Pragmatic techniques for monitoring and coaching breathing
Posted: December 14, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, emotions, meditation, mindfulness, neurofeedback, Pain/discomfort, posture, relaxation, self-healing, Uncategorized | Tags: art, books, Breathing rate, coaching, FlowMD app, nasal breathing, personal-development, self-monitoring, writing 4 CommentsDaniella Matto, MA, BCIA BCB-HRV , Erik Peper, PhD, BCB, and Richard Harvey, PhD
Adapted from: Matto, D., Peper, E., & Harvey, R. (2025). Monitoring and coaching breathing patterns and rate. Townsend Letter-Innovative Health Perspectives. https://townsendletter.com/monitoring-and-coaching-breathing-patterns-and-rate/
This blog aims to describe several practical strategies to observe and monitor breathing patterns to promote effortless diaphragmatic breathing. The goal of these strategies is to foster effortless, whole-body diaphragmatic breathing that promote health.
Breathing is usually covert and people are not usually aware of their breathing rate (breaths per minute) or pattern (abdominal or thoracic, breath holding or shallow breathing) unless they have an illness such as asthma, emphysema or are performing physical activity (Boulding et al, 2015)). Observing breathing is challenging; awareness of respiration often leads to unaware changes in the breath pattern or to an attempt to breathe perfectly (van Dixhoorn, 2021). Ideally breathing patterns should be observed/monitored when the person is unaware of their breathing pattern and the whole body participates (van Dixhoorn, 2008). A useful strategy is to have the person perform a task and then ask, “What happened to your breathing?”. For example, ask a person to simulate putting a thread through the eye of a needle or quickly look to the extreme right and left while keeping their head still. In almost all cases, the person holds their breath (Peper et al., 2002).
Teaching effortless slow diaphragmatic breathing is a precursor of Heart rate variability (HRV) biofeedback and is based on slow paced breathing (Lehrer & Gevirtz, 2014; Steffen et al., 2017; Shaffer and Meehan, 2020). Mastering effortless diaphragmatic breathing is a powerful tool in the treatment of a variety of physical, behavioural, and cognitive conditions; however, to integrate this method into clinical or educational practice is easier said than done. Clients with dysfunctional breathing patterns often have difficulty following a breath pacer or mastering effortless breathing at a slower pace.
The purpose of this paper is to describe a few simple strategies that can be used to observe and monitor breathing patterns, provide economic strategies for observation and training, and suggestions to facilitate effortless diaphragmatic breathing.
Strategies to observe and monitor breathing pattern
Observation of the breathing patterns
- Is the breathing through the nose or mouth? Nose is usually better (Watso et al., 2023; Nestor, 2020).
- Does the abdomen expand during inhalation and constricts during exhalation or does the chest expand and rise during inhalation and fall during exhalation? Abdominal movement is usually better.
- Is exhalation flow softly or explosively like a sigh? Slow flow exhalation is preferred.
- Is the breath held or continues during activities? In most cases continued breathing is usually better.
- Does the person gasp before speaking or allows to speak while normally exhaling?
- What is the breathing rate (breaths per minute)? When sitting peacefully less than 14 breaths/minute is usually better and about 6 breaths per minute to optimize HRV
Physiological monitoring.
- Monitoring breathing with strain gauges around the abdomen and chest, and heart rate is the most common approach to identify the location of breath, the breathing pattern and heart rate variability. The strain gauges are placed around the chest and abdomen and heart rate is monitored with a blood volume pulse amplitude sensor from the finger. representative recording shows the effect of thoughts on breathing, heartrate and pulse amplitude of which the participant is totally unaware as shown in Figure 1.
Figure 1. Physiological recording of breathing patterns with strain gauges.
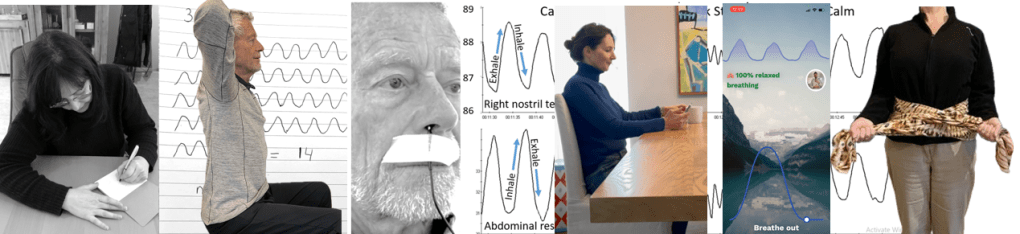
- Monitoring breathing with a thermistor placed at the entrance of the nostril that has the most airflow (nasal patency) (Jovanov et al., 2001; Lerman et al., 2016). When the person exhales through the nose, the thermistor temperature increases and decreases when they inhale. A representative recording of a person being calm, thinking a stressful thought. and being calm. Although there were significant changes as indicated by the change in breathing patterns, the person was unaware of the changes as shown in Figure 2.
Figure 2. Use of a thermistor to monitor breathing from the dominant nostril compared to the abdominal expansion as monitored by a strain gauge around the abdomen.
- Additional physiological monitoring approaches. There are many other physiological measures can be monitored to such as end-tidal carbon dioxide (EtCO2), a non-invasive measurement of the amount of carbon dioxide (CO2) in exhaled breath (Meuret et al., 2008; Meckley, 2013); scalene/trapezius EMG to identify thoracic breathing (Peper & Tibbett, 1992; Peper & Tibbets, 1994); low abdominal EMG to identify transfers and oblique tightening during exhalation and relaxation during inhalation (Peper et al., 2016; and heart rate to monitor cardiorespiratory synchrony (Shaffer & Meehan, 2020). Physiological monitoring is useful; since, the clinician and the participant can observe the actual breathing pattern in real time, how the pattern changes in response the cognitive and physical tasks, and used for feedback training. The recorded data can document breathing problems and evidence of mastery.
The challenges of using physiological monitoring arethat the equipment may be expensive, takes skill to operate and interpret the data, and is usually located in the office and not at home.
Economic strategies for observation and training breathing
To complement the physiological monitoring and allow observations outside the office and at home, some of the following strategies may be used to observe breathing pattern (rate and expansion of the breath in the body), and suggestion to facilitate effortless diaphragmatic breathing. These exercises make excellent homework for the client. Practicing awareness and internal self-regulation by the client outside the clinic contributes enormously to the effect of biofeedback training (Wilson et al., 2023),
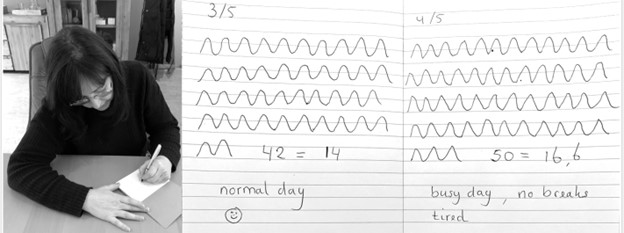
Observe breathing rate: Draw the breathing pattern
Take a piece of paper, a pen and a timer, set to 3 minutes. Start the timer. Upon inhalation draw the line up and upon exhalation draw the line down, creating a wave. When the timer stops, after 3 minutes, calculate the breathing rate per minute by dividing the number of waves by 3 as shown in Figure 3.
Figure 3. Drawing the breathing pattern for three minutes during two different days.
From these drawings, the breathing rate become evident. Many individuals are often surprised to discover that their breathing rate increased during periods of stress, such as a busy day with no breaks, compared to their normal days.
Monitoring and training diaphragmatic breathing
The scarf technique for abdominal feedback
Many participants are unaware that they are predominantly breathing in their chest and their abdomen expansion is very limited during inhalation. Before beginning, have participant loosen their belt and or stand upright since sitting collapsed/slouched or having the waist constriction such as a belt of tight constrictive clothing that inhibits abdominal expansion during inhalation.
Place the middle part of a long scarf or shawl on your lower back, take the ends in both hands and cross the ends: your left hand is holding the right part of the scarf, and the right hand is holding the left end of the scarf. Give a bit of a pull, so you can feel any movement of the scarf. When breathing more abdominally you will feel a pull at the ends of the scarf as you lower back, and flanks will expand as shown in Figure 4.

Figure 4. Using a scarf as feedback.
FlowMD app
A recent cellphone app, FlowMD, is unique because it uses the cellphone camera to detect the subtle movements of the chest and abdomen (FlowMD, 2024). It provides real time feedback of the persons breathing pattern. Using this app, the person sits in front of their cellphone camera and after calibration, the breathing pattern is displayed as shown in Figure 5.

Figure 5. Training breathing with FlowMD,.
Suggestions to optimize abdominal breathing that may lead to a slower breath rate when the client practices the technique
Beach pose
By locking the upper chest and sitting up straight it is often easier to breathe so that the abdomen can expand and constrict. Place your hands behind your head and Interlock your finger of both hands, pull your elbows back and up. The person can practice this either laying down on their back or sitting straight up at the edge of the chair as shown in Figure 6.

Figure 6. Sitting erect with the shoulders pulled back and up to allow abdominal expansion and constriction as the breathing pattern.
Observe the effect of posture on breathing
Have the person sit slouched/collapsed like a letter C and take a few slow breath, then have them sit up in a tall and erect position and take a few slow breaths. Usually they will observe that it is easier to breathe slower and lower and tall and erect.
Using your hands for feedback to guide natural breathing
Holding your hands with index fingers and thumbs touching the lower abdomen. When inhaling the fingers and thumbs separate and when exhaling they touch again (ensuring a full exhale and avoiding over breathing). The slight increase in lower abdominal muscle tension during the exhalation and relaxation during inhalation and the abdominal wall expands can also be felt with fingertips as shown in Figure 7.
Figure 7. Using your hands and finger for feedback to guide the natural breathing of expansion and constriction of the abdomen. Reproduced by permission from Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49.
Coaching suggestions
There are many strategies to observe, teach and implement effortless breathing (Peper et al., 2024).. Even though breathing is natural and babies and young children breathe diaphragmatically as their large belly expands and constricts. Yet, in many cases the natural breathing shifts to dysfunctional breathing for multiple reasons such as chronic triggering defense reactions to avoiding pain following abdominal surgery (Peper et al, 2015). When participants initially attempt to relearn this natural pattern, it can be challenging especially, if the person habitually breathes shallowly, rapidly and predominantly in their chest.
When initially teaching effortless breathing, have the person exhale more air than normal without the upper chest compressing down and instead allow the abdomen comes in and up thereby exhaling all the air. If the person is upright then allow inhalation to occur without effort by letting the abdominal wall relaxes and expands. Initially inhale more than normal by expanding the abdomen without lifting the chest. Then exhale very slowly and continue to breathe so that the abdomen expands in 360 degrees during inhalation and constricts during exhalation. Let the breathing go slower with less and less effort. Usually, the person can feel the anus dropping and relaxing during inhalation.
Another technique is to ask the person to breathe in more air than normal and then breathe in a little extra air to completely fill the lungs, before exhaling fully. Clients often report that it teaches them to use the full capacity of the lungs.
The goal is to breath without effort. Indirectly this can be monitored by finger temperature. If the finger temperature decreases, the participant most likely is over-breathing or breathing with too much effort, creating sympathetic activity; if the finger temperature increases, breathing occurs slower and usually with less effort indicating that the person’s sympathetic activation is reduced.
Conclusion
There are many strategies to monitor and coach breathing. Relearning diaphragmatic breathing can be difficult due to habitual shallow chest breathing or post-surgical adaptations. Initial coaching may involve extended exhalations, conscious abdominal expansion, and gentle inhalation without chest movement. Progress can be monitored through indirect physiological markers like finger temperature, which reflects changes in sympathetic activity. The integration of these techniques into clinical or educational practice enhances self-regulation, contributing significantly to therapeutic outcomes. In this article we provided a few strategies which may be useful for some clients.
Additional blogs on breathing
https://peperperspective.com/2015/09/25/resolving-pelvic-floor-pain-a-case-report/
REFERENCES
Boulding, R., Stacey, R., & Niven, N. (2016). Dysfunctional breathing: a review of the literature and proposal for classification. European Respiratory Review, 25(141),: 287-294. https://doi.org/10.1183/16000617.0088-2015
FlowMD. (2024). FlowMD app. Accessed December 13, 2024. https://desktop.flowmd.co/
Jovanov, E., Raskovic, D., & Hormigo, R. (2001). Thermistor-based breathing sensor for circadian rhythm evaluation. Biomedical sciences instrumentation, 37, 493–497. https://pubmed.ncbi.nlm.nih.gov/11347441/
Lehrer, P. & Gevirtz R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol, 5,756. https://doi.org/10.3389/fpsyg.2014.00756
Lerman, J., Feldman, D., Feldman, R. et al. Linshom respiratory monitoring device: a novel temperature-based respiratory monitor. (2016). Can J Anesth/J Can Anesth, 63, 1154–1160. https://doi.org/10.1007/s12630-016-0694-y
Meckley, A. (2013). Balancing Unbalanced Breathing: The Clinical Use of Capnographic Biofeedback. Biofeedback, 41(4), 183–187. https://doi.org/10.5298/1081-5937-41.4.02
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (2008). Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of psychiatric research, 42(7), 560–568. https://doi.org/10.1016/j.jpsychires.2007.06.005
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath-New-Science-Lost-Art/dp/0735213615/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Gibney, K.H., & Holt, C.F. (2002). Make Health Happen. Dubuque, IA: Kendall/Hunt Publishing Company. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/
Peper, E., & Tibbetts, V. (1992). Fifteen-month follow-up with asthmatics utilizing EMG/incentive inspirometer feedback. Biofeedback and self-regulation, 17(2), 143–151. https://doi.org/10.1007/BF01000104
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. https://biofeedbackhealth.org/wp-content/uploads/2011/01/peper-and-tibbets-effortless-diaphragmatic.pdf
Shaffer, F. and Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., and Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
van Dixhoorn, J.V. (2008). Whole-body breathing. Biofeedback, 36,54–58. https://www.euronet.nl/users/dixhoorn/L.513.pdf
van Dixhoorn, J.V. (2021). Functioneel ademen-Adem-en ontspannings oefeningen voor gevorderden. Amersfoort: Uiteveriy Van Dixhoorn. https://www.bol.com/nl/nl/p/functioneel-ademen/9300000132165255/
Watso, J. C., Cuba, J.N., Boutwell, S.L, Moss, J…(2023). Acute nasal breathing lowers diastolic blood pressure and increases parasympathetic contributions to heart rate variability in young adults. American Journal of Physiology Regulatory, Integrative and Comparative Physiology.
325I(6), R797-R80. https://doi.org/10.1152/ajpregu.00148.2023
Wilson, V., Somers, K. & Peper, E. (2023). Differentiating Successful from Less Successful Males and Females in a Group Relaxation/Biofeedback Stress Management Program. Biofeedback, 51(3), 53–67. https://doi.org/10.5298/608570
[1] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Health Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Tel: 415 338 7683 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com
Suggestions for mastering and generalizing breathing skills
Posted: October 30, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cellphone, cognitive behavior therapy, emotions, ergonomics, healing, health, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, self-healing, stress management, Uncategorized | Tags: abdominal beathing, anxiety, diaphragmatic braething, health, hyperventilation, meditation, mental-health, mindfulness, mouth breathing, Toning 3 CommentsAdapted from: Peper, E., Oded, Y., Harvey, R., Hughes, P., Ingram, H., & Martinez, E. (2024). Breathing for health: Mastering and generalizing breathing skills. Townsend Letter-Innovative Health Perspectives. November 15, 2024. https://townsendletter.com/suggestions-for-mastering-and-generalizing-breathing-skills/

Breathing techniques are commonly employed with complimentary treatments, biofeedback, neurofeedback or adjunctive therapeutic strategies to reduce stress and symptoms associated with excessive sympathetic arousal such as anxiety, high blood pressure, insomnia, or gastrointestinal discomfort. Even though it seems so simple, some participants experience difficulty in mastering effortless breathing and/or transferring slow breathing skills into daily life. The purpose of this article is to describe: 1) factors that may interfere with learning slow diaphragmatic breathing (also called cadence or paced breathing, HRV or resonant frequency breathing along with other names), 2) challenges that may occur when learning diaphragmatic breathing, and 3) strategies to generalize the effortless breathing into daily life.
Background
A simple two-item to-do list could be: ‘Breathe in, breathe out.’ Simple things are not always easy to master. Mastering and implementing effortless ‘diaphragmatic’ or ‘abdominal belly’ breathing may be simple, yet not easy. Breathing is a dynamic process that involves the diaphragm, abdominal, pelvic floor and intercostal muscles that can include synchronizing the functions of the heart and lungs and may result in cardio-respiratory synchrony or coupling, as well as ‘heart-rate variability breathing training (Codrons et al., 2014; Dick et al., 2014; Elstad et al., 2018; Maric et al., 2020; Matic et al., 2020). Improving heart-rate variability is a useful approach to reduce symptoms of stress and promotes health and reduce anxiety, asthma, blood pressure, insomnia, gastrointestinal discomfort and many other symptoms associated with excessive sympathetic activity (Lehrer & Gevirtz, 2014; Xiao et al., 2017; Jerath et al., 2019; Chung et al., 2021; Magnon et al., 2021; Peper et al., 2022).
Breathing can be effortful and In some cases people have dysfunctional breathing patterns such as breath holding, rapid breathing (hyperventilation), shallow breathing and lack of abdominal movement. This usually occurs without awareness and may contribute to illness onset and maintenance. When participants learn and implement effortless breathing, symptoms often are reduced. For example, when college students are asked to practice effortless diaphragmatic breathing twenty-minutes a day for one week, as well as transform during the day dysfunction breathing patterns into diaphragmatic breathing, they report a reduction in shallow breathing, breath holding,, and a decrease of symptoms as shown in Fig 1 (Peper et al, 2022).

Figure 1. Percent of people who reported that their initial symptoms improved after practicing slow diaphragmatic breathing for twenty minutes per day over the course of a week (reproduced from: Peper et al, 2022).
Most students became aware of their dysfunctional breathing and substituted slow, diaphragmatic breathing whenever they realized they were under stress; however, some students had difficulty mastering ‘effortless’ (e.g., automated, non-volitional) slow, diaphragmatic breathing that allowed abdominal expansion during inhalation.
Among those had more difficulty, they tended to have almost no abdominal movement (expansion during inhalation and abdominal constriction during exhalation). They tended to breathe shallowly as well as quickly in their chest using the accessory muscles of breathing (sternocleidomastoid, pectoralis major and minor, serratus anterior, latissimus dorsi, and serratus posterior superior).
The lack of abdominal movement during breathing reduced the movement of lymph as well as venous blood return in the abdomen; since; the movement of the diaphragm (the expansion and constriction of the abdomen) acts a pump. Breathing predominantly in the chest may increase the risk of anxiety, neck, back and shoulder pain as well as increase abdominal discomfort, acid reflux, irritable bowel, dysmenorrhea and pelvic floor pain (Banushi et al., 2023; Salah et al., 2023; Peper & Cohen, 2017; Peper et al., 2017; Peper et al., 2020, Peper et al., 2023). Learning slow, diaphragmatic or effortless breathing at about six breaths per minute (resonant frequency ) is also an ‘active ingredient’ in heartrate variability (HRV) training (Steffen et al., 2017; Shaffer & Meehan, 2020).
1. Factors that interfere with slow, diaphragmatic breathing
Difficulty allowing the skeletal and visceral muscles in the abdomen to expand or constrict in ‘three-dimensions’ (e.g., all around you in 360 degrees) during inhalation or exhalation. Whereas internal factors under volitional control and will mediate breathing practices, external factors can restrict and moderate the movement of the muscles. For example:
Clothing restrictions (designer jeans syndrome). The clothing is too tight around the abdomen; thereby, the abdomen cannot expand (MacHose & Peper, 1991; Peper et al., 2016). An extreme example were the corsets worn in the late 19th century that was correlated with numerous illnesses.
Suggested solutions and recommendations: Explain the physiology of breathing and how breathing occurs by the diaphragmatic movement. Discuss how babies and dogs breathe when they are relaxed; namely, the predominant movement is in the abdomen while the chest is relaxed. This would also be true when a person is sitting or standing tall. Discuss what happens when the person is eating and feels full and how they feel better when they loosen their waist constriction. When their belt is loosened or the waist button of their pants is undone, they usually feel better.
Experiential practice. If the person is wearing a belt, have the person purposely tighten their belt so that the circumference of the stomach is made much smaller. If the person is not wearing a belt, have them circle their waist with their hands and compress it so that the abdomen can not expand. Have them compare breathing with the constricted waist versus when the belt is loosened and then describe what they experienced.
Most participants will feel it is easier to breathe and much more comfortable when the abdomen is not constricted.
Previous abdominal injury. When a person has had abdominal surgery (e.g., Cesarean section, appendectomy, hernia repair, or episiotomy), they unknowingly may have learned to avoid pain by not moving (relaxing or tensing) the abdomen muscles (Peper et al., 2015; Peper et al., 2016). Each time the abdomen expands or constricts, it would have pulled on the injured area or stitches that would have cause pain. The body immediately learns to limit movement in the affected area to avoid pain. The reduction in abdominal movement becomes the new normal ‘feeling’ of abdominal muscle inactivity and is integrated in all daily activities. This is a process known as ‘learned disuse’ (Taub et al., 2006). In some cases, learned disuse may be combined with fear that abdominal movement may cause harm or injury such as after having a kidney transplant. The reduction in abdominal movement induces shallow thoracic breathing which could increase the risk of anxiety and would reduce abdominal venous and lymph circulation that my interfere with the healing.
Suggested solutions and recommendations. Discuss the concept of learned disuse and have participant practice abdominal movement and lower and slower breathing.
Experiential practices: Practicing abdominal movements
Sit straight up and purposely exhale while pulling the abdomen in and upward and inhale while expanding the abdomen. Even with these instructions, some people may continue to breathe in their chest. To limit chest movement, have the person interlock their hands and bring them up to the ceiling while going back as far as possible. This would lock the shoulders and allows the abdomen to elongate and thereby increase the diaphragmatic movement by allowing the abdomen to expand. If people initially have held their abdomen chronically tight then the initial expansion of abdomen by relaxing those muscle occurs with staccato movement. When the person becomes more skilled relaxing the abdominal muscles during inhalation the movement becomes smoother.
Make a “psssssst” sound while exhaling. Sit tall and erect and slightly pull in and up the abdominal wall and feel the anus tightening (pulling the pelvic floor up) while making the sound. Then allow inhalation to occur by relaxing the stomach and feeling the anus go down.
Use your hands as feedback. Sit up straight, placing one hand on the chest and another on the abdomen. While breathing feel the expansion of the abdomen and the contraction of the abdomen during exhalation. Use a mirror to monitor the chest-muscle movement to ensure there is limited rising and falling in this area.
Observe the effect of collapsed sitting. When sitting with the lower back curled, there is limited movement in the lower abdomen (between the pubic region and the umbilicus/belly button) and the breathing movement is shallower without any lower pelvic involvement (Kang et al., 2016). This is a common position of people who are working at their computer or looking at their cellphone.
Experiential practice: looking at your cellphone
Sit in a collapsed position and look down at your cellphone. Look at the screen and text as quickly as possible.
Compare this to sitting up and then lift the cell phone at eye level while looking straight ahead at the cellphone. Look at the screen and text as quickly as possible.
Observe how the position effected your breathing and peripheral awareness. Most likely, your experience is similar those reported by students. Close to 85%% of students who complete this activity reported that their breathing was shallower sitting slouched versus erect and about 85% of the students reported that their peripheral awareness and vision improved when sitting erect (Peper et al., 2024).
Suggested solutions and recommendations. Be aware how posture affect breathing. While sitting, place a rolled-up towel against the lower back so that the person sits more erect which would allow the abdomen to expand when inhaling.
Self-image, self-esteem, and confidence. Participants may hold their abdomen in because they want to look slim (sometimes labeled as the “hourglass syndrome” associate expanding the abdomen as unattractive (PTI, 2023). A flat abdomen is culturally reinforced by social media and fashion models and encouraged in some activities such as ballet. On the other hand, some people purposely puff up their chest to increase size and dominance (Cohen & Leung, 2009).
Suggested solutions and recommendations. Discuss the benefits of diaphragmatic breathing including its ability to reduce anxiety in social settings that may enhance confidence. Similar to an earlier suggestion, have the person explore clothing with a looser waist that still supports feelings of attractiveness and power.
Feeling anxious, fearful or threatened. The normal physiological stress reaction is a slight gasp with the tightening of the abdomen muscles for protection when a stressor occurs (Gilbert, 1998; Ekerholt & Bergland., 2008). The stressor can be an actual physical event, social situation or thoughts and emotions. Shallow breathing is a natural self-protective response. This pattern is often maintained until one feels ‘safe’ enough to relax, which for many can have a duration of the entire day or until finding the relative safety of sleep.
Suggested solutions and recommendations. Discuss how the physiological stress reaction is a normal response pattern that the person most likely learned in early childhood for self-protection. This pattern is often observed in clients who are emotionally sensitive and/or react excessively to a variety of stimuli. Note that some people have learned not to show their reactivity on their face or in the overt behaviors, yet they continue to breathe shallowly as a telltale sign of ‘distress.’ People who breath shallowly may experience this response as burdensome. Discuss with them how to reframe their sensitivity as a gift; namely, they are more aware of other people’s reactions and emotions. They just need to learn how not to respond automatically. Encourage awareness of their breath-holding and shallow breathing. Follow this by teaching them to replace the dysfunctional breathing with slow, diaphragmatic breathing at 6-breaths-per-minute. A possible training sequence is the following:
- Teach slow, diaphragmatic breathing
- Practice evoking a stressor and the moment the client senses the stress response, shallow breaths or holds their breath have them shift to slow, diaphragmatic breathing.
- If the person slouches in response to stress, the moment they become aware of slouching, have then sit erect, look up and then breathe diaphragmatically. (Peper et al., 2019)
Experiential practice: Transform stressful thoughts by looking up, breathing, and changing thoughts.
Evoke a stressor and then attempt to reframe the experience (cognitive behavior therapy or CBT approach).
Compare this to evoking a stressor, then shift to an upright position while looking up, take a few slow, diaphragmatic breaths, and reframe the experience.
In almost all cases, when the client shifts position, looks up and then reframes, the stress reaction is significantly reduced and it is much easier to reframe the experiences positively compared to when only attempting to reframe the experience (Peper et al., 2019).
Diaphragmatic breathing feels abnormal. How you breathe habitually is what feels normal unless there is overt illness such as asthma or emphysema. Any new pattern usually feels abnormal. When the person shifts their breathing pattern, such as in a transition from habitual shallow chest breathing to slower diaphragmatic abdominal breathing, it feels strange and wrong.
Suggested solutions and recommendations. Discuss the concept that habitual patterns are normal (e.g., a person who typically slouches when standing straight may experience that they are going to fall backwards). Emphasize the importance of making a shift in posture and leaning into the discomfort of the new experience. Often after practicing slow diaphragmatic breathing, the person may report feeling much more relaxed (e.g., sensing heaviness and warmth) with their fingers increasing in temperature.
2. Challenges that may occur when learning diaphragmatic breathing
Ideally, breathing is an effortless diaphragmatic process as described by the phrase, “it breathes me” (Luthe & Schultz, 1970; Luthe, 1979); however, some participants struggle to achieve this type of breathing. The following are common challenges and possible solutions:
Distraction and internal dialogue. Many people struggle with thoughts jumping from one area to another. Some people refer to this mental state as “monkey mind.”
Suggested solutions and recommendations. Validate that distraction and internal dialogue are normal and require continual managing and practice to overcome. Experimental Practice: Have the person train focus during diaphragmatic breathing techniques by focusing on 1 item in the room. Remind them that when thoughts arise, note them briefly instead of engaging with them and then refocus on the item. Start with increments of time and increase with practice.
Effect of gravity on breathing. In the vertical position, exhalation occurs when the abdomen constricts (slight tightening of the transverse and oblique abdominal muscles and the pelvic floor) pushes the diaphragm up, allowing the air to go out. It needs to push against gravity.
In the vertical position, inhalation occurs when the abdominal muscles and pelvic floor muscles relax and the abdomen widens in all directions (360 degrees) which causes the diaphragm to descend as it is being pulled down by gravity. This process allows effortless inhalation. The experience is the opposite when lying supine on one’s back. While lying down, gravity pulls on the abdomen that cause the diaphragm to go upward allowing the air to flow out during exhalation. Inhalation takes work because as the diaphragm descends it has to push the abdominal content upward against gravity.
Experiential practice: Erect versus supine
- Vertical position. Begin by exhaling completely by pulling the abdomen in and up while staying erect and not pressing/contracting the chest downward. At the end of exhalation, allow the abdomen to relax (pop out) and feel how the air is sucked in without trying to inhale
- Horizontal position. Begin by lying down, with the face pointing up. Inhale by expanding your abdomen and pushing your abdomen upward against gravity. Then let exhalation occur while totally relaxing as gravity pushes the abdomen downward, which pushes the diaphragm upward into the chest allowing the air to flow out. Optionally, place a small bag of rice/beans (e.g., approximately one to five pound or. One-half to two kilograms) on your lower abdomen while lying down. When you inhale, push the weight upward and away from you by allowing the stomach, but not the chest, to expand. Allow exhalation to occur as the weight pushes your abdomen down and upward into your chest. The weight is useful as it allows the mind to focus more easily on the task of feeling the movement of the abdomen.
Over breathing/hyperventilation. Even breathing at about six breaths per minute can cause hyperventilation can occur. Hyperventilation occurs when a person is breathing in excess of the metabolic needs of the body and thereby eliminating more carbon dioxide. The result is respiratory alkalosis and an elevated blood pH as the dissolved carbon dioxide (pCO2) in the blood is reduced (Folgering, 1999).
The most common symptoms of over breathing are colder sweaty hands and light-headedness. If this starts to occur, focus on decreasing the airflow during exhalation by exhaling through pursed lips making the sound, “Pssssssst.” While making this sound, make the sound softer with less airflow. Alternatively, have them imagine a holding a dandelion flower a few inches from their lips and blow so softly the seeds do not blow away. The blowing away of the seed is the feedback that you are blowing to hard as shown in Figure 2.

Figure 2. Dandelion seeds as feedback when the person is blowing with too much effort. Alternatively, we recommend that the client imagine smelling the scent/fragrance of a flower that usually causes nose inhalation and then exhale gently through pursed lips ast if the air flows over a candle and, the flame does not move back and forth.
Mouth breathing. Mouth breathing contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded miss-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. Nose breathing reduces airway irritation since the nose filters, humidifies, warms/cools the inhaled air as well as reduces the air turbulence in the upper airways. The epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation (McKeown, 2019; Allen, 2024). Note that alternate nostril breathing, such as breathing in one nostril for 5-seconds and out of the other for 5-seconds is another technique which some people find beneficial.
Slower breathing approaches also facilitates sympathetic parasympathetic balance and reduces airway irritation. If the person breathes habitually through their mouth, refer them to health care provider to explore factors that may contribute to mouth breathing such as enlarged tonsils and adenoids or deviated septum. In addition, explore environmental factors that could contribute nasal inflammation such as allergies or foods such as dairy (Al-Raby, 2016).
Performance anxiety. Many participants are concerned about their performance. The direct instructions such as “follow the graphic” causes the person to try hard to breathe with too much effort. Explore some of the following indirect strategies to interrupt ongoing cognitive judgements and self-talk.
- Toning or humming (Peper et al., 2019a). While exhaling, have the person hum a sound with their mouth closed. Let the sound go for about 6 seconds, relax, inhale and hum again. Toning is very similar except you verbalize a tone such as “Oammm.” (For detailed instructions on toning, see: Anziani & Peper (2021)).
- Stroking down arms and legs during exhalation. Have a partner gently stroke down your arms from your shoulder past your fingertips as you are exhaling. The downward stroking is in rhythm with the exhalation. As the arm is being stroked, attend to the sensations going down the arms. Be sure that the toucher exhales at the same time and the stroking down the arm takes about six seconds. After being stroked for a few times, have the person imagine that each time they exhale they feel a flow down through their arms and out their fingers.
- Repeat the same process while stroking down the legs from the side of their hips to their toes.
- Finally, have the person imagine/feel the sensation streaming down their legs with each exhalation.
- Many participants will report that they sense a steaming going down their arms, that they hands warm up, and their thought have stopped.
- Integrated body movement with breathing especially flexion and contraction (Meehan & Shaffer, 2023). Integrate the normal response of flexion that induces exhalation and extension evokes inhalation. Be careful that the flexion movement does not encourage participants to compress their chest during exhalation, which tends to encourage chest breathing. Have the person focus on their head staying tall and erect. Have the person sit straight up with their feet slight apart and their hands palm down on their lap. Allow inhaling to initiate as the person simultaneously arches their lower back expanding the stomach, separating the knees and turning the hands palm up. Initiate exhalation while simultaneously bringing the knees together, turning the palms face down on the thighs and rolling the pelvic back slightly rounding the lower back. Do the movements smoothly while keeping the legs and shoulders relaxed.
Flooded by emotions. Although very rare, at times when the person allows the abdomen to relax, they may experience by the emotions from a past trauma as the habitual bracing patterns are relaxed.
Suggested solutions and recommendations. Validate these emotions for the person. Explain that this is a normal process that may occur if past trauma has occurred. Clients who have had past trauma often experience hypervigilance, which may interfere with the relaxation response that occurs during more optimal states of breathing. Transitioning to a more optimal rest state may be uncomfortable for a person who has experienced trauma because it reduces hypervigilance. This can feel uncomfortable as hypervigilance in these cases serves a protective role, even if it is an illusory feeling of protection from future harm. Since persistent hypervigilance can interfere with the relaxation response, the benefits of allowing a relaxation response to occur through slower breathing should be highlighted. Grounding techniques as described by Peper et al (2024a) can be useful to become centered.
3. Strategies to generalize the effortless breathing into daily life.
Generalizing the skill occurs after having mastered diaphragmatic breathing in different positions (sitting, standing, lying down, and while performing tasks). It is important to remember that our breathing patterns are conditioned with our behavior. Become aware how breathing affects cognitions and emotions and how emotions and cognitions affects breathing. The following are some strategies that may facilitate learning and generalizing the slower breathing skills.
Observing how our behavior affects our breathing: Anything that may evoke the alarm or defense reaction tends to cause the person gasp and/or hold their breath. For example, when a person is sitting peacefully, make an unexpected noise behind their back or movement in their periphery of vision. In most cases they will gasp or hold their breath. Usually, they are unaware of this process unless they are asked what happened to their breathing. The major reason for the breath holding is that the stimuli triggers an alarm/defense reaction and when we hold our breath our hearing is more acute (we can hear approaching danger earlier). The problem is that we give this response when there is no actual, immediate or present threat.
Experiential practice. Sit comfortably. Now as quickly as possible without rotating the head, look with your eyes to the extreme right and then left and back and forth as if trying to identify danger at the periphery. Do this for a few eye movements. Almost everyone holds their breath when doing this exercise. For generalizing the skill, ask the person to observe during the day situations in which they hold their breath, ask them if it was necessary and encourage them to start diaphragmatic breathing.
Observing how breathing affects our thoughts and emotions. Breathing patterns are intrinsically linked to our emotions and thoughts as illustrated in the many language phrases such as sigh of relief, full of hot air, waiting with bated breath. At the same time, our breathing patterns also affect our thoughts. For instance, when we breathe shallowly and more rapidly, we can induce feelings of fear or anxiety. If we gasp, we can experience thought stopping.
Experiential practices: Incomplete exhalation: Observe what happens when you exhale less than you inhale. Begin by exhaling only 70% of the air you inhaled, then inhale and exhale again only 70% of the air you just inhaled continue this for 30 seconds. Many people will experience the onset of anxiety symptoms, lightheadedness, dizziness, neck and shoulder tension, etc. (Peper & MacHose, 1993). If you experience symptoms during this exercise and you have experienced these symptoms in the past, it is likely that unknowingly breathing in a dysfunctional pattern could have evoked them. Therefore, practicing effortless breathing may interrupt and reduce the symptoms. Do this practice while observing the person carefully and immediately interrupt and distract the person if they start feeling dizzy, too anxious, or trigger the beginning of a panic attack or PTSD symptoms.
Experiential practice: Gasp or sniff-hold sniff. Observe what happens when you are performing a cognitive task and you rapidly gasp or do sniff-hold-sniff again before exhaling. Begin by sequentially subtracting mentally, the number 7 from 146 (e.g., 146, 139, 132….). Do this as rapidly as possible and do not make a mistake. While doing the subtracting, take a rapid gasp (such as one is triggered by surprise or fear), alternatively, take a quick sniff through your nose, hold your breath and take another sniff on top of the first one, then exhale. Whereas subtrating numbers is a skill most adults can perform, the ‘time pressure’ along with the direction to avoid mistakes may be the ‘immediate’ source of strain. Whether it was the time pressure, the direction to avoid mistakes or the direction to gasp, observe what happened to your thinking process. In almost all cases, your higher-order thoughts (doing the sequential subtraction under time pressure while gasping) have disappeared, replaced by the immediate thoughts of ‘performance anxiety.’
If you blank out on exams or experience anxiety, gasping and breath holding may be one of the factors that increases symptoms and affects your performance. If you are aware that you are holding your breath or gasped, use that as the cue to shift to slow diaphragmatic breathing and you may find that your performance improves. Therefore, observe when and where you were blanking out, gasping and/or holding your breathing then substitute slow, effortless diaphragmatic breathing.
How to develop awareness and interrupting of dysfunctional breathing response. Most participants are unaware of their somatic responses until symptoms occur. Being aware of the initiation of a somatic response may assist you in identifying triggers and interrupting the developing process. A significant component of the training is symptom prescription rehearsal.
Symptom prescription is a practice in which the participant simulates/acts out the psychophysiological pattern associated with their symptoms. They amplify the body pattern until they feel the onset of the actual symptoms. The moment the person feels the beginning of the symptom, they stop the practice and initiate slow breathing and relaxation. After practicing the symptom rehearsal, they are instructed to become aware of the onset of the symptom and then use that signal to trigger the effortless breathing while looking up and shifting the body into an upright sitting position (Peper et al., 2019). Gasping and breath holding are normal responses to unexpected stimuli; however, they may trigger sympathetic activation even when there is no actual danger.
Experiential practice: Developing awareness on neck and shoulder tension:
Sit comfortably and practice effortless breathing for a minute. Take a fearful gasp and observe what happens in your body (e.g., slight neck and upper chest tension, light headedness, slight radiating pain into the eye, etc.). Shift back to effortless breathing until all symptoms /sensations have disappeared.
- Now gasp with less effort and observe the first sensations, use the awareness of first sensations to trigger the effortless breathing and continue to breathe until symptoms have disappeared
- Continue this practice. Reduce the gasping effort each time.
- After having developed the initial somatic sensation then during the day observe what triggers this response and immediately shift to slower diaphragmatic breathing. After you have shifted to effortless breathing, reflect on the trigger. Was it necessary to react? If yes, explore strategies to resolve the issue.
The same process can be done to assist with desensitization to painful memories or stressful events. Each time the person becomes aware of their somatic reaction to an evoked memory or stressful event, they shift to effortless diaphragmatic breathing. If they find that it is difficult to interrupt the emotional memories and it triggers more and more negative thoughts and associations, use the sniff-hold-sniff technique and follow that with box-breathing or any of the other quick somatic rescue techniques (Peper et al., 2024a). Box-breathing in this context could include a brief breath-holding. A typical box-breathing technique is to breath in for a count of four, hold for a count of four, breath out for a count of four, then breath in again for a count of four, continuing the figurative 4-4-4-4 count of breathing.
Practice slower diaphragmatic breathing during the day. Implement effortless diaphragmatic breathing through regeneration and interrupting the stress response.
- Support regeneration. Each day set aside 10 to 20 minutes to practice slow effortless diaphragmatic breathing at about 6-breaths-per-minute. In the beginning 10 to 20 minutes may be too long, thus in some cases have the person practice a few times a day for two minutes and slowly build up to 10 or more minutes. The practice is not just a mechanical process of breathing it includes mindfulness training. Namely, as you are breathing each time you exhale imagine a flow doing down your arms and legs and as you inhale an energy coming into you. Whenever your attention drifts bring it back to the breathing.
- Integrate breathing with daily activities. Practice slower breather before eating, after putting the seat belt on in the car, or whenever a notification pops up on the cell phone.
- Set reminders and alarms on your phone to check how you are feeling and breathing. Leave notes on nearby furniture such as a nightstand, on the shower door, and/or on the kitchen table as reminders to be mindful of your breath. If stressed or breathing shallowly, take a moment to breathe slowly.
- Interrupt the stress response. During the day when you are aware that you shallow breathe, are holding your breath, feel anxious, experience neck and shoulder tightness, or worry and use that as a cue to shift position by sitting or standing more erect, looking upward and take a few slow diaphragmatic breaths.
- Use cue condition to facilitate this process. Each time you begin the practice smell a specific aroma or do some behavioral movement and then do the breathing. After a while the aroma or behavioral movement will become the classically conditioned cue to trigger the effortless breathing.
- Use role rehearsal and conditioning to generalize the skill. Generalizing the skills often takes more time than what may be expected. In a culture where instant relief is expected— implied message associated with medication— self-mastery techniques are different and challenging as they take time to master the skill and implement them during daily life. The process of mastery is similar to learning to play a musical instrument or sports. Learning to play the violin requires practice as well as practice with failures along the way until one is ready for more challenging musical pieces, recitals, or performances.
A useful strategy to implement the learning is role rehearsal in the office, at home at work, and in real life. It is usually much easier to practice these skills in a safe space such as your own room or, with a therapist compared to with other people or, at work. To generalize the skill most efficiently, it can be helpful to practice in a safe environment while imagining being in the actual stressful location This process is illustrated by the strategy to reduce social anxiety and menstrual cramps.
Social anxiety when seeing my supervisor. Master effortless breathing in a safe environment. Role rehearsal in imagery. If you observed that you held your breath when your supervisor is around, begin with imagery when your supervisor is not present. Sit, comfortably. Let go of muscle tension and breathe effortlessly, evoking a scenario where your supervisor is walking by and continue to breathe slowly as you imagine the scene. Role rehearsal in action. Ask another person to role-play your supervisor. Sit, comfortably. Let go of muscle tension and breathe effortlessly. Have this person walk into the room in a similar way that your supervisor would. Imagine that person is your supervisor while practicing your effortless breathing. Repeat until the effortless breathing is more automatic. Practice many times in real life. Whenever the rehearsed situation occurs, implement slower paced breathing.
Menstrual cramps that causes most women to curl up and breathe shallowly when experiencing menstrual cramps (Peper et al., 2023). Master effortless breathing in a safe environment. Practice breathing lying down. While lying down, breathe diaphragmatically by having a three-to-five-pound weight such as a bag of rice or hot water pad on your abdomen. If you have a partner, have the person stroke your legs from the abdomen to your toes while you exhale. Role rehearse experiencing pain and then practice lower diaphragmatic breathing. Namely, tighten your abdomen as if you have discomfort, then focus on relaxing the buttocks and sensing the air flowing down your legs and out your feet as you exhale. Practice in real life. A few days before you expected menstruation, practice slow diaphragmatic breathing several times for at least 5-10 minutes during the day. When your menstruation starts practice the slower and lower breathing while imagining the air flowing down the abdomen, through the legs and out the feet.
Summary/Conclusion
Breathing is the mind-body bridge. It usually occurs without awareness and breathing changes affect our thought, emotions and body. Mastering and implementing slower breathing during the day takes time and practice. By observing when breathing patterns change, participants may identify internal and external factors that affect breathing which provides an opportunity to implement effortless diaphragmatic breathing to optimize health as well as resolve some of the triggers. As one 20-year-old, female student reported,
The biggest benefit from learning diaphragmatic breathing was that it gave me the feeling of safety in many moments. My anxiety tended to make me feel unsafe in many situations but homing in and mastering diaphragmatic breathing helped tremendously. I shifted from constant chest breathing to acknowledging it and in turn, reminding myself to breathe with my diaphragm.
References
Allen, R. (2024). The health benefits of nose breathing. Nursing in General Practice. http://hdl.handle.net/10147/559021
Al-Rabia, M.W. (2016). Food-induced immunoglobulin E-mediated allergic rhinitis. J Microsc Ultrastruct, 4(2), 69-75. https://doi.org/doi.org/10.1016/j.jmau.2015.11.004
Anziani, M. & Peper, E. (2021). Healing from paralysis-Music (toning) to activate health. Peperperspective –ideas on illness, health and well-being from Erik Peper. Accessed April 16, 2024. https://peperperspective.com/2021/11/22/healing-from-paralysis-music-toning-to-activate-health/
Banushi, B., Brendle, M., Ragnhildstveit, A., Murphy, T., Moore, C., Egberts, J., & Robison, R. (2023). Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sci. 13(2), 256. https://doi.org/10.3390/brainsci13020256
Chung, A.H., Gevirtz, R.N., Gharbo, R.S. et al. (2021).Pilot Study on Reducing Symptoms of Anxiety with a Heart Rate Variability Biofeedback Wearable and Remote Stress Management Coach. Appl Psychophysiol Biofeedback 46, 347–358. https://doi.org/10.1007/s10484-021-09519-x
Cohen, D. & Leung, A.K.Y. (2009). The hard embodiment of culture. European Journal of Social Psychology, 9, 1278–1289 https://doi.org/10.1002/ejsp.671
Codrons, E., Bernardi, N. F., Vandoni, M., & Bernardi, L. (2014). Spontaneous group synchronization of movements and respiratory rhythms. PloS one, 9(9), e107538. https://doi.org/10.1371/journal.pone.0107538
Dick, T. E., Mims, J. R., Hsieh, Y. H., Morris, K. F., & Wehrwein, E. A. (2014). Increased cardio-respiratory coupling evoked by slow deep breathing can persist in normal humans. Respiratory physiology & neurobiology, 204, 99-111. https://doil.org/10.1016/j.resp.2014.09.013
Ekerholt, K. & Bergland, A. (2008). Breathing: A sign of life and a unique area for reflection and action. Physical therapy, 88(7), 832-840. https://doi.org/10.2522/ptj.20070316
Elstad, M., O’Callaghan, E. L., Smith, A. J., Ben-Tal, A., & Ramchandra, R. (2018). Cardiorespiratory interactions in humans and animals: rhythms for life. American Journal of Physiology-Heart and Circulatory Physiology, 315(1), H6-H17. https://doi.org/10.1152/ajpheart.00701.2017
Folgering, H. (1999). The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis, 54(4), 365-72. https://pubmed.ncbi.nlm.nih.gov/10546483/
Gilbert, C. (1998). Emotional sources of dysfunctional breathing. Journal of bodywork and movement therapies, 2(4), 224-23. https://doi.org/10.1016/S1360-8592(98)80019-3
Jerath, R., Beveridge, C., & Barnes, V.A. (2019). Self-Regulation of Breathing as an Adjunctive Treatment of Insomnia. Front Psychiatry, 9(780). https://doi.org/10.3389/fpsyt.2018.00780
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Kang, K.W., Jung, S.I., Lee, do Y., Kim, K., & Lee, N.K. (2016) Effect of sitting posture on respiratory function while using a smartphone. J Phys Ther Sci, 28(5), 1496-8. https://doi.org/10.1589/jpts.28.1496
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lehrer, P.M. & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Front Psychol. 5, 756. https://doi.org/10.3389/fpsyg.2014.00756
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
Luthe, W. (1979). About the Methods of Autogenic Therapy. In: Peper, E., Ancoli, S., Quinn, M. (eds). Mind/Body Integration. Springer, Boston, MA. https://doi.org/10.1007/978-1-4613-2898-8_12
Luthe, W. & Schultz, J. H. (1970). Autogenic therapy: Medical applications. New York: Grune and Stratton. https://www.amazon.com/Autogenic-Therapy-II-Medical-Applications/dp/B001J9W7L6
MacHose, M., & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Magnon. V., Dutheil, F., & Vallet, G.T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 11(1),19267. https://doi.org/10.1038/s41598-021-98736-9
Maric, V., Ramanathan, D., & Mishra, J. (2020). Respiratory regulation & interactions with neuro-cognitive circuitry. Neuroscience & Biobehavioral Reviews, 112, 95-106. https://doi.org/10.1016/j.neubiorev.2020.02.001
Matić, Z., Platiša, M. M., Kalauzi, A., & Bojić, T. (2020). Slow 0.1 Hz breathing and body posture induced perturbations of RRI and respiratory signal complexity and cardiorespiratory coupling. Frontiers in physiology, 11, 24. https://doi.org/10.3389/fphys.2020.00024
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Meehan, Z.M. & Shaffer, F. (2023). Adding Core Muscle Contraction to Wrist-Ankle Rhythmical Skeletal Muscle Tension Increases Respiratory Sinus Arrhythmia and Low-Frequency Power. Appl Psychophysiol Biofeedback. 48(1), 127-134. https://doi.org/10.1007/s10484-022-09568-w
McKeown, P. (2021). The breathing cure: Develop new habits for a healthier, happier, and longer life. Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E. & Cohen, T. (2017). Inhale to Breathe Away Pelvic Floor Pain and Enjoy Intercourse. Biofeedback, 45 (1), 21–24. https://doi.org/10.5298/1081-5937-45.1.04
Peper, E., Gilbert, C.D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173-179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153-169. https://doi.org/10.15540/nr.6.3.153
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07 or https://www.researchgate.net/publication/383151816_WHAT_ABOUT_THIS_Increase_Attention_Concentration_and_School_Performance_with_Posture_Feedback
Peper, E. & MacHose, M. (1993). Symptom prescription: Inducing anxiety by 70% exhalation. Applied Psychophysiology and Biofeedback, 18(3), 133-138. https://doi.org/10.1007/BF00999790
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback. 45(4), 83–87. https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Oded, Y., & Harvey, R. (2024a). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019a). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128-133. https://doi.org/10.15540/nr.6.3.12
Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512
PTI. (2023 August 3). Often suck your stomach in to look slimmer in pictures? It can lead to ‘hourglass syndrome.’ The Economic Times Panache. Accessed March 26, 2024. https://economictimes.indiatimes.com/magazines/panache/often-suck-your-stomach-in-to-look-slimmer-in-pictures-it-can-lead-to-hourglass-syndrome/articleshow/102392681.cms?from=mdr
Salah, H.M., Goldberg, L.R., Molinger, J., Felker, G.M., Applefeld, W., Rassaf, T., Tedford, R.J., Mirro, M., Cleland, J.GF., & Fudim, M. (2022). Diaphragmatic Function in Cardiovascular Disease: JACC Review Topic of the Week, Journal of the American College of Cardiology, 80(17), 1647-1659. https://doi.org/10.1016/j.jacc.2022.08.760
Shaffer, F. & Meehan, Z.M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience,14. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.570400
Steffen, P.R., Austin, T., DeBarros, A., & Brown, T. (2017). The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood. Front Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
Taub, E., Uswatte, G., Mark, V. W., Morris, D. M. (2006). The learned nonuse phenomenon: Implications for rehabilitation. Europa Medicophysica, 42(3), 241-256. https://pubmed.ncbi.nlm.nih.gov/17039223/
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Xiao, M., Zi-Qi, Y., Gong, Z.Q., Zhang, H., Duan, N.Y., Shi, Y.T,, Wei, G.X., Li, Y.F. (2017).The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front Psychol. 8(874). https://doi.org/10.3389/fpsyg.2017.00874
Cellphones affects social communication, vision, breathing, and health: What to do!
Posted: September 4, 2024 Filed under: ADHD, attention, behavior, Breathing/respiration, cellphone, computer, digital devices, educationj, ergonomics, health, laptops, Neck and shoulder discomfort, posture, screen fatigue, self-healing, stress management, techstress, Uncategorized, vision, zoom fatigue | Tags: communication, myopia, pedestrian deaths, peripheral vision, text neck 7 CommentsAdapted from: Peper, E. & Harvey, R. (2024). Cell phones affects social communication, vision, breathing, and mental and physical health: What to do! TownsendLetter-The Examiner of Alternative Medicine,September 15, 2024. https://townsendletter.com/smartphone-affects-social-communication-vision-breathing-and-mental-and-physical-health-what-to-do/

Abstract
Smartphones are an indispensable part of our lives. Unfortunately too much of a ‘good thing’ regarding technology can work against us, leading to overuse, which in turn influences physical, mental and emotional development among current ‘Generation Z’ and ‘Millennial’ users (e.g., born 1997-2012, and 1981-1996, respectively). Compared to older technology users, Generation Z report more mental and physical health problems. Categories of mental health include attentional deficits, feelings of depression, anxiety social isolation and even suicidal thoughts, as along with physical health complaints such as sore neck and shoulders, eyestrain and increase in myopia. Long duration of looking downward at a smartphone affects not only eyestrain and posture but it also affects breathing which burden overall health. The article provides evidence and practices so show how technology over use and slouching posture may cause a decrease in social interactions and increases in emotional/mental and physical health symptoms such as eyestrain, myopia, and body aches and pains. Suggestions and strategies are provided for reversing the deleterious effects of slouched posture and shallow breathing to promote health.
We are part of an uncontrolled social experiment
We, as technology users, are all part of a social experiment in which companies examine which technologies and content increase profits for their investors (Mason, Zamparo, Marini, & Ameen, 2022). Unlike University research investigations which have a duty to warn of risks associated with their projects, we as participants in ‘profit-focused’ experiments are seldom fully and transparently informed of the physical, behavioral and psychological risks (Abbasi, Jagaveeran, Goh, & Tariq, 2021; Bhargava, & Velasquez, 2021). During university research participants must be told in plain language about the risks associated with the project (Huh-Yoo & Rader, 2020; Resnik, 2021). In contrast for-profit technology companies make it possible to hurriedly ‘click through’ terms-of-service and end-user-license-agreements, ‘giving away’ our rights to privacy, then selling our information to the highest bidder (Crain, 2021; Fainmesser, Galeotti, & Momot, 2023; Quach et al., 2022; Yang, 2022).
Although some people remain ignorant and or indifferent (e.g., “I don’t know and I don’t care”) about the use of our ‘data,’ an unintended consequence of becoming ‘dependent’ on technology overuse includes the strain on our mental and physical health (Abusamak, Jaber & Alrawashdeh, 2022; Padney et al., 2020). We have adapted new technologies and patterns of information input without asking the extent to which there were negative side effects (Akulwar-Tajane, Parmar, Naik & Shah, 2020; Elsayed, 2021). As modern employment shifted from predominantly blue-collar physical labor to white collar information processing jobs, people began sitting more throughout the day. Workers tended to look down to read and type. ‘Immobilized’ sitting for hours of time has increased as people spend time working on a computer/laptop and looking down at smartphones (Park, Kim & Lee, 2020). The average person now sits in a mostly immobilized posture 10.4 hours/day and modern adolescents spent more than two thirds of their waking time sitting and often looking down at their smartphones (Blodgett, et al., 2024; Arundell et al., 2019).
Smartphones are an indispensable part of our lives and is changing the physical and mental emotional development especially of Generation Z who were born between 1997-2012 (Haidt, 2024). They are the social media and smartphone natives (Childers & Boatwright, 2021). The smartphone is their personal computer and the gateway to communication including texting, searching, video chats, social media (Hernandez-de-Menendez, Escobar Díaz, & Morales-Menendez, 2020; Nichols, 2020; Schenarts, 2020; Szymkowiak et al., 2021). It has 100,000 times the processing power of the computer used to land the first astronauts on the moon on July 20, 1969 according to University of Nottingham’s computer scientist Graham Kendal (Dockrill, 2020). More than one half of US teens spend on the average more than 7 hours on daily screen time that includes watching streaming videos, gaming, social media and texting and their attention span has decreased from 150 seconds in 2004 to an average of 44 seconds in 2021 (Duarte, F., 2023; Mark, 2022, p. 96).
For Generation Z, social media use is done predominantly with smartphones while looking down. It has increased mental health problems such as attentional deficits, depression, anxiety suicidal thoughts, social isolation as well as decreased physical health (Haidt, 2024; Braghieri et al., 2023; Orsolini, Longo & Volpe, 2023; Satılmış, Cengız, & Güngörmüş, 2023; Muchacka-Cymerman, 2022; Fiebert, Kistner, Gissendanner & DaSilva, 2021; Mohan et al., 2021; Goodwin et al., 2020).
The shift in communication from synchronous (face-to-face) to asynchronous (texting) has transformed communications and mental health as it allows communication while being insulated from the other’s reactions (Lewis, 2024). The digital connection instead of face-to-face connection by looking down at the smart phone also has decreased the opportunity connect with other people and create new social connections, with three typical hypotheses examining the extent to which digital technologies (a) displace/ replace; (b) compete/ interfere with; and/or, (c) complement/ enhance in-person activities and relationships (Kushlev & Leitao, 2020).
As described in detail by Jonathan Haidt (2024), in his book, The Anxious Generation, the smartphone and the addictive nature of social media combined with the reduction in exercise, unsupervised play and childhood independence was been identified as the major factors in the decrease in mental health in your people (Gupta, 2023). This article focuses less on distraction such as attentional deficits, or dependency leading to tolerance, withdrawal and cravings (e.g., addiction-like symptoms) and focuses more on ‘dysregulation’ of body awareness (posture and breathing changes) and social communication while people are engaged with technology (Nawaz,Bhowmik, Linden & Mitchell, 2024).
The excessive use of the smartphones is associated with a significant reduction of physical activity and movement leading to a so-called sedentarism or increases of sitting disease (Chandrasekaran & Ganesan, 2021; Nakshine, Thute, Khatib, & Sarkar, 2022). Unbeknown to the smartphone users their posture changes, as they looks down at their screen, may also affect their mental and physical health (Aliberti, Invernizzi, Scurati & D’lsanto, 2020).
(1) Explore how looking at your smartphone affects you (adapted from: Peper, Harvey, & Rosegard, 2024)
For a minute, sit in your normal slouched position and look at your smartphone while intensely reading the text or searching social media. For the next minute sit tall and bring the cell phone in front of you so you can look straight ahead at it. Again, look at your smartphone while intensely reading the text or searching social media.
Compare how the posture affects you. Most likely, your experience is similar to the findings from students in a classroom observational study. Almost all experienced a reduction in peripheral awareness and breathed more shallowly when they slouched while looking at their cellphone.
Decreased peripheral awareness and increased shallow breathing that affects physical and mental health and performance. The students reported looking down position reduces the opportunity of creating new social connections. Looking down my also increases the risk for depression along with reduced cognitive performance during class (Peper et al., 2017; Peper et al., 2018).
(2) Explore how posture affects eye contact (adapted from the exercise shared by Ronald Swatzyna, 2023)[2]
Walk around your neighborhood or through campus either looking downwards or straight ahead for 30 minutes while counting the number of eye contacts you make.
Most likely, when looking straight ahead and around versus slouched and looking down you had the same experience as Ronald Swatzyna (2023), Licensed Clinical Social Worker. He observed that when he walked a three-mile loop around the park in a poor posture with shoulders forward in a head down position, and then reversed direction and walked in good posture with the shoulders back and the head level, he would make about five times as many eye contacts with a good posture compared to the poor posture.
Anecdotal observations, often repeated by many educators, suggest before the omnipresent smartphone, students would look around and talk to each other before a university class began. Now, when Generation Z students enter an in-person class, they sit down, look down at their phone and tend not to interact with other students.
(3) Experience the effect of face-to-face in-person communication
During the first class meeting, ask students to put their cellphones away, meet with three or four other students for a few minutes, and share a positive experience that happened to them last week as well as what they would like to learn in the class. After a few minutes, ask them to report how their energy and mood changed.
In our observational class study with 24 junior and senior college students in the in-person class and 54 students in the online zoom class, almost all report that that their energy and positive mood increased after they interacted with each other. The effects were more beneficial for the in-person small group sharing than the online breakout groups sharing on Zoom as shown in Figure 1.

Figure 1. Change in subjective energy and mood after sharing experiences synchronously in small groups either in-person or online.
Without direction of a guided exercise to increase social connections, students tend to stay within their ‘smartphone bubble’ while looking down (Bochicchio et al., 2022). As a result, they appear to be more challenged to meet and interact with other people face-to-face or by phone as is reflected in the survey data that Generation Z is dating much less and more lonely than the previous generations (Cox et al., 2023).
What to do:
- Put the smartphone away so that you do not see it in social settings such as during meals or classes. This means that other people can be present with you and the activity of eating or learning.
- Do not permit smartphones in the classroom including universities unless it is required for a class assignment.
- In classrooms and in the corporate world, create activities that demands face-to-face synchronous communication.
- Unplug from the audio programs when walking and explore with your eyes what is going on around you.
(4) Looking down increases risk of injury and death
Looking down at a close screen reduces peripheral awareness and there by increases the risk of accidents and pedestrian deaths. Pedestrian deaths are up 69% since 2011 (Cova, 2024) and have consistently increased since the introduction of the iPhone in 2007 as shown in Figure 3.

Figure 3. Increase in pedestrian death since the introduction of the iphone (data plotted from https://www.iihs.org/topics/fatality-statistics/detail/pedestrians)
In addition, the increase use of mobile phones is also associated with hand and wrist pain from overuse and with serious injuries such as falls and texting while driving due to lack of peripheral awareness. McLaughlin et al (2023) reports an increase in hand and wrist injuries as well serious injuries related to distracted behaviors, such as falls and texting while driving. The highest phone related injuries (lacerations) as reported from the 2011 to 2020 emergency room visits were people in the age range from 11–20 years followed by 21–30 years.
What to do:
- Do not walk while looking at your smartphone. Attend to the environment around you.
- Unplug from the audio podcasts when walking and explore with your eyes what is going on around you.
- Sit or stop walking when answering the smartphone to reduce the probability of an accident.
- For more pragmatic suggestions, see the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics, by Peper, Harvey and Faass (2020).
(5) Looking at screens increases the risk of myopia
Looking at a near screen for long periods of time increases the risk of myopia (near sightedness) which means that distant vision is more blurry. Myopia has increased as children predominantly use computers or, smartphones with smaller screen at shorter distances. By predominantly focusing on nearby screens without allowing the eye to relax remodels the eyes structure. Consequently, myopia has increase in the U.S. from 25 percent in the early 1970s to nearly 42 percent three decades later (OHSU, 2022).
Looking only at nearby screens, our eyes converge and the ciliary muscles around the lens contract and remain contracted until the person looks at the far distance. The less opportunity there is to allow the eyes to look at distant vision, the more myopia occurs. in Singapore 80 per cent of young people aged 18 or below have nearsightedness and 20 % of the young people have high myopia as compared to 10 years ago (Singapore National Eye Centre, 2024). The increase in myopia is a significant concern since high myopia is associated with an increased risk of vision loss due to cataract, glaucoma, and myopic macular degeneration (MMD). MMD is rapidly increasing and one of the leading causes of blindness in East Asia that has one of the highest myopia rates in the world (Sankaridurg et al., 2021).
What to do:
- Every 20 minutes stop looking at the screen and look at the far distance to relax the eyes for 20 seconds.
- Do not allow young children access to cellphones or screens. Let them explore and play in nature where they naturally alternate looking at far and near objects.
- Implement the guided eye regenerating practices descrubed in the article, Resolve eyestrain and screen fatigue, by Peper (2021).
- Read Meir Schneider’s (2016) book, Vision for Life, for suggestions how to maintain and improve vision.
(6) Looking down increases tech neck discomfort
Looking down at the phone while standing or sitting strains the neck and shoulder muscles because of the prolonged forward head posture as illustrated in the YouTube video, Tech Stress Symptoms and Causes (DeWitt, 2018). Using a smartphone while standing or walking causes a significant increase in thoracic kyphosis and trunk (Betsch et al., 2021). When the head is erect, the muscle of the neck balance a weight of about 10 to 12 pounds or, approximately 5 kilograms; however, when the head is forward at 60 degrees looking at your cell phone the forces on the muscles are about 60 pound or more than 25 kilograms, as illustrated in Figure 4 (Hansraj, 2014).

Figure 4. The head forward position puts as much as sixty pounds of pressure on the neck muscles and spine (by permission from Dr. Kenneth Hansraj, 2014).
This process is graphically illustrated in the YouTube video, Text Neck Symptoms and Causes Video, produced by Veritas Health (2020).
What to do:
- Keep the phone in front of you so that you do not slouch down by having your elbow support on the table.
- Every ten minutes stretch, look up and roll your shoulders backwards.
- Wear a posture feedback device such as the UpRight Go 2 to remind you when you slouch to change posture and activity (Peper et al., 2019; Stuart, Godfrey & Mancini, 2022).
- Take Alexander Technique lessons to improve your posture (Cacciatore, Johnson, & Cohen, 2020; AmAT, 2024; STAT, 2024).
(7) Looking down increases negative memory recall and depression
In our previous research, Peper et al. (2017) have found that recalling hopeless, helpless, powerless, and defeated memories is easier when sitting in a slouched position than in an upright position. Recalling positive memories is much easier when sitting upright and looking slightly upward than sitting slouched position. If attempting to recall positive memories the brain has to work hard as indicated by an significantly higher amplitudes of beta2, beta3, and beta4 EEG (i.e., electroencephalograph) when sitting slouched then when sitting upright (Tsai et al., 2016).
Not only does the postural position affect memory recall, it also affects mental math under time-pressure performance. When students sit in a slouched position, they report that is much more difficult to do mental math (serial 7ths) than when in the upright position (Peper et al., 2018). The effect of posture is most powerful for the 70% of students who reported that they blanked out on exams, were anxious, or worried about class performance or math. For the 30% who reported no performance anxiety, posture had no significant effect. When students become aware of slouching thought posture feedback and then interrupt their slouching by sitting up, they report an increase in concentration, attention and school performance (Peper et al., 2024).
How we move and walk also affects our subjective energy. In most cases, when people sit for a long time, they report feeling more fatigue; however, if participants interrupt sitting with short movement practices they report becoming less fatigue and improved cognition (Wennberg et al., 2016). The change in subjective energy and mood depends upon the type of movement practice. Peper & Lin (2012) reported that when students were asked to walk in a slow slouching pattern looking down versus to walk quickly while skipping and looking up, they reported that skipping significantly increased their subjective energy and mood while the slouch walking decreased their energy. More importantly, student who had reported that they felt depressed during the last two years had their energy decrease significantly more when walking very slowly while slouched than those who did not report experiencing depression. Regardless of their self-reported history of depression, when students skipped, they all reported an increase in energy (Peper & Lin, 2012; Miragall et al., 2020).
What to do:
- Walk with a quick step while looking up and around.
- Wear a posture feedback device such as the UpRight Go 2 to remind you when you slouch to change posture and activity (Peper et al., 2019; Roggio et al., 2021).
- When sitting put a small pillow in the mid back so that you can sit more erect (for more suggestions, see the article by Peper et al., 2017a, Posture and mood: Implications and applications to therapy).
- Place photo and other objects that you like to look a slightly higher on your wall so that you automatically look up.
(8) Shallow breathing increases the risk for anxiety
When slouching we automatically tend to breathe slightly faster and more shallowly. This breathing pattern increases the risk for anxiety since it tends to decrease pCO2 (Feinstein et al., 2022; Meuret, Rosenfield, Millard & Ritz, 2023; Paulus, 2013; Smits et al., 2022; Van den Bergh et al., 2013). Sitting slouched also tends to inhibit abdominal expansion during the inhalation because the waist is constricted by clothing or a belt –sometimes labeled as ‘designer jean syndrome’ and may increase abdominal symptoms such as acid reflux and irritable bowel symptoms (Engeln & Zola, 2021; Peper et al., 2016; Peper et al., 2020). When students learn diaphragmatic breathing and practice diaphragmatic breathing whenever they shallow breathe or hold their breath, they report a significant decrease in anxiety, abdominal symptoms and even menstrual cramps (Haghighat et al., 2020; Peper et al., 2022; Peper et al., 2023).
What to do:
- Loosen your belt and waist constriction when sitting so that the abdomen can expand.
- Learn and practice effortless diaphragmatic breathing to reduce anxiety.
Conclusion
There are many topics related to postural health and technology overuse that were addressed in this article. Some topics are beyond the scope of the article, and therefore seen as limitations. These relate to diagnosis and treatment of attentional deficits, or dependency leading to tolerance, withdrawal and cravings (e.g., addiction-like symptoms), or of modeling relationships between factors that contribute to the increasing epidemic of mental and physical illness associated with smartphone use and social media, such as hypotheses examining the extent to which digital technologies (a) displace/ replace; (b) compete/ interfere with; and/or, (c) complement/ enhance in-person activities and relationships. Typical pharmaceutical ‘treat-the-symptom’ approaches for addressing ‘tech stress’ related to technology overuse includes prescribing ‘anxiolytics, pain-killers and muscle relaxants’ (Kazeminasab et al., 2022; Kim, Seo, Abdi, & Huh, 2020). Although not usually included in diagnosis and treatment strategies, suggesting improving posture and breathing practices can significantly affect mental and physical health. By changing posture and breathing patterns, individuals may have the option to optimize their health and well-being.
See the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics by Erik Peper, Richard Harvey and Nancy Faass. Available from: https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/

Explore the following blogs for more background and useful suggestions
References
Abbasi, G. A., Jagaveeran, M., Goh, Y. N., & Tariq, B. (2021). The impact of type of content use on smartphone addiction and academic performance: Physical activity as moderator. Technology in Society, 64, 101521. https://doi.org/10.1016/j.techsoc.2020.101521
Abusamak, M., Jaber, H. M., & Alrawashdeh, H. M. (2022). The effect of lockdown due to the COVID-19 pandemic on digital eye strain symptoms among the general population: a cross-sectional survey. Frontiers in Public Health, 10, 895517. https://doi.org/10.3389/fpubh.2022.895517
Akulwar-Tajane, I., Parmar, K. K., Naik, P. H., & Shah, A. V. (2020). Rethinking screen time during COVID-19: impact on psychological well-being in physiotherapy students. Int J Clin Exp Med Res, 4(4), 201-216. https://doi.org/10.26855/ijcemr.2020.10.014
Aliberti, S., Invernizzi, P. L., Scurati, R., & D’Isanto, T. (2020). Posture and skeletal muscle disorders of the neck due to the use of smartphones. Journal of Human Sport and Exercise , 15 (3proc), S586-S598. https://www.jhse.ua.es/article/view/2020-v15-n3-proc-posture-skeletal-muscle-disorders-neck-smartpho; https://air.unimi.it/retrieve/handle/2434/774436/1588570/HSE%20-%20Posture%20and%20skeletal%20muscle%20disorders.pdf
AmSAT. (2024). American Society for the Alexander Technique. Accessed July 27, 2024. https://alexandertechniqueusa.org/
Arundell, L., Salmon, J., Koorts, H. et al. (2019). Exploring when and how adolescents sit: cross-sectional analysis of activPAL-measured patterns of daily sitting time, bouts and breaks. BMC Public Health 19, 653. https://doi.org/10.1186/s12889-019-6960-5
Bhargava, V. R., & Velasquez, M. (2021). Ethics of the attention economy: The problem of social media addiction. Business Ethics Quarterly, 31(3), 321-359. https://doi.org/10.1017/beq.2020.32
Betsch, M., Kalbhen, K., Michalik, R., Schenker, H., Gatz, M., Quack, V., Siebers, H., Wild, M., & Migliorini, F. (2021). The influence of smartphone use on spinal posture – A laboratory study. Gait Posture, 85, 298-303. https://doi.org/10.1016/j.gaitpost.2021.02.018
Blodgett, J.M., Ahmadi, M.N., Atkin, A.J., Chastin, S., Chan, H-W., Suorsa, K., Bakker, E.A., Hettiarcachchi, P., Johansson, P.J., Sherar,L. B., Rangul, V., Pulsford, R.M…. (2024). ProPASS Collaboration , Device-measured physical activity and cardiometabolic health: the Prospective Physical Activity, Sitting, and Sleep (ProPASS) consortium, European Heart Journal, 45(6) 458–471, https://doi.org/10.1093/eurheartj/ehad717
Bochicchio, V., Keith, K., Montero, I., Scandurra, C., & Winsler, A. (2022). Digital media inhibit self-regulatory private speech use in preschool children: The “digital bubble effect”. Cognitive Development, 62, 101180. https://doi.org/10.1016/j.cogdev.2022.101180
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Cacciatore, T. W., Johnson, P. M., & Cohen, R. G. (2020). Potential mechanisms of the Alexander technique: Toward a comprehensive neurophysiological model. Kinesiology Review, 9(3), 199-213. https://doi.org/10.1123/kr.2020-0026
Chandrasekaran, B., & Ganesan, T. B. (2021). Sedentarism and chronic disease risk in COVID 19 lockdown–a scoping review. Scottish Medical Journal, 66(1), 3-10. https://doi.org/10.1177/0036933020946336
Childers, C., & Boatwright, B. (2021). Do digital natives recognize digital influence? Generational differences and understanding of social media influencers. Journal of Current Issues & Research in Advertising, 42(4), 425-442. https://doi.org/10.1080/10641734.2020.1830893
Cox, D.A., Hammond, K.E., & Gray, K. (2023). Generation Z and the Transformation of American Adolescence: How Gen Z’s Formative Experiences Shape Its Politics, Priorities, and Future. Survey Center of American Life, November 23, 2023. Accessed July 4, 2024. https://www.americansurveycenter.org/research/generation-z-and-the-transformation-of-american-adolescence-how-gen-zs-formative-experiences-shape-its-politics-priorities-and-future/
Crain, M. (2021). Profit over privacy: How surveillance advertising conquered the internet. U of Minnesota Press. https://www.amazon.com/Profit-over-Privacy-Surveillance-Advertising/dp/1517905044
Cova, E. (2024). Pedestrian fatalities at historic high. Smart Growth America (data from U.S. Department of Transportation (USDOT). Accessed July 2, 2024. https://smartgrowthamerica.org/pedestrian-fatalities-at-historic-high/
Duarte, F. (2023). Average Screen Time for Teens (2024). Exploding Topics. Accessed July 5, 2024. https://explodingtopics.com/blog/screen-time-for-teens#average
DeWitt, D. (2018). How Does Text Neck Cause Pain? Spine-Health October 26, 2018. Accessed July 5, 2024. https://www.spine-health.com/conditions/neck-pain/how-does-text-neck-cause-pain
Dockrill, P. (2020). Your laptop charger is more powerful than Apollo11’s computer, says apple developer. Science Alert, Janural 12, 2020. Accessed July 4, 2024. https://www.sciencealert.com/apollo-11-s-computer-was-less-powerful-than-a-usb-c-charger-programmer-discovers
Elsayed, W. (2021). Covid-19 pandemic and its impact on increasing the risks of children’s addiction to electronic games from a social work perspective. Heliyon, 7(12). https://doi.org/10.1016/j.heliyon.2021.e08503
Engeln, R., & Zola, A. (2021). These boots weren’t made for walking: gendered discrepancies in wearing painful, restricting, or distracting clothing. Sex roles, 85(7), 463-480. https://doi.org/10.1007/s11199-021-01230-9
Fainmesser, I. P., Galeotti, A., & Momot, R. (2023). Digital privacy. Management Science, 69(6), 3157-3173. https://doi.org/10.1287/mnsc.2022.4513
Feinstein, J. S., Gould, D., & Khalsa, S. S. (2022). Amygdala-driven apnea and the chemoreceptive origin of anxiety. Biological psychology, 170, 108305. https://10.1016/j.biopsycho.2022.108305
Fiebert, I., Kistner, F., Gissendanner, C., & DaSilva, C. (2021). Text neck: An adverse postural phenomenon. Work, 69(4), 1261-1270. https://doi.org/10.3233/WOR-213547
Goodwin, R. D., Weinberger, A. H., Kim, J. H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. Journal of Psychiatric Research. 130, 441–446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Gupta, N. (2023). Impact of smartphone overuse on health and well-being: review and recommendations for life-technology balance. Journal of Applied Sciences and Clinical Practice, 4(1), 4-12. https://doi.org/10.4103/jascp.jascp_40_22
Haghighat, F., Moradi, R., Rezaie, M., Yarahmadi, N., & Ghaffarnejad, F. (2020). Added Value of Diaphragm Myofascial Release on Forward Head Posture and Chest Expansion in Patients with Neck Pain: A Randomized Controlled Trial. Research Square. https://doi.org/10.21203/rs.3.rs-53279/v1
Haidt, J. (2024). The Anxious generation: How the great rewiring of childhood is causing an epidemic of mental illness. New York: Penguin Press. https://www.anxiousgeneration.com/book
Hansraj, K.K. (2014). Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 25, 277-279. https://pubmed.ncbi.nlm.nih.gov/25393825/
Hernandez-de-Menendez, M., Escobar Díaz, C. A., & Morales-Menendez, R. (2020). Educational experiences with Generation Z. International Journal on Interactive Design and Manufacturing (IJIDeM), 14(3), 847-859. https://doi.org/10.1007/s12008-020-00674-9
Huh-Yoo, J., & Rader, E. (2020). It’s the Wild, Wild West: Lessons learned from IRB members’ risk perceptions toward digital research data. Proceedings of the ACM on Human-Computer Interaction, 4(CSCW1), 1-22. https://doi.org/10.1145/3392868
IIHS (2024). Fatality Facts 2022Pedestrians. The Insurance Institute for Highway Safety (IIHS). Accessed July 2, 2024. https://www.iihs.org/topics/fatality-statistics/detail/pedestrians
Kazeminasab, S., Nejadghaderi, S. A., Amiri, P., Pourfathi, H., Araj-Khodaei, M., Sullman, M. J., … & Safiri, S. (2022). Neck pain: global epidemiology, trends and risk factors. BMC musculoskeletal disorders, 23, 1-13. https://doi.org/10.1186/s12891-021-04957-4
Kim, K. H., Seo, H. J., Abdi, S., & Huh, B. (2020). All about pain pharmacology: what pain physicians should know. The Korean journal of pain, 33(2), 108-120. https://doi.org/10.3344/kjp.2020.33.2.108
Kushlev, K., & Leitao, M. R. (2020). The effects of smartphones on well-being: Theoretical integration and research agenda. Current opinion in psychology, 36, 77-82. https://doi.org/10.1016/j.copsyc.2020.05.001
Lewis, H.R. (2024). Mechanical intelligence and counterfeit humanity. Harvard Magazine, 126(6), 38-40. https://www.harvardmagazine.com/2024/07/harry-lewis-computers-humanity#google_vignette
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press. https://www.amazon.com/Attention-Span-Finding-Fighting-Distraction-ebook/dp/B09XBJ29W9
Mason, M. C., Zamparo, G., Marini, A., & Ameen, N. (2022). Glued to your phone? Generation Z’s smartphone addiction and online compulsive buying. Computers in Human Behavior, 136, 107404. https://doi.org/10.1016/j.chb.2022.107404
McLaughlin, W.M., Cravez, E., Caruana, D.L., Wilhelm, C., Modrak, M., & Gardner, E.C. (2023). An Epidemiological Study of Cell Phone-Related Injuries of the Hand and Wrist Reported in United States Emergency Departments From 2011 to 2020. J Hand Surg Glob, 5(2),184-188. https://doi.org/10.1016/j.jhsg.2022.11.009
Meuret, A. E., Rosenfield, D., Millard, M. M., & Ritz, T. (2023). Biofeedback Training to Increase Pco2 in Asthma With Elevated Anxiety: A One-Stop Treatment of Both Conditions?. Psychosomatic medicine, 85(5), 440-448. https://doi.org/10.1097/PSY.0000000000001188
Miragall, M., Borrego, A., Cebolla, A., Etchemendy, E., Navarro-Siurana, J., Llorens, R., … & Baños, R. M. (2020). Effect of an upright (vs. stooped) posture on interpretation bias, imagery, and emotions. Journal of Behavior Therapy and Experimental Psychiatry, 68, 101560. https://doi.org/10.1016/j.jbtep.2020.101560
Mohan, A., Sen, P., Shah, C., Jain, E., & Jain, S. (2021). Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1). Indian journal of ophthalmology, 69(1), 140-144. https://doi.org/10.4103/ijo.IJO_2535_20
Muchacka-Cymerman, A. (2022). ‘I wonder why sometimes I feel so angry’ The associations between academic burnout, Facebook intrusion, phubbing, and aggressive behaviours during pandemic Covid 19. Polish Psychological Bulletin, 53(4). https://doi.org/10.24425/ppb.2022.143376
Nakshine, V. S., Thute, P., Khatib, M. N., & Sarkar, B. (2022). Increased screen time as a cause of declining physical, psychological health, and sleep patterns: a literary review. Cureus, 14(10). https://doi.org/10.7759/cureus.30051
Nawaz, S., Bhowmik, J., Linden, T., & Mitchell, M. (2024). Validation of a modified problematic use of mobile phones scale to examine problematic smartphone use and dependence. Heliyon, 10(2). https://doi.org/10.1016/j.heliyon.2024.e24832
Nicholas, A. J. (2020). Preferred learning methods of generation Z. Faculty and Staff – Articles & Papers. Digital Commons @ Salve Regina. Salve Regina University. https://digitalcommons.salve.edu/fac_staff_pub/74
OHSU. (2022). Myopia on the rise, especially among children. Casey Eye Institute. Oregan Health and Science University. Accessed July 7, 2024. https://www.ohsu.edu/casey-eye-institute/myopia-rise-especially-among-children
Orsolini, L., Longo, G., & Volpe, U. (2023). The mediatory role of the boredom and loneliness dimensions in the development of problematic internet use. International Journal of Environmental Research and Public Health, 20(5), 4446. https://doi.org/10.3390/ijerph20054446
Pandey, R., Gaur, S., Kumar, R., Kotwal, N., & Kumar, S. (2020). Curse of the technology-computer related musculoskeletal disorders and vision syndrome: a study. International Journal of Research in Medical Sciences, 8(2), 661. https://doi.org/10.18203/2320-6012.ijrms20200253
Park, J. C., Kim, S., & Lee, H. (2020). Effect of work-related smartphone use after work on job burnout: Moderating effect of social support and organizational politics. Computers in human behavior, 105, 106194. https://doi.org/10.1016/j.chb.2019.106194
Paulus, M.P. (2013). The breathing conundrum-interoceptive sensitivity and anxiety. Depress Anxiety.30(4), 315-20. https://doi.org/10.1002/da.22076
Peper, E. (2021). Resolve eyestrain and screen fatigue. Well Being Journal, 30(1), 24-28. https://wellbeingjournal.com/resolve-eyestrain-and-screen-fatigue/
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://doi.org/10.5298/1081-5937-44.1.03
Peper, E., Chen, S., Heinz, N. & Harvey, R. (2023). Hope for menstrual cramps (dysmenorrhea) with breathing. Biofeedback, 51(2), 44–51. https://doi.org/10.5298/1081-5937-51.2.04
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C. (2022). Reduce anxiety. NeuroRegulation, 9(2), 91–97. https://doi.org/10.15540/nr.9.2.91
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Mason, L. (2019). “Don’t slouch!” Improve health with posture feedback. Townsend Letter-The Examiner of Alternative Medicine, 436, 58-61. https://www.researchgate.net/publication/337424599_Don%27t_slouch_Improve_health_with_posture_feedback
Peper, E., Harvey, R., Mason, L., & Lin, I.-M. (2018). Do better in math: How your body posture may change stereotype threat response. NeuroRegulation, 5(2), 67–74. http://dx.doi.org/10.15540/nr.5.2.67
Peper, E., Harvey, R. & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2). https://doi.org/10.5298/1081-5937-52.02.07
Peper, E. & Lin, I-M. (2012). Increase or decrease depression-How body postures influence your energy level. Biofeedback, 40 (3), 126-130. https://doi.org/10.5298/1081-5937-40.3.01
Peper, E., Lin, I-M, & Harvey, R. (2017a). Posture and mood: Implications and applications to therapy. Biofeedback, 35(2), 42-48. https://doi.org/10.5298/1081-5937-45.2.03
Peper, E., Lin, I-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45 (2), 36-41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44-47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Quach, S., Thaichon, P., Martin, K. D., Weaven, S., & Palmatier, R. W. (2022). Digital technologies: tensions in privacy and data. Journal of the Academy of Marketing Science, 50(6), 1299-1323. https://doi.org/10.1007/s11747-022-00845-y
Resnik, D. B. (2021). Standards of evidence for institutional review board decision-making. Accountability in research, 28(7), 428-455. https://doi.org/10.1080/08989621.2020.1855149
Roggio, F., Ravalli, S., Maugeri, G., Bianco, A., Palma, A., Di Rosa, M., & Musumeci, G. (2021). Technological advancements in the analysis of human motion and posture management through digital devices. World journal of orthopedics, 12(7), 467. https://doi.org/10.5312/wjo.v12.i7.467
Sankaridurg, P., Tahhan, N., Kandel, H., Naduvilath, T., Zou, H., Frick,K.D., Marmamula, S., Friedman, D.S., Lamoureux, e. Keeffe, J. Walline, J.J., Fricke, T.R., Kovai, V., & Resnikoff, S. (2021) IMI Impact of Myopia. Invest. Ophthalmol. Vis. Sci, 62(5), 2. https://doi.org/10.1167/iovs.62.5.2
Satılmış, S. E., Cengız, R., & Güngörmüş, H. A. (2023). The relationship between university students’ perception of boredom in leisure time and internet addiction during social isolation process. Bağımlılık Dergisi, 24(2), 164-173. https://doi.org/10.51982/bagimli.1137559
Schenarts, P. J. (2020). Now arriving: surgical trainees from generation Z. Journal of surgical education, 77(2), 246-253. https://doi.org/10.1016/j.jsurg.2019.09.004
Schneider, M. (2016). Vision for life. Ten Steps to Natural Eyesight Improvement. Berkeley: North Atlantic books. https://www.amazon.com/Vision-Life-Revised-Eyesight-Improvement/dp/1623170087
Singapore National Eye Centre. (2024). Severe myopia cases among children in Singapore almost doubled in past decade. CAN. Accessed July 4, 2024. https://www.channelnewsasia.com/singapore/myopia-children-cases-almost-double-glasses-eye-checks-4250266
Smits, J. A., Monfils, M. H., Otto, M. W., Telch, M. J., Shumake, J., Feinstein, J. S., … & Exposure Therapy Consortium. (2022). CO2 reactivity as a biomarker of exposure-based therapy non-response: study protocol. BMC psychiatry, 22(1), 831. https://doi.org/10.1186/s12888-022-04478-x
STAT (2024). The society of teachers of the Alexander Technique. Assessed July 27, 2024. https://alexandertechnique.co.uk/
Stuart, S., Godfrey, A., & Mancini, M. (2022). Staying UpRight in Parkinson’s disease: A pilot study of a novel wearable postural intervention. Gait & Posture, 91, 86-93. https://doi.org/10.1016/j.gaitpost.2021.09.202
Swatzyna, R. (2023). Personal communications.
Szymkowiak, A., Melović, B., Dabić, M., Jeganathan, K., & Kundi, G. S. (2021). Information technology and Gen Z: The role of teachers, the internet, and technology in the education of young people. Technology in Society, 65, 101565. https://doi.org/10.1016/j.techsoc.2021.101565
Tsai, H. Y., Peper, E., & Lin, I. M.*(2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23-27. https://doi.org/10.15540/nr.3.1.23
Van den Bergh, O., Zaman, J., Bresseleers, J., Verhamme, P., Van Diest, I. (2013). Anxiety, pCO2 and cerebral blood flow, International Journal of Psychophysiology, 89 (1), 72-77. https://doi.org/10.1016/j.ijpsycho.2013.05.011
Veritas Health. (2020). Text Neck Symptoms and Causes Video. YouTube video, accessed August 29, 2024. https://www.spine-health.com/conditions/neck-pain/how-does-text-neck-cause-pain?source=YT
Wennberg, P., Boraxbekk, C., Wheeler, M., et al. (2016). Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open, 6, e009630. https://doi.org/10.1136/bmjopen-2015-009630
Yang, K. H. (2022). Selling consumer data for profit: Optimal market-segmentation design and its consequences. American Economic Review, 112(4), 1364-1393. https://www.aeaweb.org/articles/pdf/doi/10.1257/aer.20210616
[1] Correspondence should be addressed to: Erik Peper, Ph.D., Institute for Holistic Health Studies, Department of Recreation, Parks, Tourism and Holistic Health, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 Email: epeper@sfsu.edu; web: www.biofeedbackhealth.org; blog: www.peperperspective.com
[2] I thank Ronald Swatzyna (2023), Licensed Clinical Social Worker for sharing this exercise with me. He discovered that a difference in the number of eye contacts depending how he walked. When he walked a 3.1 mile loop around the park in a poor posture- shoulders forward, head down position- and then reversed direction and walked in good posture with the shoulders back and the head level, that that he make about 5 times as many eye contacts with good posture compared to the poor posture. He observed that he make about five times as many eye contacts with good posture as compared to the poor posture.
Increase attention, concentration and school performance
Posted: August 15, 2024 Filed under: ADHD, attention, behavior, Breathing/respiration, digital devices, education, ergonomics, posture, screen fatigue, stress management, vision, zoom fatigue | Tags: cellphone, concentration 5 CommentsReproduced from: Peper, E., Harvey, R., & Rosegard, E. (2024). Increase attention, concentration and school performance with posture feedback. Biofeedback, 52(2), 48-52. https://doi.org/10.5298/1081-5937-52.02.07

When I sit with good posture on my computer, I am significantly more engaged in what I’m doing. When I slouch on my computer I tend to procrastinate, go on my phone, and get distracted so it ends up taking much longer to do my work when my posture is bad.…I have ADHD and I struggle a lot with my mind wandering when I should be paying attention. Having good posture really helps me to lock in and focus.—22 year old male student.
Over the past two decades, there has been a significant increase in the prevalence of attention-deficit/hyperactivity disorder (ADHD), anxiety, and depression. ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18–25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020). Students are more distracted, stressed and exhausted (Hanscom, 2022; Hoyt et al., 2021). The more students are distracted, the lower their academic achievement (Feng et al., 2019). In our recent class survey of more than 100 junior and senior college students on the first day of class, 54% reported that they were tired and dreading the day when they woke up. When you are tired and stressed it is difficult to focus attention and have clarity of thought. Their self-report is similar to the mental health trends in the United States by age group in 2008–2019. Mental health of young people has significantly deteriorated over the last 15 years (Braghieri et al., 2021/2023).
The increase in psychological distress is most prevalent in people ages 18–29 and who were brought up with the cellphone (the iPhone was introduced in 2007) and social media. Now when students enter a class, they tend to sit down, look down at their cellphone while slouching, and they do not make contact with most other students unless instructed or reminded by the instructor. When instructed to talk to another student for less than 5 minutes (e.g., share something positive that happened to you this week), 93% of the students reported an increase in subjective energy and alertness (Peper, 2024).
As a group, students are social media and cell phone natives and thus have many distractions and stimuli to which they continuously respond. It is not surprising that the average attention span has decreased from 150 seconds in 2004 to 44 seconds in 2021 (Mark, 2023). More importantly, they now tend to sit in a slouched collapsed position, which facilitates access to hopeless, helpless, powerless and defeated thoughts and memories (Tsai et al., 2016; Peper et al., 2017) and reduces cognitive performance when performing mental math (Peper et al., 2018). Sitting slouched and looking down also reduces peripheral awareness and increases shallow thoracic breathing—a breathing pattern that increases the risk of anxiety. Experience this yourself.
For a minute, look at your cellphone while intensely reading the text or searching social media in the following two positions: sitting straight up and looking straight ahead at your cell phone or slouching and looking down at your cell phone, as shown in Figure 1. Most likely, your experience is similar to the findings from the classroom observational study in which half the students looked down and the other half looked straight ahead and then reversed their positions (Peper, unpublished). They then compared the subjective experience associated with the position. In the slouched position, most experienced a reduction in peripheral awareness and breathed more shallowly (see Figure 1).

Figure 1. Effect of slouching or looking straight ahead on vision and breathing.
The slouched position reduces social awareness and decreases awareness of external stimuli as illustrated in Steve Cutts’ superb animation, Mobile world (https://www.youtube.com/watch?v=wUW1wjlKvmY).
Given the constant stimulation, distractions and shortened attention span, it is more challenging to be calm and have clarity of mind when having to study or take an exam at school. As educators, we constantly explore ways to engage students and support their learning and especially share quick skills they can use to optimize performance (Peper& Wilson, 2021). In previous research, Harvey et al., 2020 showed that students who used posture feedback improved their health scores compared to the control group. The purpose of this paper is to share a 4-week class assignment by which numerous students reported an increase in attention, concentration, confidence, school performance and a decrease in stress.
Participants: 18 undergraduate students (7 males and 11 females, average age 22 [STDEV 2.2]) enrolled in an upper division class. As a report about an effort to improve the quality of a classroom activity, this report of findings was exempted from Institutional Review Board oversight.
Equipment: Wearable posture feedback device, UpRight Go 2, which the person wears on their neck and which provides vibratory feedback whenever they slouch, as shown in Figure 2. It is used in conjunction with the cellphone app that allows them to calibrate the feedback device.

Figure 2. Attachment of posture feedback device on neck or spine and the app to calibrate the device.
Procedure: Students attended the 3-hour weekly class that explored autogenic training, somatic awareness, psychobiology of stress, the role of posture, and the psychophysiology of respiration. The lectures included short experiential practices demonstrating the body-mind connections such as imagining a lemon to increase salivation, the effect of slouched versus erect posture on evoking positive/empowering or hopeless/helpless/powerless/defeated thoughts, and the effect of sequential 70% exhalation for 30 seconds on increasing anxiety (Tsai et al., 2016; Peper et al., 2017).
Each week for 4 weeks the students were assigned a self-practice that they would implement daily at home and record their experiences. At the end of the week, they reviewed their own log and summarized their own observations (benefits, difficulties). During the next class session, they met in small groups of 5 to 6 students to discuss their experiences and extract common themes.
The 4-week curriculum was sequenced as follows:
Week 1
- Lecture on the benefits/harms of posture with experiential practices (effect of slouching vs erect on access to hopeless/helpless/powerless thoughts versus optimistic and empowering thoughts; posture and arm strength (Peper, 2022).
- Homework assignments:
- Watch the great Ted Talk and one of the most viewed by Amy Cuddy (2013), “Your body language shapes who you are.”
- Keep a detailed log to monitor situations where they slouched and identify situations that were associated with slouching.
Week 2
- Lecture on psychophysiology and class discussion in which students shared their experiences of slouching; namely, what were the triggers, how it affected them and what they could do to change.
- Demonstration, explanation, and how to use the posture feedback device, UpRight Go 2.
- Homework assignment: Wear UpRight Go 2 during the day, use it in different settings (studying, walking, work), and keep a log. When it vibrates (slouching) observe what was going on and change your behavior such as when tired>get rest or do exercise; when depressed>change internal language; ergonomic issues>change the environment, posture>give yourself lower back support.
Week 3
- Class discussion on what to do when slouching is triggered by tiredness, negative and hopeless thoughts, ergonomics such as laptop placement and chair. Students meet in groups to share their experiences and what they did in response to the vibratory feedback.
- Homework assignment: Continue to wear the UpRight Go 2 during the day and keep a log.
Week 4
- Class discussion in groups of five students about their experiences of slouching, what to do and how it affects them.
- Homework assignment: Wear UpRight Go 2 during the day and keep a log. Submit a paper that describes their experience with the posture feedback from the UpRight Go 2 and fill out a short anonymous survey in which they rated their change in experience since using the posture feedback device on a scale from 3 (worse) to 0 (no change) to 3 (better) .
Results
All students reported that wearing the feedback device increased attention and concentration as shown in Figure 3.

Figure 3.
Amount of time using the UpRight Go 2:On the average the students used the device 4.8 days a week (STDEV 2.0) and 2.2 hours per day (STDEV 1.3).
Location of use:Although most students practiced sitting in front of their computer, they also reported using it while at work, playing pool or doing yoga and even while seeing a therapist.
Discussion
All the students reported that the posture feedback helped them to become more aware of slouching and when they then interrupted their slouching, they experienced an increase in energy and a decrease in stress. As a 21-year-old male student said: “I felt more engaged with whatever I was doing. I tend to … daydream and get distracted, but I experience much less of that when I sit with good posture.”
Many reported that it helped identify their emotions when they were feeling overwhelmed. Then they could sit up, shift their perspective, and many reported a decrease in back and neck pain as well as a decrease in tiredness. When participants wear non-invasive wearables that provide accurate feedback, they are often surprised what triggers are associated with feedback or how their performance improves when they respond to the feedback signal by changing their thoughts and behavior. This posture self-awareness project should be embedded in strategies that optimize the learning state as described by Peper & Wilson (2021).
To the students’ surprise, they were often unaware that they started to slouch, nor were they aware of how much this slouching was connected to their emotions, mental state or external factors. For example, one student reported that he wore the device while being in a therapy session. All of a sudden, it vibrated. At that moment, he realized that he was becoming anxious, although he and therapist were unaware. He then shared what happened with the therapist, and that helped the therapeutic process.
The benefits may not only be due to posture change but that the students became aware and interrupted their habitual pattern. This process is similar to that described by Charles Stroebel (1985) when he taught patients the Quieting Reflect that reduced numerous somatic symptoms ranging from headaches to hypertension.
The posture feedback intervention is both simple and challenging since it requires the participants to wear the device, identify factors that trigger the slouching, and interrupt their automatic patterns by changing posture and behavior whenever they felt the vibratory feedback. The awareness gave them the opportunity to change posture and thoughts. By shifting to an upright posture, they experienced that they could concentrate more and have increased energy. As a 19-year-old female student wrote: “My breathing was better and sitting in an upright position gave me more energy when doing tasks.”
Conclusion
We recommend that a 4-week home practice module that incorporates wearable posture feedback is offered to all students to enhance their well-being. With the posture feedback, participants can increase their awareness of slouching, identify situations that trigger slouch, and learn strategies to shift their posture, thoughts, emotions and external environment to optimize maintaining an empowered position. As a 20-year old male student reported, “The app helped me when I was feeling overwhelmed and then I would sit up. When I had it on, I did a lot of work. I was more concentrated.”
Explore the following blogs for more background and useful suggestions
References
Braghieri, L., Levy, R., & Makarin, A. (2023). Media and mental health (July 28, 2022). SSRN. (Original work published 2021). https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Centers for Disease Control and Prevention. (n.d.). ADHD through the years. Attention-Deficit / Hyperactivity Disorder (ADHD). Retrieved March 27, 2023, from https://www.cdc.gov/ncbddd/adhd/timeline.html
Cuddy, A. (2012) Your body language may shape who you are. TED Talk. Retrieved March 16, 2024 from https://www.youtube.com/watch?v=Ks-_Mh1QhMc
Feng, S., Wong, Y. K., Wong, L. Y., & Hossain, L. (2019). The internet and Facebook usage on academic distraction of college students, Computers & Education, 134, 41-49. https://doi.org/10.1016/j
Goodwin, R. D., Weinberger, A. H., Kim, J. H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. Journal of Psychiatric Research. 130, 441–446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hanscom, N. (2022). Students, staff notice higher levels of student distraction this school year, reflect on potential causes. Retrieved September 28, 2023, from https://dgnomega.org/13162/feature/students-staff-notice-higher-levels-of-student-distraction-this-school-year-reflect-on-potential-causes/
Harvey, R., Peper, E., Mason, L., & Joy, M. (2020). Effect of posture feedback training on health. Applied Psychophysiology and Biofeedback, 45(1), 59–65. https://doi.org/10.1007/s10484-020-09457-0
Hoyt, L. T., Cohen, A. K., Dull, B., Castro, E. M., & Yazdani, N. (2021). “Constant stress has become the new normal”: Stress and anxiety inequalities among U.S. college students in the time of COVID-19. Journal of Adolescent Health. 68(2), 270–276. https://doi.org/10.1016/j.jadohealth.2020.10.030
Mark, G. (2023). Attention span: A groundbreaking way to restore balance, happiness and productivity. Hanover Square Press.
Peper, E. (2022, March 4). A breath of fresh air: Breathing and posture to optimize health. [Conference presentation at the 2nd Virtual Ergonomics Summit], Krista Burns, PhD. https://www.youtube.com/watch?v=PhV7Ulhs38s
Peper, E. (2024a). Change in energy and alertness after talking with each other versus looking at cellphone. Data collected from HH380 class fall 2023. Unpublished.
Peper, E. (2024b). Changes in vision and breathing when looking down or straight ahead at the cellphone. Data collected from HH380 class, Spring, 2024, San Francisco State University. Unpublished.
Peper, E., Harvey, R., Mason, L., & Lin, I.-M. (2018). Do better in math: How your body posture may change stereotype threat response. NeuroRegulation, 5(2), 67–74. http://dx.doi.org/10.15540/nr.5.2.67
Peper, E., Lin, I.-M., Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback.45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 49(2), 46-49. https://doi.org/10.5298/1081-5937-49-2-04
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-Quieting-Charles-M-D-Stroebel/dp/0399126570
Tsai, H. Y., Peper, E., & Lin, I.-M.(2016). EEG patterns under positive/negative body postures and emotion recall tasks. NeuroRegulation, 3(1), 23–27. https://doi.org/10.15540/nr.3.1.23
Grandmother Therapy: A Common-Sense Approach to Health and Wellness
Posted: July 24, 2024 Filed under: ADHD, attention, behavior, education, Evolutionary perspective, Exercise/movement, Nutrition/diet, Pain/discomfort, relaxation, self-healing | Tags: anxiety, depression, epilepsy, exhaustion, grandmother therapy, health, insomnia, life style change, mental-health, therapy 1 CommentErik Peper, PhD and Angelika Sadar, MA

In today’s fast-paced world, college students and young adults often struggle with various health issues. From anxiety and depression to ADHD and epilepsy, these challenges can significantly impact their daily lives. But what if the solution to many of these problems lies in something as simple as “Grandmother Therapy”?
What is Grandmother Therapy? Grandmother Therapy is all about going back to basics and establishing healthy lifestyle habits. It’s the common-sense approach that our grandmothers might have suggested: regular sleep patterns, balanced nutrition, increased social connections, and regular physical activity.
The Problem: Many college students:
- Skip breakfast before their first class
- Rely on fast food and sugary stimulants
- Have irregular sleep schedules
- Spend excessive time on gaming and social media
The Medical Approach: Often, the quick solution is medication:
- Depression? Take antidepressants.
- Insomnia? Use sleeping pills.
- Anxiety? Try anti-anxiety medication.
- ADHD? Prescribe Ritalin or similar drugs.
While these treatments may help manage symptoms, they often overlook the underlying lifestyle factors contributing to these issues.
The Grandmother Therapy Approach:
- Establish regular sleep patterns
- Adopt healthy eating habits
- Increase social connections
- Incorporate regular physical activity
- Reduce gaming and social media use
Case Study #1: The Power of Sleep
This illustrates the simple intervention of having a bedtime routine. A college student in a holistic health class complained that she was tired most of the time and had difficulty focusing her attention and continuously drifted off in class.
Here is her reported sleep schedule:
- last night I went to bed at 3am and woke up 7;
- the day before, I went to bed at 1pm and woke up at 6,
- two nights before, I went to bed at 4pm and woke up at 10 am.
Holistic treatment approach:
Set a sleep schedule: she was provided with information about the importance of having a regular pattern of sleep and waking. Namely, go to bed at the same time and get up 8 hours later. She agreed to do an experiment for a week to go to bed at 12 and wake up at 8m. To her surprise, she felt so much more energized and could pay attention in class during the week of the experiment.
Case Study #2: Beyond Seizures: A Holistic Approach to Treating Psychogenic Nonepileptic Seizures
This case study highlights the importance of a comprehensive, lifestyle-based approach to treating psychogenic nonepileptic seizures (PNES). It follows a 24-year-old male student initially diagnosed with intractable epilepsy, experiencing over 10 seizures per week that didn’t respond to medication.
Key points:
1. Initial misdiagnosis: Despite normal MRI and EEG results, the client was initially treated for epilepsy.
2. Limited assessment: Traditional medical evaluations focused solely on seizure descriptions and diagnostics, overlooking crucial lifestyle factors.
3. Comprehensive evaluation: A psychophysiological assessment revealed high sympathetic arousal, including rapid breathing, sweaty palms, and muscle tension.
4. Lifestyle factors: The client’s diet consisted of high-glycemic fast foods, excessive caffeine, alcohol, and daily marijuana use. He also had significant student debt and a history of abdominal surgery.
Holistic treatment approach:
– Dietary changes: Switching to unprocessed, low-glycemic foods and increasing vegetable and fruit intake
– Breathing techniques: Learning and practicing slow diaphragmatic breathing
– Stress management: Addressing underlying stressors and practicing relaxation techniques
– Supplements: Adding omega-3 and multivitamins to support brain health
Remarkable results: Within four months, the patient became seizure-free, reduced marijuana use significantly, and decreased medication dosage.
Summary
These cases underscore the potential of integrating lifestyle modifications and stress management techniques in treating attention, anxiety and even psychogenic nonepileptic seizures; offering hope for patients who don’t respond to traditional treatments alone. Before turning to medication or complex treatments, consider the power of Grandmother Therapy. By addressing fundamental lifestyle factors, we can often improve our health and well-being significantly. Remember, sometimes the most effective solutions are the simplest ones.
The Challenges of Simplicity: While Grandmother Therapy may seem straightforward, its simplicity can make it challenging to implement. It requires commitment and a willingness to change long-standing habits.
Implement many Life Style Changes at once: Recommending one change at the time is logical; however, participants will more likely experience rapid benefits and are more motivated to continue when they change multiple lifestyle factors at once.
Call to Action: Are you struggling with health issues? Try implementing some aspects of Grandmother Therapy in your life. Implement changes and see how they impact your overall well-being.
Please let us know your experience with implementing Grandmother Therapy.
See the following blogs for more background information
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods
Posted: June 30, 2024 Filed under: ADHD, attention, behavior, CBT, digital devices, education, emotions, Evolutionary perspective, health, mindfulness, neurofeedback, Nutrition/diet, Uncategorized | Tags: ADHD, anxiety, depression, diet, glyphosate, herbicide, herbicites, mental-health, neurofeedback, pesticides, supplements', ultraprocessed foods, vitamins 4 CommentsAdapted from: Peper, E. & Shuford, J. (2024). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 2- Exposure to neurotoxins and ultra-processed foods. NeuroRegulation, 11(2), 219–228. https://doi.org/10.15540/nr.11.2.219
Look at your hand and remember that every cell in your body including your brain is constructed out the foods you ingested. If you ingested inferior foods (raw materials to be built your physical structure), then the structure can only be inferior. If you use superior foods, you have the opportunity to create a superior structure which provides the opportunity for superior functioning. -Erik Peper
Summary
Mental health symptoms of attention deficit hyperactivity disorder (ADHD), Autism, anxiety and depression have increased over the last 15 years. An additional risk factor that may affect mental and physical health is the foods we eat. Even though, our food may look and even taste the same as compared to 50 years ago, it contains herbicide and pesticide residues and often consist of ultra-processed foods. These foods (low in fiber, and high in sugar, animal fats and additives) are a significant part of the American diet and correlate with higher levels of inattention and hyperactivity in children with ADHD. Due to affluent malnutrition, many children are deficient in essential vitamins and minerals. We recommend that before beginning neurofeedback and behavioral treatments, diet and lifestyle are assessed (we call this Grandmother therapy assessment). If the diet appears low in organic foods and vegetable, high in ultra-processed foods and drinks, then nutritional deficiencies should be assessed. Then the next intervention step is to reduce the nutritional deficiencies and implement diet changes from ultra-processed foods to organic whole foods. Meta-analysis demonstrates that providing supplements such as Vitamin D, etc. and reducing simple carbohydrates and sugars and eating more vegetables, fruits and healthy fats during regular meals can ameliorate the symptoms and promote health.
The previous article and blog, Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms, pointed out how the changes in bonding, screen time and circadian rhythms affected physical and mental health (Peper, 2023a; Peper, 2023b). However, there are many additional factors including genetics that may contribute to the increase is ADHD, autism, anxiety, depression, allergies and autoimmune illnesses (Swatzyna et al., 2018). Genetics contribute to the risk of attention deficit hyperactivity disorder (ADHD); since, family, twin, and adoption studies have reported that ADHD runs in families (Durukan et al., 2018; Faraone & Larsson, 2019). Genetics is in most cases a risk factor that may or may not be expressed. The concept underlying this blog is that genetics loads the gun and environment and behavior pulls the trigger as shown in Figure 1.

Figure 1. Interaction between Genetics and Environment
The pandemic only escalated trends that already was occurring. For example, Bommersbach et al (2023) analyzed the national trends in mental health-related emergency department visits among USA youth, 2011-2021. They observed that in the USA, Over the last 10 years, the proportion of pediatric ED visits for mental health reasons has approximately doubled, including a 5-fold increase in suicide-related visits. The mental health-related emergency department visits increased an average of 8% per year while suicide related visits increased 23.1% per year. Similar trends have reported by Braghieri et al (2022) from the National Survey on Drug Use and Health as shown in Figure 2.

Figure 2. Mental health trends in the United States by age group in 2008–2019. The data come from the National Survey on Drug Use and Health. Reproduced with permission from Braghieri, Luca and Levy, Ro’ee and Makarin, Alexey, Social Media and Mental Health (July 28, 2022) https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
The trends reported from this data shows an increase in mental health illnesses for young people ages 18-23 and 24-29 and no changes for the older groups which could be correlated with the release of the first iPhone 2G on June 29, 2007. Thus, the Covid 19 pandemic and social isolation were not THE CAUSE but an escalation of an ongoing trend. For the younger population, the cellphone has become the vehicle for personal communication and social connections, many young people communicate more with texting than in-person and spent hours on screens which impact sleep (Peper, 2023a). At the same time, there are many other concurrent factors that may contributed to increase of ADHD, autism, anxiety, depression, allergies and autoimmune illnesses.
Without ever signing an informed consent form, we all have participated in lifestyle and environmental changes that differ from that evolved through the process of evolutionary natural selection and promoted survival of the human species. Many of those changes in lifestyle are driven by demand for short-term corporate profits over long-term health of the population. As exemplified by the significant increase in vaping in young people as a covert strategy to increase smoking (CDC, 2023) or the marketing of ultra-processed foods (van Tulleken, 2023).
This post focusses how pesticides and herbicides (exposure to neurotoxins) and changes in our food negatively affects our health and well-being and is may be another contributor to the increase risk for developing ADHD, autism, anxiety and depression. Although our food may look and even taste the same compared to 50 years ago, it is now different–more herbicide and pesticide residues and is often ultra-processed. lt contains lower levels of nutrients and vitamins such as Vitamin C, Vitamin B2, Protein, Iron, Calcium and Phosphorus than 50 years ago (Davis et al, 2004; Fernandez-Cornejo et al., 2014). Non-organic foods as compared to organic foods may reduce longevity, fertility and survival after fasting (Chhabra et al., 2013).
Being poisoned by pesticide and herbicide residues in food
Almost all foods, except those labeled organic, are contaminated with pesticides and herbicides. The United States Department of Agriculture reported that “Pesticide use more than tripled between 1960 and 1981. Herbicide use increased more than tenfold (from 35 to 478 million pounds) as more U.S. farmers began to treat their fields with these chemicals” (Fernandez-Cornejo, et al., 2013, p 11). The increase in herbicides and pesticides is correlated with a significant deterioration of health in the United States (Swanson, et al., 2014 as illustrated in the following Figure 3.


Figure 3. Correlation between Disease Prevalence and Glyphosate Applications (reproduced with permission from Swanson et al., 2014.
Although correlation is not causation and similar relationships could be plotted by correlating consumption of ultra-refined foods, antibiotic use, decrease in physical activity, increase in computer, cellphone and social media use, etc.; nevertheless, it may suggest a causal relationship. Most pesticides and herbicides are neurotoxins and can accumulate in the person over time this could affect physical and mental health (Bjørling-Poulsen et al., 2008; Arab & Mostaflou, 2022). Even though the United States Environmental Protection Agency (EPA) has determined that the residual concentrations in foods are safe, their long-term safety has not been well established (Leoci & Ruberti, 2021). Other countries, especially those in which agribusiness has less power to affect legislation thorough lobbying, and utilize the research findings from studies not funded by agribusiness, have come to different conclusions…
For example, the USA allows much higher residues of pesticides such as, Round-Up, with a toxic ingredient glyphosate (0.7 parts per million) in foods than European countries (0.01 parts per million) (Wahab et al., 2022; EPA, 2023; European Commission, 2023) as is graphically illustrated in figure 4.

Figure 4: Percent of Crops Sprayed with Glyphosate and Allowable Glyphosate Levels in the USA versus the EU
The USA allows this higher exposure than the European Union even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbo et al., 2022). The negative effects most likely would be more harmful in a rapidly growing infant than for an adult. Most likely, some individuals are more vulnerable than others and are the “canary in mine.” They are the early indicators for possible low-level long-term harm. Research has shown that fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021). Also, organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010). We hypothesize this exposure is one of the co-factors that have contributed to the decrease in mental health of adults 18 to 29 years.
At the same time as herbicides and pesticides acreage usage has increased, ultra-processed food have become a major part of the American diet (van Tulleken, 2023). Eating a diet high in ultra-processed foods, low in fiber, high sugar, animal fats and additives has been associated with higher levels of inattention and hyperactivity in children with ADHD; namely, high consumption of sugar, candy, cola beverages, and non-cola soft drinks and low consumption of fatty fish were also associated with a higher prevalence of ADHD diagnosis (Ríos-Hernández et al., 2017).
In international studies, less nutritional eating behaviors were observed in ADHD risk group as compared to the normal group (Ryu et al., 2022). Artificial food colors and additives are also a public health issue and appear to increase the risk of hyperactive behavior (Arnold et al., 2012). In a randomized double-blinded, placebo controlled trial 3 and 8/9 year old children had an increase in hyperactive behavior for those whose diet included extra additives (McCann et al., 2007). The risk may occur during fetal development since poor prenatal maternal is a critical factor in the infants neurodevelopment and is associated with an increased probability of developing ADHD and autism (Zhong et al., 2020; Mengying et al., 2016).
Poor nutrition even affects your unborn grandchild
Poor nutrition not only affects the mother and the developing fetus through epigenetic changes, it also impacts the developing eggs in the ovary of the fetus that can become the future granddaughter (Wilson, 2015). At birth, the baby has all of her eggs. Thus, there is a scientific basis for the old wives tale that curses may skip a generation. Providing maternal support is even more important since it affects the new born and the future grandchild. The risk may even begin a generation earlier since the grandmother’s poor nutrition as well as stress causes epigenetic changes in the fetus eggs. Thus 50% of the chromosomes of the grandchild were impacted epigenetically by the mother’s and grandmother’s dietary and health status .
Highly processed foods
Highly refined foods have been processed to remove many of their nutrients. These foods includes white bread, white rice, pasta, and sugary drinks and almost all the fast foods and snacks. These foods are low in fiber, vitamins, and minerals, and they are high in sugars, unhealthy fats, and calories. In addition, additives may have been added to maximize taste and mouth feel and implicitly encourage addiction to these foods. A diet high in refined sugars and carbohydrates increases the risk of diabetes and can worsen the symptoms of ADHD, autism, depression, anxiety and increase metabolic disease and diabetes (Woo et al., 2014; Lustig, 2021; van Tulleken, 2023). Del-Ponte et al. (2019) noted that a diet high in refined sugar and saturated fat increased the risk of symptoms of ADHD, whereas a healthy diet, characterized by high consumption of fruits and vegetables, would protect against the symptoms.
Most likely, a diet of highly refined foods may cause blood sugar to spike and crash, which can lead to mood swings, irritability, anxiety, depression and cognitive decline and often labeled as “hangryness” (the combination of anger and hunger) (Gomes et al., 2023; Barr et al., 2019). At the same time a Mediterranean diet improves depression significantly more than the befriending control group (Bayles et al., 2022). In addition, refined foods are low in essential vitamins and minerals as well as fiber. Not enough fiber can slow down digestion, affect the human biome, and makes it harder for the body to absorb nutrients. This can lead to nutrient deficiencies, which can contribute to the symptoms of ADHD, autism, depression, and anxiety. Foods do impact our mental and physical health as illustrated by foods that tend to reduce depression (LaChance & Ramsey, 2018; MacInerney et al., 2017). By providing appropriate micronutrients such as minerals (Iron, Magnesium Zinc), vitamins (B6, B12, B9 and D), Omega 3s (Phosphatidylserine) and changing our diet, ADHD symptoms can be ameliorated.
Many children with ADHD, anxiety, depression are low on essential vitamins and minerals. For example, low levels of Omega-3 fatty acids and vitamin D may be caused by eating ultra-refined foods, fast foods, and drinking soft drink. At the same time, the children are sitting more in indoors in front of the screen and thereby have lower sun exposure that is necessary for the vitamin D production.
“Because of lifestyle changes and sunscreen use, about 42% of Americans are deficient in vitamin D. Among children between 1 to 11 years old, an estimated 15% have vitamin D deficiency. And researchers have found that 17% of adolescents and 32% of young adults were deficient in vitamin D.” (Porto and Abu-Alreesh, 2022).
Reduced sun exposure is even more relevant for people of color (and older people); since, their darker skin (increased melanin) protects them from ultraviolet light damage but at the same time reduces the skins production of vitamin D. Northern Europeans were aware of the link between sun exposure and vitamin D production. To prevent rickets (a disease caused by vitamin D deficiency) and reduce upper respiratory tract infections the children were given a tablespoon of cod liver oil to swallow (Linday, 2010). Cod liver oil, although not always liked by children, is more nutritious than just taking a Vitamin D supplements. It is a whole food and a rich source of vitamin A and D as well as containing a variety of Omega 3 fatty acids (eicosapentaenoic acid (EPA) (USDA, 2019).
Research studies suggest that ADHD can be ameliorated with nutrients, and herbs supplements (Henry & CNS, 2023). Table 1 summarizes some of the nutritional deficits observed and the reduction of ADHD symptoms when nutritional supplements were given (adapted from Henry, 2023; Henry & CNS, 2023).
| Nutritional deficits observed in people with ADHD | Decrease in ADHD symptoms with nutritional supplements |
| Vitamin D: In meta-analysis with a total number of 11,324 children, all eight trials reported significantly lower serum concentrations of 25(OH)D in patients diagnosed with ADHD compared to healthy controls. (Kotsi et al, 2019) | After 8 weeks children receiving vitamin D (50,000 IU/week) plus magnesium (6 mg/kg/day) showed a significant reduction in emotional problems as observed in a randomized, double blind, placebo-controlled clinical trial (Hemamy et al., 2021). |
| Iron: In meta-analysis lower serum ferritin was associated with ADHD in children (Wang et al., 2017) and the mean serum ferritin levels are lower in the children with ADHD than in the controls (Konofal et al., 2004). | After 12 weeks of supplementation with Iron (ferrous sulfate) in double-blind, randomized placebo-controlled clinical trial, clinical trials symptoms of in children with ADHD as compared to controls were reduced (Tohidi et al., 2021; Pongpitakdamrong et all, 2022). |
| Omega 3’s: Children with ADHD are more likely to be deficient in omega 3’s than children without ADHD (Chang et al., 2017). | Adding Omega-3 supplements to their diet resulted in an improvement in hyperactivity, impulsivity, learning, reading and short term memory as compared to controls in 16 randomized controlled trials including 1514 children and young adults with ADHD (Derbyshire, 2017) |
| Magnesium: In meta-analysis, subjects with ADHD had lower serum magnesium levels compared with to their healthy controls (Effatpahah et al., 2019) | 8 weeks of supplementation with Vitamin D and magnesium caused a significant decrease in children with conduct problems, social problems, and anxiety/shy scores (Hemamy et al., 2020). |
| Vitamin B2, B6, B9 and B12deficiency has been found in many patients with Attention Deficit and Hyperactivity Disorder (Landaas et al, 2016; Unal et al., 2019). | Vitamin therapy appears to reduce symptoms of ADHD and ASD (Poudineh et al., 2023; Unal et al., 2019). An 8 weeks supplementing with Vitamin B6 and magnesium decreased hyperactivity and hyperemotivity/aggressiveness. When supplementation was stopped, clinical symptoms of the disease reappeared in few weeks (Mousain-Bosc et al., 2006). |
Table 1. Examples of vitamin and mineral deficiencies associated with symptoms of ADHD and supplementation to reduction of ADHD symptoms.
Supplementation of vitamins and minerals in many cases consisted of more than one single vitamin or mineral. For an in-depth analysis and presentation, see the superb webinar by Henry & CNS (2023): https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback? (Henry & CNS, 2023).
Whole foods are more than the sum of individual parts (the identified individual constituents/nutrients). The process of digestion is much more complicated than ingesting simple foods with added vitamins or minerals. Digestion is the interaction of many food components (many of which we have not identified) which interact and affect the human biome. A simple added nutrient can help; however, eating whole organic foods it most likely be healthier. For example, whole-wheat flour is much more nutritious. Whole wheat is rich in vitamins B-1, B-3, B-5, riboflavin, folate well as fiber while refined white flour has been bleached and stripped of fiber and nutrients to which some added vitamins and iron are added.
Recommendation
When working with clients, follow Talib’s principles as outlined in Part 1 by Peper (2023) which suggests that to improve health first remove the unnatural which in this case are the ultra-processed foods, simple carbohydrates, exposure to pesticides and herbicides (Taleb, 2014). The approach is beneficial for prevention and treatment. This recommendation to optimize health is both very simple and very challenging. The simple recommendation is to eat only organic foods and as much variety as possible as recommended by Professor Michael Pollan in his books, Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules (Pollan, 2006; Pollan, 2011).
Do not eat foods that contain herbicides and pesticide residues or are ultra-processed. Although organic foods especially vegetable and fruits are often much more expensive, you have choice: You can pay more now to optimize health or pay later to treat disease. Be safe and not sorry. This recommendation is similar to the quote, “Let food be thy medicine and medicine be thy food,” that has been attributed falsely since the 1970s to Hippocrates, the Greek founder of western medicine (5th Century, BC) (Cardenas, 2013).
There are many factors that interfere with implementing these suggestions; since, numerous people live in food deserts (no easy access to healthy unprocessed foods ) or food swamps (a plethora of fast food outlets) and 54 million Americans are food insecure (Ney, 2022). In addition, we and our parents have been programmed by the food industry advertising to eat the ultra- processed foods and may no longer know how to prepare healthy foods such as exemplified by a Mediterranean diet. Recent research by Bayles et al (2022) has shown that eating a Mediterranean diet improves depression significantly more than the befriending control group. In addition, highly processed foods and snacks are omnipresent, often addictive and more economical.
Remember that clients are individuals and almost all research findings are based upon group averages. Even when the data implies that a certain intervention is highly successful, there are always some participants for whom it is very beneficial and some for whom it is ineffective or even harmful. Thus, interventions need to be individualized for which there is usually only very limited data. In most cases, the original studies did not identify the characteristics of those who were highly successful or those who were unsuccessful. In addition, when working with specific individuals with ADHD, anxiety, depression, etc. there are multiple possible causes.
Before beginning specific clinical treatment such as neurofeedback and/or medication, we recommend the following:
- “Grandmother assessment” that includes and assessment of screen time, physical activity, outdoor sun exposure, sleep rhythm as outlined in Part 1 by Peper (2023). Then follow-up with a dietary assessment that investigates the prevalence of organic/non organic foods, ingestion of fast foods, ultra-processed foods, soft drinks, high simple carbohydrate and sugar, salty/sugary/fatty snacks, fruits, vegetables, and eating patterns (eating with family or by themselves in front of screens). Be sure to include an assessment of emotional reactivity and frequency of irritability and “hangryness”.
- If the assessment suggest low level of organic whole foods and predominance of ultra- refined foods, it may be possible that the person is deficient in vitamins and minerals. Recommend that the child is tested for the vitamin deficiencies. If vitamin deficiencies identified, recommend to supplement the diet with the necessary vitamins and mineral and encourage eating foods that naturally include these substances (Henry & CNS, 2023). If there is a high level of emotional reactivity and “hangryness,” a possible contributing factor could be hypoglycemic rebound from a high simple carbohydrate (sugar) intake or not eating breakfast combined with hyperventilation (Engel et al., 1947; Barr et al., 2019). Recommend eliminating simple carbohydrate breakfast and fast food snacks and substitute organic foods that include complex carbohydrates, protein, fats, vegetables and fruit. Be sure to eat breakfast.
- Implement “Grandmother Therapy”. Encourage the family and child to change their diet to eating a whide variety of organic foods (vegetables, fruits, some fish, meat and possibly dairy) and eliminate simple carbohydrates and sugars. This diet will tend to reduce nutritional deficits and may eliminate the need for supplements.
- Concurrent with the stabilization of the physiology begin psychophysiological treatment strategies such as neurofeedback biofeedback and cognitive behavior therapy.
Relevant blogs
Author Disclosure
Authors have no grants, financial interests, or conflicts to disclose.
References
Arnold, L, Lofthouse, N., & Hurt, E. (2012). Artificial food colors and attention-deficit/hyperactivity symptoms: conclusions to dye for. Neurotherapeutics, 9(3), 599-609. https://doi.org/10.1007/s13311-012-0133-x
Arab, A. & Mostafalou, S. (2022). Neurotoxicity of pesticides in the context of CNS chronic diseases. International Journal of Environmental Health Research, 32(12), 2718-2755. https://doi.org/10.1080/09603123.2021.1987396
Barr, E.A., Peper, E., & Swatzyna, R.J. (2019). Slouched Posture, Sleep Deprivation, and Mood Disorders: Interconnection and Modulation by Theta Brain Waves. NeuroRegulation, 6(4), 181–189. https://doi.org/10.15540/nr.6.4.181
Bayes. J., Schloss, J., Sibbritt, D. (2022). The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND: A Mediterranean Diet in MEN with Depression” study): a randomized controlled trial. Am J Clin Nutr. 116(2), 572-580. https://doi.org/10.1093/ajcn/nqac106
Bjørling-Poulsen, M., Andersen, H.R. & Grandjean, P. Potential developmental neurotoxicity of pesticides used in Europe. Environ Health 7, 50 (2008). https://doi.org/10.1186/1476-069X-7-50
Bommersbach, T.J., McKean, A.J., Olfson, M., Rhee, T.G. (2023). National Trends in Mental Health–Related Emergency Department Visits Among Youth, 2011-2020. JAMA, 329(17):1469–1477. https://doi.org/10.1001/jama.2023.4809
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Cardenas, D. (2013). Let not thy food be confused with thy medicine: The Hippocratic misquotation. e-Spen Journal, 8(6), 3260-3262. https://doi.org/10.1016/j.clnme.2013.10.002
CDC, (2023). Quick Facts on the Risks of E-cigarettes for Kids, Teens, and Young Adults. CDC. Centers for Disease Control and Prevention. Accessed September 23, 2023. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html
Chang, J.C., Su, K.P., Mondelli, V. et al. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: a Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacol. 43, 534–545. https://doi.org/10.1038/npp.2017.160
Chhabra, R., Kolli, S., & Bauer, J.H. (2013). Organically Grown Food Provides Health Benefits to Drosophila melanogaster. PLoS ONE, 8(1): e52988. https://doi.org/10.1371/journal.pone.0052988
Davis, D. R., Epp, M. D., & Riordan, H. D. (2004). Changes in USDA food composition data for 43 garden crops, 1950 to 1999. Journal of the American College of Nutrition, 23(6), 669-682. https://doi.org/10.1080/07315724.2004.10719409
Derbyshire, E. (2017). Do Omega-3/6 Fatty Acids Have a Therapeutic Role in Children and Young People with ADHD? J Lipids. 6285218. https://doi.org/10.1155/2017/6285218
Del-Ponte, B., Quinte, G.C., Cruz, S., Grellert, M., & Santos, I. S. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): A systematic review and meta-analysis. Journal of Affective Disorders, 252, 160-173. https://doi.org/10.1016/j.jad.2019.04.061
Durukan, İ., Kara, K., Almbaideen, M., Karaman, D., & Gül, H. (2018). Alexithymia, depression and anxiety in parents of children with neurodevelopmental disorder: Comparative study of autistic disorder, pervasive developmental disorder not otherwise specified and attention deficit-hyperactivity disorder. Pediatrics International, 60(3), 247–253. https://doi.org/10.1111/ped.13510
Effatpanah, M., Rezaei, M., Effatpanah, H., Effatpanah, Z., Varkaneh, H.K., Mousavi. S.M., Fatahi, S., Rinaldi, G., & Hashemi, R. (2019). Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Res, 274, 228-234. https://doi.org/10.1016/j.psychres.2019.02.043
Engel, G.L., Ferris, E.B., & Logan, M. (1947). Hyperventilation; analysis of clinical symptomatology. Ann Intern Med, 27(5), 683-704. https://doi.org/10.7326/0003-4819-27-5-683
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians
Faraone, S.V. & Larsson, H. (2019). Genetics of attention deficit hyperactivity disorder. Mol Psychiatry, 24(4), 562-575. https://doi.org/10.1038/s41380-018-0070-0
Fernandez-Cornejo, J. Nehring, R, Osteen, C., Wechsler, S., Martin, A., & Vialou, A. (2014). Pesticide use in the U.S. Agriculture: 21 Selected Crops, 1960-2008. Economic Information Bulletin Number 123, United State Department of Agriculture. https://www.ers.usda.gov/webdocs/publications/43854/46734_eib124.pdf
Gomes, G. N., Vidal, F. N., Khandpur. N., et al. (2023). Association Between Consumption of Ultraprocessed Foods and Cognitive Decline. JAMA Neurol, 80(2),142–150. https://doi.org/10.1001/jamaneurol.2022.4397
Hemamy, M., Heidari-Beni, M., Askari, G., Karahmadi, M., & Maracy, M. (2020). Effect of Vitamin D and Magnesium Supplementation on Behavior Problems in Children with Attention-Deficit Hyperactivity Disorder. Int J Prev Med, 11(1), 4. https://doi.org/10.4103/ijpvm.IJPVM_546_17
Henry, K. (2023). An Integrative Medicine Approach to ADHD. Rupa Health. Accessed September 30, 2023. https://www.rupahealth.com/post/an-integrative-medicine-approach-to-adhd
Henry, K. & CNS, L.A. (2023). Natural treatments for ADHD. Webinar Presentation by IntegrativePractitioner.com and sponsored by Rupa Health, June 6, 2023 https://divcom-events.webex.com/recordingservice/sites/divcom-events/recording/e29cefcae6c1103bb7f3aa780efee435/playback?
Hemamy, M., Pahlavani, N., Amanollahi, A. et al. (2021). The effect of vitamin D and magnesium supplementation on the mental health status of attention-deficit hyperactive children: a randomized controlled trial. BMC Pediatr, 21, 178. https://doi.org/10.1186/s12887-021-02631-1
Konofal, E., Lecendreux, M., Arnulf, I., & Mouren, M. (2004). Iron Deficiency in Children With Attention-Deficit/Hyperactivity Disorder. Arch Pediatr Adolesc Med, 158(12), 1113–1115. https://doi.org/10.1001/archpedi.158.12.1113
Kotsi, E., Kotsi, E. & Perrea, D.N. (2019). Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): a meta-analysis. ADHD Atten Def Hyp Disord, 11, 221–232. https://doi.org/10.1007/s12402-018-0276-7
LaChance, L.R. & Ramsey, D. (2018). Antidepressant foods: An evidence-based nutrient profiling system for depression. World J Psychiatr, 8(3): 97-104. World J Psychiatr., 8(3): 97-104. https://doi.org/10.5498/wjp.v8.i3.97
Landaas, E.T., Aarsland, T.I., Ulvik, A., Halmøy, A., Ueland. P.M., & Haavik, J. (20166). Vitamin levels in adults with ADHD. BJPsych Open, 2(6), 377-384. https://doi.org/10.1192/bjpo.bp.116.003491
Linday, L.A. (2010). Cod liver oil, young children, and upper respiratory tract infections. J Am Coll Nutr, 29(6), 559-62. https://doi.org/10.1080/07315724.2010.10719894
Leoci, R. & Ruberti, M. (2021) Pesticides: An Overview of the Current Health Problems of Their Use. Journal of Geoscience and Environment Protection, 9, 1-20. https://doi.org/10.4236/gep.2021.98001
Lustig, R.H. (2021). Metaboical: The lure and the lies of processed food, nutrition, and modern medicine. New York: Harper Wave. https://www.amazon.com/Metabolical-processed-poisons-people-planet/dp/1529350077
MacInerney, E. K., Swatzyna, R. J., Roark, A. J., Gonzalez, B. C., & Kozlowski, G. P. (2017). Breakfast choices influence brainwave activity: Single case study of a 12-year-old female. NeuroRegulation, 4(1), 56–62. https://doi.org/10.15540/nr.4.1.56
McCann, D., Barrett, A., Cooper, A., Crumpler, D., Dalen, L., Grimshaw, K., et al. (2007). Food additives and hyperactive behavior in 3-year old and 8/9-year-old children in the community: a randomized, double-blinded, placebo-controlled trial. Lancet, 370(9598), 1560-1567. https://doi.org/10.1016/S0140-6736(07)61306-3
Mengying, L.I, Fallin, A, D., Riley,A., Landa, R., Walker, S.O., Silverstein, M., Caruso, D., et al. (2016). The Association of Maternal Obesity and Diabetes With Autism and Other Developmental Disabilities. Pediatrics, 137(2), e20152206. https://doi.org/10.1542/peds.2015-2206
Mousain-Bosc, M., Roche, M., Polge, A., Pradal-Prat, D., Rapin, J., & Bali, J.P. (2006). Improvement of neurobehavioral disorders in children supplemented with magnesium-vitamin B6. I. Attention deficit hyperactivity disorders. Magnes Res. 19(1), 46-52. https://pubmed.ncbi.nlm.nih.gov/16846100/#:~:text=In%20almost%20all%20cases%20of,increase%20in%20Erc%2DMg%20values.
Ney, J. (2022). Food Deserts and Inequality. Social Policy Data Lab. Updated: Jan 24, 2022. Accessed September, 23, 2023. https://www.socialpolicylab.org/post/grow-your-blog-community
Peper, E. (2023a). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. the peperperspective July 2, 2023. Accessed august 8, 2024, https://peperperspective.com/2023/07/04/reflections-on-the-increase-in-autism-adhd-anxiety-and-depression-part-1-bonding-screen-time-and-circadian-rhythms/
Peper, E. (2023b). Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation, 10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Pollan, M. (2006). Omnivore’s Dilemma: A Natural History of Four Meals and Food Rules. New York Penguin Press. https://www.amazon.com/Omnivores-Dilemma-Natural-History-Meals/dp/1594200823/ref=tmm_hrd_swatch_0?_
Pollan, M. (2011). Food rules. New York Penguin Press. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/B00VSBILFG/ref=tmm_hrd_swatch_0?
Pongpitakdamrong, A., Chirdkiatgumchai, V., Ruangdaraganon, N., Roongpraiwan, R., Sirachainan, N., Soongprasit, M., & Udomsubpayakul, U. (2022). Effect of Iron Supplementation in Children with Attention-Deficit/Hyperactivity Disorder and Iron Deficiency: A Randomized Controlled Trial. Journal of Developmental & Behavioral Pediatrics, 43(2), 80-86., https://doi.org/10.1097/DBP.0000000000000993
Porto, A. & Abu-Alreesh, S. (2022). Vitamin D for babies, children & adolescents. Health Living. Healthychildren.org. Accessed September 24, 2023. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/vitamin-d-on-the-double.aspx#
Poudineh, M., Parvin, S., Omidali, M., Nikzad, F., Mohammadyari, F., Sadeghi Poor Ranjbar, F., F., Nanbakhsh, S., & Olangian-Tehrani, S. (2023). The Effects of Vitamin Therapy on ASD and ADHD: A Narrative Review. CNS & Neurological Disorders – Drug Targets (Formerly Current Drug Targets – CNS & Neurological Disorders), (22), 5, 2023, 711-735. https://doi.org/10.2174/1871527321666220517205813
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Ríos-Hernández, A., Alda, J.A., Farran-Codina, A., Ferreira-García, E., & Izquierdo-Pulido, M. (2017). The Mediterranean Diet and ADHD in Children and Adolescents. Pediatrics, 139(2):e20162027. https://doi.org/10.1542/peds.2016-2027
Ryu, S.A., Choi, Y.J., An, H., Kwon, H.J., Ha, M., Hong, Y.C., Hong, S.J., & Hwang, H.J. (2022). Associations between Dietary Intake and Attention Deficit Hyperactivity Disorder (ADHD) Scores by Repeated Measurements in School-Age Children. Nutrients, 14(14), 2919. https://doi.org/10.3390/nu14142919
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Swanson, N.L., Leu, A., Abrahamson, J., & Wallet, B. (2014). Genetically engineered crops, glyphosate and the deterioration of health in the United States of America. Journal of Organic Systems, 9(2), 6-17. https://www.organic-systems.org/journal/92/JOS_Volume-9_Number-2_Nov_2014-Swanson-et-al.pdf
Swatzyna, R. J., Boutros, N. N., Genovese, A. C., MacInerney, E. K., Roark, A. J., & Kozlowski, G. P. (2018). Electroencephalogram (EEG) for children with autism spectrum disorder: Evidential considerations for routine screening. European Child & Adolescent Psychiatry, 28(5), 615–624. https://doi.org/10.1007/s00787-018-1225-x
Taleb, N. N. (2014). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. https://www.amazon.com/Antifragile-Things-That-Disorder-Incerto/dp/0812979680/ref=tmm_pap_swatch_0
Tohidi, S., Bidabadi, E., Khosousi, M.J., Amoukhteh, M., Kousha, M., Mashouf, P., Shahraki, T. (2021). Effects of Iron Supplementation on Attention Deficit Hyperactivity Disorder in Children Treated with Methylphenidate. Clin Psychopharmacol Neurosci, 19(4), 712-720. https://doi.org/10.9758/cpn.2021.19.4.712
Unal, D. Çelebi, F., Bildik,H.N., Koyuncu, A., & Karahan, S. (2019). Vitamin B12 and haemoglobin levels may be related with ADHD symptoms: a study in Turkish children with ADHD, Psychiatry and Clinical Psychopharmacology, 29(4), 515-519. https://doi.org/10.1080/24750573.2018.1459005
USDA. (2019). Fish oil, cod liver. FoodData Central. USDA U.S> Department of Agriculture. Published 4/1/2019. Accessed September 24, 2024. https://fdc.nal.usda.gov/fdc-app.html#/food-details/173577/nutrients
Van Tulleken, C. (2023). Ultra-Processed People. The Science Behind Food That Isn’t Food. New York: W.W. Norton & Company. https://www.amazon.com/Ultra-Processed-People-Science-Behind-Food/dp/1324036729/ref=asc_df_1324036729/?
Wahab, S., Muzammil, K., Nasir, N., Khan, M.S., Ahmad, M.F., Khalid, M., Ahmad, W., Dawria, A., Reddy, L.K.V., & Busayli, A.M. (2022). Advancement and New Trends in Analysis of Pesticide Residues in Food: A Comprehensive Review. Plants (Basel), 11(9), 1106. https://doi.org/10.3390/plants11091106
Wang. Y., Huang, L., Zhang, L., Qu, Y., & Mu, D. (2017). Iron Status in Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. PLoS One, 12(1):e0169145. https://doi.org/10.1371/journal.pone.0169145
Wilson, L. (2015). Mothers, beware: Your lifestyle choices will even affect your grandkids.
News Corp Australia Network. Accessed Jun 24, 2024. https://www.news.com.au/lifestyle/parenting/kids/mothers-beware-your-lifestyle-choices-will-even-affect-your-grandkids/news-story/3f326f457546cfb32af5c409f335fb56
Woo, H.D.,; Kim, D.W., Hong, Y.-S., Kim, Y.-M.,Seo, J.-H.,; Choe, B.M., Park, J.H.,; Kang, J.-W., Yoo, J.-H.,; Chueh, H.W., et al. (2014). Dietary Patterns in Children with Attention Deficit/Hyperactivity Disorder (ADHD). Nutrients, 6, 1539-1553. https://doi.org/10.3390/nu6041539
Zhong, C., Tessing, J., Lee, B.K., Lyall, K. Maternal Dietary Factors and the Risk of Autism Spectrum Disorders: A Systematic Review of Existing Evidence. Autism Res,13(10),1634-1658. https://doi.org/10.1002/aur.2402
Playful practices to enhance health with biofeedback
Posted: May 4, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, computer, Exercise/movement, health, Neck and shoulder discomfort, Pain/discomfort, self-healing, Uncategorized | Tags: exercise, Feldenkrais, pain, Play, somatics 1 CommentAdapted from: Gibney, K.H. & Peper, E. (2003). Exercise or play? Medicine of fun. Biofeedback, 31(2), 14-17.

Homework assignments are sometimes viewed as chore and one more thing to do. Changing the perception from that of work to fun by encouraging laughter and joy often supports the healing process. This blog focusses on utilizing childhood activities and paradoxical movement to help clients release tension patterns and improve range of motion. A strong emphasis is placed on linking diaphragmatic breathing to movement.
When I went home I showed my granddaughter how to be a tree swaying in the wind, she looked at me and said, “Grandma, I learned that in kindergarten!”
‘Betty’ laughed heartily as she relayed this story. Her delight in being able to sway her arms like the limbs of a tree starkly contrasted with her demeanor only a month prior. Betty was referred for biofeedback training after a series of 9 surgeries – wrists, fingers, elbows and shoulders. She arrived at her first session in tears with acute, chronic pain accompanied by frequent, incapacitating spasms in her shoulders and arms. She was unable to abduct her arms more than a few inches without triggering more painful spasms. Her protective bracing and rapid thoracic breathing probably exacerbated her pain and contributed to a limited range of motion of her arms. Unable to work for over a year, she was coping not only with pain, but also with weight gain, poor self-esteem and depression.
The biofeedback training began with effortless, diaphragmatic breathing which is often the foundation of health (Peper and Gibney, 1994). Each thoracic breath added to Betty’s chronic shoulder pain. Convincing Betty to drop her painful bracing pattern and to allow her arms to hang freely from her shoulders as she breathed diaphragmatically was the first major step in regaining mobility. She discovered in that first session that she could use her breathing to achieve control over muscle spasms when she initiated the movement during the exhalation phase of breathing as shown in Figure 1.

Figure 1. Initiate the physical activity after exhaling has begun and body is relaxing especially if the movement or procedure such as an injection would cause pain. Pause the movement when inhaling and then continue the movement again during the exhalation phase. The simple rule is to initiate the activity slightly after beginning exhaling and when the heart rate started to decrease (reproduced with permission from Gorter & Peper, 2012).
During the first week, she practiced her breathing assiduously at home and had fewer spasms. Betty was able to move better during her physical therapy sessions. Each time she felt the onset of muscle spasms she would stop all activity for a moment and ‘go into my trance’ to prevent a recurrence. For the first time in many months, she was feeling optimistic.
Subsequent sessions built upon the foundation of diaphragmatic breathing: boosting Betty’s confidence, increasing range of motion (ROM), and bringing back some fun in life. Activities included many childhood games: tossing a ball, swaying like a tree in the wind, pretending to conduct an orchestra, bouncing on gym balls, playing “Simon Says” (following the movements of the therapist), and dancing. Laughter and childlike joy became a common occurrence. She looked forward to receiving the sparkly star stickers she was given after successful sessions. With each activity, Betty gained more confidence, gradually increased ROM, and began losing weight. Although she had some days where the pain was strong and spasms threatened, Betty reframed the pain as occurring as a result of healing and expanding her ROM—she was no longer a victim of the pain. In addition, her family was proud of her, she was doing more fun activities, and she felt confident that she would return to work.
Betty’s story is similar to other clients whom we have seen. The challenge presented to therapists is to help the client better cope with pain, increase ROM, regain function and, often the most important, to reclaim a “joie de vivre”. Increasing function includes using the minimum amount of effort necessary for the task, allowing unnecessary muscles to remain relaxed (inhibition of dysponesis[i]), and quickly releasing muscle tension when the muscle is no longer required for the activity (work/rest) (Whatmore & Kohli, 1974; Peper et al, 2010; Sella, 2019). The challenge is to perform the task without concurrent evocation of components of the alarm reaction, which tend to be evoked when “we try to do it perfectly,” or “it has to work,” “If I do not do it correctly,” or “I will be judged.” For example, when people learn how to implement micro-breaks (1–2 second rest periods) at the computer, they often sit quietly believing that they are relaxed; however, they may continue a bracing pattern (Peper et al, 2006). Alternatively, tossing a small ball rather than resting at the keyboard will generally evoke laughter, encourage generalization of skills, and covertly induce more relaxation. In some cases, therapists in their desire to help clientss to get well assign structured exercises as homework that evoke striving for performance and boredom—this striving to perform the structured exercises may inhibit healing. Utilizing tools other than those found in the work setting helps the client achieve a broader perspective of the healing/preventive concepts that are taught.
To optimize success, clients are active participants in their own healing process which means that they learn the skills during the therapeutic session and practice at home and at work. Home practices are assigned to integrate the mastery of news skills into daily life. To help clients achieve increased health through physical activity three different approaches are often used: movement reeducation, youthful play, and pure exercise. How the client performs the activity may be monitored with surface electromyography (SEMG) to identify muscles tightening that are not needed for the task and how the muscle relaxes when not needed for the task performance. This monitoring can be done with a portable biofeedback device or multi-channel system when walking or performing the exercises. Clients can even use a single channel SEMG at home.
When working to improve ROM and physical function, explore the following:
- Maintain diaphragmatic breathing – rhythm or tempo may change but the breath must be generated from the diaphragm with emphasis on full exhalation. Use strain gauge feedback and/or SEMG feedback to monitor and train effortless breathing (Peper et al., 2016). Strain gauge feedback is used to teach a slower and diaphragmatic breathing pattern, while SEMG recorded from the scalene to trapezius is used to teach how to reduce shoulder and ancillary muscle tension during inhalation
- Perform activities or stretching/strengthening exercises so slowly that they don’t trigger or aggravate pain during the exhalation phase of breathing.
- Use the minimum amount of tension necessary for the task and let unnecessary muscles remain relaxed. Use SEMG feedback recorded from muscles not needed for the performance of the task to teach clients awareness of inappropriate muscle tension and to learn relaxation of those muscles.
- Release muscle tension immediately when the task is accomplished. Use SEMG feedback to monitor that the muscles are completely relaxed. If rapid relaxation is not achieved, first teach the person to relax the muscles before repeating the muscle activity.
- Perform the exercises as if you have never performed them and do them with a childlike, beginner’s mind, and exploratory attitude (Kabat-Zinn, 1990).
- Create exercises that are totally new and novel so that the participant has no expectancy of outcome can be surprised by their own experience. This approach is part of many somatic educational and therapeutic approaches such as Feldenkrais or Somatics (Hanna, 2004; Feldenkrais, 2009).
Movement and exercise can be taught as pure physical exercise, movement reeducation or youthful playing. Physical exercise is necessary for strength and endurance and at the same time, improves our mood (Thayer, 1996; Mahindru et al., 2023). However, many exercises are considered a burden and are often taught without a sense of lightness and fun, which results in the client thinking in terms that are powerless and helpless (depressive)—“I have to do them.” Helping your clients to understand that exercise is simply a part of every day life, that it encourages healing and improves health, and that they can “cheat” at it, may help them to reframe their attitudes toward it and accomplish their healing goals.
Pure Physical Exercise—Enjoyment through Strength and Flexibility
The major challenge of structured exercises is that the person is very serious and strives too hard to attain the goal. In the process of striving, the body is often held rigid: Breath is shallow and halted and shoulders are slightly braced. Maintaining a daily chart is an excellent tool to show improvement (e.g., more repetitions, more weight, increased flexibility; since, structured exercises are very helpful for improving ROM and strength. When using pure exercise, remember that injured person may have a sense of urgency – they want to get well quickly and, if work stress was a factor in developing pain, they often rush when they need to meet a deadline.
As much as possible make the exercise fun. Help the client understand that he/she can be quick while not rushed. For example, monitor SEMG from an upper trapezius muscle using a portable electromyography. For example, begin by walking slowly. Add a ramp or step to ensure that there is no bracing when climbing (a common occurrence). Walk around the room, down the hall, around the block. Maintain relaxed shoulders, an even swing of the arms, and diaphragmatic breathing. Walk more quickly while emphasizing relaxation with speed rather than rushing. Go faster and faster. Up the stairs. Down the stairs. Walk backward. Skip. Hop. Laugh.
Movement Reeducation – Be ‘Oppositional’ And Do It Differently
Movement reeducation, such as Feldenkrais, Alexander Technique or Hannah Somatics, involves conscious awareness of movement (Alexander, 2001; Hanna, 2004; Murphy, 1993). Many daily patterns of movement become imbedded in our consciousness and, over the years, may include a pain trigger. A common trigger is lifting the shoulders when reaching for the keyboard or mouse, people suffering from thoracic outlet syndrome (TOS) often have such patterns (Peper & Harvey, 2021). A keyboard can often inadvertently cue the client to trigger this dysponetic, and frequently painful, pattern. Have the client do movement reeducation exercises as they are guided through practices in which they have no expectancy and the movements are novel. The focus is on awareness without triggering any fight/flight or startle responses.
Ask the client to explore performing many functional activities with the opposite hand, such as brushing his/her hair or teeth, eating, blowing his/her hair dry, or doing household chores, such as vacuuming. (Explore this for yourself, as well!). Be aware of how much shoulder muscle tension is needed to raise the arms for combing or blow-drying the hair. Explore how little effort is required to hold a fork or knife (you might want to do this in the privacy of your own home!).
Do movements differently such as, practicing alternating hands when leading with the vacuum or when sweeping, changing routes when driving/walking to work or the store, getting out of bed differently. Break up habitual conditioned reflex patterns such as eye, head and hand coordination. For example, slowly rotate your head from left to right and simultaneously shift your eyes in the opposite direction (e.g., turn your head fully to the right while shifting your eyes fully to the left, and then reverse) or before reaching forward, drop your elbows to your sides then, bend your elbows and touch your shoulders with your thumbs then, reach forward. Often, when we change our patterns we increase our flexibility, inhibit bracing and reduce discomfort.
Free Your Neck and Shoulders (adapted from a demonstration by Sharon Keane and developed by Ilana Rubenfeld, 2001)
–Push away from the keyboard and sit at the edge of the chair with your knees bent at right angles and your feet shoulder-width apart and flat on the floor. Do the following movements slowly. Do NOT push yourself if you feel discomfort. Be gentle with yourself.
–Look to the right and gently turn your head and body as far as you can go to the right. When you have gone as far as you can comfortably go, look at the furthest spot on the wall and remember that spot. Gently rotate your head back to center. Close your eyes and relax.
–Reach up with your left hand; pass it over the top of your head and hold on to your right ear. Then, gently bend to the left lowering your elbow towards the floor. Slowly straighten up. Repeat for a few times feeling as if you are a sapling flexing in the breeze. Observe what your body is doing as it bends and comes back up to center. Notice the movements in your ribs, back and neck. Then, drop your arm to your lap and relax. Make sure you continue to breathe diaphragmatically throughout the exercise.
–Reach up with your right hand and pass it over the top of your head and hold on to your left ear. Repeat as above except bending to the right.
–Reach up with your left hand and pass it over the top of your head and hold on to your right ear. Then, look to the left with your eyes and rotate your head to the left as if you are looking behind you. Return to center and repeat the movement a few times. Then, drop your arm to your lap and relax for a few breaths.
–Again, reach over your head with your left hand and hold onto your right ear. Repeat the same rotating motion of your head to the left except that your eyes look to the right. Repeat this a few times then, drop your arm to your lap and relax for a few breaths.
–Reach up with your right hand and pass it over the top of your head and hold on to your left ear. Then, look to the right with your eyes and rotate your head to the right as if you are looking behind you. Return to center and repeat a few times. Then, drop your arm to your lap and relax for a few breaths.
–Again, reach over your head with your right hand and hold onto your left ear. Repeat the same rotating motion of your head to the right except that your eyes look to the left. Repeat this a few times then, drop your arm to your lap and relax for a few breaths.
–Now, look to the right and gently turn your head and body as far as you can go. When you can not go any further, look at that point on the wall. Did you rotate further than at the beginning of the exercise?
–Gently rotate your head back to center, close your eyes, relax and notice the feeling in your neck, shoulders and back.
Youthful Playing – Pavlovian Practice
Evoking positive past memories and actually acting them out may enhance health as is illustrated by the recovery of serious illness of Ivan Pavlov, the discovery of classical conditioning. When Pavlov quietly lay in his hospital bed, many, including his family, thought he was slipping into death. He then ask the nurse to get him a bowl of water with earth in it and the whole night long he gently played with the mud. He recreated the experience when as a child he was playing in mud along a river’s bank. Pavlov knew that evoking the playful joy of childhood would help to encourage mental and physical healing. The mud in hands was the conditioned stimulus to evoke the somatic experience of wellness (Peper, Gibney, & Holt, 2002).
Having clients play can encourage laughter and joie de vivre, which may help in physical healing. Being involved in childhood games and actually playing these games with children removes one from worries and concerns—both past and future—and allows one to be simply in the present. Just being present is associated with playfulness, timelessness, passive attention, creativity and humor. A state in which one’s preconceived mental images and expectancies—the personal, familial, cultural, and healthcare provider’s hypnotic suggestions—are by-passed and for that moment, the present and the future are yet undefined. This is often the opposite of the client’s expectancy; since, remembering the past experiences and the diagnosis creates a fixed mental image that may expect pain and limitation.
Explore some of the following practices as strategies to increase movement and flexibility without effort and to increase joy. Use your creativity and explore your own permutations of the practices. Observe how your mood improves and your energy increases when you play a childhood game instead of an equivalent exercise. For example, instead of dropping your hands to your lap or stretching at the computer terminal during a micro- or meso-break[ii], go over to your coworker and play “pattycake.” This is the game in which you and your partner face each other and then clap your hands and then touch each other’s palms. Do this in all variations of the game.
For increased ROM in the shoulders explore some of the following (remember the basics: diaphragmatic breathing, minimum effort, rapid release) in addition, do the practices to the rhythm of the music that you enjoyed as a young person.
Ball Toss: a hand-sized ball that is easily squeezed is best for this exercise. Monitor respiration patterns, and SEMG forearm extensors and/or flexors, and upper trapezii muscles. Sit quietly in a chair and focus on a relaxed breathing rhythm. Toss the ball in the air with your right hand and catch it with your left hand. As soon as you catch the ball, drop both hands to your lap. Toss the ball back only when you achieve relaxation—both with the empty hand and the hand holding the ball. Watch for over-efforting in the upper trapezii. Begin slowly and increase the pace as you train yourself to quickly release unnecessary muscle tension. Go faster and faster (just about everyone begins to laugh, especially each time they drop the ball).
Ball Squeeze/Toss: Expand upon the above by squeezing the ball prior to tossing. When working with a client, call out different degrees of pressure (e.g., 50%, 10%, 80%, etc.). The same rules apply as with the ball toss.
Ball Hand to Hand: Close your eyes and hand the ball back and forth. Go faster and faster and add ball squeezes prior to passing the ball.
Gym Ball Bounces: Sit on a gym ball and find your balance. Begin bouncing slowly up and down. Reach up and lower your left then, right hand. Abduct your arms forward then, laterally. Turn on the radio and bounce to music.
Simon Says: This can be done standing, sitting in a chair or on a gym ball. When on a gym ball, bounce during the game. Have your client do a mirror image of your movements: reaching up, down, left, right, forward or backward. Touch your head, nose, knees or belly. Have fun and go more quickly.
Back-To-Back Massage: With a partner, stand back-to-back. Lean against each other’s back so that you provide mutual support. Then each rub your back against each other’s back. Enjoy the wiggling movement and stimulation. Be sure to continue to breathe.
Summary: An Attitude of Fun
In summary, it is not what you do; it is also the attitude by which you do it that affects health. From this perspective,when exercises are performed playfully, flexibility, movement and health are enhanced while discomfort is decreased. Inducing laughter promotes healing and disrupts the automatic negative hypnotic suggestion/self-images of what is expected. The clients begins to live in the present moment and thereby decreases the anticipatory bracing and dysponetic activity triggered by striving. By decreasing striving and concern for results, clients may allow themselves to perform the practices with a passive attentive attitude that may facilitate healing. For that moment, the client forgets the painful past and a future expectances that are fraught with promises of continued pain and inactivity. At moment, the pain cycle is interrupted which provides hope for a healthier future.
References
Alexander, F.M. (2001). The Use of the Self. London: Orion Publishing. https://www.amazon.com/Use-Self-F-M-Alexander/dp/0752843915
Feldenkrais, M. (2009). Awareness Through Movement Easy-to-Do Health Exercises to Improve Your Posture, Vision, Imagination, and Personal Awareness. New York: HarperOne. https://www.amazon.com/Awareness-Through-Movement-Easy-Do/dp/0062503227
Gibney, K.H. & Peper, E. (2003). Exercise or play? Medicine of fun. Biofeedback, 31(2), 14-17. https://www.researchgate.net/publication/380317304_EXERCISE_OR_PLAY_MEDICINE_OF_FUN
Gorter, R. & Peper, E. (2012). Fighting Cancer- A Nontoxic Approach to Treatment. Berkeley: North Atlantic Books. https://www.amazon.com/Fighting-Cancer-Nontoxic-Approach-Treatment/dp/1583942483
Hanna, T. (2004). Somatics: Reawakening The Mind’s Control Of Movement, Flexibility, And Health. Da Capo Press. https://www.amazon.com/Somatics-Reawakening-Control-Movement-Flexibility/dp/0738209570
Kabat-Zinn, J. (1990). Full catastrophe living. New York: Delacorte Press.
Mahindru, A., Patil, P., & Agrawal, V. (2023). Role of Physical Activity on Mental Health and Well-Being: A Review. Cureus, I5(1), e33475. https://doi.org/10.7759/cureus.33475
Murphy, M. (1993). The future of the body. New York: Jeremy P. Tarcher/Perigee. https://www.amazon.com/Future-Body-Explorations-Further-Evolution/dp/0874777305
Peper, E., Booiman, A., Lin, I-M, Harvey, R., & Mitose, J. (2016). Abdominal SEMG Feedback for Diaphragmatic Breathing: A Methodological Note. Biofeedback. 44(1), 42-49. https://www.researchgate.net/publication/300365890_Abdominal_SEMG_Feedback_for_Diaphragmatic_Breathing_A_Methodological_Note
Peper, E., Booiman, A., Tallard, M., & Takebayashi, N. (2010). Surface electromyographic biofeedback to optimize performance in daily life: Improving physical fitness and health at the worksite. Japanese Journal of Biofeedback Research, 37(1), 19-28. https://doi.org/10.20595/jjbf.37.1_19
Peper, E., Gibney, K. & Holt, C. (2002). Make health happen: Training yourself to create wellness. Dubuque, IA: Kendall-Hunt. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E. & Harvey, R. (2021). Causes of TechStress and ‘Technology-Associated Overuse’ Syndrome and Solutions for Reducing Screen Fatigue, Neck and Shoulder Pain, and Screen Addiction. Townsend Letter-The examiner of Alternative Medicine, Oct 28, 2021. https://www.townsendletter.com/article/459-techstress-how-technology-is-hurting-us
Peper, E., Harvey, R. & Tylova, H. (2006). Stress protocol for assessing computer related disorders. Biofeedback. 34(2), 57-62. https://www.researchgate.net/publication/242549995_FEATURE_Stress_Protocol_for_Assessing_Computer-Related_Disorders
Peper, E. & Tibbetts, V. (1994). Effortless diaphragmatic breathing. Physical Therapy Products. 6(2), 67-71. Also in: Electromyography: Applications in Physical Therapy. Montreal: Thought Technology Ltd. https://www.bfe.org/protocol/pro10eng.htm
Rubenfeld, I. (2001). The listening hands: Self-healing through Rubenfeld Synergy method of talk and touch. New York: Random House. https://www.amazon.com/Listening-Hand-Self-Healing-Through-Rubenfeld/dp/0553379836
Sella, G. E. (2019). Surface EMG (SEMG): A Synopsis. Biofeedback, 47(2), 36–43. https://doi.org/10.5298/1081-5937-47.1.05
Thayer, R.E. (1996). The origin of everyday moods—Managing energy, tension, and stress. New York: Oxford University Press. https://www.amazon.com/Origin-Everyday-Moods-Managing-Tension/dp/0195118057
Whatmore, G. and Kohli, D. The Physiopathology and Treatment of Functional Disorders. New York: Grune and Stratton, 1974. https://www.amazon.com/physiopathology-treatment-functional-disorders-biofeedback/dp/0808908510
[i] Dysponesis involves misplaced muscle activities or efforts that are usually covert and do not add functionally to the movement. From: Dys” meaning bad, faulty or wrong, and “ponos” meaning effort, work or energy (Whatmore and Kohli, 1974)
[ii] A meso-break is a 10 to 90 second break that consists of a change in work position, movement or a structured activity such as stretching that automatically relaxes those muscles that were previously activated while performing a task.
Quick Rescue Techniques When Stressed
Posted: February 4, 2024 Filed under: attention, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, education, emotions, Evolutionary perspective, Exercise/movement, health, mindfulness, Neck and shoulder discomfort, posture, relaxation, stress management, Uncategorized | Tags: alarm reaction, anxiety, box breathing, Breathing, conditioning, defense reaction, health, huming, Parasympathetic response, rumination, safety, sniff inhale, somatic practices, stress, sympathetic arousal, tactical breathing, Toning, yoga 9 CommentsErik Peper, PhD, Yuval Oded, PhD, and Richard Harvey, PhD
Adapted from Peper, E., Oded, Y, & Harvey, R. (2024). Quick somatic rescue techniques when stressed. Biofeedback, 52(1), 18–26. https://doi.org/10.5298/982312

“If a problem is fixable, if a situation is such that you can do something about it, then there is no need to worry. If it’s not fixable, then there is no help in worrying. There is no benefit in worrying whatsoever.” ― Dalai Lama XIV
To implement the Dalai Lama’s quote is challenging. When caught up in an argument, being angry, extremely frustrated, or totally stressed, it is easy to ruminate, worry. It is much more challenging to remember to stay calm. When remembering the message of the Dalai Lama’s quote, it may be possible to shift perspective about the situation although a mindful attitude may not stop ruminating thoughts. The body typically continues to reacti to the torrents of thoughts that may occur when rehashing rage over injustices, fear over physical or psychological threats, or profound grief and sadness over the loss of a family member. Some people become even more agitated and less rational as illustrated in the following examples.
I had an argument with my ex and I am still pissed off. Each time I think of him or anticipate seeing them, my whole body tightened. I cannot stomach seeing him and I already see the anger in his face and voice. My thoughts kept rehashing the conflict and I am getting more and more upset.
A car cut right in front of me to squeeze into my lane. I had to slam on my brakes. What an idiot! My heart rate was racing and I wanted to punch the driver.
When threatened, we respond quickly in our thoughts and body with a defense reaction that may negatively affect those around us as well as ourselves. What can we do to interrupt negative stress reactions?
Background
Many approaches exist that allow us to become calmer and less reactive. General categories include techniques of cognitive reappraisal (seeing the situation from the other person’s point of view and labeling your own feelings and emotions) and stress management techniques. Practices that are beneficial include mindfulness meditation, benign humor (versus gallows humor), listening to music, taking a time out while implementing a variety of self-soothing practices, or incorporating slow breathing (e.g., heart rate variability and/or box breathing) throughout the day.
No technique fits all as we respond differently to our stressful life circumstances. For example, some people during stress react with a “tend and befriend stress response” (Cohen & Lansing, 2021; Taylor et al., 2000). This response appears to be mostly mediated by the hormone oxytocin acting in ways that sooth or calm the nervous system as an analgesic. These neurophysiological mechanisms of the soothing with the calming analgesic effects of oxytocin have been characterized in detail by Xin, et al. (2017).
The most common response is a fight/flight/freeze stress response that is mediated by excitatory hormones such as adrenalin and inhibitory neurotransmitters such as gamma amino butyric acid (GABA). There is a long history of fight/flight/freeze stress response research, which is beyond the scope of this blog with major theories and terms such as interior milleau (Bernard, 1872); homeostasis and fight/flight (Cannon, 1929); general adaptation syndrome (Selye, 1951); polyvagal theory (Porges, 1995); and, allostatic load (McEwen, 1998). A simplified way to start a discussion about stress reactions begins with the fight/flight stress response. When stressed our defense reactions are triggered. Our sympathetic nervous system becomes activated our mind and body stereotypically responds as illustrated in Figure 1.

Figure 1. An intense confrontation tends to evoke a stress response (reproduced from Peper et al., 2020).
The flight/fight response triggers a cascade of stress hormones or neurotransmitters (e.g., hypothalamus-pituitary-adrenal cascade) and produces body changes such as the heart pounding, quicker breathing, an increase in muscle tension and sweating. Our body mobilizes itself to protect itself from danger. Our focus is on immediate survival and not what will occur in the future (Porges, 2021; Sapolsky, 2004). It is as if we are facing an angry lion—a life-threatening situation—and we feel threatened and unsafe.
Rather than sitting still, a quick effective strategy is to interrupt this fight/flight response process by completing the alarm reaction such as by moving our muscles (e.g., simulating a fight or flight behavior) before continuing with slower breathing or other self-soothing strategies. Many people have experienced their body tension is reduced and they feel calmer when they do vigorous exercise after being upset, frustrated or angry. Similarly, athletes often have reported that they experience reduced frequency and/or intensity of negative thoughts after an exhausting workout (Thayer, 2003; Liao et al., 2015; Basso & Suzuki, 2017).
Becoming aware of the escalating cascades of physical, behavioral and psychological responses to a stressor is the first step in interrupting the escalating process. After becoming aware, reduce the body’s arousal and change the though patterns using any of the techniques described in this blog. The self-regulation skills presented in this blog are ideally over-learned and automated so that these skills can be rapidly implemented to shift from being stressed to being calm. Examples of skills that can shift from sympathetic neervous system overarousal to parasympathetic nervous system calm include techniques of autogenic traing (Schulz & Luthe, 1959), the quieting reflex developed by Charles Stroebel in 1985 or more recently rescue breathing developed by Richard Gevirtz (Stroebel, 1985; Gevirtz, 2014; Peper, Gibney & Holt, 2002; Peper & Gibney, 2003).
Concepts underlying the rescue techniques
- Psychophysiological principle: “Every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, conscious or unconscious, and conversely, every change in the mental-emotional state, conscious or unconscious, is accompanied by an appropriate change in the physiological state” (Green et al. 1970, p. 3).
- Posture evokes memories and feelings associated with the position. When the body posture is erect and tall while looking slightly up. It is easier to evoke empowering, positive thoughts and feelings. When looking down it is easier to evoke hopeless, helpless and powerless thoughts and feelings (Peper et al., 2017).
- Healing occurs more easily when relaxed and feeling safe. Feeling safe and nurtured enhances the parasympathetic state and reduces the sympathetic state. Use memory recall to evoke those experiences when you felt safe (Peper, 2021).
- Interrupting thoughts is easier with somatic movement than by redirecting attention and thinking of something else without somatic movement.
- Focus on what you want to do not want to do. Attempting to stop thinking or ruminating about something tends to keeps it present (e.g., do not think of pink elephants. What color is the elephant? When you answer, “not pink,” you are still thinking pink). A general concept is to direct your attention (or have others guide you) to something else (Hilt & Pollak, 2012; Oded, 2018; Seo, 2023).
- Skill mastery takes practice and role rehearsal (Lally et al., 2010; Peper & Wilson, 2021).
- Use classical conditioning concepts to facilitate shifting states. Practice the skills and associate them with an aroma, memory, sounds or touch cues. Then when you the situation occurs, use these classical conditioned cues to facilitate the regeneration response (Peper & Wilson, 2021).
Rescue techniques
Coping When Highly Stressed and Agitated
- Complete the alarm/defense reaction with physical activity (Be careful when you do these physical exercises if you have back, hip, knee, or ankle problems).
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Check whether the situation is actually a threat. If yes, then do anything to get out of immediate danger (yell, scream, fight, run away, or dial 911).
- If there is no actual physical threat, then leave the situation and perform vigorous physical activity to complete your alarm reaction, such as going for a run or walking quickly up and down stairs. As you do the exercise, push yourself so that the muscles in your thighs are aching, which focusses your attention on the sensations in your thighs. In our experience, an intensive run for 20 minutes quiets the brain while it often takes 40 minutes when walking somewhat quickly.
- After recovering from the exhaustive exercise, explore new options to resolve the conflict.
- Complete the alarm/defense reaction and evoke calmness with the S.O.S™ technique (Oded, 2023)
- Acknowledge you have reacted and have chosen to interrupt your automatic response.
- Squat against a wall (similar to the wall-sit many skiers practice). While tensing your arms and fists as shown in Figure 2, gaze upward because it is more difficult to engage in negative thinking while looking upwards. If you continue to ruminate, then scan the room for object of a certain color or feature to shift visual attention and be totally present on the visual object.
- Do this set of movements for 7 to 10 seconds or until you start shaking. Than stand up and relax hands and legs. While standing, bounce up and down loosely for 10 to 15 seconds as you become aware of the vibratory sensations in your arms and shoulders, as shown in Figure 3.

Figure 2.Defense position wall-sit to tighten muscles in the protective defense posture (Oded, 2023). Figure 3. Bouncing up and down to loosen muscles ((Oded, 2023).
- Acknowledge you have reacted and have chosen to interrupt your automatic response. Swing your arms back and forth for 20 seconds. Allow the arms to swing freely as illustrated in Figure 4.

Figure 4. Swinging the arms to loosen the body and spine (Oded, 2023).
- Rest and ground. Lie on the floor and put your calves and feet on a chair seat so that the psoas muscle can relax, as illustrated in Figure 5. Allow yourself to be totally supported by the floor and chair. Be sure there is a small pillow under your head and put your hand on your abdomen so that you can focus on abdominal breathing.

Figure 5. Lying down to allow the psoas muscle to relax and feel grounded (Oded, 2023).
- While lying down, imagine a safe place or memory and make it as real as possible. It is often helpful to listen to a guided imagery or music. The experience can be enhanced if cues are present that are associated with the safe place, such as pictures, sounds, or smells. Continue to breathe effortlessly at about six breaths per minute. If your attention wanders, bring it back to the memory or to the breathing. Allow yourself to rest for 10 minutes.
In most cases, thoughts stop and the body’s parasympathetic activity becomes dominant as the person feels safe and calm. Usually, the hands warm and the blood volume pulse amplitude increases as an indicator of feeling safe, as shown in Figure 6.

Figure 6. Blood volume pulse increases as the person is relaxing, feels safe and calm.
Coping When You Can’t Get Away (adapted from Peper, Harvey & Faass, 2020)
In many cases, it is difficult or embarrassing to remove yourself from the situation when you are stressed out such as at work, in a business meeting or social gathering.
- Become aware that you have reacted.
- Excuse yourself for a moment and go to a private space, such as a restroom. Going to the bathroom is one of the only acceptable social behaviors to leave a meeting for a short time.
- In the bathroom stall, do the 5-minute Nyingma exercise, which was taught by Tarthang Tulku Rinpoche in the tradition of Tibetan Buddhism, as a strategy for thought stopping (see Figure 7). Stand on your toes with your heels touching each other. Lift your heels off the floor while bending your knees. Place your hands at your sides and look upward. Breathe slowly and deeply (e.g., belly breathing at six breaths a minute) and imagine the air circulating through your legs and arms. Do this slow breathing and visualization next to a wall so you can steady yourself if necessary to keep balance. Stay in this position for 5 minutes or longer. Do not straighten your legs—keep squatting despite the discomfort. In a very short time, your attention is captured by the burning sensation in your thighs. Continue. After 5 minutes, stop and shake your arms and legs.

Figure 7. Stressor squat Nyingma exercise (reproduced from Peper et al., 2020).
- Follow this practice with slow abdominal breathing to enhance the parasympathetic response. Be sure that the abdomen expands as the inhalation occurs. Breathe in and out through the nose at about six breaths per minute.
- Once you feel centered and peaceful, return to the room.
- After this exercise, your racing thoughts most likely will have stopped and you will be able to continue your day with greater calm.
What to do When Ruminating, Agitated, Anxious or Depressed
(adapted from Peper, Harvey, & Hamiel, 2019).
- Shift your position by sitting or standing erect in a power position with the back of the head reaching upward to the ceiling while slightly gazing upward. Then sniff quickly through nose, hold and again sniff quickly then very slowly exhale. Be sure as you exhale your abdomen constricts. Then sniff again as your abdomen gets bigger, hold, and sniff one more time letting the abdomen get even bigger. Then, very slow, exhale through the nose to the internal count of six (adapted from Balban et al., 2023). When you sniff or gasp, your racing thoughts will stop (Peper et al., 2016).
- Continue with box breathing (sometimes described as tactical breathing or battle breathing) by exhaling slowly through your nose for 4 seconds, holding your breath for 4 seconds, inhaling slowly for 4 seconds through your nose, holding your breath for 4 seconds and then repeating this cycle of breathing for a few minutes (Röttger et al., 2021; Balban et al., 2023). Focusing your attention on performing the box breathing makes it almost impossible to think of anything else. After a few minutes, follow this with slow effortless diaphragmatic breathing at about six breaths per minute. While exhaling slowly through your nose, look up and when you inhale imagine the air coming from above you. Then as you exhale, imagine and feel the air flowing down and through your arms and legs and out the hands and feet.
- While gazing upward, elicit a positive memory or a time when you felt safe, powerful, strong and/or grounded. Make the positive memory as real as possible.
- Implement cognitive strategies such as reframing the issue, sending goodwill to the person, seeing the problem from the other person’s point of view, and ask is this problem worth dying over (Peper, Harvey, & Hamiel, 2019).
What to Do When Thoughts Keep Interrupting
Practice humming or toning. When you are humming or toning, your focus is on making the sound and the thoughts tend to stop. Generally, breathing will slow down to about six breaths per minute (Peper, Pollack et al., 2019). Explore the following:
- Box breathing (Röttger et al., 2021; Balban et al., 2023)
- Humming also known as bee breath (Bhramari Pranayama) (Abishek et al., 2019; Yoga, 2023) – Allow the tongue to rest against the upper palate, sit tall and erect so that the back of the head is reaching upward to the ceiling, and inhale through your nose as the abdomen expands. Then begin humming while the air flows out through your nose, feel the vibration in the nose, face and throat. Let humming last for about 7 seconds and then allow the air to blow in through the nose and then hum again. Continue for about 5 minutes.
- Toning – Inhale through your nose and then vocalize a single sound such as Om. As you vocalize the lower sound, feel the vibration in your throat, chest and even going down to the abdomen. Let each toning exhalation last for about 6 to 7 seconds and then inhale through your nose. Continue for about 5 minutes (Peper, al., 2019).
Many people report that after practice these skills, they become aware that they are reacting and are able to reduce their automatic reaction. As a result, they experience a significant decrease in their stress levels, fewer symptoms such as neck and holder tension and high blood pressure, and they feel an increase in tranquility and the ability to communicate effectively.
Practicing these skills does not resolve the conflicts; they allow you to stop reacting automatically. This process allows you a time out and may give you the ability to be calmer, which allows you to think more clearly. When calmer, problem solving is usually more successful. As phrased in a popular meme, “You cannot see your reflection in boiling water. Similarly, you cannot see the truth in a state of anger. When the waters calm, clarity comes” (author unknown).

Boiling water (photo modified from: https://www.facebook.com/photo/?fbid=388991500314839&set=a.377199901493999)
Below are additional resources that describe the practices. Please share these resources with friends, family and co-workers.
Stressor squat instructions
Toning instructions
Diaphragmatic breathing instructions
Reduce stress with posture and breathing
Conditioning
References
Abishek, K., Bakshi, S. S., & Bhavanani, A. B. (2019). The efficacy of yogic breathing exercise bhramari pranayama in relieving symptoms of chronic rhinosinusitis. International Journal of Yoga, 12(2), 120–123. https://doi.org/10.4103/ijoy.IJOY_32_18
Balban, M. Y., Neri, E., Kogon, M. M., Weed, L., Nouriani, B., Jo, B., Holl, G., Zeitzer, J. M., Spiegel, D., Huberman, A. D. (2023). Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Reports Medicine, 4(1), 10089. https://doi.org/10.1016/j.xcrm.2022.100895
Basso, J. C. & Suzuki, W. A. (2017). The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: A review. Brain Plast, 2(2), 127–152. https://doi.org/10.3233/BPL-160040
Bernard, C. (1872). De la physiologie générale. Paris: Hachette livre. https://www.amazon.ca/PHYSIOLOGIE-GENERALE-BERNARD-C/dp/2012178596
Cannon, W. B. (1929). Organization for Physiological Homeostasis. Physiological Reviews, 9, 399–431. https://doi.org/10.1152/physrev.1929.9.3.399
Cohen, L. & Lansing, A. H. (2021). The tend and befriend theory of stress: Understanding the biological, evolutionary, and psychosocial aspects of the female stress response. In: Hazlett-Stevens, H. (eds), Biopsychosocial Factors of Stress, and Mindfulness for Stress Reduction. pp. 67–81, Springer, Cham. https://doi.org/10.1007/978-3-030-81245-4_3
Gevirtz, R. (2014). HRV Training and its Importance – Richard Gevirtz, Ph.D., Pioneer in HRV Research & Training. Thought Technology. Accessed December 29, 2023. https://www.youtube.com/watch?v=9nwFUKuJSE0
Green, E. E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological. Journal of Transpersonal Psychology, 2, 1–26. https://atpweb.org/jtparchive/trps-02-70-01-001.pdf
Hilt, L. M., & Pollak, S. D. (2012). Getting out of rumination: comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165.
https://doi.org/10.1007/s10802-012-9638-3
Lally, P., VanJaarsveld, C. H., Potts, H. W., & Wardle, J. (2010). How habits are formed: Modelling habit formation the real world. European Journal of Social Psychology, 40, 998–1009. https://doi.org/10.1002/ejsp.674
Liao, Y., Shonkoff, E. T., & Dunton, G. F. (2015). The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology. 6, 1975. https://doi.org/10.3389/fpsyg.2015.01975
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44.
https://doi.org/10.1111/j.1749-6632.1998.tb09546.x
Oded, Y. (2018). Integrating mindfulness and biofeedback in the treatment of posttraumatic stress disorder. Biofeedback, 46(2), 37-47. https://doi.org/10.5298/1081-5937-46.02.03
Oded, Y. (2023). Personal communication. S.O.S 1™ technique is part of the Sense Of Safety™ method. www.senseofsafety.co
Peper, E. (2021). Relive memory to create healing imagery. Somatics, XVIII(4), 32–35.https://www.researchgate.net/publication/369114535_Relive_memory_to_create_healing_imagery
Peper, E., Gibney, K.H. & Holt. C. (2002). Make Health Happen: Training Yourself to Create Wellness. Dubuque, IA: Kendall-Hunt. https://he.kendallhunt.com/product/make-health-happen-training-yourself-create-wellness
Peper, E., & Gibney, K.H. (2003). A teaching strategy for successful hand warming. Somatics. XIV(1), 26–30. https://www.researchgate.net/publication/376954376_A_teaching_strategy_for_successful_hand_warming
Peper, E., Harvey, R., & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. North Atlantic Books. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X
Peper, E., Harvey, R., & Hamiel, D. (2019). Transforming thoughts with postural awareness to increase therapeutic and teaching efficacy. NeuroRegulation, 6(3),153–160. https://doi.org/10.15540/nr.6.3.153
Peper, E., Lee, S., Harvey, R., & Lin, I-M. (2016). Breathing and math performance: Implication for performance and neurotherapy. NeuroRegulation, 3(4), 142–149. http://dx.doi.org/10.15540/nr.3.4.142
Peper, E., Lin, I-M, Harvey, R., & Perez, J. (2017). How posture affects memory recall and mood. Biofeedback, 45(2), 36–41. https://doi.org/10.5298/1081-5937-45.2.01
Peper, E., Pollack, W., Harvey, R., Yoshino, A., Daubenmier, J. & Anziani, M. (2019). Which quiets the mind more quickly and increases HRV: Toning or mindfulness? NeuroRegulation, 6(3), 128–133. https://www.neuroregulation.org/article/view/19345/13263
Peper, E. & Wilson, V. (2021). Optimize the learning state: Techniques and habits. Biofeedback, 9(2), 46–49. https://doi.org/10.5298/1081-5937-49-2-04
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology, 32(4), 301–318. https://doi.org/10.1111/j.1469-8986.1995.tb01213.x
Porges, S.W. (2021) Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry, 20(2),296-298. Porges SW. Cardiac vagal tone: a neurophysiological mechanism that evolved in mammals to dampen threat reactions and promote sociality. World Psychiatry. 2021 Jun;20(2):296-298. https://doi.org10.1002/wps.20871
Röttger, S., Theobald, D. A., Abendroth, J., & Jacobsen, T. (2021). The effectiveness of combat tactical breathing as compared with prolonged exhalation. Applied Psychophysiology and Biofeedback, 46, 19–28. https://doi.org/10.1007/s10484-020-09485-w
Sapolsky, R. (2004). Why zebras don’t get ulcers (3rd ed.). New York:Holt. https://www.amazon.com/Why-Zebras-Dont-Ulcers-Third/dp/0805073698/
Schultz, J. H., & Luthe, W. (1959). Autogenic training: A psychophysiologic approach to psychotherapy. Grune & Stratton. https://www.google.com/books/edition/Autogenic_Training/y8SwQgAACAAJ?hl=en
Selye, H. (1951). The general-adaptation-syndrome. Annual Review of Medicine, 2(1), 327–342. https://doi.org/10.1146/annurev.me.02.020151.001551
Seo, H. (2023). How to stop ruminating. The New York Times. Accessed January 3, 2024. https://www.nytimes.com/2023/02/01/well/mind/stop-rumination-worry.html
Stroebel, C. F. (1985). QR: The Quieting Reflex. Berkley. https://www.amazon.com/Qr-quieting-reflex-Charles-Stroebel/dp/0425085066
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A. R., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. https://doi.org/10.1037/0033-295X.107.3.411
Thayer, R. E. (2003). Calm energy: How people regulate mood with food and exercise. Oxford University Press. https://www.amazon.com/Calm-Energy-People-Regulate-Exercise/dp/0195163397
Xin, Q., Bai, B., & Liu, W. (2017). The analgesic effects of oxytocin in the peripheral and central nervous system. Neurochemistry International, 103, 57–64. https://doi.org/10.1016/j.neuint.2016.12.021
Yoga, N. (2023). This simple breath practice is scientifically proven to calm your mind. The nomadic yogi. Accessed December 31, 2023. https://www.leahsugerman.com/blog/bhramari-pranayama-humming-bee-breath#
Reduce the risk for colds and flu and superb science podcasts
Posted: January 24, 2024 Filed under: attention, behavior, education, Evolutionary perspective, Exercise/movement, healing, health, Nutrition/diet, self-healing, stress management, Uncategorized, vision | Tags: colds, darkness, flu, influenza, light 2 Comments
What can we do to reduce the risk of catching a cold or the flu? It is very challenging to make sense out of all the recommendations found on internet and the many different media site such as X(Twitter), Facebook, Instagram, or TikTok. The following podcasts are great sources that examine different topics that can affect health. They are in-depth presentations with superb scientific reasoning.
Huberman Lab podcasts discusses science and science based tools for everyday life. https://www.hubermanlab.com/podcast. Select your episode and they are great to listen to on your cellphone.
THE PODCAST episode, How to prevent and treat cold and flu, is outstanding. Skip the long sponsor introductdion and start listening at the 6 minute point. In this podcast, Professor Andrew Huberman describes behavior, nutrition and supplementation-based tools supported by peer-reviewed research to enhance immune system function and better combat colds and flu. I also dispel common myths about how the cold and flu are transmitted and when you and those around you are contagious. I explain if common preventatives and treatments such as vitamin C, zinc, vitamin D and echinacea work. I also highlight other compounds known to reduce contracting and duration of colds and flu. I discuss how to use exercise and sauna to bolster the immune response. This episode will help listeners understand how to reduce the chances of catching a cold or flu and help people recover more quickly from and prevent the spread of colds and flu.
PODCAST, ScienceVS, is an outstanding podcast series that takes on fads, trends, and opinionated mob to find out what’s fact, what’s not, and what’s somewhere in between. Select your episode and listen.
Link: https://gimletmedia.com/shows/science-vs/episodes#show-tab-picker

PODCAST episode, The Journal club podcast and Youtube, presentation from Huberman Lab is a example of outstanding scientific reasoning. In this presentation, Professor Andrew Huberman and Dr. Peter Attia (author of Outlive: The Science and Art of Longevity) discuss two peer-reviewed scientific papers in-depth. The first discussion explores the role of bright light exposure during the day and dark exposure during the night and its relationship to mental health. The second paper explores a novel class of immunotherapy treatments to combat cancer.