TechStress: Building Healthier Computer Habits
Posted: August 30, 2023 Filed under: ADHD, behavior, biofeedback, Breathing/respiration, cognitive behavior therapy, computer, digital devices, education, emotions, ergonomics, Evolutionary perspective, Exercise/movement, health, laptops, Neck and shoulder discomfort, Pain/discomfort, posture, screen fatigue, stress management, Uncategorized, vision, zoom fatigue | Tags: cellphone, fatigue, gaming, mobile devices, screens 5 CommentsBy Erik Peper, PhD, BCB, Richard Harvey, PhD, and Nancy Faass, MSW, MPH
Adapted by the Well Being Journal, 32(4), 30-35. from the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics by Erik Peper, Richard Harvey, and Nancy Faass.

Every year, millions of office workers in the United States develop occupational injuries from poor computer habits—from carpal tunnel syndrome and tension headaches to repetitive strain injury, such as “mouse shoulder.” You’d think that an office job would be safer than factory work, but the truth is that many of these conditions are associated with a deskbound workstyle.
Back problems are not simply an issue for workers doing physical labor. Currently, the people at greatest risk of injury are those with a desk job earning over $70,000 annually. Globally, computer-related disorders continue to be on the rise. These conditions can affect people of all ages who spend long hours at a computer and digital devices.
In a large survey of high school students, eighty-five percent experienced tension or pain in their neck, shoulders, back, or wrists after working at the computer. We’re just not designed to sit at a computer all day.
Field of Ergonomics
For the past twenty years, teams of researchers all over the world have been evaluating workplace stress and computer injuries—and how to prevent them. As researchers in the fields of holistic health and ergonomics, we observe how people interact with technology. What makes our work unique is that we assess employees not only by interviewing them and observing behaviors, but also by monitoring physical responses.
Specifically, we measure muscle tension and breathing, in the moment, in real-time, while they work. To record shoulder pain, for example, we place small sensors over different muscles and painlessly measure the muscle tension using an EMG (electromyograph)—a device that is employed by physicians, physical therapists, and researchers. Using this device, we can also keep a record of their responses and compare their reactions over time to determine progress.
What we’ve learned is that people get into trouble if their muscles are held in tension for too long. Working at a computer, especially at a stationary desk, most people maintain low-level chronic tension for much of the day. Shallow, rapid breathing is also typical of fine motor tasks that require concentration, like data entry.
Muscle tension and breathing rate usually increase during data entry or typing without our awareness.
When these patterns are paired with psychological pressure due to office politics or job insecurity, the level of tension and the risk of fatigue, inflammation, pain, or injury increase. In most cases, people are totally unaware of the role that tension plays in injury. Of note, the absolute level of tension does not predict injury—rather, it is the absence of periodic rest breaks throughout the day that seems to correlate with future injuries.
Restbreaks
All of life is the alternation between movement and rest, inhaling and exhaling, sleeping and waking. Performing alternating tasks or different types of activities and movement is one way to interrupt the couch potato syndrome—honoring our evolutionary background.
Our research has confirmed what others have observed: that it’s important to be physically active, at least periodically, throughout the day. Alternating activity and rest recreate the pattern of our ancestors’ daily lives. When we alternate sedentary tasks with physical activity, and follow work with relaxation, we function much more efficiently. In short, move your body more.
Better Computer Habits: Alternate Periods of Rest and Activity
As mentioned earlier, our workstyle puts us out of sync with our genetic heritage. Whether hunting and gathering or building and harvesting, our ancestors alternated periods of inactivity with physical tasks that required walking, running, jumping, climbing, digging, lifting, and carrying, to name a few activities. In contrast, today many of us have a workstyle that is so immobile we may not even leave our desk for lunch.
As health researchers, we have had the chance to study workstyles all over the world. Back pain and strain injuries now affect a large proportion of office workers in the US and in high-tech firms worldwide. The vast majority of these jobs are sedentary, so one focus of the research is on how to achieve a more balanced way of working.
A recent study on exercise looked at blood flow to the brain. Researchers Carter and colleagues found that if people sit for four hours on the job, there’s a significant decrease in blood flow to the brain. However, if every thirty or forty minutes they get up and move around for just two minutes, then brain blood flow remains steady. The more often you interrupt sitting with movement, the better.
It may seem obvious that to stay healthy, it’s important to take breaks and be physically active from time to time throughout the day. Alternating activity and rest recreate the pattern of our ancestors’ daily lives. The goal is to alternate sedentary tasks with physical activity and follow work with relaxation. When we keep this type of balance going, most people find that they have more energy, are more productive, and can be more effective.
Genetics: We’re Hardwired Like Ancient Hunters

Despite a modern appearance, we carry the genes of our forebearers—for better and for worse. (Art courtesy of Peter Sis). Reproduced from Peper, E., Harvey, R., & Faass (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
In the modern workplace, most of us find ourselves working indoors, in small office spaces, often sitting at a computer for hours at a time. In fact, the average Westerner spends more than nine hours per day sitting indoors, yet we’re still genetically programmed to be physically active and spend time outside in the sunlight most of the day, like the nomadic hunters and gatherers of forty thousand years ago.
Undeniably, we inherently conserve energy in order to heal and regenerate. This aspect of our genetic makeup also helps burn fewer calories when food is scarce. Hence the propensity for lack of movement and sedentary lifestyle (sitting disease).
In times of famine, the habit of sitting was essential because it reduced calorie expenditure, so it enabled our ancestors to survive. In a prehistoric world with a limited food supply, less movement meant fewer calories burned. Early humans became active when they needed to search for food or shelter. Today, in a world where food and shelter are abundant for most Westerners, there is no intrinsic drive to initiate movement.
It is also true that we have survived as a species by staying active. Chronic sitting is the opposite of our evolutionary pattern in which our ancestors alternated frequent movement while hunting or gathering food with periods of rest. Whether they were hunters or farmers, movement has always been an integral aspect of daily life. In contrast, working at the computer—maintaining static posture for hours on end—can increase fatigue, muscle tension, back strain, and poor circulation, putting us at risk of injury.
Quit a Sedentary Workstyle
Almost everyone is surprised by how quickly tension can build up in a muscle, and how painful it can become. For example, we tend to hover our hands over the keyboard without providing a chance for them to relax. Similarly, we may tighten some of the big muscles of our body, such as bracing or crossing our legs.
What’s needed is a chance to move a little every few minutes—we can achieve this right where we sit by developing the habit of microbreaks. Without regular movement, our muscles can become stiff and uncomfortable. When we don’t take breaks from static muscle tension, our muscles don’t have a chance to regenerate and circulate oxygen and necessary nutrients.
Build a variety of breaks into your workday:
- Vary work tasks
- Take microbreaks (brief breaks of less than thirty seconds)
- Take one-minute stretch breaks
- Fit in a moving break
Varying Work Tasks
You can boost physical activity at work by intentionally leaving your phone on the other side of the desk, situating the printer across the room, or using a sit-stand desk for part of the day. Even a few minutes away from the desk makes a difference, whether you are hand delivering documents, taking the long way to the bathroom, or pacing the room while on a call.
When you alternate the types of tasks and movement you do, using a different set of muscles, this interrupts the contractions of muscle fibers and allows them to relax and regenerate. Try any of these strategies:
- Alternate computer work with other activities, such as offering to do a coffee run
- Schedule walking meetings with coworkers
- Vary keyboarding and hand movements
Ultimately, vary your activities and movements as much as possible. By changing your posture and making sure you move, you’ll find that your circulation and your energy improve, and you’ll experience fewer aches and pains. In a short time, it usually becomes second nature to vary your activities throughout the day.
Experience It: “Mouse Shoulder” Test
You can test this simple mousing exercise at the computer or as a simulation. If you’re at the computer, sit erect with your hand on the mouse next to the keyboard. To simulate the exercise, sit with erect posture as if you were in front of your computer and hold a small object you can use to imitate mousing.
With the mouse (or a sham mouse), simulate drawing the letters of your name and your street address, right to left. Be sure each letter is very small (less than half an inch in height). After drawing each letter, click the mouse.
As part of the exercise, draw the letters and numbers as quickly as possible for ten to fifteen seconds. What did you observe? In almost all cases, you may note that you tightened your mousing shoulder and your neck, stiffened your trunk, and held your breath. All this occurred without awareness while performing the task. Over time, this type of muscle tension can contribute to discomfort, soreness, pain, or eventual injury.
Microbreaks
If you’ve developed an injury—or have chronic aches and pains—you’ll probably find split-second microbreaks invaluable. A microbreak means taking brief periods of time that last just a few seconds to relax the tension in your wrists, shoulders, and neck.
For example, when typing, simply letting your wrists drop to your lap for a few seconds will allow the circulation to return fully to help regenerate the muscles. The goal is to develop a habit that is part of your routine and becomes automatic, like driving a car. To make the habit of microbreaks practical, think about how you can build the breaks into your workstyle. That could mean a brief pause after you’ve completed a task, entered a column of data, or before starting typing out an assignment.
For frequent microbreaks, you don’t even need to get up—just drop your hands in your lap or shake them out, move your shoulders, and then resume work. Any type of shaking or wiggling movement is good for your circulation and kind of fun.
In general, a microbreak may be defined as lasting one to thirty seconds. A minibreak may last roughly thirty seconds to a few minutes, and longer large-movement breaks are usually greater than a few minutes. Popular microbreaks:
- Take a few deep breaths
- Pause to take a sip of water
- Rest your hands in your lap
- Stretch
- Let your arms drop to your sides
- Shake out your hands (wrists and fingers)
- Perform a quick shoulder or neck roll
Often, we don’t realize how much tension we’ve been carrying until we become more mindful of it. We can raise our awareness of excess tension—this is a learned skill—and train ourselves to let go of excess muscle tension. As we increase our awareness, we’re able to develop a new, more dynamic workstyle that better fits our goals and schedule.
One-Minute Stretch Breaks

We all benefit from a brief break, even with the best of posture (left). One approach is to totally release your muscles (middle). That release can be paired with a series of brief stretches (right). Reproduced from Peper, E., Harvey, R., & Faass (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books.
The typical mini-stretch break lasts from thirty seconds to a few minutes, and ideally you want to take them several times per hour. Similar to microbreaks, mini-stretch breaks are especially important for people with an injury or those at risk of injury. Taking breaks is vital, especially if you have symptoms related to computer stress or whenever you’re working long hours at a sedentary job. To take a stretch break:
Begin with a big stretch, for example, by reaching high over your head then drop your hands in your lap or to your sides.
Look away from the monitor, staring at near and far objects, and blink several times. Straighten your back and stretch your entire backbone by lifting your head and neck gently, as if there were an invisible string attached to the crown of your head.
Stretch your mind and body. Sitting with your back straight and both feet flat on the floor, close your eyes and listen to the sounds around you, including the fan on the computer, footsteps in the hallway, or the sounds in the street.
Breathe in and out over ten seconds (breathe in for four or five seconds and breathe out for five or six seconds), making the exhale slightly longer than the inhale. Feel your jaw, mouth, and tongue muscles relax. Feel the back and bottom of the chair as your body breathes all around you. Envision someone in your mind’s eye who is kind and reassuring, who makes you feel safe and loved, and who can bring a smile to your face inwardly or outwardly.
Do a wiggling movement. When you take a one-minute break, wiggling exercises are fast and easy, and especially good for muscle tension or wrist pain. Wiggle all over—it feels good, and it’s also a great way to improve circulation.
Building Exercise and Movement into Every Day
Studies show that you get more benefit from exercising ten to twenty minutes, three times a day, than from exercising for thirty to sixty minutes once a day. The implication is that doing physical activities for even a few minutes can make a big difference.
Dunstan and colleagues have found that standing up three times an hour and then walking for just two minutes reduced blood sugar and insulin spikes by twenty-five percent.Fit in a Moving Break
Fit in a Moving Break
Once we become conscious of muscle tension, we may be able to reverse it simply by stepping away from the desk for a few minutes, and also by taking brief breaks more often. Explore ways to walk in the morning, during lunch break, or right after work. Ideally, you also want to get up and move around for about five minutes every hour.
Ultimately, research makes it clear that intermittent movement, such as brief, frequent stretching throughout the day or using the stairs rather than elevator, is more beneficial than cramming in a couple of hours at the gym on the weekend. This explains why small changes can have a big impact—it’s simply a matter of reminding yourself that it’s worth the effort.
Workstation Tips
Your ability to see the display and read the screen is key to reducing neck and eye strain. Here are a few strategic factors to remember:
Monitor height: Adjust the height of your monitor so the top is at eyebrow level, so you can look straight ahead at the screen.
Keyboard height: The keyboard height should be set so that your upper arms hang straight down while your elbows are bent at a 90-degree angle (like the letter L) with your forearms and wrists held horizontally.
Typeface and font size: For email, word processing, or web content, consider using a sans serif typeface. Fonts that have fewer curved lines and flourishes (serifs) tend to be more readable on screen.
Checking your vision: Many adults benefit from computer glasses to see the screen more clearly. Generally, we do not recommend reading glasses, bifocals, trifocals, and progressive lenses as they tend to allow clear vision at only one focal length. To see through the near-distance correction of the lens requires you to tilt your head back. Although progressive lenses allow you to see both close up and at a distance, the segment of the lens for each focal length is usually too narrow for working at the computer.
Wearing progressive lenses requires you to hold your head in a fixed position to be in focus. Yet you may be totally unaware that you are adapting your eye and head movements to sustain your focus. When that is the case, most people find that special computer glasses are a good solution.
Consider computer glasses if you must either bring your nose to the screen to read the text, wear reading glasses and find that their focal length is inappropriate for the monitor distance, wear bi- or trifocal glasses, or are older than forty.
Computer glasses correct for the appropriate focal distance to the computer. Typically, monitor distance is about twenty-three to twenty-eight inches, whereas reading glasses correct for a focal length of about fifteen inches. To determine your individual, specific focal length, ask a coworker to measure the distance from the monitor to your eyes. Provide this personal focal distance at the eye exam with your optometrist or ophthalmologist and request that your computer glasses be optimized for that distance.
Remembering to blink: As we focus on the screen, our blinking rate is significantly reduced. Develop the habit of blinking periodically: at the end of a paragraph, for example, or when sending an email.
Resting your eyes: Throughout the day, pause and focus on the far distance to relax your eyes. When looking at the screen, your eyes converge, which can cause eyestrain. Each time you look away and refocus, that allows your eyes to relax. It’s especially soothing to look at green objects such as a tree that can be seen through a window.
Minimizing glare: If the room is lit with artificial light, there may be glare from your light source if the light is right in front of you or right behind you, causing reflection on your screen. Reflection problems are minimized when light sources are at a 90-degree angle to the monitor (with the light coming from the side). The worst situations occur when the light source is either behind or in front of you.
An easy test is to turn off your monitor and look for reflections on the screen. Everything that you see on the monitor when it’s turned off is there when you’re working at the monitor. If there are bright reflections, they will interfere with your vision. Once you’ve identified the source of the glare, change the location of the reflected objects or light sources, or change the location of the monitor.
Contrast: Adjust the light contrast in the room so that it is neither too bright nor too dark. If the room is dark, turn on the lights. If it is too bright, close the blinds or turn off the lights. It is exhausting for your eyes to have to adapt from bright outdoor light to the lighting of your computer screen. You want the light intensity of the screen to be somewhat similar to that in the room where you’re working. You also do not want to look from your screen to a window lit by intense sunlight.
Don’t look down at phone: According to Kenneth Hansraj, MD, chief of spine surgery at New York Spine Surgery and Rehabilitation Medicine, pressure on the spine increases from about ten pounds when you are holding your head erect, to sixty pounds of pressure when you are looking down. Bending forward to look at your phone, your head moves out of the line of gravity and is no longer balanced above your neck and spine. As the angle of the face-forward position increases, this intensifies strain on the neck muscles, nerves, and bones (the vertebrae).
The more you bend your neck, the greater the stress since the muscles must stretch farther and work harder to hold your head up against gravity. This same collapsed head-forward position when you are seated and using the phone repeats the neck and shoulder strain. Muscle strain, tension headaches, or neck pain can result from awkward posture with texting, craning over a tablet (sometimes referred to as the iPad neck), or spending long hours on a laptop.
A face-forward position puts as much as sixty pounds of pressure on the neck muscles and spine.
Repetitive strain of neck vertebrae (the cervical spine), in combination with poor posture, can trigger a neuromuscular syndrome sometimes diagnosed as thoracic outlet syndrome. According to researchers Sharan and colleagues, this syndrome can also result in chronic neck pain, depression, and anxiety.
When you notice negative changes in your mood or energy, or tension in your neck and shoulders, use that as a cue to arch your back and look upward. Think of a positive memory, take a mindful breath, wiggle, or shake out your shoulders if you’d like, and return to the task at hand.
Strengthen your core: If you find it difficult to maintain good posture, you may need to strengthen your core muscles. Fitness and sports that are beneficial for core strength include walking, sprinting, yoga, plank, swimming, and rowing. The most effective way to strengthen your core is through activities that you enjoy.
Final Thoughts
If these ideas resonate with you, consider lifestyle as the first step. We need to build dynamic physical activity into our lives, as well as the lives of our children. Being outside is usually an uplift, so choose to move your body in natural settings whenever possible, whatever form that takes. Being outside is the factor that adds an energetic dimension. Finally, share what you learn, and help others learn and grow from your experiences.
If you spend time in front of a computeror using a mobile device, read the book, TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. It provides practical, easy-to-use solutions for combating the stress and pain many of us experience due to technology use and overuse. The book offers extremely helpful tips for ergonomic use of technology, it
goes way beyond that, offering simple suggestions for improving muscle health that seem obvious once you read them, but would not have thought of yourself: “Why didn’t I think of that?” You will learn about the connection between posture and mood, reasons for and importance of movement breaks, specific movements you can easily perform at your desk, as well as healthier ways to utilize technology in your everyday life.
See the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics by Erik Peper, Richard Harvey and Nancy Faass. Available from: https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/
Additional resources
Are food companies responsible for the epidemic in diabetes, cancer, dementia and chronic disease and do their products need to be regulated like tobacco? Is it time for a class action suit?
Posted: July 15, 2023 Filed under: behavior, cancer, Evolutionary perspective, health, Nutrition/diet, self-healing | Tags: dementia, diabetes, diet, high fructose corn syrup, mortality, obsity, smoking, sugar, ultra-processed foods, UPF 4 CommentsAdapted from: Peper, E. & Harvey, R. (2024). Are Food Companies Responsible for the Epidemic in Diabetes, Cancer, Dementia and Chronic Disease and Do Their Products Need to Be Regulated Like Tobacco? Is It Time for a Class Action Suit? Thownsend Letter-the examiner of alternative medicine. https://www.townsendletter.com/e-letter-26-ultra-processed-foods-and-health-issues/
Erik Peper, PhD and Richard Harvey, PhD

Why are one third of young Americans becoming obese and at risk for diabetes?
Why are heart disease, cancer, and dementias occurring earlier and earlier? Is it genetics, environment, foods, or lifestyle?
Is it individual responsibility or the result of the quest for profits by agribusiness and the food industry?
Like the tobacco industry that sells products regulated because of their public health dangers, is it time for a class action suit against the processed food industry? The argument relates not only to the regulation of toxic or hazardous food ingredients (e.g., carcinogenic or obesogenic chemicals) but also to the regulation of consumer vulnerabilities. Addressing vulnerabilities to tobacco products include regulations such as how cigarette companies may not advertise their products for sale within a certain distance from school grounds.
Is it time to regulate nationally the installation of vending machines on school grounds selling sugar-sweetened beverages? Students have sensitivity to the enticing nature of advertised, and/or conveniently available consumable products such as ‘fast foods’ that are highly processed (e.g., packaged, preserved and practically imperishable). Whereas ‘processed foods’ have some nutritive value, and may technically pass as ‘nutritious’ food, the quality of processed ‘nutrients’ can be called into question. For the purpose of this blog other important questions to raise relate to ingredients which, alone or in combination, may contribute to the onset of or, the acceleration of a variety of chronic health outcomes related to various kinds of cancers, cardiovascular diseases, and diabetes.
It may be an over statement to suggest that processed food companies are directly responsible for the epidemic in diabetes, cancer, dementia and chronic disease and need to be regulated like tobacco. On the other hand, processed food companies should become much more regulated than they are now.
More than 80 years ago, smoking was identified as a significant factor contributing to lung cancer, heart disease and many other disorders. In 1964 the Surgeon Generals’ report officially linked smoking to deaths of cancer and heart disease (United States Public Health Service, 1964). Another 34 years pased before California prohibited smoking in restaurants in 1998 and, eventually inside all public buildings. The harms of smoking tobacco products were well known, yet many years passed with countless deaths and suffering which could have been prevented before regulation of tobacco products took place. Reviewing historical data there is about a 20 year delay (e.g., a whole generation) before death rates decrease in relation to when regulations became effective and smoking rates decreased, as shown in figure 1.

Figure 1. The relationship between smoking and lung cancer. Reproduced by permission from Roser, M. (2021). Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data.
During those interim years before government actions limited smoking more effectively, tobacco companies hid data regarding the harmful effects of smoking. Arguably, the ‘Big Tobacco’ industry paid researchers to publish data which could confuse readers about tobacco product harm. There is evidence of some published articles suggesting that the harm of cigarette smoking was a hoax– all for the sake of boosting corporate profits (Bero, 2005).
Now we are experiencing a similar problem with the processed food industry. It has been suggested that alongside smoking and vaping, opioid use, a sedentary ‘couch potato’ lifestyle, and lack of exercise, ultra-processed food (UPF) that we eat severely affects our health.
Ultra-processed foods, which for many constitutes a majority of calories ranging from 55% to over 80% of the food they eat, contain chemical additives that trick the tastebuds, mouth and eventually our brain to desire those processed foods and eat more of them (Srour et al., 2022).
What are ultra-processed foods? Any foods that your great grandmother would not recognize as food. This includes all soft drinks, highly processed chips, additives, food coloring, stabilizers, processed proteins, etc. Even oils such as palm oil, canola oil, or soybean are ultra processed since they heated, highly processed with phosphoric acid to remove gums and waxes, neutralized with chemicals, bleached, and deodorized with high pressure steam (van Tulleken, 2023).
The data is clear! Since the 1970s obesity and inflammatory disease have exploded after ultra-processed foods became the constituents of the modern diet as shown in figure 2.

Figure 2. A timeline from 1850 to 2000 reflects the increase in use of refined sugar and high fructose corn syrup (HFCS) to the U.S. diet, together with the increase in U.S. obesity rate. The data for sugar, dairy and HFCS consumption per capita are from USDA Economic Research Service (Johnson et al., 2009) and reflects historical estimates before 1967 (Guyenet et al., 2017). The obesity data (% of U.S. adult population) are from the Robert Wood Johnson Foundation’s Trust for America’s Health. (stateofobesity.org). Total U.S. television advertising data are from the World Advertising Research Center (www.warc.com). The vertical measure (y–axis) for kilograms per year (kg/yr) on the left covers all data except advertising expenditures, which uses the vertical measure for advertising on the right. Reproduced by permission from Bentley et al, 2018.
This graph clearly shows a close association between the years that high fructose corn syrups (HFCS) were introduced into the American diet and an increase in TV advertising with corresponding increase in obesity. HFCS is an ultra-processed food and is a surrogate marker for all other ultra-processed foods. The best interpretation is that ultra-processed foods, which often contain HFCS, are a causal factor of the increase in obesity, and diabetes and in turn are risk factors for heart disease, cancers and dementias.
Ultra-processed foods are novel from an evolutionary perspective.
The human digestive system has only recently encountered sources of calories which are filled with so many unnatural chemicals, textures and flavors. Ultra-processed foods have been engineered, developed and product tested to increase the likelihood they are wanted by consumers and thereby increase sales and profits for the producers. These foods contain the ‘right amount’ processed materials to evoke the taste, flavor and feel of desired foods that ‘trick’ the consumer it eat them because they activate evolutionary preference for survival. Thus, these ultra-processed foods have become an ‘evolutionary trap’ where it is almost impossible not to eat them. We eat the food because it capitalized on our evolutionary preferences even though doing so is ultimately harmful for our health (for a detailed discussion on evolutionary traps, see Peper, Harvey & Faass, 2020).
An example is a young child wanting the candy while waiting with her parents at the supermarket checkout line. The advertised images of sweet foods trigger the cue to eat. Remember, breast milk is sweet and most foods in nature that are sweet in taste, provide calories for growth and survival and are not harmful. Calories are essential of growth. Thus, we have no intrinsic limit on eating sweets unlike foods that taste bitter.
As parents, we wish that our children (and even adults) have self-control and no desire to eat the candy or snacks that is displayed at eye level (eye candy) especially while waiting at the cashier. When reflecting about food advertising and the promotion of foods that are formulated to take advantage of ‘evolutionary traps’, who is responsible? Is it the child, who does not yet have the wisdom and self-control or, is it the food industry that ultra-processes the foods and adds ingredients into foods which can be harmful and then displays them to trigger an evolutionary preference for food that have been highly processed?
Every country that has adapted the USA diet of ultra-processed foods has experienced similar trends in increasing obesity, diabetes, cardiovascular disease, etc. The USA diet is replacing traditional diets as illustrated by the availability of Coca-Cola. It is sold in over 200 countries and territories (Coca-Cola, 2023).
An increase in ultra-processed foods by 10 percent was associated with a 25 percent increase in the risk of dementia and a 14 per cent increase in the risk of Alzheimers’s (Li et al., 2022). More importantly, people who eat the highest proportion of their diet in ultra-processed foods had a 22%-62% increased risk of death compared to the people who ate the lowest proportion of processed foods (van Tulleken, 2023). In the USA, counties with the highest food swamp scores (the availability of fast food outlets in a county) had a 77% increased odds of high obesity-related cancer mortality (Bevel et al., 2023). The increase risk has also been observed for cardiovascular disease, coronary heart disease, cerebrovascular disease and all cause mortality as is shown in figure 3 (Srour et al., 2019; Rico-Campà et al., 2019).

Figure 3. Association between consumption of ultra-processed foods and all cause mortality. Reproduced from Rico-Campà et al, 2019.
The harmful effects of UPF holds up even when correcting for the amount of sugars, carbohydrates or fats in the diet and controlling for socio economic variables.
The logic that underlies this perspective is based upon the writing by Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto). He provides an evolutionary perspective and offers broad and simple rules of health as well as recommendations for reducing UPF risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, added sugars, textured proteins, gums, stabilizers (guar gum, sodium alginate), emulsifiers (mono-and di-glycerides), modified starches, dextrose, palm stearin, and fats, colors and artificial flavoring or other ultra-processed food additives).
What can we do?
The solutions are simple and stated by Michael Pollan in his 2007 New York Times article, “Eat food. Not too much. Mostly Plants.” Eat foods that your great grandmother would recognize as foods (Pollan, 2009). Do not eat any of the processed foods that fill a majority of a supermarket’s space.
- Buy only whole organic natural foods and prepare them yourself.
- Request that food companies only buy and sell non-processed foods.
- Demand government action to tax ultra-processed food and limit access to these foods. In reality, it is almost impossible to expect people to choose healthy, organic foods when they are more expensive and not easily available in the American ‘food swamps and deserts’ (the presence of many fast food outlets or the absence of stores that have fresh produce and non-processed foods). We do have a choice. We can spend more money now for organic, health promoting foods or, pay much more later to treat illness related to UPF.
- It is time to take our cues from the tobacco wars that led to regulating tobacco products. We may even need to start class action suits against producers and merchants of UPF for causing increased illness and premature morbidity.
For more background information and the science behind this blog, read, the book, Ultra-processed people, by Chris van Tulleken.

Look at the following blogs for more background information.
References
Bentley, R.A., Ormerod, P. & Ruck, D.J. (2018). Recent origin and evolution of obesity-income correlation across the United States. Palgrave Commun 4, 146. https://doi.org/10.1057/s41599-018-0201-x
Bero, L. A. (2005). Tobacco Industry Manipulation of Research. Public Health Reports (1974-), 120(2), 200–208. http://www.jstor.org/stable/20056773
Bevel, M.S., Tsai, M., Parham, A., Andrzejak, S.E., Jones, S., & Moore, J.X. (2023). Association of Food Deserts and Food Swamps With Obesity-Related Cancer Mortality in the US. JAMA Oncol. 9(7), 909–916. https://doi.org/10.1001/jamaoncol.2023.0634
Coca-Cola. (2023). More on Coca-Cola. Accessed July 14, 2023. https://www.coca-cola.co.uk/our-business/faqs/how-many-countries-sell-coca-cola-is-there-anywhere-in-the-world-that-doesnt
Johnson, R.K., Appel, L.J., Brands, M., Howard, B.V., Lefevre, M., Lustig, R.H., Sacks, F., Steffen, L.M., & Wylie–Rosett, J. (2009). Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation, 120(10), 1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Li, H., Li, S., Yang, H., et al, 2022. Association of ultraprocessed food consumption with the risk of dementia: a prospective cohort study. Neurology, 99, e1056-1066. https://doi.org/10.1212/WNL.0000000000200871
Peper, E., Harvey, R. & Faass, N. (2020). TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics. Berkeley: North Atlantic Books, pp 18-22, 151. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/ref=sr_1_1?crid=1U9Y82YO4DKKP&keywords=erik+peper&qid=1689372466&sprefix=erik+peper%2Caps%2C187&sr=8-1
Pollan, M. (2007). Unhappy meals. The New York Times Magazine. https://www.nytimes.com/2007/01/28/magazine/28nutritionism.t.html
Pollan, M. (2009). Food Rules: An Eater’s Manual. New York: Penguin Books. https://www.amazon.com/Food-Rules-Eaters-Michael-Pollan/dp/014311638X/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1689373484&sr=8-2
Rico-Campà, A., Martínez-González, M. A., Alvarez-Alvarez, I., de Deus Mendonça, R., Carmen de la Fuente-Arrillaga, C., Gómez-Donoso, C., & Bes-Rastrollo, M. (2019). Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ; 365: l1949 https://doi.org/10.1136/bmj.l1949
Roser, M. (2021).Smoking: How large of a global problem is it? And how can we make progress against it? Our world in data. Assessed July 13, 2023. https://ourworldindata.org/smoking-big-problem-in-brief
Srour, B., Fezeu, L.K., Kesse-Guyot, E.,Alles, B., Mejean, C…(2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé) BMJ,365:l1451. https://doi.org/10.1136/bmj.l1451
Srour, B., Kordahi, M. C., Bonazzi, E., Deschasaux-Tanguy, M., Touvier, M., & Chassaing, B. (2022). Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. The Lancet Gastroenterology & Hepatology. https://doi.org/10.1016/S2468-1253(22)00169-8
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto). New York: Random House Publishing Group. (Kindle Locations 5906-5908). https://www.amazon.com/Antifragile-Things-Disorder-ANTIFRAGILE-Hardcover/dp/B00QOJ6MLC/ref=sr_1_4?crid=3BISYYG0RPGW5&keywords=Antifragile%3A+Things+That+Gain+from+Disorder+%28Incerto%29&qid=1689288744&s=books&sprefix=antifragile+things+that+gain+from+disorder+incerto+%2Cstripbooks%2C158&sr=1-4
Van Tulleken, C. (2023). Ultra-processed people. The science behind food that isn’t food. New Yoerk: W.W. Norton & Company. https://www.amazon.com/gp/product/1324036729/ref=ox_sc_act_title_1?smid=ATVPDKIKX0DER&psc=1
United States Public Health Service. (1964). The 1964 Report on Smoking and Health. United States. Public Health Service. Office of the Surgeon General. https://profiles.nlm.nih.gov/spotlight/nn/catalog?f%5Bexhibit_tags%5D%5B%5D=smoking
Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythm
Posted: July 4, 2023 Filed under: ADHD, behavior, computer, digital devices, education, emotions, Evolutionary perspective, health, laptops, screen fatigue, Uncategorized | Tags: anxiety, autism, bonding, circadian rhythms, depression, nature, still face experiment 10 Comments
Adapted from: Peper, E. Reflections on the increase in Autism, ADHD, anxiety and depression: Part 1-bonding, screen time, and circadian rhythms. NeuroRegulation,10(2), 134-138. https://doi.org/10.15540/nr.10.2.134
Over the past two decades, there has been a significant increase in the prevalence of autism, Attention-Deficit/hyperactivity disorder (ADHD), anxiety, depression, and pediatric suicidal behavior. Autism rates have risen from 1 in 150 children in 2000 to 1 in 36 children in 2020 (CDC, 2023), while ADHD rates have increased from 6% in 1997 to approximately 10% in 2018 (CDC, 2022). The rates of anxiety among 18-25 year-olds have also increased from 7.97% in 2008 to 14.66% in 2018 (Goodwin et al., 2020), and depression rates for U.S. teens ages 12-17 have increased from 8% in 2007 to 13% in 2017 (Geiger & Davis, 2019; Walrave et al., 2022). Pediatric suicide attempts have also increased by 163% from 2009 to 2019 (Arakelyan et al., 2023), and during the COVID-19 pandemic, these rates have increased by more than 25% (WHO, 2022; Santomauro et al., 2021). In addition, the prevalence of these disorders has tripled for US adults during the pandemic compared to before (Ettman et al., 2020).
The rapid increase of these disorders is not solely due to improved diagnostic methods, genetic factors or the COVID-19 pandemic. The pandemic amplified pre-existing increasing trends. More likely, individuals who were at risk had their disorders triggered or amplified by harmful environmental and behavioral factors. Conceptually, Genetics loads the gun; epigenetics, behavior, and environment pull the trigger.
While behavioral strategies such as neurofeedback, Cognitive Behavior Therapy, biofeedback, meditation techniques, and pharmaceuticals can treat or ameliorate these disorders, the focus needs to be on risk reduction. In some ways, treatment can be likened to closing the barn doors after the horses have bolted.
Evolutionary perspective to reduce risk factors
Nassim Taleb (2012) in his book, Antifragile: Things That Gain from Disorder (Incerto), provides an evolutionary perspective and offers simple rules of health by reducing risk factors:
- Assume that anything that was not part of our evolutionary past is probably harmful.
- Remove the unnatural/unfamiliar (e.g. smoking/ e-cigarettes, sugar, digital media).
- We do not need evidence of harm to claim that a drug or an unnatural procedure is dangerous. If evidence of harm does not exist, it does not mean harm does not exist.
- Only resort to medical techniques when the health payoff is very large (to save a life), exceeds its potential harm, such as incontrovertibly needed surgery or life-saving medicine (penicillin).
- Avoid the iatrogenics and negative side effects of prescribed medication.
Writer and scholar Taleb’s suggestions are reminiscent of the perspective described by the educator Joseph C. Pearce (1993) in his book, Evolution’s End. Pearce argued that modern lifestyles have negatively affected the secure attachment and bonding between caregivers and infants. The lack of nurturing and responsive caregiving in early childhood may lead to long-term emotional and psychological problems. He points out that we have radically adapted behaviors that differ from those that evolved over thousands of generations and that allowed us to thrive and survive. In the last 100 years, babies have often been separated from their mothers at birth or early infancy by being put in a nursery or separate room, limited or no breastfeeding with the use of formula, exposure to television for entertainment, lack of exploratory play outdoors, and the absence of constant caretakers in high-stress and unsafe environments.
As Pearce pointed out, “If you want true learning, learning that involves the higher frontal lobes – the intellectual, creative brain – then again, the emotional environment must be positive and supportive. This is because at the first sign of anxiety the brain shifts its functions from the high, prefrontal lobes to the old defenses of the reptilian brain… These young people need audio-vocal communication, nurturing, play, body movement, eye contact, sweet sounds and close heart contact on a physical level” (Mercogliano & Debus, 1999).
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past. The proposed recommendations are based upon Talib’s perspective that anything that was not part of our evolutionary past is probably harmful; thus, it is wise to remove the unnatural/unfamiliar and adopt the precautionary principle, which states that if evidence of harm does not exist, it does not mean harm does not exist (Kriebel et al., 2010).
This article is the first of a three-part series. Part 1 focuses on increasing reciprocal communication between infant and caretaker, reducing screen time, and re-establishing circadian rhythms; Part 2 focuses on reducing exposure to neurotoxins, eliminating processed foods, and supporting the human biome; and Part 3 focuses on respiration and movement.
Part 1- Increase bonding, reduce screen time, and re-establish circadian rhythms
Increase bonding between infant and caretaker
Infants develop emotional communication through reciprocal interactions with their caregivers, during which the caregiver responds to the infant’s expressions. When this does not occur, it can be highly stressful and detrimental to the infant’s development. Unfortunately, more and more babies are emotionally and socially isolated while their caregivers are focussed on, and captured by, the content on their digital screens. Moreover, infants and toddlers are entertained (babysat) by cellphones and tablets instead of dynamically interacting with their caretakers. Screens do not respond to the child’s expressions; the screen content is programmed to capture the infant’s attention through rapid scene changes. Without reciprocal interaction, babies often become stressed, as shown by the research of developmental psychologist Professor Edward Tronick, who conducted the “Still Face” experiment (Tronick & Beeghly, 2011; Weinberg et al, 2008).
The “Still Face” experiment illustrated what happens when caregivers are not responding to infants’ communication. The caregivers were asked to remain still and unresponsive to their babies, resulting in the infants becoming increasingly distressed and disengaged from their surroundings. Not only does this apply to infants but also to children, teenagers and older individuals. Watch the short Still Face experiment, which illustrates what happens when the caretaker is not responding to the infant’s communication.
Recommendation. Do not use cellphone and digital media while being with an infant in the first two years of life. It is important for caregivers to limit their cellphone use and prioritize reciprocal interactions with their infants for healthy emotional and psychological development.
Reduce screen time (television, social media, streaming videos, gaming)[1]
From an evolutionary perspective, screen time is an entirely novel experience. Television, computers, and cellphones are modern technologies that have significantly impacted infants’ and young people’s development. To grow, infants, toddlers, and children require opportunities to explore the environment through movement, touch, and play with others, which is not possible with screens. Research has shown that excessive screen time can negatively affect children’s motor development, attention span, socialization skills, and contribute to obesity and other health problems (Hinkley et al., 2014; Carson et al., 2016; Mark, 2023).
When four-year-olds watch fast-paced videos, they exhibit reduced executive functions and impulse control, which may be a precursor for ADHD, compared to children who engage in activities such as drawing (Lillard & Peterson, 2011; Mark, 2023).
Furthermore, excessive screen time and time spent on social media are causal in increasing depression in young adults-–as was discovered when Facebook became available at selected universities. Researchers compared the mental health of students at similar universities where Facebook was or was not available and observed how the students’ mental health changed when Facebook became available (Braghieri et al., 2022). Their research showed that “College-wide access to Facebook led to an increase in severe depression by 7% and anxiety disorders by 20%. In total, the negative effect of Facebook on mental health appeared to be roughly 20% the magnitude of what is experienced by those who lose their job” (Walsh, 2022).
Exposure to digital media has also significantly reduced our attention span from 150 seconds in 2004 to an average of 44 seconds in 2021. The shortening of attention span may contribute to the rise of ADHD and anxiety (Mark, 2022, p. 96).
Recommendations: Reduce time spent on social media, gaming, mindlessly following one link after the other, or watching episode after episode of streaming videos. Instead, set time limits for screen use, turn off notifications, and prioritize in-person interactions with friends, family and colleagues while engaging in collaborative activities. Encourage children to participate in physical and social activities and to explore nature.
To achieve this, follow the guidelines from the American Academy of Pediatrics’ recommendation on screen time (Council on Communications and Media, 2016), which suggest these limits on screen time for children of different age groups:
- Children under 18 months of age should avoid all screen time, except for video chatting with family and friends.
- Children aged 18-24 months should have limited screen time, and only when watched together with a caretaker.
- Children aged 2 to 5 years should have no more than one hour of screen time per day with parental supervision.
- For adolescents, screen and social media time should be limited to no more than an hour a day.
In our experience, when college students reduce their time spent on social media, streaming videos, and texting, they report that it is challenging; however, they then report an increase in well-being and performance over time (Peper et al., 2021). It may require more effort to provide children with actual experiential learning and entertainment than allowing them to use screens, but it is worthwhile. Having children perform activities and play outdoors–in a green nature environment–appears to reduce ADHD symptoms (Louv, 2008; Kuo & Taylor, 2004).
Reestablish circadian (daily) rhythms
Our natural biological and activity rhythms were regulated by natural light until the 19th century. It is hard to imagine not having light at night to read, to work on the computer, or to answer email. However, light not only illuminates, but also affects our physiology by regulating our biological rhythms. Exposure to light at night can interfere with the production of melatonin, which is essential for sleep. Insufficient sleep affects 30% of toddlers, preschoolers, and school-age children, as well as the majority of adolescents. The more media is consumed at bedtime, the more bedtime is delayed and total sleep time is reduced (Hale et al., 2018). Reduced sleep is a contributing factor to increased ADHD symptoms of inattention, hyperactivity and impulsivity (Cassoff et al., 2012).
Recommendations: Support the circadian rhythms. Avoid screen time one hour before bedtime. This will reduce exposure to blue light and reduce sympathetic arousal triggered by the content on the screen or reactions to social media and emails. Sleep in total darkness, and establish a regular bedtime and waking time to avoid “social jetlag,” which can negatively affect health and performance (Caliandro et al., 2021). Implement sleep hygiene strategies such as developing a bedtime ritual to improve sleep quality (Stager et al., 2023; Suni, 2023). Thus, go to bed and wake up at the same time each day, including weekends. Avoid large meals, caffeine, and alcohol before bedtime. Consistency is key to success.
Conclusion
To optimize health, eliminate or reduce those factors that have significantly changed or were not part of our evolutionary past, and explore strategies that support behaviors that have allowed the human being to thrive and survive. Improve clinical outcomes and optimize health by enhancing reciprocal communication interactions, reducing screen time and re-establishing the circadian rhythm.
References
Arakelyan, M., Freyleue, S., Avula, D., McLaren, J.L., O’Malley, A.J., & Leyenaar, J.K. (2023). Pediatric Mental Health Hospitalizations at Acute Care Hospitals in the US, 2009-2019. JAMA, 329(12), 1000–1011. https://doi.org/10.1001/jama.2023.1992
Braghieri, L., Levy, R., & Makarin, A. (2022). Social Media and Mental Health (July 28, 2022). Available at SSRN: https://ssrn.com/abstract=3919760 or http://dx.doi.org/10.2139/ssrn.3919760
Caliandro, R., Streng, A.A., van Kerkhof, L.W.M., van der Horst, G.T.J., & Chaves, I. (2021). Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients, 13(12), 4543. https://doi.org/10.3390/nu13124543
Carson, V., Tremblay, M.S., Chaput, J.P., & Chastin, S.F. (2016). Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab, 41(6 Suppl 3), S294-302. https://doi.org/10.1139/apnm-2016-0026
Cassoff, J., Wiebe, S.T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nat Sci Sleep, 4, 73-80. https://doi.org/10.2147/NSS.S31269
CDC. (2022). Attention-Deficit/hyperactivity disorder (ADHD): ADHD through the years. Centers for Disease Control and Prevention. Assessed March 27, 2023. https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. (2023). Data & Statistics on Autism Spectrum Disorder. CDC Centers for Disease Control and Prevention. Assessed March 25, 2023. https://www.cdc.gov/ncbddd/autism/data.html
Council on Communications and Media. (2016). Media and young minds. Pediatrics, 138(5), e20162591. https://doi.org/10.1542/peds.2016-2591
Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M.,& Galea, S. (2020), Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Geiger, A.W. & Davis, L. (2019). A growing number of American teenagers-particularly girls-are facing depression. Pew Research Center. Accessed March 28, 2023.
Goodwin, R.D., Weinberger, A.H., Kim, J.H., Wu. M., & Galea, S. (2020). Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. J Psychiatr Res. 130, 441-446. https://doi.org/10.1016/j.jpsychires.2020.08.014
Hale, L., Kirschen, G/W., LeBourgeois, M.K., Gradisar, M., Garrison, M.M., Montgomery-Downs, H., Kirschen, H., McHale, S.M., Chang, A.M., & Buxton, O.M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc Psychiatr Clin N Am, 27(2),229-245. https://doi.org/10.1016/j.chc.2017.11.014
Hinkley, T., Verbestel, V., Ahrens, W., Lissner, L., Molnár, D., Moreno, L.A., Pigeot, I., Pohlabeln, H., Reisch, L.A., Russo, P., Veidebaum, T., Tornaritis, M., Williams, G., De Henauw, S., De Bourdeaudhuij, I; IDEFICS Consortium. (2014). Early childhood electronic media use as a predictor of poorer well-being: a prospective cohort study. JAMA Pediatr,. May;168(5):485-92. https://doi.org/10.1001/jamapediatrics.2014.94
Kriebel, D., Tickner, J., Epstein, P., Lemons, J., Levins, R., Loechler, E.L., Quinn, M., Rudel, R., Schettler, T., Stoto, M. (2001). The precautionary principle in environmental science. Environ Health Perspect, 109(9):871-6. https://doi.org/10.1289/ehp.01109871
Kuo. F.E. & Taylor, A.F. (2004). A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 94(9),1580-6. https://doi.org/10.2105/ajph.94.9.1580
Lillard, A.S. & Peterson, J. The immediate impact of different types of television on young children’s executive function. Pediatrics, 128(4), 644-9. https://doi.org/10.1542/peds.2010-1919
Louv, R. (2008). Last Child in the Woods: Saving Our Children from Nature-Deficit Disorder. Algonquin Books. Chapel Hill, NC: Algonquin Books
Mark, G. (2023). Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Toronto, Canada: Hanover Square Press.
Mercogliano, C. & Debus, K. (1999). Nurturing Heart-Brain Development Starting With Infants 1999 Interview with Joseph Chilton Pearce. Journal of Family Life, 5(1). https://www.michaelmount.co.za/nurturing-heart-brain-development-starting-with-infants-1999-interview-with-joseph-chilton-pearce/
Pearce, J.C. (1993). Evolutions’s End. New York: HarperOne.
Peper, E., Wilson, V., Martin, M., Rosegard, E., & Harvey, R. (2021). Avoid Zoom fatigue, be present and learn. NeuroRegulation, 8(1), 47–56. https://doi.org/10.15540/nr.8.1.47
Santomauro, D.F., Mantilla Herrera, A.M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D.M., Abbafati, C., Adolph, C., …. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(103121700-1712., https://doi.org/10.1016/S0140-6736(21)02143-7
Stager, L.M., Caldwell, A., Bates, C., & Laroche, H. (2023). Helping kids get the sleep they need. Society of Behavioral Medicine. Accessed March 29, 2023 https://www.sbm.org/healthy-living/helping-kids-get-the-sleep-they-need?gclid=Cj0KCQjww4-hBhCtARIsAC9gR3ZM7v9VSvqaFkLnceBOH1jIP8idiBIyQcqquk5y_RZaNdUjAR9Wpx4aAhTBEALw_wcB
Suni, E. (2023). Sleep hygiene- What it is, why it matters, and how to revamp your habits to get better nightly sleep. Sleep Foundation. Accessed March 29, 2023. https://www.sleepfoundation.org/sleep-hygiene
Taleb, N. N. (2012). Antifragile: Things That Gain from Disorder (Incerto) Random House Publishing Group. (Kindle Locations 5906-5908).
Tronick, E. & Beeghly, M. (2011).Infants’ meaning-making and the development of mental health problems. Am Psychol, 66(2),107-19. https://doi.org/10.1037/a0021631
Walrave, R., Beerten, S.G., Mamouris, P. et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 23, 163 (2022). https://doi.org/10.1186/s12875-022-01769-w
Walsh, D. (2022 September 14). Study: Social media use linked to decline in mental health. MIT Management Ideas Made to Matter. Accessed March 28, 2023. https://mitsloan.mit.edu/ideas-made-to-matter/study-social-media-use-linked-to-decline-mental-health#:~:text=College%2Dwide%20access%20to%20Facebook,with%20either%20psychotherapy%20or%20antidepressants
Weinberg, M.K., Beeghly, M., Olson, K.L., & Tronick, E. (2008). A Still-face Paradigm for Young Children: 2½ Year-olds’ Reactions to Maternal Unavailability during the Still-face. J Dev Process, 3(1):4-22. https://pubmed.ncbi.nlm.nih.gov/22384309/
WHO (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. Assessed march 26, 2023. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide
[1] The critique of social media does not imply that there are no benefits. If used judiciously, it is a powerful tool to connect with family and friends or access information.
Mouth breathing and tongue position: a risk factor for health
Posted: June 8, 2023 Filed under: ADHD, behavior, Breathing/respiration, cognitive behavior therapy, Evolutionary perspective, healing, health, Nutrition/diet, self-healing, Uncategorized | Tags: babies, breastfeedging, development, infants, jaw, mouth breathing, neurocognitive develoment, nose breathing, sleep, tongue-tie Leave a commentErik Peper, PhD, BCB and Ron Swatzyna, PhD, LCSW, BCB, BCN
Adapted from: Peper, E., Swatzyna, R., & Ong, K. (2023). Mouth breathing and tongue position: a risk factor for health. Biofeedback. 51(3), 74–78 https://doi.org/10.5298/912512

Breathing usually occurs without awareness unless there are problems such as asthma, emphysema, allergies, or viral infections. Infant and child development may affect how we breathe as adults. This blog discusses the benefits of nasal breathing, factors that contribute to mouth breathing, how babies’ breastfeeding and chewing decreases the risk of mouth breathing, recommendations that parents may implement to support healthy development of a wider palate, and the embedded video presentation, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development, by Karindy Ong, MA, CCC-SLP, CFT, .
Benefits of nasal breathing
Breathing through the nose filters, humidifies, warms, or cools the inhaled air as well as reduces the air turbulence in the upper airways. In addition, the epithelial cells of the nasal cavities produce nitric oxide that are carried into the lungs when inhaling during nasal breathing (Lundberg & Weitzberg, 1999). The nitric oxide contributes to healthy respiratory function by promoting vasodilation, aiding in airway clearance, exerting antimicrobial effects, and regulating inflammation. Breathing through the nose is associated with deeper and slower breathing rate than mouth breathing. This slower breathing also facilitates sympathetic parasympathetic balance and reduces airway irritation.
Mouth breathing
Some people breathe predominantly through their mouth although nose breathing is preferred and health promoting. Mouth breathing negatively impacts the ability to perform during the day as well as affect our cognitions and mood (Nestor, 2020). It contributes to disturbed sleep, snoring, sleep apnea, dry mouth upon waking, fatigue, allergies, ear infections, attention deficit disorders, crowded mis-aligned teeth, and poorer quality of life (Kahn & Ehrlich, 2018). Even the risk of ear infections in children is 2.4 time higher for mouth breathers than nasal breathers (van Bon et al, 1989) and nine and ten year old children who mouth breath have significantly poorer quality of life and have higher use of medications (Leal et al, 2016).
One recommendation to reduce mouth breathing is to tape the mouths closed with mouth tape (McKeown, 2021). Using mouth tape while sleeping bolsters nose breathing and may help people improve sleep, reduce snoring, and improves alertness when awake (Lee et al, 2022).
Experience how mouth breathing affects the throat and upper airway
Inhale quickly, like a gasp, as much air as possible through your open mouth. Exhale letting the air flow out through your mouth. Repeat once more.
Inhale quickly as much air through the nose, then exhale by allow the airflow out through the nose. Repeat once more.
What did you observe? Many people report that rapidly inhaling through the mouth causes the back of the throat and even upper airways to feel drier and irritated. This does not occur when inhaling through the nose. This simple experiment illustrates how habitual mouth breathing may irritate the airways.
Developmental behavior that contributes to mouth breathing
The development of mouth breathing may begin right at birth when the mouth, tongue, jaw and nasal area are still developing. The arch of the upper palate forms the roof of the oral cavity that separates the oral and nasal cavities. When the palate and jaw narrows, the arch of the palate increases and pushes upwards into the nasal area. This reduces space in the nasal cavity for the air to flow and obstructs nasal breathing. The highly vaulted palate is not only genetically predetermined but also by how we use our tongue and jaw from birth. The highly arched palate is only a recent anatomical phenomena since the physical structure of the upper palate and jaw from the pre- industrial era was wider (less arched upper palate) than many of our current skulls (Kahn & Ehrlich, 2018).
The role of the tongue in palate development
After babies are born, they breastfeed by sucking with the appropriate tongue movements that help widen the upper palate and jaw. On the other hand, when babies are bottle fed, the tongue tends to move differently which causes the cheek to pull in and the upper palate to arch which may create a high narrow upper palate and making the jaw narrower. There are many other possible factors that could cause mouth breathing such as tongue-tie (ankyloglossia), septal deviation, congenital malformation, enlarged adenoids and tonsils (Aden tonsillar hyperplasia), inflammatory diseases such as allergic rhinitis (Trabalon et al, 2012). Whatever the reasons, the result of the impoverished tongue movement and jaw increases the risk for having a higher arched upper palate that impedes nasal breathing and contributes to habitual mouth breathing.
The forces that operate on the mouth, jaw and palate during bottle feeding may be similar to when you suck on straw and the cheeks coming in with the face narrowing. The way the infants are fed will change the development of the physical structure that may result in lifelong problems and may contribute to developing a highly arched palate with a narrow jaw and facial abnormalities such as long face syndrome (Tourne, 1990).
To widen the upper palate and jaw, the infant needs to chew, chew and tear the food with their gums and teeth. Before the industrialization of foods, children had to tear food with their teeth, chew fibrous foods or gnaw at the meat on bones. The chewing forces allows the jaw to widen and develop so that when the permanent teeth are erupting, they would more likely be aligned since there would be enough space–eliminating the need for orthodontics. On the other hand, when young children eat puréed and highly processed soft foods (e.g., cereals soaked in milk, soft breads), the chewing forces are not powerful enough to encourage the widening of the palate and jaw.
Although the solution in adults can be the use of mouth tape to keep the mouth closed at night to retrain the breathing pattern, we should not wait until we have symptoms. The focus needs to be on prevention. The first step is an assessment whether the children’s tongue can do its job effectively or limited by tongue-tie and the arch of the palate. These structures are not totally fixed and can change depending on our oral habits. The field of orthodontics is based upon the premise that the physical structure of the jaw and palate can be changed, and teeth can be realigned by applying constant forces with braces.
Support healthy development of the palate and jaw
Breastfeed babies (if possible) for the first year of life and do NOT use bottle feeding. When weaning, provide chewable foods (fruits, vegetable, roots, berries, meats on bone) that was traditionally part of our pre-industrial diet. These foods support in infants’ healthy tongue and jaw development, which helps to support the normal widening of the palate to provide space for nasal breathing.
Provide fresh organic foods that children must tear and chew. Avoid any processed foods which are soft and do not demand chewing. This will have many other beneficial health effects since processed foods are high in simple carbohydrates and usually contain color additives as well as traces of pesticides and herbicides. The highly processed foods increase the risk of developing depression, type 2 diabetes, inflammatory disease, and colon cancer (Srour et al., 2019).
Sadly, the USA allows much higher residues of pesticide and herbicides that act as neurotoxins than are allowed in by the European Union. For example, the acceptable level of the herbicide glyphosate (Round-Up) is 0.7 parts per million in the USA while in the acceptable level is 0.01 parts per million in European countries (Tano, 2016; EPA, 2023; European Commission, 2023). The USA allows this higher exposure even though about half of the human gut microbiota are vulnerable to glyphosate exposure (Puigbò et al., 2022).
The negative effects of herbicides and pesticides are harmful for growing infants. Even fetal exposure from the mother (gestational exposure) is associated with an increase in behaviors related to attention-deficit/hyperactivity disorders and executive function in the child when they are 7 to 12 years old (Sagiv et al., 2021) and organophosphate exposure is correlated with ADHD prevalence in children (Bouchard et al., 2010).
To implement these basic recommendations are very challenging. It means the mother has to breastfeed her infant during the first year of life. This is often not possible because of socioeconomic inequalities; work demands and medical complications. It also goes against the recent cultural norm that fathers should participate in caring for the baby by giving the baby a bottle of stored breast milk or formula.
From our perspective, women who give birth must have a year paid maternity leave to provide their infants with the best opportunity for health (e.g., breast-feeding, emotional bonding, and reduced financial stress). As a society, we have the option to pay the upfront cost now by providing a year- long maternity leave to mothers or later pay much more costs for treating chronic conditions that may have developed because we did not support the natural developmental process of babies.
Relevance to the field of neurofeedback and biofeedback
Clinicians often see clients, especially children with diagnostic labels such as ADHD who have failed to respond to numerous psychotherapies and pharmacotherapies. In the recent umbrella review and meta-analytic evaluation of recent meta-analyses, Leichsenring et al. (2022) found only small benefits overall for both types of intervention. They suggest that a paradigm shift in research seems to be required to achieve further progress in resolving mental health issues. As the past director of National Institute of Health, Dr. Thomas Insel pointed out that the Diagnostic and Statistical Manual of Mental Disorders (DSM) is not a valid instrument and should be a big wake up call for all of us to think outside the box (Insel, 2009). One factor that starts right at birth is the oral cavity development by dysfunctional tongue movements.
We want to make all of you aware of a serious issue in children that you may come across. For those of us who work with children children, we need to ask their parents about the following: tongue-tie, mouth breathing, bedwetting, high-vaulted palate, thumb sucking, abnormal eating issues, apraxia, dysarthria, and hypotonia. Research suggests that the palates of these children are so arched that the tongue cannot do its job effectively, causing multiple issues which may be related.
Please view the webinar from May 17, 2023. Presented by Karindy Ong, MA, CCC-SLP, CFT, How the Tongue Informs Healthy (or Unhealthy) Neurocognitive Development. The presentation explains the developmental process of the role the tongue plays and how it contributes to nasal breathing. Please pass it on to others who may have interest.
References
Bouchard, M.F., Bellinger, D.C., Wright, R.O., & Weisskopf, M.G. (2010). Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics, 125(6), e1270-7. https://doi.org/10.1542/peds.2009-3058
EPA. (2023). Glyphosate. United States Environmental Protection Agency. Accessed April 1, 2023. https://www.epa.gov/ingredients-used-pesticide-products/glyphosate
European Commission. (2023). EU legislation on MRLs.Food Safety. Assessed April 1, 2023. https://food.ec.europa.eu/plants/pesticides/maximum-residue-levels/eu-legislation-mrls_en#:~:text=A%20general%20default%20MRL%20of,e.g.%20babies%2C%20children%20and%20vegetarians.
Insel, T.R. (2009). Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry, 66(2), 128-133. https://doi.org/10.1001/archgenpsychiatry.2008.540
Kahn, S. & Ehrlich, P.R. (2018). Jaws. Stanford, CA: Stanford University Press. https://www.amazon.com/Jaws-Hidden-Epidemic-Sandra-Kahn/dp/1503604136/ref=tmm_hrd_swatch_0?_encoding=UTF8&qid=1685135054&sr=1-1
Leal, R.B., Gomes, M.C., Granville-Garcia, A.F., Goes, P.S.A., & de Menezes, V.A. (2016). Impact of Breathing Patterns on the Quality of Life of 9- to 10-year-old Schoolchildren. American Journal of Rhinology & Allergy, 30(5):e147-e152. https://doi.org/10.2500/ajra.2016.30.4363
Lee, Y.C., Lu, C.T., Cheng, W.N., & Li, H.Y. (2022).The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare (Basel), 10(9), 1755. https://doi.org/10.3390/healthcare10091755
Leichsenring, F., Steinert, C., Rabung, S. and Ioannidis, J.P.A. (2022), The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry, 21: 133-145. https://doi.org/10.1002/wps.20941
Lundberg, J.O. & Weitzberg, E. (1999). Nasal nitric oxide in man. Thorax. (10):947-52. https://doi.org/10.1136/thx.54.10.947
McKeown, P. (2021). The Breathing Cure: Develop New Habits for a Healthier, Happier, and Longer Life. Boca Raton, Fl “Humanix Books. https://www.amazon.com/BREATHING-CURE-Develop-Healthier-Happier/dp/1630061972/
Nestor, J. (2020). Breath: The New Science of a Lost Art. New York: Riverhead Books. https://www.amazon.com/Breath/dp/0593191358/ref=tmm_pap_swatch_0?_encoding=UTF8&qid=1686191995&sr=8-1
Puigbò, P., Leino, L. I., Rainio, M. J., Saikkonen, K., Saloniemi, I., & Helander, M. (2022). Does Glyphosate Affect the Human Microbiota?. Life, 12(5), 707. https://doi.org/10.3390/life12050707
Sagiv, S.K., Kogut, K., Harley, K., Bradman, A., Morga, N., & Eskenazi, B. (2021). Gestational Exposure to Organophosphate Pesticides and Longitudinally Assessed Behaviors Related to Attention-Deficit/Hyperactivity Disorder and Executive Function, American Journal of Epidemiology, 190(11), 2420–2431. https://doi.org/10.1093/aje/kwab173
Srour, B. et al. (2019). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé).BMJ, 365. https://doi.org/10.1136/bmj.l1451
Tano, B. (2016). The Layman’s Guide to Integrative Immunity. Integrative Medical Press. https://www.amazon.com/Laymans-Guide-Integrative-Immunity-Discover/dp/0983419299/_
Tourne, L.P. (1990). The long face syndrome and impairment of the nasopharyngeal airway. Angle Orthod, 60(3):167-76. https://doi.org/10.1043/0003
Trabalon, M. & Schaal, B. (2012). It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr, 207605. https://doi.org/10.1155/2012/207605
van Bon, M.J., Zielhuis, G.A., Rach, G.H., & van den Broek, P. (1989). Otitis media with effusion and habitual mouth breathing in Dutch preschool children. Int J Pediatr Otorhinolaryngol, (2), 119-25. https://doi.org/10.1016/0165-5876(89)90087-6
Biofeedback, posture and breath: Tools for health
Posted: December 1, 2022 Filed under: ADHD, behavior, biofeedback, Breathing/respiration, CBT, cognitive behavior therapy, computer, digital devices, education, emotions, ergonomics, Evolutionary perspective, Exercise/movement, healing, health, laptops, mindfulness, Neck and shoulder discomfort, Pain/discomfort, posture, relaxation, screen fatigue, self-healing, stress management, Uncategorized, vision, zoom fatigue 3 CommentsTwo recent presentations that that provide concepts and pragmatic skills to improve health and well being.
How changing your breathing and posture can change your life.
In-depth podcast in which Dr. Abby Metcalf, producer of Relationships made easy, interviews Dr. Erik Peper. He discusses how changing your posture and how you breathe may result in major improvement with issues such as anxiety, depression, ADHD, chronic pain, and even insomnia! In the presentation he explain how this works and shares practical tools to make the changes you want in your life.
How to cope with TechStress
A wide ranging discussing between Dr. Russel Jaffe and Dr Erik that explores the power of biofeedback, self-healing strategies and how to cope with tech-stress.
These concepts are also explored in the book, TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics. You may find this book useful as we spend so much time working online. The book describes the impacts personal technology on our physical and emotional well-being. More importantly, “Tech Stress” provides all of the basic tools to be able not only to survive in this new world but also thrive in it.
Additiona resources:
Gonzalez, D. (2022). Ways to improve your posture at home.
Hope for abdominal discomfort
Posted: June 21, 2022 Filed under: behavior, biofeedback, Breathing/respiration, emotions, Evolutionary perspective, healing, health, Pain/discomfort | Tags: functional abdominal pain, heart rate variability, HRV, IBS, irritable bowel syndrome, neurasthenia, Rap, recurrent abdominal pain, respiration 3 CommentsAdapted from: Peper, E. & Harvey, R. (2022). Nausea and GI discomfort: A biofeedback assessment model to create a rational for training. Biofeedback, 50(1), 24–32. https://doi.org/10.5298/1081-5937-50.1.05
Abdominal discomfort and pain such as functional abdominal pain, acid reflux or irritable bowel affects many people. Teaching slower biofeedback-assisted HRV breathing with biofeedback is a useful strategy by which the person may be able to reduce symptoms. This essay provides detailed instruction for a first session assessment for clients who have abdominal discomfort (functional abdominal pain). Descriptions include how the physiological recording can be used to understand a possible etiology of the illness, to create a biological/evolutionary based explanation that is readily understood by the client, and finally to offer self-regulation suggestions to improve health.
Background of abdominal discomfort (irritable bowel syndrome, acid reflux, functional abdominal pain, recurrent abdominal pain)
Irritable bowel syndrome (IBS) affects 7% to 21% of the general population in Western cultures with a global prevalence estimated at around 11% (Fairbrass, Costantino, Gracie, & Ford, 2020). The chronic symptoms (i.e., lasting more than 30 days) usually include abdominal cramping, discomfort or pain, bloating, loose or frequent stools and constipation, which can significantly reduce the quality of life (Chey et al., 2015). A precursor of IBS in children is called recurrent abdominal pain (RAP), which affects 0.3% to 19% of school children (Chitkara et al., 2005). Both IBS and RAP appear to be functional illnesses, as no organic causes have been identified to explain the symptoms. IBS and RAP are contrasted to various types of diseases such as Crohn’s disease, inflammatory bowel disease or ulcerative colitis.
Multiple factors may contribute to IBS, such as genetics, food allergies, previous treatment with antibiotics, infections, psychological status and stress. More recently, dietary factors contributing to changes in the intestinal and colonic microbiome resulting in small intestine bacterial overgrowth have been suggested as another risk factor (Dupont, 2014). Generally, standard medical treatments (reassurance, dietary manipulation and of pharmacological therapy) are often ineffective in reducing IBS symptoms (Chey et al., 2015). On the other hand, complementary and alternative approaches such as biofeedback-assisted relaxation techniques (Davidoff & Whitehead, 1996; Goldenberg et al., 2019; Stern et al. 2014), autogenic training (Luthe & Schultz, 1969) and cognitive therapy are more effective than traditional medical treatment (Vlieger et al., 2008).
Biofeedback-assisted relaxation training typically moderates IBS or RAP symptoms by restoring balance in the nervous system (sympathetic/parasympathetic autonomic balance), such as through heart rate variability (HRV) breathing training. For example, Sowder et al. (2010) as well as Sun et al. (2016) demonstrated that functional abdominal pain can be reduced with HRV feedback training. In most cases, increased vagal tone was achieved by breathing at about six breaths per minute. While Taneja et al. (2004) reported that yogic breathing decreased diarrhea-predominant irritable bowel syndrome symptoms significantly more than conventional treatment in a randomized control study.Sympathetic/parasympathetic balance can be enhanced by increasing HRV, which occurs when a person breathes at their resonant frequency, which is usually 5–7 breaths per minute. For most people, the HRV training means breathing at much slower rate. A benefit of slow abdominal breathing appears to be a self-control strategy that can reduce symptoms of IBS, RAP and similar functional abdominal pain symptoms.
Mastery of effortless diaphragmatic breathing can be affected by injury, surgery or similar insults to the abdominal area (Peper et al., 2015). In addition, dysregulation of diaphragm, which is enervated by the phrenic nerve and the vagus nerve, along with dysregulation of other abdominal muscles appears to be associated with irritable bowel syndrome (Bordoni & Morabito, 2018). It is likely that slower biofeedback-assisted HRV breathing training restores abdominal muscles and diaphragmatic movement, theoretically by tonic and phasic regulation of the phrenic and vagal nerve activity (cf. Marchenko et al., 2015; Streeter et al., 2012). The theory, simply stated, is that HRV breathing training at an individual’s resonant frequency produces increases in regulatory neurotransmitters, particularly gamma amino butyric acid (GABA). Many of our students who complain of abdominal discomfort report reductions of symptoms following HRV breathing training.
Consistently for more than 40 years, we have taught undergraduate students a semester-long integrated stress management program that includes modified progressive relaxation, slow diaphragmatic breathing and changing internal language as outlined in the book, Make Health Happen, by Peper, Gibney & Holt (2002). At the end of each semester, numerous students report that their anxiety, gastrointestinal distress and other symptoms related to self-described IBS or RAP have decreased or disappeared (Peper et al., 2014; Peper, Miceli, & Harvey, 2016; Peper, Mason, Huey, 2017; Peper et al., 2020). Abdominal discomfort is prevalent experience of distress by college students. In our recent survey of 99 undergraduate students, 41% self-reported abdominal discomfort (25% irritable bowel or acid reflux), 86% self-reported anxiety, 70% neck and shoulder tension and 48% headaches. After practicing slower breathing (i.e., typically directing them to breath abdominally at a rate of about six breaths a minute) and focus on slower exhalation and allowing the air to flow in without effort as the abdominal wall expands, as a homework assignment for a week, many reported that their symptoms significantly decreased (Peper, Harvey, Cuellar, & Membrila, in press).
Case example illustrating how to use the physiological recording to guide the client discussion and provide motivation
A 16-year-old high school junior suffered from abdomen discomfort for years. The symptoms mainly consisted of frequent constipation, and when it occurred, great discomfort from nausea. After having been diagnosed and undergoing all the necessary tests by the gastroenterologist, there was no identifiable cause of the chief complaints. Biofeedback was suggested as an alternative to medications for symptom reduction. During the biofeedback assessment and training session, the client discussed what she would like to learn from the session. It was challenging for her to respond to those questions. Not being able to report what the client would like from a training session is also a very common experience when working with students. A useful strategy is to describe experiences of other students that the clients could relate to, and imply that their abdominal discomfort is somewhat commonplace in other students.
Discussed during the session was the link between being very sensitive and reactive to other people’s feeling and being concerned about what others think of her. The client nodded her head in agreement. When describing herself, she discussed being very perfectionistic using a scale from being lackadaisical/undemanding to being perfectionistic (i.e., self-oriented perfectionism, self-worth contingencies, concern over mistakes, doubts about actions, self-criticism, socially prescribed perfectionism, other-oriented perfectionism, hypercriticism; see Smith, Saklofske, Stoeber, & Sherry, 2016).
Furthermore, the client sat slouched in the chair. Possibly her slouched posture implied a state of powerlessness instead of empowerment, a state of being ready to react and protect (Carney, Cuddy, & Yap, 2010; Cuddy, 2012; Peper, Lin, & Harvey, 2017).
Working hypotheses. The client was very sensitive and continuously reacted to external and internal signals with sympathetic arousal, while masking her reactions. These ongoing flight/flight responses would decrease intestinal peristalsis and abdominal blood flow, which would result in nausea, constipation and abdominal distress. Namely, the body reacts to the stimuli as signals of danger and blood flow is shunted away from the abdomen into the large muscles to run and fight. To paraphrase Stanford University professor Robert Sapolsky (2004): Why should the body digest food and repair itself, if it is going to be the predator’s lunch? It is only when we are safe that we can digest and regenerate.
The session began by exploring how pressure on the abdomen could potentially affect experiences of nausea and abdominal distress. After explaining how the diaphragm descends and how abdominal content in the stomach can be displaced (spread out) during inhalation, we systematically changed her posture by placing and adjusting a small pillow behind her middle back so that she could sit tall. The tall posture resulted in an open feeling of empowerment not felt during slouching. She observed that breathing was slightly easier and felt there was more space in her abdomen. As she began to feel more comfortable during the training session, we discussed the impact of posture on the body. We also discussed the relationship between thoughts of perfectionism and abdominal discomfort. The discussion also included an exploration of why some people tend to curl-up and slouch in a protective posture (e.g., head down to protect the neck region and big bones of the arms and legs positioned to protect the core organs) when feeling self-consciousness or perfectionistic about body image.
Biofeedback monitoring for assessment
Psychophysiology was recorded with multichannel physiological system (Procomp Infinity System running Biograph Infinity software version 6.7.1, Thought Technology Ltd). Respiration was monitored with strain-gauge sensors placed around the abdomen and thoracic regions (for a discussion on sensor placement see Peper et al., 2016 and Chu et al., 2019). Blood volume pulse was recorded with the sensor placed on the left thumb. The thumb was used because the participant had small and cold fingers (for a discussion about blood volume pulse, see Peper et al, 2007 and Peper, Shafer, & Lin, 2010). Skin conductance was recorded with the sensor wrapped around the left index and middle fingers with the electrodes on the finger pads (for a discussion about skin conductance and normal values, see Khazan, 2019, and Shafer et al, 2016).
After sensors were attached and the signals explained, the client sat comfortably while looking at the screen. Unexpectedly the clinician clapped his hands and made a loud noise. The client reacted with a momentary startle and smile. The physiological response, showed an increase in skin conductance, decrease in pulse amplitude, decrease in abdominal diameter, and increase in heart rate, is shown in Figure 1.
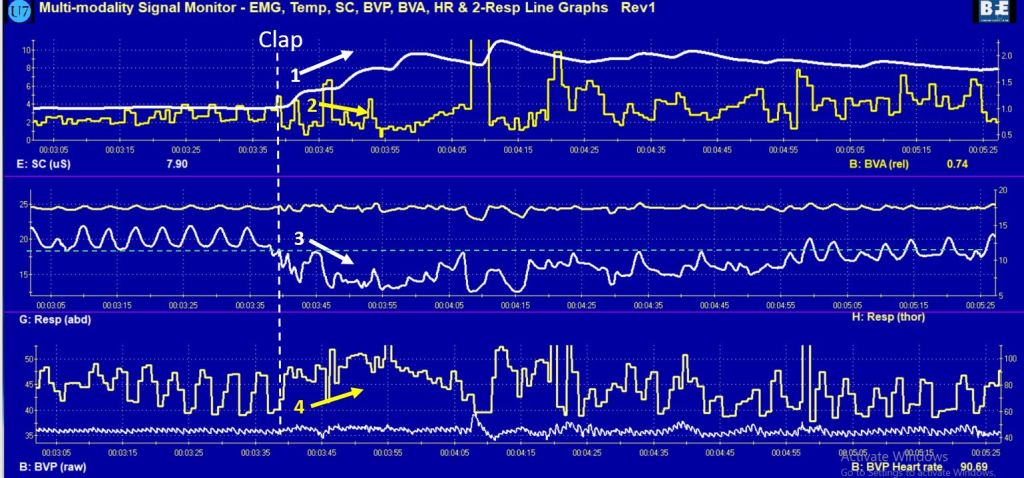
Figure 1. Physiological response to a loud noise (clap) (1) increased skin conductance, (2) decrease in pulse amplitude, (3) decrease in decreased abdominal circumference, and (4) increased heart rate and decreased heart rate variability.
The client was aware that she reacted to the clap; however, she was totally unaware how much her body responded. The computer screen display of her physiological reaction made the invisible visible. It provided the opportunity to discuss how various body reactions related to heart rate, breathing, and skin conductance could contribute to experiences of abdominal discomfort.
She was unaware that skin conductance did not return to baseline levels for more than 20 minutes. An elevated skin conductance level may mean that the body’s reaction to the hand-clap noise triggered a defense reaction and maintained the increased sympathetic activity for more than 20 minutes. Having a sustained flight/fight reaction to external stimuli such as a hand-clap would most likely affect digestive and peristalsis processes, contributing to symptoms found in IBS and RAP. The observations made during biofeedback monitoring led to a discussion of how sympathetic activation affects the gastrointestinal track.
Blood volume pulse amplitude decreased, which indicated a decrease in blood flow through her hands, which would decrease hand temperature and again indicated a systemic sympathetic activation.
Abdominal circumference decreased, which indicated that she tightened her abdominal muscles as a protective response to the hand-clap. She was unaware of the abdominal muscles tightening; however, she stated that she was aware that her breathing had changed. The abdominal muscle, which pulled the abdomen in, took almost two minutes to relax. The sustained muscle constriction around the abdomen increased pressure around the core organs, which may contribute to ongoing abdominal discomfort. A fight-flight reaction includes body bracing (e.g. tightened muscles, head down to protect the neck, big bones of arms and legs curled to protect core organs), and she confirmed that she experienced neck and shoulder tensions.
The discussion of abdominal muscle tension led to another discussion of how holding your stomach in may relate to self-image. For example, tight clothing can contribute to constricted movement around the abdomen. Wearing corsets contributed to psychophysiological symptoms, mainly for women in the late 19th and early 20th centuries, during a time when women who wore very tight corsets were diagnosed with neurasthenia. Simply stated, neurasthenia was characterized as a condition of mental and/or physical fatigue with at least two of the following symptoms: dyspepsia, dizziness, muscular aches or pains, tension headaches, inability to relax, irritability and sleep disturbance.
“Dyspepsia” was the commonly reported symptom of neurasthenia, which included upset stomach, a gnawing or burning stomach pain, heartburn, bloating, and or burping, nausea, and vomiting. The constricted waist region that resulted from wearing a corset in the name of fashion compromises the functions of both digestion and breathing. When the person inhales, the abdomen cannot expand as the diaphragm is flattening and pushing downward. Thus, the person is forced to breathe more shallowly by lifting their ribs; this increases neck and shoulder tension as well as the risk of anxiety, heart palpitation, and fatigue (Cohen & White, 1947; Courtney, 2009).
It also can contribute to abdominal discomfort since the abdomen is being squeezed by the corset and forcing the abdominal organs upward. Even architects of the Victorian era recognized a need for a place to position a chair or chaise lounge, such as at the top of some stairs, because people wearing corsets could faint, pass out or otherwise experience breathlessness through the effort of climbing the stairs with restrictive clothing around their abdomen (Melissa, 2015). Many of these symptoms could be easily reduced by wearing looser clothing and learning slower diaphragmatic breathing. In modern times, a related phenomenon results when people wear items of clothing that are too tight around their waist or abdomen (e.g., tight jeans) in service to fashion trends often labeled as designer jean syndrome (MacHose & Peper, 1991; Stonehewer, 2009). Similarly, when people wear garments that are too tight around their chest or thoracic region (e.g., tight vests) in service to external protection (e.g., athletes, industrial workers, police or soldiers wearing heavy, restrictive gear), then restrictive ventilatory disorders can occur (Harty et al., 1999). Simply stated, when the muscles related to breathing are restricted from moving, respiration is affected.
The client’s heart rate increased and stayed high for more than 30 seconds. The first decrease in heart rate at about 20 seconds after the hand-clap was a long sigh of relief as breathing (i.e., oxygen/carbon dioxide exchange) started again. It took almost 90 seconds before breathing and heart rate returned to normal as reflected by measures of HRV. The computer screen showing increased heart rate was reviewed with the client to explain how her body reacted with a fight-flight response to the hand-clap, as well as how regulating breathing through biofeedback training could lower the heart rate and reduce the sympathetic activation and enhance the parasympathetic activation.
Body responds to cognitive stressful thoughts
After discussion about the psychophysiological response to the hand-clap (a physical external stressor) and how other external stressors (e.g., startling noise) or internal stressors (e.g., perfectionistic ruminations) could trigger a similar response of abdominal muscle tightening, the assessment was repeated by having her relax and then think about a mental stressor, as shown in Figure 2.

Figure 2. Physiological responses to thinking about a past stressor (1) increased skin conductance, (2) decreased pulse amplitude, (3) decreased abdominal circumference, and (4) increased heart rate and decreased HRV.
The physiological response pattern to thinking about a past stressor was similar to the bodily reaction to a loud noise. The skin conductance increased and blood volume pulse amplitude decreased immediately after hearing (e.g., anticipating) the task of evoking/thinking of a past stressor. Most likely, the initial response was triggered by performance anxiety, then 6 seconds later the heart rate increased and breathing changed as she began experiencing the somatic reaction evoked by the recall of a negative stressor. The recordings also showed that her pulse amplitude decreased. The decrease in pulse amplitude suggested that her hands would probably become colder, which was confirmed by her self-report that she often experienced cold hands and feet. She reported being aware of the feeling an emotional reaction, but mainly noticing the change of breathing in her chest, and she was unaware of the abdominal changes. The client was surprised by how her body reacted to emotional thoughts. The recording viewed on the computer screen demonstrated objectively that her thoughts (initial performance anxiety) had a physical effect on her body. Specifically, experiencing the emotions that were evoked by recalling the stressful memory had a direct effect on the body in the same way that a physical external threat leads to a fight-flight response.
Building a psychophysiological model
Using these recorded computer images reflecting physical reactions to the hand clap and emotional thoughts, the discussion focused on how abdominal discomfort could be the result of activating a normal biological survival response. Survival responses would occur hundreds of times throughout a day, especially when worrying. Each thought would evoke the response, and the awareness of body reaction would evoke another reaction. Similar to how awareness of blushing amplifies blushing.
The client shared that she was very sensitive and reactive especially when other people were upset. She reported feeling “cursed” by their sensitivity and reactivity. The linguistic metaphor that could be used to describe her reactions is “she could not stomach what was going on.”
The discussion about physiological reactions provided the client with a model how her disorder (IBS and RAP) could have developed and been maintained over the years. The model matched her subjective experience: when stressed, the discomfort often increased. The discussion shifted to reframing her internal labels. Instead of describing her sensitivity as a curse, the sensitivity was reframed and labeled a gift; namely, she could sense many people’s emotional reactions, to which they would react in a variety of ways. She just needed to learn how to manage this sensitivity. Once she learned to manage it, she would have many advantages in interpersonal relations at home and at work. She would be able to sense what other people are experiencing. By reframing her symptoms as a result of a survival physiological response pattern, it reduces self- blame and offers solutions about how to master and change reactions and thereby have more control in the world.
Training to demonstrate control is possible.
The discussion was followed by teaching her diaphragmatic breathing in sitting and lying down positions. As she had no history of abdominal injuries, similar to many of our students, she rapidly demonstrated slower diaphragmatic breathing as shown in Figures 3 and 4.

Figure 3. The client practiced a few slower diaphragmatic breaths in the sitting and reclining position, which increased heart rate variability, decreased skin conductance and increased blood volume pulse amplitude.

Figure 4. Practicing slower diaphragmatic breathing at about six breaths per minute in a reclining position increased HRV.
With tactile coaching, she demonstrated that she could breathe at about six breaths per minute with the heart rate increasing during inhalation and decreasing during exhalation. She reported feeling more relaxed and that the sensations of nausea had disappeared. Additionally, her hands felt warmer. This recording provided proof that there was hope and that she could do something about her body’s psychophysiological responses.
The discussion focused on how breathing affecting heart rate variability. Namely, if she allowed exhalation to occur without effort, her heart rate decreased (the vagal response of slowing the heart) and thereby increased the parasympathetic activation that would support digestion and gastrointestinal functioning. Often when people practice effortless diaphragmatic breathing, abdominal noises (borborygmus)– the gurgling, rumbling, or squeaking noise from the abdomen–occur and indicate that intestinal activity is being activated, and that food, liquids and digestive juice are moving through the intestines. It is usually a positive indicator that the person is relaxing and sympathetic activity has been reduced.
During the last part of session, we reviewed how posture affects physiology, emotions and cognitions, as well as how posture and breathing would be the first step in beginning to reduce symptoms and enhance health. To provide additional information using video and bibliotherapy/education, we suggested that she watches the embedded videos in the blogs listed at the end of the article.
Recommendations for future sessions and home practice
The recommended strategies for future sessions would focus on teaching the client to master slow diaphragmatic breathing and practicing that for 10–20 minutes per day. The teaching techniques would incorporate imagery to imagine air flowing down their arms and legs as she exhaled. . More importantly, the focus would shift to generalize the skill during the day; namely, whenever she would become aware of feeling stressed or observed herself holding her breath or breathing in her chest, she would use that as the cue to shift to slower abdominal breathing. Had the client continued training, future sessions would focus on mastering slower diaphragmatic breathing. The training would include relaxing the lower abdominal muscles during inhalation, increasing control of HRV, practicing imagining stress and use image to trigger slower breathing, and cognitive reframing practices to interrupt worrying and promote self-acceptance. The final goal is to generalize these skills into daily life as illustrated in the successful cases described in the following blogs
Blogs on posture:
References
Bordoni, B. & Morabito, B. (2018). Symptomatology correlations between the diaphragm and irritable bowel syndrome. Cureus, 10(7), e3036. https://doi.org/10.7759/cureus.3036
Carney, D. R., Cuddy, A. J., & Yap, A. J. (2010). Power posing: brief nonverbal displays affect neuroendocrine levels and risk tolerance. Psychological Science, 10, 1363-1368. https://dx.doi.org/10.1177/0956797610383437
Chey, W. D., Kurlander, J., & Eswaran, S. (2015). Irritable bowel syndrome: a clinical review. Jama, 313(9), 949–958. https://doi.org/10.1001/jama.2015.0954
Chitkara, D. K., Rawat, D. J., & Talley, N. J. (2005). The epidemiology of childhood recurrent abdominal pain in Western countries: a systematic review. American journal of Gastroenterology, 100(8), 1868–1875. https://doi.org/10.1111/j.1572-0241.2005.41893.x
Chu, M., Nguyen, T., Pandey, V., Zhou, Y., Pham, H. N., Bar-Yoseph, R., Radom-Aizik, S., Jain, R., Cooper, D. M., & Khine, M. (2019). Respiration rate and volume measurements using wearable strain sensors. NPJ digital medicine, 2(1), 1–9. https://doi.org/10.1038/s41746-019-0083-3
Cohen, M. E. & White, P. D. (1947). Studies of breathing, pulmonary ventilation and subjective awareness of shortness of breath (dyspnea) in neurocirculatory asthenia, effort syndrome, anxiety neurosis. Journal of Clinical Investigation, 26(3), 520–529. https://doi.org/10.1172/JCI101836
Courtney, R. (2009). The functions of breathing and its dysfunctions and their relationship to breathing therapy. International Journal of Osteopathic Medicine, 12, 78–85. https://doi.org/10.1016/j.ijosm.2009.04.002
Cuddy, A. (2012). Your body language shapes who you are. Technology, Entertainment, and Design (TED) Talk, available at: http://www.ted.com/talks/amy_cuddy_your_body_language_shapes_who_you_are
Davidoff, A. L., & Whitehead, W. E. (1996). Biofeedback, relaxation training, and cognitive behavior modification: Treatments for functional GI disorders, In Olden, K, W. (ed). Handbook of Functional Gastrointestinal Disorders. CRC Press, 361–384.
Dupont, H. L. (2014). Review article: evidence for the role of gut microbiota in irritable bowel syndrome and its potential influence on therapeutic targets. Alimentary Pharmacology & Therapeutics, 39(10), 1033–1042. https://doi.org/10.1111/apt.12728
Fairbrass, K. M., Costantino, S. J., Gracie, D. J., & Ford, A. C. (2020). Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology, 5(12), 1053–162. https://doi.org/10.1016/s2468-1253(20)30300-9
Goldenberg, J. Z., Brignall, M., Hamilton, M., Beardsley, J., Batson, R. D., Hawrelak, J., Lichtenstein, B., & Johnston, B. C. (2019). Biofeedback for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews, (11). https://doi.org/10.1002/14651858.CD012530.pub2
Harty, H. R., Corfield, D. R., Schwartzstein, R. M., & Adams, L. (1999). External thoracic restriction, respiratory sensation, and ventilation during exercise in men. Journal of Applied Physiology, 86(4), 1142–1150. https://doi.org/10.1152/jappl.1999.86.4.1142
Khazan, I. (2019). A guide to normal values for biofeedback. Biofeedback, 47(1), 2–5. https://doi.org/10.5298/1081-5937-47.1.03
Luthe, W. & Schultz, J. H. (1969). Autogenic Therapy Volume II: Medical Applications. Grune & Stratton.
MacHose, M., & Peper, E. (1991). The effect of clothing on inhalation volume. Biofeedback and Self-Regulation, 16(3), 261–265. https://doi.org/10.1007/BF01000020
Marchenko, V., Ghali, M. G., & Rogers, R. F. (2015). The role of spinal GABAergic circuits in the control of phrenic nerve motor output. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 308(11), R916–R926. https://doi.org/10.1152/ajpregu.00244.2014
Melissa. (2015). Why women fainted so much in the 19th century. May 20, 2015. Downloaded October 2, 2021. http://www.todayifoundout.com/index.php/2015/05/women-fainted-much-19th-century/
Peper, E., Gibney, K. H., & Holt, C. F. (2002). Make Health Happen—Training Yourself to Create Wellness. Kendall/Hunt Publishing Company.
Peper, E., Gilbert, C. D., Harvey, R. & Lin, I-M. (2015). Did you ask about abdominal surgery or injury? A learned disuse risk factor for breathing dysfunction. Biofeedback. 34(4), 173–179. https://doi.org/10.5298/1081-5937-43.4.06
Peper, E., Groshans, G. H., Johnston, J., Harvey, R., & Shaffer, F. (2016). Calibrating respiratory strain gauges: What the numbers mean for monitoring respiration. Biofeedback, 44(2), 101–105. https://doi.org/10.5298/1081-5937-44.2.06
Peper, E., Harvey, R., Cuellar, Y., & Membrila, C.(in press). Reduce anxiety. NeuroRegulation.
Peper, E., Harvey, R., Lin, I. M., Tylova, H., & Moss, D. (2007). Is there more to blood volume pulse than heart rate variability, respiratory sinus arrhythmia, and cardiorespiratory synchrony? Biofeedback, 35(2), 54–61. https://www.researchgate.net/publication/259560204_Is_There_More_to_Blood_Volume_Pulse_Than_Heart_Rate_Variability_Respiratory_Sinus_Arrhythmia_and_Cardiorespiratory_Synchrony
Peper, E., Lin, I-M, & Harvey, R. (2017). Posture and mood: Implications and applications to therapy. Biofeedback, 35(2), 42–48. https://doi.org/10.5298/1081-5937-45.2.03
Peper, E., Lin, I-M, Harvey, R., Gilbert, M., Gubbala, P., Ratkovich, A., & Fletcher, F. (2014). Transforming chained behaviors: Case studies of overcoming smoking, eczema and hair pulling (trichotillomania). Biofeedback, 42(4), 154–160. https://doi.org/10.5298/1081-5937-42.4.06
Peper, E., Mason, L., Harvey, R., Wolski, L, & Torres, J. (2020). Can acid reflux be reduced by breathing? Townsend Letters-The Examiner of Alternative Medicine, 445/446, 44–47. https://www.townsendletter.com/article/445-6-acid-reflux-reduced-by-breathing/
Peper, E., Mason, L., Huey, C. (2017). Healing irritable bowel syndrome with diaphragmatic breathing. Biofeedback, 45(4), 83–87. https://doi.org/10.5298/1081-5937-45.4.04
Peper, E., Miceli, B., & Harvey, R. (2016). Educational model for self-healing: Eliminating a chronic migraine with electromyography, autogenic training, posture, and mindfulness. Biofeedback, 44(3), 130–137. https://www.aapb.org/files/publications/biofeedback/2016/biof-44-03-130-137.pdf
Peper, E., Shaffer, F., & Lin, I. M. (2010). Garbage in; Garbage out—Identify blood volume pulse (BVP) artifacts before analyzing and interpreting BVP, blood volume pulse amplitude, and heart rate/respiratory sinus arrhythmia data. Biofeedback, 38(1), 19–23. https://doi.org/10.5298/1081-5937-38.1.19
Sapolsky, R. (2004). Why Zebras Don’t Get Ulcers. Owl Books ISBN: 978-0805073690
Shaffer, F., Combatalade, D., Peper, E., & Meehan, Z. M. (2016). A guide to cleaner electrodermal activity measurements. Biofeedback, 44( 2), 90–100. https://doi.org/10.5298/1081-5937-44.2.01
Smith, M. M., Saklofske, D. H., Stoeber, J., & Sherry, S. B. (2016). The big three perfectionism scale: A new measure of perfectionism. Journal of Psychoeducational Assessment, 34(7), 670–687. https://doi.org/10.1177/0734282916651539
Sowder, E., Gevirtz, R., Shapiro, W., & Ebert, C. (2010). Restoration of vagal tone: a possible mechanism for functional abdominal pain. Applied Psychophysiology and Biofeedback, 35(3), 199–206. https://doi.org/10.1007/s10484-010-9128-8
Stern, M. J., Guiles, R. A., & Gevirtz, R. (2014). HRV biofeedback for pediatric irritable bowel syndrome and functional abdominal pain: A clinical replication series. Applied Psychophysiology and Biofeedback, 39(3), 287–291. https://doi.org/10.1007/s10484-014-9261-x
Stonehewer, L. (2009). Dysfunctional breathing for women’s health physiotherapists. Journal of the Association of Chartered Physiotherapists in Women’s Health, 104, 38–40. https://pogp.csp.org.uk/system/files/stonehewer_hr.pdf
Streeter, C. C., Gerbarg, P. L., Saper, R. B., Ciraulo, D. A., & Brown, R. P. (2012). Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Medical hypotheses, 78(5), 571–579. https://doi.org/10.1016/j.mehy.2012.01.021
Sun, X., Shang, W., Wang, Z., Liu, X., Fang, X., & Ke, M. (2016). Short-term and long-term effect of diaphragm biofeedback training in gastroesophageal reflux disease: An open-label, pilot, randomized trial. Diseases of the Esophagus, 29(7), 829–836. https://doi.org/10.1111/dote.12390
Taneja. I., Deepak, K.K., Poojary, G., Acharya, I.N., Pandey, R.M., & Sharma, M.P. (2004). Yogic versus conventional treatment in diarrhea-predominant irritable bowel syndrome: a randomized control study. Appl Psychophysiol Biofeedback, 29(1), 19-33. https://doi.org/10.1023/b:apbi.0000017861.60439.95
Vlieger, A. M., Blink, M., Tromp, E., & Benninga, M. A. (2008). Use of complementary and alternative medicine by pediatric patients with functional and organic gastrointestinal diseases: results from a multicenter survey. Pediatrics, 122(2), e446–e451. https://doi.org/10.1542/peds.2008-0266
Addicted to your phone? How to separate from your phone for a healthy lifestyle[1]
Posted: September 21, 2021 Filed under: behavior, computer, digital devices, education, ergonomics, Evolutionary perspective, Exercise/movement, health, Neck and shoulder discomfort, posture, vision, zoom fatigue 6 CommentsErik Peper, PhD[2] and Monica Almendras

Our evolutionary traps with technology
Maintaining and optimizing health at the computer means re-envisioning our relationship with technology—and reclaiming health, happiness, and sanity in a plugged-in world. We have the ability to control everything from our mobile phones without needing to get up from our seat. Work, social life and online learning all involve the mobile phone or some type of smart devices.
A convenient little device that is supposed to simplify our lives has actually trapped us into a vicious cycle of relying on it for every single thing we must do. We spend most of our day being exposed to digital displays on our smartphones, computers, gaming consoles, and other digital devices, immersing ourselves in the content we are viewing. From work related emails or tasks, to spending our free time looking at the screen for texting, playing games, and updating social media sites on a play-by-play of what we are eating, wearing, and doing. We click on one hyperlink after the other and create a vicious cycle trapped for hours until we realize we need to move. We are unaware how much time has frittered away without actually doing anything productive and then, we realize we have wasted another day. Below are some recent estimates of ‘daily active user’ minutes per day that uses a screen.
- Facebook about an hour per day
- Instagram just under an hour per day
- Texting about 45 minutes per day
- Internet browsing, about 45 minutes per day
- Snapchat, about 30 minutes per day
- Twitter, about 25 minutes per day
Adolescents and college students interact with media for over 40 hours per week, or around 6 hours per day. That is a lot of hours spent on staring at the screen, which it is almost impossible not to be distracted by the digital screen. In time, we rehearse a variety of physical body postures as well as a variety of cognitive and behavioral states that impact our physical, mental, emotional, and social health. The powerful audiovisual formats override our desires to do something different, that some of us become enslaved to streaming videos, playing virtual games, or texting. We then tell ourselves that the task that needs to be done, will be finished later. That later becomes never by the end of the day, since the ongoing visual and auditory notifications from our apps interrupt and/or capture our attention. This difficulty to turn away from visual or auditory stimuli roots in our survival instincts.
Each time visual or auditory stimuli occur, we automatically check it out and see if it is a friend or foe, safety or danger. It is such an automatic response that we are unaware are reacting. The good news is that we all have experienced this compelling effect. Even when we are waiting for a response and the notifications has not arrived, we may anticipate or project that there may be new information on our social media accounts, and sometimes we become disappointed when the interval between notification is long. As one student said, “Don’t worry, they’ll respond. It’s only been 30 seconds”. Anticipating responses from the media can interrupt what we are otherwise doing. Rather than finishing our work or task, we continuously check for updates on social media, even though we probably know that there are no new important messages to which we would have to respond right away.
Unfortunately, some forms of social media interactions also lead to a form of social isolation, loneliness–sometimes called phoneliness (Christodoulou, G., Majmundar, A., Chou, C-P, & Pentz, M.A., 2020; Kardaras, 2017). Digital content requires the individual to respond to the digital stimuli, without being aware of the many verbal and nonverbal communication cues (facial expressions, gestures, tone of voice, eye contact, body language, posture, touch, etc.) that are part of social communication (Remland, 2016). It is no wonder that more and more adolescents experience anxiety, depression, loneliness, and attention deficit disorders with a constant ‘digital diet’ that some have suggested that include not only media, but junk food as well.
In my class survey of 99 college students, 85% reported experiencing anxiety, 48% neck and should tension, and 41% abdominal discomfort.
We are not saying to avoid the beneficial parts of the digital age. Instead, it should be used in moderation and to be aware of how some material and digital platforms prey upon our evolutionary survival mechanisms. Unfortunately, most people -especially children- have not evolved skills to counter the negative impacts of some types of media exposure. Parental control and societal policies may be needed to mitigate the damage and enhance the benefits of the digital age.
Zoom Fatigue- How to reduce it and configure your brain for better learning
Zoom became the preferred platform for academic teaching and learning for synchronous education during the pandemic. Thus, students and faculty have been sitting and looking at the screen for hours end. While looking at the screen, the viewers were often distracted by events in their environment, notifications from their mobile phones, social media triggers, and emails; which promoted multitasking (Solis, 2019). These digital distractions cause people to respond to twice as many devices with half of our attention- a process labeled semi-tasking’ -meaning getting twice as much done and half as well.
We now check our phones an average of 96 times a day – that is once every 10 minutes and an increase of 20% as compared to two years ago (Asurion Research, 2019). Those who do media multitasking such as texting while doing a task perform significantly worse on memory tasks than those who are not multitasking (Madore et al., 2020). Multitasking is negatively correlated with school performance (Giunchiglia et al, 2018). The best way to reduce multitasking is to turn off all notifications (e.g., email, texts, and social media) and let people know that you will look at the notifications and then respond in a predetermined time, so that you will not be interrupted while working or studying.
When students from San Francisco State University in the United States chose to implement a behavior change to monitor mobile phone and media use and reduce the addictive behavior during a five-week self-healing project, many reported a significant improvement of health and performance. For example one student reported that when she reduced her mobile phone use, her stress level equally decreased as shown in Fig 1 (Peper et al, 2021).

Figure 1. Example of student changing mobile phone use and corresponding decrease in subjective stress level. Reproduced by permission from Peper et al. (2021).
During this class project, many students observed that the continuous responding to notifications and social media affected their health and productivity. As one student reported,
The discovery of the time I wasted giving into distractions was increasing my anxiety, increasing my depression and making me feel completely inadequate. In the five-week period, I cut my cell phone usage by over half, from 32.5 hours to exactly 15 hours and used some of the time to do an early morning run in the park. Rediscovering this time makes me feel like my possibilities are endless. I can go to work full time, take online night courses reaching towards my goal of a higher degree, plus complete all my homework, take care of the house and chores, cook all my meals, and add reading a book for fun! –22-year-old College Student
Numerous students reported that it was much easier to be distracted and multitask, check social media accounts or respond to emails and texts than during face-to-face classroom sessions as illustrated by two student comments from San Francisco State University.
“Now that we are forced to stay at home, it’s hard to find time by myself, for myself, time to study, and or time to get away. It’s easy to get distracted and go a bit stir-crazy.”
“I find that online learning is more difficult for me because it’s harder for me to stay concentrated all day just looking at the screen.”
Students often reported that they had more difficulty remembering the material presented during synchronous presentations. Most likely, the passivity while watching Zoom presentations affected the encoding and consolidation of new material into retrievable long-term memory. The presented material was rapidly forgotten when the next screen image or advertisement appeared and competed with the course instructor for the student’s attention. We hypothesize that the many hours of watching TV and streaming videos have conditioned people to sit and take in information passively, while discouraging them to respond or initiate action (Mander, 1978; Mărchidan, 2019).
To reduce the deleterious impact of media use, China has placed time limits on cellphone use, gaming, and social media use for children. On February 2021 Chinese children were banned from taking their mobile phones into school, on August 2021 Children under 18 were banned from playing video games during the week and their play was restricted to just one hour on Fridays, weekends and holidays, and beginning on September 20, 2021 children under 14 who have been authenticated using their real name can access Douyin, the Chinese version of Tik Tok, for maximum of 40 minutes a day between the hours of 6:00 and 22:00.
Ways to avoid Zoom
Say goodnight to your phone
It is common for people to use their mobile phone before going to bed, and then end up having difficult falling asleep. The screen emits blue light that sends a signal to your brain that says it is daytime instead of night. This causes your body to suppress the production of the melatonin hormone, which tells your body that it is time to sleep. Reading or watching content also contributes, since it stimulates your mind and emotions and thereby promote wakefulness (Bravo, 2020). Implement sleep hygiene and stop using your phone or watching screens 30-minutes before going to bed for a better night’s sleep.
Maintaining a healthy vision
We increase near visual stress and the risk of developing myopia when we predominantly look at nearby surfaces. We do not realize that eyes muscles can only relax when looking at the far distance. For young children, the constant near vision remodels the shape of eye and the child will likely develop near sightedness. The solutions are remarkably simple. Respect your evolutionary background and allow your eyes to spontaneously alternate between looking at near and far objects while being upright (Schneider, 2016; Peper, 2021; Peper, Harvey & Faass, 2020).
Interrupt sitting disease
We sit for the majority of the day while looking at screens that is a significant risk factor for diabetes, cardiovascular disease, depression and anxiety (Matthews et al., 2012; Smith et al., 2020). Interrupt sitting by getting up every 30 minutes and do a few stretches. You will tend to feel less sleepy, less discomfort and more productive. As one of our participants reported that when he got up, moved and exercised every 30 minutes at the end of the day he felt less tired. As he stated, “There is life after five”, which meant he had energy to do other activities after working at the computer the whole day. While working time flies and it is challenging to get up every 30 minutes. Thus, install a free app on your computer that reminds you to get up and move such as StretchBreak (www.stretchbreak.com).
Use slouching as a cue to change
Posture affects thoughts and emotions as well as, vice versa. When stressed or worried (e.g., school performance, job security, family conflict, undefined symptoms, or financial insecurity), our bodies tend to respond by slightly collapsing and shifting into a protective position. When we collapse/slouch, we are more at risk to:
- Feel helpless (Riskind & Gotay, 1982).
- Feel powerless (Westfeld & Beresford, 1982; Cuddy, 2012).
- Recall and being more captured by negative memories (Peper, Lin, Harvey, & Perez, 2017; Tsai, Peper, & Lin, 2016),
- Experience cognitive difficulty (Peper, Harvey, Mason, & Lin, 2018).
When stressed, anxious or depressed, it is challenging to change. The negative feelings, thoughts and worries continue to undermine the practice of reframing the experience more positively. Our recent study found that a simple technique, that integrates posture with breathing and reframing, rapidly reduces anxiety, stress, and negative self-talk (Peper, Harvey, Hamiel, 2019). When you are captured by helpless defeated thoughts and slouch, use the thought or posture as the trigger to take change. The moment you are aware of the thoughts or slouched posture, sit up straight, look up, take a slow large diaphragmatic breath and only then think about reframing the problem positively (Peper, Harvey, Hamiel, 2019).
When we are upright and look up, we are more likely to:
- Have more energy (Peper & Lin, 2012).
- Feel stronger (Peper, Booiman, Lin, & Harvey, 2016).
- Find it easier to do cognitive activity (Peper, Harvey, Mason, & Lin, 2018).
- Feel more confident and empowered (Cuddy, 2012).
- Recall more positive autobiographical memories (Michalak, Mischnat,& Teismann, 2014).
The challenge is that we are usually unaware we have begun to slouch. A very useful solution is to use a posture feedback device to remind us, such as the UpRight Go (https://www.uprightpose.com/). This simple device and app signals you when you slouch. The device attaches to your neck and connects with blue tooth to your cellphone. After calibrating, it provides vibrational feedback on your neck each time you slouch. When participants use the vibration feedback to become aware of what is going on and interrupt their slouch by stretching and sitting up, they report a significant decrease in symptoms and an increase in productivity. As one student reported: “Having immediate feedback on my posture helped me to be more aware of my body and helped me to link my posture to my emotions. Before using the tracker, doing this was very difficult for me. It not only helped my posture but my awareness of my mental state as well.”
[1] Adapted from the bookby Erik Peper, Richard Harvey and Nancy Faass,TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics, North Atlantic Press. https://www.amazon.com/Beyond-Ergonomics-Prevent-Fatigue-Burnout/dp/158394768X/

[2] Correspondence should be addressed to:
Erik Peper, Ph.D., Institute for Holistic Healing Studies, San Francisco State University, 1600 Holloway Avenue, San Francisco, CA 94132 COVID-19 mailing address: 2236 Derby Street, Berkeley, CA 94705 Email: epeper@sfsu.edu web: www.biofeedbackhealth.org blog: www.peperperspective.com
Rest Rusts: Increase dynamic movement to improve health
Posted: September 16, 2021 Filed under: behavior, computer, ergonomics, Evolutionary perspective, Exercise/movement, health, laptops, Neck and shoulder discomfort, Pain/discomfort, posture, screen fatigue, zoom fatigue | Tags: dynamic movement, static postures 2 CommentsIn hunting and gathering cultures, alternating movement patterns was part of living and essential for health. This shift from dynamic movement to static or awkward positions is illustrated in Figure 1.

Figure 1. The shift from dynamic movement to immobility and near vision as illustrated by the Hadzabe men in Tanzania returning from a hunt to our modern immobilized work and pleasure positions (Reproduced by permission from Peper, Harvey & Faass, 2020).
Dynamic movement promotes blood and lymph circulation and reduces static pressures. At present times our work and leisure activities increase immobility and static positions as we predominantly have shifted to a sitting immobilized position. This significantly increases musculoskeletal discomfort, cardiovascular disease, diabetes etc. The importance of movement as a factor to enhance health is illustrated in the recent findings of 2110 middle aged participants who were followed up for ten years. Those who took approximately 7000 steps per day or more experienced significantly lower mortality rates compared with participants taking fewer than 7000 steps per day (Paluch et al., 2021). Just having the head forward while looking at the cellphone significantly increases the forces on the muscles holding the head up as illustrated in Figure 2.

Figure 2. The head-forward position puts as much as sixty pounds of pressure on the neck muscles and spine (reproduced by permission from Dr. Kenneth Hansaraj, 2014).
For background and recommendations on what how to reduce static positions, look at our book, TechStress-How technology is hijacking our lives, strategies for coping and pragmatic ergonomics. and the superb article, Static postures are harmful – dynamic postures at work are key to musculoskeletal health, published by the European Agency for Safety and Health at Work (EU-OSHA, Sept 16, 2021) and reproduced below.
Static postures are harmful – dynamic postures at work are key to musculoskeletal health
Our bodies are built for movement – it’s a central part of maintaining a healthy musculoskeletal system and the less we move, the more chance we have of developing health issues including musculoskeletal disorders (MSDs), type 2 diabetes, cardiovascular disease, cancer and more. However, the negative effects of sedentary work can be mitigated by paying attention to the postures we adopt when we work.
Whether workers are standing or seated while working, maintaining a good ergonomic posture is essential when it comes to preventing MSDs. Poor or awkward postures put unnecessary strain on the musculoskeletal system and, over time, can cause the deterioration of muscle fibres and joints.
Poor or awkward postures include those which involve parts of the body not being in their natural position. More muscular effort is needed to maintain unnatural postures, which increases the energy used by the body and can cause fatigue, discomfort and pain. Unnatural postures also put strain on tendons, ligaments and nerves, which increases the risk of injury. For example, the risk of neck pain increases when the neck is rotated more than 45 degrees for more than 25% of the working day.
These postures, including slouching, rotation of the forearms, or prolonged periods of sitting or standing in the same spot, can cause pain in the lower back and upper limbs. The risk increases when combined with repetitive work, static muscle load, or the need to apply force or reach. And even natural or good postures maintained for any length of time become uncomfortable and eventually painful. Everyone has experienced stiffness after being in the same position for any length of time.
What do we mean by ‘good posture’?
For workers, especially those in sedentary jobs such as office work, factory work or driving, it is important to recognise and adopt good postures. A good posture should be comfortable and allow the joints to be naturally aligned. The segments of our body can be divided into three cross-sectional anatomical planes: the sagittal plane, which concerns bending forwards and backwards; the frontal plane, which concerns bending sideways; and finally the transverse plane, which refers to rotation or twisting of the body parts. A good posture is one that ensures that all three of these planes are set at neutral positions as much as possible, in that the worker is not leaning backwards, forwards or to any particular side, and their limbs and torso are not rotated or twisted. Adopting neutral postures will help to lessen the strain on the worker’s muscles, tendons and skeletal system, and reduces the risk of them causing or aggravating an MSD.
In practice, workers can consider the following checklist to ensure that they’re standing or sitting in a neutral position:
- Keep the neck vertical and the back in an upright position.
- Ensure the elbows are below the chest and avoid having to reach excessively.
- Keep the shoulders relaxed and use back and arm rests where possible and ensure that they are adjusted to the size and shape of the worker.
- Avoid rotating the forearms or excessively moving the wrists.
- Ensure that any work tools can be held comfortably, and that clothing doesn’t restrain or prevent movement.
- Allow room to comfortably move the legs and feet and avoid frequent kneeling or squatting.
- Ensure that long periods of standing or sitting in the same posture can be broken up.
Employers can assist workers in adopting good postures by communicating checklists such as this one, and by promoting physical activity where possible, encouraging the fair rotation of tasks between employees to avoid them consistently making repetitive movements, and ensuring that workers have the capacity to take regular breaks.
Why our next posture is the best posture
However, maintaining a good posture at all times is not enough to reduce the risk of MSDs, and can even be harmful. Static postures, even if ergonomic, are still a risk factor if over-used. Our body requires movement and variety, which is why the best approach is to use a variety of ergonomic postures in rotation, breaking up long periods of static working with stretching, exercise, and movement. This is known as adopting ‘dynamic positions’.
It is important not only for workers who spend much of their day seated, but also for workers who primarily stand – such as factory workers in assembly lines. In both cases, sitting and standing are not opposites. The opposite of both is movement. Changing postures between sitting and standing is not sufficient for any worker – the working environment must still offer ways of varying their postures and incorporating movement into their daily working routines. What’s more, if standing work cannot be avoided, workers do not need lots of space in order to adopt dynamic positions in a healthy way. Blood flow propulsion mechanisms can still work correctly even if the worker is only moving around in one square metre. However it is still the case that they should have a break after 30 minutes of standing.
Work should therefore not only facilitate good postures, but ensure that good, ergonomic postures are also dynamic. Switching between sitting, standing and moving while ensuring that the musculoskeletal frame is not under any unnecessary tension can help sedentary workers avoid the onset of MSDs and other health problems. For more information visit the priority area on sedentary work.
References
EU-OSHA. (September 16, 2021). Static postures are harmful – dynamic postures at work are key to musculoskeletal health. https://healthy-workplaces.eu/en/media-centre/news/static-postures-are-harmful-dynamic-postures-work-are-key-musculoskeletal-health?
Hansraj, K. K. (2014). Assessment of Stresses in the Cervical Spine Caused by Posture and Position of the Head. Surgical Technology International, 25, 277–79. https://pubmed.ncbi.nlm.nih.gov/25393825/
Paluch, A.E., Gabriel, K.P., Fulton, J.E., et al.(2021). Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study. JAMA Netw Open, 4(9):e2124516. https://doi.org/10.1001/jamanetworkopen.2021.24516
Peper, E., Harvey, R. & Faass, N. (2020). TechStress-How Technology is Hijacking our Lives, Strategies for Coping and Pragmatic Ergonomics. Berkeley: North Atlantic books. https://www.penguinrandomhouse.com/books/232119/tech-stress-by-erik-peper-phd/
Useful resources about breathing, phytonutrients and exercise
Posted: June 30, 2021 Filed under: behavior, Breathing/respiration, cancer, Evolutionary perspective, health, Nutrition/diet, self-healing, Uncategorized | Tags: diet, exercise, immune system, nasal breathing, phytonutrients, respiration 1 Comment
Dysfunctional breathing, eating highly processed foods, and lack of movement contribute to development of illnesses such as cancer, diabetes, cardiovascular disease and many chronic diseases. They also contributes to immune dysregulation that increases vulnerability to infectious diseases, allergies and autoimmune diseases. If you wonder what breathing patterns optimize health, what foods have the appropriate phytonutrients to support your immune system, or what the evidence is that exercise reduces illness and promotes longevity, look at the following resources.
Breath: the mind-body connector that underlies health and illness
Read the outstanding article by Martin Petrus (2021). How to breathe.
https://psyche.co/guides/how-to-breathe-your-way-to-better-health-and-transcendence
You are the food you eat
Watch the superb webinar presentation by Deanna Minich, MS., PHD., FACN, CNS, (2021) Phytonutrient Support for a Healthy Immune System.
Movement is life
Explore the summaries of recent research that has demonstrated the importance of exercise to increase healthcare saving and reduce hospitalization and death.
Reactivate your second heart
Posted: June 14, 2021 Filed under: behavior, computer, digital devices, ergonomics, Evolutionary perspective, Exercise/movement, health, Pain/discomfort, posture, screen fatigue, self-healing, zoom fatigue | Tags: blood clots, blood flow, calf muscle, cardiovascular disease, deep vein thrombosis, edema, exhaustion, Sitting disease, tired legs, Type 2 diabetes 6 CommentsMonica Almendras and Erik Peper
Adapted from: Almendras, M. & Peper, E. (2021). Reactivate your second heart. Biofeedback, 49(4), 99-102. https://doi.org/10.5298/1081-5937-49.04.07
Have you ever wondered why after driving long distances or sitting in a plane for hours your feet and lower leg are slightly swollen (Hitosugi, Niwa, & Takatsu, 2000)? It is the same process by which soldiers standing in attention sometimes faint or why salespeople or cashiers, especially those who predominantly stand most of the day, have higher risk of developing varicose veins. By the end of the day, they feel that their legs being heavy and tired? In the vertical position, gravity is the constant downward force that pools venous blood and lymph fluid in the legs. The pooling of the blood and reduced circulation is a contributing factor why airplane flights of four or more hours increases the risk for developing blood clots-deep vein thrombosis (DVT) (Scurr, 2002; Kuipers et al., 2007). When blood clots reaches the lung, they can cause a pulmonary embolisms that can be fatal. In other cases, they may even travel to the brain and cause strokes.[1]
Sitting without moving the leg muscles puts additional stress on your heart, as the blood and lymph pools in the legs. Tightening and relaxing the calf muscles can prevent the pooling of the blood. The inactivity of your calf muscles does not allow the blood to flow upwards. The episodic contractions of the calf muscles squeezes the veins and pumps the venous blood upward towards the heart as illustrated in figure 1. Therefore, it is important to stand, move, and walk so that your calf muscle can act as a second heart (Prevosti, April 16, 2020).

Figure 1. Your calf muscles are your second heart! The body is engineered so that when you walk, the calf muscles pump venous blood back toward your heart. Reproduced by permission from Dr. Louis Prevosti of the Center for Vein Restoration (https://veinatlanta.com/your-second-heart/).
To see the second heart in action watch the YouTube video, Medical Animation Movie on Venous Disorders, by the Sigvaris Group Europe (2017).
If you stand too long and experienced slight swelling of the legs, raise your feet slightly higher than the head, to help drain the fluids out of the legs. Another way to reduce pooling of fluids and prevent blood clots and edema is to wear elastic stockings or wrap the legs with intermittent pneumatic compression (IPC) devices that periodically compresses the leg (Zhao et al., 2014). You can also do this by performing foot rotations or other leg and feet exercises. The more the muscle of the legs and feet contract and relax, the more are the veins episodically compressed which increases venous blood return. Yet in our quest for efficiency and working in front of screens, we tend to sit for long time-periods.
Developing sitting disease
Have you noticed how much of the time you sit during the day? We sit while studying, working, socializing and entertaining in front of screens. This sedentary behavior has significantly increased during the pandemic (Zheng et al, 2010). Today, we do not need to get up because we call on Amazon’s Alexa, Apple’s Siri or Google’s Hey Google to control timers, answer queries, turn on the lights, fan, TV, and other home devices. Everything is at our fingertips and we have finally become The Jetsons without the flying cars (an American animated sitcom aired in the 1960s). There is no need to get up from our seat to do an activity. Everything can be controlled from the palm of our hand with a mobile phone app.
With the pandemic, our activities involve sitting down with minimum or no movement at all. We freeze our body’s position in a scrunch–a turtle position–and then we wonder why we get neck, shoulder, and back pains–a process also observed in young adults or children. Instead of going outside to play, young people sit in front of screens. The more we sit and watch screens, the poorer is our mental and physical health (Smith et al., 2020; Matthews et al., 2012). We are meant to move instead of sitting in a single position for eight or more hours while fixating our attention on a screen.
The visual stimuli on screen captures our attention, whether it is data entry, email, social media, or streaming videos (Peper, Harvey & Faass, 2020). While at the computer, we often hold up our index finger on the mouse and wait with baited breath to react. Holding this position and waiting to click may look harmless; however, our right shoulder is often elevated and raised upward towards our ear. This bracing pattern is covert and contributes to the development of discomfort. The moment your muscles tighten, the blood flow through the muscle is reduced (Peper, Harvey, & Tylova, 2006). Muscles are most efficient when they alternately tighten and relax. It is no wonder that our body starts to scream for help when feeling pain or discomfort on our neck, shoulders, back and eyes.
Why move?

Figure 2a and 2b Move instead of sit (photos source: Canva.com).
The importance of tightening and then relaxing muscles is illustrated during walking. During the swing phase of walking, the hip flexor muscles relax, tighten, relax again, tighten again, and this is repeated until the destination is reached. It is important to relax the muscles episodically for blood flow to bring nutrients to the tissue and remove the waste product. Most people can walk for hours; however, they can only lift their foot from the floor (raise their leg up for a few minutes) till discomfort occurs.
Movement is what we need to do and play is a great way to do it. Dr. Joan Vernikos (2016) who conducted seminal studies in space medicine and inactivity physiology investigated why astronauts rapidly aged in space and lost muscle mass, bone density and developed a compromised immune system. As we get older, we are hooked on sitting, and this includes the weekends too. If you are wondering how to separate from your seat, there are ways to overcome this. In the research to prevent the deterioration caused by simulating the low gravity experience of astronauts, Dr. Joan Vernikos (2021) had earthbound volunteers lie down with the head slightly lower than the feet on a titled bed. She found that standing up from lying down every 30-minutes was enough to prevent the deterioration of inactivity, standing every hour was not enough to reverse the degeneration. Standing stimulated the baroreceptors in the neck and activated a cardiovascular response for optimal health (Vernikos, 2021).
We have forgotten something from our evolutionary background and childhood, which is to play and move around. When children move around, wiggle, and contort themselves in different positions, they maintain and increase their flexibility. Children can jump and move their arms up, down, side to side, forward, and backward. They do this every day, including the weekends.
When was the last time you played with a child or like a child? As an adult, we might feel tired to play with a child and it can be exhausting after staring at the screen all day. Instead of thinking of being tired to play with your child, consider it as a good workout. Then you and your child bond and hopefully they will also be ready for a nap. For you, not only do you move around and wake up those muscles that have not worked all day, you also relax the tight muscles, stretch and move your joints. Do playful activities that causes the body to move in unpredictable fun ways such as throwing a ball or roleplaying being a different animal. It will make both of you smile–smiling helps relaxation and rejuvenates your energy.
It is not how much exercise you do, it is how long you sit. The longer you sit without activating your second heart the more are you at risk for cardiovascular disease and diabetes independent of how much exercise you do (Bailey et al., 2019).
Use it or lose it! Activate your calves!
- Interrupt sitting at your desk/computer every 30-minutes by getting up and walking around.
- Stand up and walk around when using your phone.
- Organize walking meetings instead of sitting around a table.
- Invest in a sit-stand desk while working at the computer. While working, alternate positions. There should be a balance between standing and sitting, because too much of one can lead to problems. By taking a short standing up break to let your blood pump back to the heart is beneficial to avoid health problems. Exercise alone, a fancy new ergonomic chair or expensive equipment is not enough to be healthy, it is important to add those mini breaks in between (Buckley et al, 2015).
For a holistic perspective to stay healthy while working with computers and cellphones, see the comprehensive book by Peper, Harvey and Faass (2020), TechStress: How Technology is Hijacking Our Lives, Strategies for Coping, and Pragmatic Ergonomics.
References
Buckley, J.P., Hedge, A., Yates, T., et al. (2015). The sedentary office: an expert statement on the growing case for change towards better health and productivity British Journal of Sports Medicine, 49, 1357-1362.
Prevosti, L. (2020, April 16). Your second heart. https://veinatlanta.com/your-second-heart/
Vernikos, J. (2021, February 25). Much ado about standing. Virtual Ergonomic Summit. American Posture Institute. https://api.americanpostureinstitute.com/virtual-ergonomics-summit-free-ticket?r_done=1
[1] We even wonder if excessive sitting during the COVID-19 pandemic is a hidden risk factor of the rare negative side effects of blood clots in the brain, that can occur with the AstraZeneca and Johnson and Johnson coronavirus vaccine (Mahase, 2021).