed September 24, 2024. https://fdc.nal.usda.gov/fdc-app.html#/food-details/173577/nutrients
Van Tulleken, C. (2023). Ultra-Processed People. The Science Behind Food That Isn’t Food. New York: W.W. Norton & Company. https://www.amazon.com/Ultra-Processed-People-Science-Behind-Food/dp/1324036729/ref=asc_df_1324036729/?
Wahab, S., Muzammil, K., Nasir, N., Khan, M.S., Ahmad, M.F., Khalid, M., Ahmad, W., Dawria, A., Reddy, L.K.V., & Busayli, A.M. (2022). Advancement and New Trends in Analysis of Pesticide Residues in Food: A Comprehensive Review. Plants (Basel), 11(9), 1106. https://doi.org/10.3390/plants11091106
Wang. Y., Huang, L., Zhang, L., Qu, Y., & Mu, D. (2017). Iron Status in Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. PLoS One, 12(1):e0169145. https://doi.org/10.1371/journal.pone.0169145
Wilson, L. (2015). Mothers, beware: Your lifestyle choices will even affect your grandkids.
News Corp Australia Network. Accessed Jun 24, 2024. https://www.news.com.au/lifestyle/parenting/kids/mothers-beware-your-lifestyle-choices-will-even-affect-your-grandkids/news-story/3f326f457546cfb32af5c409f335fb56
Woo, H.D.,; Kim, D.W., Hong, Y.-S., Kim, Y.-M.,Seo, J.-H.,; Choe, B.M., Park, J.H.,; Kang, J.-W., Yoo, J.-H.,; Chueh, H.W., et al. (2014). Dietary Patterns in Children with Attention Deficit/Hyperactivity Disorder (ADHD). Nutrients, 6, 1539-1553. https://doi.org/10.3390/nu6041539
Zhong, C., Tessing, J., Lee, B.K., Lyall, K. Maternal Dietary Factors and the Risk of Autism Spectrum Disorders: A Systematic Review of Existing Evidence. Autism Res,13(10),1634-1658. https://doi.org/10.1002/aur.2402
Quick Rescue Techniques When Stressed
Posted: February 4, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, education, emotions, Evolutionary perspective, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, posture, relaxation, stress management, Uncategorized | Tags: alarm reaction, anxiety, box breathing, Breathing, conditioning, defense reaction, health, huming, Parasympathetic response, rumination, safety, sniff inhale, somatic practices, stress, sympathetic arousal, tactical breathing, Toning, yoga 9 CommentsErik Peper, PhD, Yuval Oded, PhD, and Richard Harvey, PhD
Adapted from Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312

“If a problem is fixable, if a situation is such that you can do something about it, then there is no need to worry. If it’s not fixable, then there is no help in worrying. There is no benefit in worrying whatsoever.” ― Dalai Lama XIV
To implement the Dalai Lama’s quote is challenging. When caught up in an argument, being angry, extremely frustrated, or totally stressed, it is easy to ruminate, worry. It is much more challenging to remember to stay calm. When remembering the message of the Dalai Lama’s quote, it may be possible to shift perspective about the situation although a mindful attitude may not stop ruminating thoughts. The body typically continues to reacti to the torrents of thoughts that may occur when rehashing rage over injustices, fear over physical or psychological threats, or profound grief and sadness over the loss of a family member. Some people become even more agitated and less rational as illustrated in the following examples.
I had an argument with my ex and I am still pissed off. Each time I think of him or anticipate seeing them, my whole body tightened. I cannot stomach seeing him and I already see the anger in his face and voice. My thoughts kept rehashing the conflict and I am getting more and more upset.
A car cut right in front of me to squeeze into my lane. I had to slam on my brakes. What an idiot! My heart rate was racing and I wanted to punch the driver.
When threatened, we respond quickly in our thoughts and body with a defense reaction that may negatively affect those around us as well as ourselves. What can we do to interrupt negative stress reactions?
Background
Many approaches exist that allow us to become calmer and less reactive. General categories include techniques of cognitive reappraisal (seeing the situation from the other person’s point of view and labeling your own feelings and emotions) and stress management techniques. Practices that are beneficial include mindfulness meditation, benign humor (versus gallows humor), listening to music, taking a time out while implementing a variety of self-soothing practices, or incorporating slow breathing (e.g., heart rate variability and/or box breathing) throughout the day.
No technique fits all as we respond differently to our stressful life circumstances. For example, some people during stress react with a “tend and befriend stress response” (Cohen & Lansing, 2021; Taylor et al., 2000). This response appears to be mostly mediated by the hormone oxytocin acting in ways that sooth or calm the nervous system as an analgesic. These neurophysiological mechanisms of the soothing with the calming analgesic effects of oxytocin have been characterized in detail by Xin, et al. (2017).
The most common response is a fight/flight/freeze stress response that is mediated by excitatory hormones such as adrenalin and inhibitory neurotransmitters such as gamma amino butyric acid (GABA). There is a long history of fight/flight/freeze stress response research, which is beyond the scope of this blog with major theories and terms such as interior milleau (Bernard, 1872); homeostasis and fight/flight (Cannon, 1929); general adaptation syndrome (Selye, 1951); polyvagal theory (Porges, 1995); and, allostatic load (McEwen, 1998). A simplified way to start a discussion about stress reactions begins with the fight/flight stress response. When stressed our defense reactions are triggered. Our sympathetic nervous system becomes activated our mind and body stereotypically responds as illustrated in Figure 1.

Figure 1. An intense confrontation tends to evoke a stress response (reproduced from Peper et al., 2020).
The flight/fight response triggers a cascade of stress hormones or neurotransmitters (e.g., hypothalamus-pituitary-adrenal cascade) and produces body changes such as the heart pounding, quicker breathing, an increase in muscle tension and sweating. Our body mobilizes itself to protect itself from danger. Our focus is on immediate survival and not what will occur in the future (Porges, 2021; Sapolsky, 2004). It is as if we are facing an angry lion—a life-threatening situation—and we feel threatened and unsafe.
Rather than sitting still, a quick effective strategy is to interrupt this fight/flight response process by completing the alarm reaction such as by moving our muscles (e.g., simulating a fight or flight behavior) before continuing with slower breathing or other self-soothing strategies. Many people have experienced their body tension is reduced and they feel calmer when they do vigorous exercise after being upset, frustrated or angry. Similarly, athletes often have reported that they experience reduced frequency and/or intensity of negative thoughts after an exhausting workout (Thayer, 2003; Liao et al., 2015; Basso & Suzuki, 2017).
Becoming aware of the escalating cascades of physical, behavioral and psychological responses to a stressor is the first step in interrupting the escalating process. After becoming aware, reduce the body’s arousal and change the though patterns using any of the techniques described in this blog. The self-regulation skills presented in this blog are ideally over-learned and automated so that these skills can be rapidly implemented to shift from being stressed to being calm. Examples of skills that can shift from sympathetic neervous system overarousal to parasympathetic nervous system calm include techniques of autogenic traing (Schulz & Luthe, 1959), the quieting reflex developed by Charles Stroebel in 1985 or more recently rescue breathing developed by Richard Gevirtz (Stroebel, 1985; Gevirtz, 2014; Peper, Gibney & Holt, 2002; Peper & Gibney, 2003).
Concepts underlying the rescue techniques
- Psychophysiological principle: “Every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, conscious or unconscious, and conversely, every change in the mental-emotional state, conscious or unconscious, is accompanied by an appropriate change in the physiological state” (Green et al. 1970, p. 3).
- Posture evokes memories and feelings associated with the position. When the body posture is erect and tall while looking slightly up. It is easier to evoke empowering, positive thoughts and feelings. When looking down it is easier to evoke hopeless, helpless and powerless thoughts and feelings (Peper et al., 2017).
- Healing occurs more easily when relaxed and feeling safe. Feeling safe and nurtured enhances the parasympathetic state and reduces the sympathetic state. Use memory recall to evoke those experiences when you felt safe (Peper, 2021).
- Interrupting thoughts is easier with somatic movement than by redirecting attention and thinking of something else without somatic movement.
- Focus on what you want to do not want to do. Attempting to stop thinking or ruminating about something tends to keeps it present (e.g., do not think of pink elephants. What color is the elephant? When you answer, “not pink,” you are still thinking pink). A general concept is to direct your attention (or have others guide you) to something else (Hilt & Pollak, 2012; Oded, 2018; Seo, 2023).
- Skill mastery takes practice and role rehearsal (Lally et al., 2010; Peper & Wilson, 2021).
- Use classical conditioning concepts to facilitate shifting states. Practice the skills and associate them with an aroma, memory, sounds or touch cues. Then when you the situation occurs, use these classical conditioned cues to facilitate the regeneration response (Peper & Wilson, 2021).
Rescue techniques
Coping When Highly Stressed and Agitated
- Complete the alarm/defense reaction with physical activity (Be careful when you do these physical exercises if you have back, hip, knee, or ankle problems).
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Check whether the situation is actually a threat. If yes, then do anything to get out of immediate danger (yell, scream, fight, run away, or dial 911).
- If there is no actual physical threat, then leave the situation and perform vigorous physical activity to complete your alarm reaction, such as going for a run or walking quickly up and down stairs. As you do the exercise, push yourself so that the muscles in your thighs are aching, which focusses your attention on the sensations in your thighs. In our experience, an intensive run for 20 minutes quiets the brain while it often takes 40 minutes when walking somewhat quickly.
- After recovering from the exhaustive exercise, explore new options to resolve the conflict.
- Complete the alarm/defense reaction and evoke calmness with the S.O.S™ technique (Oded, 2023)
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Squat against a wall (similar to the wall-sit many skiers practice). While tensing your arms and fists as shown in Figure 2, gaze upward because it is more difficult to engage in negative thinking while looking upwards. If you continue to ruminate, then scan the room for object of a certain color or feature to shift visual attention and be totally present on the visual object.
- Do this set of movements for 7 to 10 seconds or until you start shaking. Than stand up and relax hands and legs. While standing, bounce up and down loosely for 10 to 15 seconds as you become aware of the vibratory sensations in your arms and shoulders, as shown in Figure 3.

Figure 2.Defense position wall-sit to tighten muscles in the protective defense posture (Oded, 2023). Figure 3. Bouncing up and down to loosen muscles ((Oded, 2023).
- Acknowledge you have reacted and have chosen to interrupt your automatic response. Swing your arms back and forth for 20 seconds. Allow the arms to swing freely as illustrated in Figure 4.

Figure 4. Swinging the arms to loosen the body and spine (Oded, 2023).
- Rest and ground. Lie on the floor and put your calves and feet on a chair seat so that the psoas muscle can relax, as illustrated in Figure 5. Allow yourself to be totally supported by the floor and chair. Be sure there is a small pillow under your head and put your hand on your abdomen so that you can focus on abdominal breathing.

Figure 5. Lying down to allow the psoas muscle to relax and feel grounded (Oded, 2023).
- While lying down, imagine a safe place or memory and make it as real as possible. It is often helpful to listen to a guided imagery or music. The experience can be enhanced if cues are present that are associated with the safe place, such as pictures, sounds, or smells. Continue to breathe effortlessly at about six breaths per minute. If your attention wanders, bring it back to the memory or to the breathing. Allow yourself to rest for 10 minutes.
In most cases, thoughts stop and the body’s parasympathetic activity becomes dominant as the person feels safe and calm. Usually, the hands warm and the blood volume pulse amplitude increases as an indicator of feeling safe, as shown in Figure 6.

Figure 6. Blood volume pulse increases as the person is relaxing, feels safe and calm.
Coping When You Can’t Get Away (adapted from Peper, Harvey & Faass, 2020)
In many cases, it is difficult or embarrassing to remove yourself from the situation when you are stressed out such as at work, in a business meeting or social gathering.
- Become aware that you have reacted.
- Excuse yourself for a moment and go to a private space, such as a restroom. Going to the bathroom is one of the only acceptable social behaviors to leave a meeting for a short time.
- In the bathroom stall, do the 5-minute Nyingma exercise, which was taught by Tarthang Tulku Rinpoche in the tradition of Tibetan Buddhism, as a strategy for thought stopping (see Figure 7). Stand on your toes with your heels touching each other. Lift your heels off the floor while bending your knees. Place your hands at your sides and look upward. Breathe slowly and deeply (e.g., belly breathing at six breaths a minute) and imagine the air circulating through your legs and arms. Do this slow breathing and visualization next to a wall so you can steady yourself if necessary to keep balance. Stay in this position for 5 minutes or longer. Do not straighten your legs—keep squatting despite the discomfort. In a very short time, your attention is captured by the burning sensation in your thighs. Continue. After 5 minutes, stop and shake your arms and legs.

Figure 7. Stressor squat Nyingma exercise (reproduced from Peper et al., 2020).
- Follow this practice with slow abdominal breathing to enhance the parasympathetic response. Be sure that the abdomen expands as the inhalation occurs. Breathe in and out through the nose at about six breaths per minute.
- Once you feel centered and peaceful, return to the room.
- After this exercise, your racing thoughts most likely will have stopped and you will be able to continue your day with greater calm.
What to do When Ruminating, Agitated, Anxious or Depressed
(adapted from Peper, Harvey, & Hamiel, 2019).
- Shift your position by sitting or standing erect in a power position with the back of the head reaching upward to the ceiling while slightly gazing upward. Then sniff quickly through nose, hold and again sniff quickly then very slowly exhale. Be sure as you exhale your abdomen constricts. Then sniff again as your abdomen gets bigger, hold, and sniff one more time letting the abdomen get even bigger. Then, very slow, exhale through the nose to the internal count of six (adapted from Balban et al., 2023). When you sniff or gasp, your racing thoughts will stop (Peper et al., 2016).
- Continue with box breathing (sometimes described as tactical breathing or battle breathing) by exhaling slowly through your nose for 4 seconds, holding your breath for 4 seconds, inhaling slowly for 4 seconds through your nose, holding your breath for 4 seconds and then repeating this cycle of breathing for a few minutes (Röttger et al., 2021; Balban et al., 2023). Focusing your attention on performing the box breathing makes it almost impossible to think of anything else. After a few minutes, follow this with slow effortless diaphragmatic breathing at about six breaths per minute. While exhaling slowly through your nose, look up and when you inhale imagine the air coming from above you. Then as you exhale, imagine and feel the air flowing down and through your arms and legs and out the hands and feet.
- While gazing upward, elicit a positive memory or a time when you felt safe, powerful, strong and/or grounded. Make the positive memory as real as possible.
- Implement cognitive strategies such as reframing the issue, sending goodwill to the person, seeing the problem from the other person’s point of view, and ask is this problem worth dying over (Peper, Harvey, & Hamiel, 2019).
What to Do When Thoughts Keep Interrupting
Practice humming or toning. When you are humming or toning, your focus is on making the sound and the thoughts tend to stop. Generally, breathing will slow down to about six breaths per minute (Peper, Pollack et al., 2019). Explore the following:
- Box breathing (Röttger et al., 2021; Balban et al., 2023)
- Humming also known as bee breath (Bhramari Pranayama) (Abishek et al., 2019; Yoga, 2023) – Allow the tongue to rest against the upper palate, sit tall and erect so that the back of the head is reaching upward to the ceiling, and inhale through your nose as the abdomen expands. Then begin humming while the air flows out through your nose, feel the vibration in the nose, face and throat. Let humming last for about 7 seconds and then allow the air to blow in through the nose and then hum again. Continue for about 5 minutes.
- Toning – Inhale through your nose and then vocalize a single sound such as Om. As you vocalize the lower sound, feel the vibration in your throat, chest and even going down to the abdomen. Let each toning exhalation last for about 6 to 7 seconds and then inhale through your nose. Continue for about 5 minutes (Peper, al., 2019).
Many people report that after practice these skills, they become aware that they are reacting and are able to reduce their automatic reaction. As a result, they experience a significant decrease in their stress levels, fewer symptoms such as neck and holder tension and high blood pressure, and they feel an increase in tranquility and the ability to communicate effectively.
Practicing these skills does not resolve the conflicts; they allow you to stop reacting automatically. This process allows you a time out and may give you the ability to be calmer, which allows you to think more clearly. When calmer, problem solving is usually more successful. As phrased in a popular meme, “You cannot see your reflection in boiling water. Similarly, you cannot see the truth in a state of anger. When the waters calm, clarity comes” (author unknown).

Boiling water (photo modified from: https://www.facebook.com/photo/?fbid=388991500314839&set=a.377199901493999)
Below are additional resources that describe the practices. Please share these resources with friends, family and co-workers.
Stressor squat instructions
Toning instructions
Diaphragmatic breathing instructions
Reduce stress with posture and breathing
Conditioning
References
Abishek, K., Bakshi, S. S., & Bhavanani, A. B. (2019). The efficacy of yogic breathing exercise bhramari pranayama in relieving symptoms of chronic rhinosinusitis. International Journal of Yoga, 12(2), 120–123. https://doi.org/10.4103/ijoy.IJOY_32_18
Balban, M. Y., Neri, E., Kogon, M. M., Weed, L., Nouriani, B., Jo, B., Holl, G., Zeitzer, J. M., Spiegel, D., Huberman, A. D. (2023). Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Reports Medicine, 4(1), 10089. https://doi.org/10.1016/j.xcrm.2022.100895
Basso, J. C. & Suzuki, W. A. (2017). The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plast, 2(2), 127–152. https://doi.org/10.3233/BPL-160040
Bernard, C. (1872). De la physiologie générale. Paris: Hachette livre. https://www.amazon.ca/PHYSIOLOGIE-GENERALE-BERNARD-C/dp/2012178596
Cannon, W. B. (1929). Organization for Physiological Homeostasis. Physiological Reviews, 9, 399–431. https://doi.org/10.1152/physrev.1929.9.3.399
Cohen, L. & Lansing, A. H. (2021). The tend and befriend theory of stress: Understanding the biological, evolutionary, and psychosocial aspects of the female stress response. In: Hazlett-Stevens, H. (eds), Biopsychosocial Factors of Stress, and Mindfulness for Stress Reduction. pp. 67–81, Springer, Cham. https://doi.org/10.1007/978-3-030-81245-4_3
Gevirtz, R. (2014). HRV Training and its Importance – Richard Gevirtz, Ph.D., Pioneer in HRV Research & Training. Thought Technology. Accessed December 29, 2023. https://www.youtube.com/watch?v=9nwFUKuJSE0
Green, E. E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological. Journal of Transpersonal Psychology, 2, 1–26. https://atpweb.org/jtparchive/trps-02-70-01-001.pdf
Hilt, L. M., & Pollak, S. D. (2012). Getting out of rumination: comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165.
https://doi.org/10.1007/s10802-012-9638-3
Lally, P., VanJaarsveld, C. H., Potts, H. W., & Wardle, J. (2010). How habits are formed: Modelling habit formation the real world. European Journal of Social Psychology, 40, 998–1009. https://doi.org/10.1002/ejsp.674
Liao, Y., Shonkoff, E. T., & Dunton, G. F. (2015). The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology. 6, 1975. https://doi.org/10.3389/fpsyg.2015.01975
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44.
https://doi.org/10.1111/j.1749-6632.1998.tb09546.x
Oded, Y. (2018). Integrating mindfulness and biofeedback in the treatment of posttraumatic stress disorder. Biofeedback, 46(2), 37-47. https://doi.org/10.5298/1081-5937-46.02.03
Oded, Y. (2023). Personal communication. S.O.S 1™ technique is part of the Sense Of Safety™ method. www.senseofsafety.co
Peper, E. (2021). Relive memory to create healing imagery. Somatics, XVIII(4), 32–35.https://www.researchgate.net/publication/369114535_Relive_memory_to_create_healing_imagery
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., & Gibney, K.H. (2003). A teaching strategy for successful hand warming. Somatics. XIV(1), 26–30. https://www.researchgate.net/publication/376954376_A_teaching_strategy_for_successful_hand_warming
Peper, E., Harvey, R., & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153–160. https://doi.org/10.15540/nr.6.3.153
Peper, E., Lee, S., Harvey, R., & Lin, I-M. (2016). Breathing and math performance: Implication for performance and neurotherapy. NeuroRegulation, 3(4), 142–149. http://dx.doi.org/10.15540/nr.3.4.142
Peper, E., Lin, I-M, Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128–133. https://www.neuroregulation.org/article/view/19345/13263
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 9(2), 46–49. https://doi.org/10.5298/1081-5937-49-2-04
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology, 32(4), 301–318. https://doi.org/10.1111/j.1469-8986.1995.tb01213.x
Porges, S.W. (2021) Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry, 20(2),296-298. Porges SW. Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry. 2021 Jun;20(2):296-298. https://doi.org10.1002/wps.20871
Röttger, S., Theobald, D. A., Abendroth, J., & Jacobsen, T. (2021). The effectiveness of combat tactical breathing as compared with prolonged exhalation. Applied Psychophysiology and Biofeedback, 46, 19–28. https://doi.org/10.1007/s10484-020-09485-w
Sapolsky, R. (2004). Why zebras don’t get ulcers (3rd ed.). New York:Holt. https://www.amazon.com/Why-Zebras-Dont-Ulcers-Third/dp/0805073698/
Schultz, J. H., & Luthe, W. (1959). Autogenic training: A psychophysiologic approach to psychotherapy. Grune & Stratton. https://www.google.com/books/edition/Autogenic_Training/y8SwQgAACAAJ?hl=en
Selye, H. (1951). The general-adaptation-syndrome. Annual Review of Medicine, 2(1), 327–342. https://doi.org/10.1146/annurev.me.02.020151.001551
Seo, H. (2023). How to stop ruminating. The New York Times. Accessed January 3, 2024. https://www.nytimes.com/2023/02/01/well/mind/stop-rumination-worry.html
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-quieting-reflex-Charles-Stroebel/dp/0425085066
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A. R., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. https://doi.org/10.1037/0033-295X.107.3.411
Thayer, R. E. (2003). Calm energy: How people regulate mood with food and exercise. Oxford University Press. https://www.amazon.com/Calm-Energy-People-Regulate-Exercise/dp/0195163397
Xin, Q., Bai, B., & Liu, W. (2017). The analgesic effects of oxytocin in the peripheral and central nervous system. Neurochemistry International, 103, 57–64. https://doi.org/10.1016/j.neuint.2016.12.021
Yoga, N. (2023). This simple breath practice is scientifically proven to calm your mind. The nomadic yogi. Accessed December 31, 2023. https://www.leahsugerman.com/blog/bhramari-pranayama-humming-bee-breath#